Abstract
Background and aim
We recently reported mucosal infiltration of IgG4-expressing plasma cells in a patient with chronic antibiotic-refractory pouchitis (CARP). The role of serum IgG4 in the pathogenesis and clinical course of ileal pouch disorders has not been investigated. We hypothesized that IgG4-mediated autoimmunity may be a contributing factor in for CARP. The aims of the study were to investigate the prevalence of elevated serum IgG4 in symptomatic patients with ileal pouches and to characterize clinical features of pouch disorders in these patients.
Methods
A total of 124 consecutive symptomatic patients with ileal pouches from our subspecialty Pouchitis Clinic were enrolled in the study from January to October 2010. Serum IgG4 was measured at the time of presentation. Demographic, clinical, and laboratory characteristics were compared between the study (with serum IgG4 ≥112 mg/dl) and control (with serum IgG4 <112 mg/dl) groups.
Results
There were ten patients (8.0%) with high serum IgG4 in the study group, while the remaining 114 (92%) patients were in the control group. The prevalence of elevated serum IgG4 in this series was 8%. None of the patients had a confirmed diagnosis of autoimmune pancreatitis. The median serum IgG4 in the study group was 144.5 vs. 14 mg/dl in the control group. The mean age of patients in the study and control groups was 35.5 ± 14.5 and 42.0 ± 13.2 years, respectively (p = 0.137). Two patients in the study group (20.0%) had concurrent autoimmune disorders as compared to 19 patients (16.7%) in the control group (p = 0.788). Three (30.0%) patients in the study group had coexisting primary sclerosing cholangitis (PSC) in contrast to 15 (13.2%) in the control group (p = 0.147). Among the study group patients, five (50.0%) had CARP and one (10%) had Crohn’s disease (CD) of the pouch, while in the control group, 23 (20.2%) had CARP and 24 (21.1%) patients had CD of the pouch (p = 0.273). CARP was more commonly seen in patients with high serum IgG4 than patients with a normal IgG4 (50.0% vs. 20.2%, p = 0.03).
Conclusions
Approximately 8% of pouch patients presenting with symptoms of pouch dysfunction to our clinic had elevated serum IgG4. Patients with elevated serum IgG4 were more likely to have CARP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Elevation of serum IgG4 is considered to be one of the biomarkers for autoimmune pancreatitis (AIP). At the tissue level, pancreas along with other involved organs has characteristic infiltration with abundant IgG4-positive plasma cells termed as IgG4-related sclerosing disease.1–6 While hypergammaglobulinemia was reported in 37–76% of individuals with AIP or IgG4-related sclerosing disease, elevated serum IgG4 appears to be more sensitive and specific for its diagnosis.7 Recent studies suggest that IgG4 may play a role in the disease process of inflammatory bowel disease (IBD) in patients with or without a history of pancreatic disease.3
Idiopathic pouchitis is believed to be associated with dysbiosis, as the majority of patients respond favorably to antibiotic therapy. However, some patients do not respond to routine 2-week antibiotic therapy, which is termed chronic antibiotic-refractory pouchitis (CARP).8 While multiple factors may contribute to the refractory course of pouchitis, autoimmunity may play a role in its pathogenesis. Our previous study showed that the presence of AID was associated with a 2-fold increase in the risk for CARP.9 In addition, we recently reported a patient with CARP and multiple autoimmune disorders (AID) who had histologic evidence of IgG4-positive plasma cell infiltration in pouch biopsy without IgG4-repressing plasma cell infiltration of the ileum prior to colectomy surgery.9 These findings lead us to embark on our current project with the hypothesis that IgG4-mediated autoimmunity may contribute to the disease process of CARP. The aims of the study were to investigate the prevalence of elevated serum IgG4 in symptomatic patients with ileal pouches and to characterize clinical features of pouch disorders in these patients.
Patients and Methods
Patients
This study was approved by our Institutional Review Board (IRB). The study involved consecutive eligible symptomatic patients presenting to the Pouchitis Clinic from January to October 2010. Patient’s demographic and clinical data were retrieved from the IRB approved, prospectively maintained database. Patients were divided into two groups: those with serum IgG4 greater than 112 mg/dl (the study group) and those with no elevation of serum IgG4 (<112 mg/dl) (the control group). The cut-off level was set by institutional laboratory normal range.
Inclusion and Exclusion Criteria
Inclusion criteria were patients with ileal pouch-anal anastomosis (IPAA) for underlying ulcerative colitis (UC) with symptoms of frequency, urgency, pelvic discomfort, and abdominal cramps. Exclusion criteria were IPAA patients with a preoperative diagnosis of familial adenomatous polyposis, and patients with surgical complications of IPAA, including pouch sinus, abscess, and pelvic sepsis.
Clinical, Endoscopic, Laboratory, and Histologic Evaluation
Demographic, clinical, endoscopic, and histologic data were reviewed. As part of our routine clinical practice, all symptomatic patients underwent an outpatient pouch endoscopy with biopsy. Segmental evaluation and biopsies of the afferent limb, pouch, and anal transitional zone (the rectal cuff) were routinely performed during pouch endoscopy. The endoscopic features were documented and biopsies from each site separately labeled and submitted. Examination under anesthesia, contrast pouchography, computed tomography enterography, or magnetic resonance imaging of the pelvis was performed when Crohn’s disease (CD) of the pouch was suspected. The modified Pouchitis Disease Activity Index (mPDAI) scores (range 0–12 points) were used to quantify symptom and endoscopy inflammation.10,11
An elevated concentration of serum IgG4 was defined by values greater than 112 mg/dl according to the reference standard used at our institution.
Definitions of Variables
CARP was defined as pouchitis (mPDAI ≥5 points) that did not respond to a 4-week antibiotic course of a single antibiotic (metronidazole [20 mg kg−1 day−1] or ciprofloxacin [500 mg bid]).12 The diagnosis of CD of the pouch was defined by ulcerated lesions of the small bowel or afferent limb without diffuse pouchitis (excluding backwash pouchitis) that persisted after ≥4 weeks of antibiotic therapy or by ulcerated strictures in the distal small bowel or pouch inlet with concurrent ulcers or inflammation of the afferent limb.13 Those criteria were applied after the exclusion of non-steroidal anti-inflammatory drug (NSAID) use at the time of diagnosis. Irritable pouch syndrome (IPS) was defined as the presence of abdominal pain, pelvic discomfort, and diarrhea with no inflammation of the afferent limb, pouch, or cuff on endoscopy. Any other associated features for AIP, including primary sclerosing cholangitis (PSC)-like biliary changes and retroperitoneal fibrosis, were evaluated.
Demographic and clinical variables were defined as follows: “smoking”: ever consumption of ≥7 cigarettes per week since the surgery; “family history of inflammatory bowel IBD”: CD or UC in first-degree relatives; “duration of UC”: the time interval between UC diagnosis and pouch construction; “duration of pouch”: the time interval between completion of IPAA with ileostomy closure and entry into the study; “extensive colitis”: endoscopic, macroscopic, or microscopic disease extending proximal to the splenic flexure; “indeterminate colitis”: a histopathological diagnosis on proctocolectomy specimens that defied a clear distinction between CD and UC; “indication for colectomy”: the primary reason for the surgery based on clinical presentation and preoperative diagnostic studies; “use of NSAID”: regular use of NSAID more often than weekly at the entry into the current study; “PSC”: the presence of intra- or extrahepatic bile duct abnormalities documented on endoscopic retrograde cholangiopancreatography and/or magnetic resonance cholangiopancreatography. Patients with PSC may or may not undergo orthotopic liver transplantation; “autoimmune mediated disorders”: including adult-onset asthma, psoriasis, type 1 diabetes, rheumatoid arthritis, ankylosing spondylitis, autoimmune thyroid disease, systemic lupus erythematosus, celiac disease, pernicious anemia, and AIP.
Statistical Analysis
Descriptive statistics were computed for all factors in both the study and the control group. This included mean and percentiles for continuous factors and frequencies for categorical factors. Associations with categorical variables were done by Fisher’s exact test or χ2 test. Associations with quantitative and ordinal variables were performed by Student’s t-test or Wilcoxon’s rank sum test as appropriate.
Results
Demographic and Clinical Characteristics
The basic demographic and clinical information including NSAID use at the time of pouch endoscopy, duration of the pouch, type of pouch, preoperative and postoperative use of biologics and immunomodulators, the presence of concomitant autoimmune disorders, co morbidities and duration of IBD are summarized in Table 1.
There were ten patients (prevalence = 8.0%) with high serum IgG4 (the study group), while the remaining 114 (92%) patients had normal IgG4 (the control group). None of the patients had a confirmed diagnosis of AIP. The median serum IgG4 in the study group was 144.5 vs. 14 mg/dl in the control group. The mean age of patients in the study and control groups was 35.5 ± 14.5 and 42.0 ± 13.2 years, respectively (p = 0.137). Two patients in the study group (20.0%) had concurrent autoimmune disorders as compared to 19 patients (16.7%) in the control group (p = 0.788). Three (30.0%) patients in the study group had coexisting PSC in contrast to 15 (13.2%) in the control group (p = 0.147). Of the ten patients in the study group, five (50%) had CARP and one (10%) had CD of the pouch, while in the control group, 23 (20.2%) had CARP and 24 (21.1%) patients had CD of the pouch (p = 0.273). CARP was significantly more common in the study group than in the control group IgG4 (50% vs. 20.2%, p = 0.03).
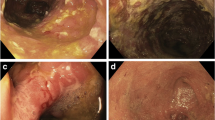
Endoscopic Evaluation
Endoscopic inflammation of the afferent limb and pouch was documented. There was a significant difference in the PDAI symptom subscores between the study and control groups (3.88 ± 0.9 vs. 2.88 ± 1.5, p = 0.042). However, there was no statistically significant difference in the PDAI endoscopic subscores in the afferent limb and pouch body between the patients in the study and control groups (Table 2).
Discussion
In this study, we investigated the possible role of serum IgG4 in pouchitis. Pouchitis likely represents a spectrum of disease processes, ranging from antibiotic-responsive, antibiotic-dependent, to antibiotic-refractory phenotypes. From etiological and pathogenetic perspectives, a variety of factors may contribute to the initiation, development, and progression of the disease process. These factors include genetic predisposition, dysbiosis, altered mucosal immunity, and colonic metaplasia due to fecal stasis. Immune-mediated factors likely play a major role in the pathogenesis of pouchitis, particularly in CARP and CD of the pouch. Our study showed that 8% of symptomatic patients at our Pouchitis Clinic had high serum IgG4. In addition, we found that patients with high serum IgG4 were more likely to have CARP. Also we found higher PDAI symptom subscores in patients with elevated serum IgG4. These findings suggest that immune-mediated mechanisms through IgG4 play a role in the disease process or pathogenesis in a subset of patients with pouchitis.
AIP is an increasingly recognized chronic inflammatory disease and criteria (the HISORt criteria) for the diagnosis of AIP were proposed.14 Association between AIP with other autoimmune conditions such as PSC, retroperitoneal fibrosis, and sclerosing sialadenitis has been described.4 One of the serology markers for AIP is an elevated serum IgG4. IgG4 is the rarest of the IgG subclasses and normally accounts for only 3% to 6% of the total IgG in the serum.15 The serological criteria dictate that serum IgG4 need to be higher than 112 mg/dl in order to be considered for the diagnosis of IgG4-associated disease. A previous study reported that in patients with IBD and AIP, serum IgG4 was elevated in 50% of patients.3 That study included all patients with a confirmed diagnosis of AIP which would explain the high prevalence of elevated IgG4. We found an elevation in serum IgG4 in 8% of patients in the study group. Similar elevations in IgG4 have been reported in 7–10% of patients with pancreatic cancer and 9% of patients with PSC.16 In this study, we observed elevated IgG4 in three patients with PSC in the study group. It would be very hard to discern whether the elevation of serum IgG4 was related to PSC or CARP or was instead just an “innocent bystander” phenomenon.
The etiology and association error of elevated IgG4 with pouchitis are not clear. The current study showed that CARP was more common in patients with high serum IgG4. However, we did not see significant difference in the prevalence of AID between the study and the control group. This might have resulted from a type II error. The relationship between serum IgG4 and CARP warrants further investigation. Since IgG4-associated cholangiopathy has also been reported in two HLA identical siblings with UC there could be a role for IgG4 in IBD pathogenesis in patients even in the absence of AIP.17
The findings of the current study have several clinical implications. Patients with elevated IgG4 may represent a distinct subtype of pouchitis. Alterations in T-cell immunity with imbalance between proinflammatory and immunoregulatory cytokines have been described in pouchitis patients.13 The findings of this study suggest a role of alterations in B cell immunity in the pathogenesis of pouchitis in some patients, as further evidenced by their role in IgG4 sclerosing disease.18 The lymphoplasmacytic infiltrates seen in these patients include polyclonal B cells, plasma cells, and T cells. B lymphocytes can affect the inflammatory response by interaction with regulatory T cells.19 Rituximab, a monoclonal antibody against CD20 has been used in the management of IgG4 related sclerosing disease.20 Similarly, in patients with elevated IgG4 in pouchitis, treatment with other options including anti-B cell therapies can be explored. By definition, patients CARP were refractory to traditional antibiotic therapy. Thus some patients with CARP or even CD of the pouch with elevated serum IgG4 might be considered to be treated with B-cell targeted therapies. Glucocorticoids suppress cellular immunity and also humoral responses via inhibiting expression of IL-2 and IL-2 receptors on B cells to diminish B cell clone expansion and antibody synthesis. This property explains the efficacy of budesonide or prednisone in some patients with CARP from our clinical experience. Serum assay of IgG4 is routinely available in clinical labs. The finding of elevated serum IgG4 may help direct a proper therapy for the patients with pouchitis as well as exploration of concurrent hepatopancreaticobiliary disease in patients with IPAA.
This study has several limitations. The study population was recruited from a subspecialty Pouchitis Clinic. This might have had referral or selection biases and the findings would be difficult to be extrapolated to the general pouch population. Statistical significance was not achieved in certain other parameters including the coexistence of AID, which might have been from type II errors. We are continuing to recruit patients to generate a larger sample size for future multivariable analyses. We do not know whether elevated IgG4 is an epiphenomenon secondary to unrecognized antigens or whether it is a result of inflammation and disease process. We know that at least in patients with IgG4-sclerosing disease, a high level of serum IgG4 is not directly pathogenic as patients may have increase in IgG4 on treatment with clinical improvement.21 The role of serum IgG4 in the pathogenesis of pouchitis in a subset of patients with IPAA warrants further study, which would help exploring treatment options for patients with refractory pouch disorders.
In conclusion, a subset of symptomatic pouch patients had elevated serum IgG4. It appears that pouch patients with an elevated serum IgG4 were more likely to have CARP. Future studies to investigate the role of IgG4 in pathogenesis of pouchitis and its clinical utility in the diagnosis, treatment, and prediction of prognosis are warranted.
Abbreviations
- AID:
-
Autoimmune disorders
- AIP:
-
Autoimmune pancreatitis
- CD:
-
Crohn’s disease
- CARP:
-
Chronic antibiotic refractory pouchitis
- IBD:
-
Inflammatory bowel disease
- IPS:
-
Irritable pouch syndrome
- IPAA:
-
Ileal pouch-anal anastomosis
- NSAID:
-
Non-steroidal anti-inflammatory drug
- PSC:
-
Primary sclerosing cholangitis
- PDAI:
-
Pouchitis Disease Activity Index
- UC:
-
Ulcerative colitis
References
Kamisawa T, Okamoto A, Funata N. Clinicopathological features of autoimmune pancreatitis in relation to elevation of serum IgG4. Pancreas 2005;31:28–31.
Hamano H, Kawa S, Horiuchi A, et al. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N Engl J Med. 2001;344:732–8.
Ravi K, Chari ST, Vege SS, Sandborn WJ, Smyrk TC, Loftus EV. Inflammatory bowel disease in the setting of autoimmune pancreatitis. Inflamm Bowel Dis. 2009;15:1326–30.
Kamisawa T, Funata N, Hayashi Y, et al. A new clincopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38:982–4.
Kamisawa T, Funata N, Hayashi Y. Lymphoplasmacytic sclerosing pancreatitis is a pancreatic lesion of IgG4-related systemic disease. Am J Surg Pathol. 2004;24:1114.
Deheragoda MG, Church NI, Rodriguez-Justo M, et al. The use of immunoglobulin G4 immunostaining in diagnosing pancreatic and extrapancreatic involvement in autoimmune pancreatitis. Clin Gastroenterol Hepatol. 2007;5:1229–34.
Kim KP, Kim MH, Song MH, et al. Autoimmune chronic pancreatitis. Am J Gastroenterol. 2004;99:1605–16.
Shen B, Remzi FH, Nutter B, Bennett AE, Lashner BA, Lavery IC, Brzezinski A, Nutter B, Bambrick ML, Queener E, Fazio VW. Association between immune-associated disorders and adverse outcomes of ileal pouch-anal anastomosis. Am J Gastroenterol. 2009;104:655–64.
Shen B, Bennett AE, Navaneethan U. IgG4 associated pouchitis. Inflamm bowel Dis. 2011;17:1247–8.
Sandborn WJ, Tremaine WJ, Batts KP, et al. Pouchitis after ileal pouch-anal anastomosis: a pouchitis disease activity index. Mayo Clin Proc. 1994;69:409–15.
Shen B, Achkar JP, Connor JT, et al. Modified pouchitis disease activity index: a simplified approach to the diagnosis of pouchitis. Dis Colon Rectum. 2003;46:748–53.
Navaneethan U, Shen B. Pros and cons of antibiotic therapy for pouchitis. Expert Rev Gastroenterol Hepatol. 2009;3:547–59.
Navaneethan U, Shen B. Diagnosis and management of pouchitis and ileoanal pouch dysfunction. Curr Gastroenterol Rep. 2010;12:485–94.
Chari ST, Smyrk TC, Levy MJ, et al. Diagnosis of autoimmune pancreatitis: the Mayo Clinic experience. Clin Gastroenterol Hepatol. 2006; 4:1010–6.
Morselli-Labate AM, Pezzilli R. Usefulness of serum IgG4 in the diagnosis and follow up of autoimmune pancreatitis: a systematic literature review and meta-analysis. J Gastroenterol Hepatol. 2009;24:15–36.
Park DH, Kim MH, Chari ST. Recent advances in autoimmune pancreatitis. Gut. 2009;58:1680–9.
Dastis SN, Latinne D, Sempoux C, Geubel AP. Ulcerative colitis associated with IgG4 cholangitis: similar features in two HLA identical siblings. J Hepatol. 2009;51:601–5.
Kojima M, Sipos B, Klapper W, et al. Autoimmune pancreatitis: frequency, IgG4 expression, and clonality of T and B cells. Am J Surg Pathol. 2007;31:521–8.
Yang Z, Novak A, Ziesmer S, et al. Attenuation of CD8(+) T-cell function by CD4(+)CD25(+) regulatory T cells in B-cell non- Hodgkin’s lymphoma. Cancer Res. 2006;15:10145–52
Khosroshahi A, Bloch DB, Deshpande V, Stone JH. Rituximab therapy leads to rapid decline of serum IgG4 levels and prompt clinical improvement in IgG4-related systemic disease. Arthritis Rheum. 2010;62:1755–62.
Topazian M, Witzig TE, Smyrk TC, et al. Rituximab therapy for refractory biliary strictures in immunoglobulin G4-associated cholangitis. Clin Gastroenterol Hepatol. 2008;6:364–6
Acknowledgement
This study was partially supported by a BMRP grant from the Eli and Edyth Broad Foundation.
Conflict of interest
The authors declared that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Navaneethan, U., Venkatesh, P.G.K., Kapoor, S. et al. Elevated Serum IgG4 is Associated with Chronic Antibiotic-Refractory Pouchitis. J Gastrointest Surg 15, 1556–1561 (2011). https://doi.org/10.1007/s11605-011-1587-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1587-6