Abstract
Background
Specific mutations leading to the development of various histological grades of intraductal papillary mucinous neoplasm (IPMN) have been partially characterized.
Methods
Analysis of 323 oncogenic mutations in 22 tumor-related genes was conducted, using a chip-based matrix-assisted laser desorption time-of-flight mass spectrometer of DNA extracted from microdissected cells of low-grade (n = 14), borderline (n = 6), and invasive IPMN (n = 7). Additional assays were performed on the DNA extracted from dyplastic cells found in the background of the adenocarcinoma.
Results
We identified 9 K-ras mutations (low grade, 2/14; borderline, 1/6; invasive, 6/7), 3 p53 mutations (low grade, 1/14; invasive 2/7), and 2 PIK3CA mutations (low grade, 1/14; invasive, 1/7). K-ras, p53, and PIK3CA mutations present in the invasive cancer were absent in the adjacent precursor cells in 50% of the cases. In one patient, K-ras mutation was present in the precursor lesion and absent in the adjacent invasive lesion.
Conclusions
Of the 22 screened tumor-related genes, only K-ras, p53, and PIK3CA mutations were found in IPMN. K-ras mutations are more prevalent in invasive than premalignant IPMN. The variable coexistence of mutations in the invasive cancer and in the adjacent precursor cells may point to the heterogeneous nature of this tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intraductal papillary mucinous neoplasm (IPMN) of the pancreas is a relatively new clinicopathological entity, first reported in 1982 by Ohhashi et al.1 and recently introduced into the World Health Association (WHO) classification.2 These tumors are characterized by papillary projections of duct epithelium, mucin production, and dilatation of the pancreatic duct. Histologically, IPMN is distinguished by replacement of normal ductal epithelium by mucinous metaplasia as well as a broad spectrum of pathological disorders, including simple hyperplasia (adenoma), cell atypia (borderline tumor), carcinoma in situ, and invasive adenocarcinoma that displays invasion of malignant cells into the pancreatic tissue surrounding the ducts. At the time of diagnosis, approximately 40–60% of the tumors have a component of invasive adenocarcinoma.3–5 In addition, IPMN is found in the background of 10% of pancreatic adenocarcinoma cases, suggesting that it had been the initial lesion leading to cancer in these patients.6
The histological variety of IPMN and the presence of premalignant dysplastic cells in the pancreatic tissue surrounding the invasive component are an excellent system in which to study the genetic alterations involved in tumor development. The specific mutations leading to the development of various histological grades of IPMN (hyperplasia, atypia, invasive cancer) have been partially characterized in previous studies. Reported genetic alterations identified in IPMN include mutations in K-ras,7 PIK3CA,8 and BRAF9 genes and overexpression of the TP53 and ERBB2 proteins.10,11 The role and the timing of specific oncogenic mutations in the gradual progression of adenoma to carcinoma in IPMN, however, have not been clearly elucidated. Attempts to characterize the oncogenic mutations in the different grades of IPMN within the same tumor by using techniques of tissue microdissection12,13 have demonstrated early polyclonal epithelia gradually replaced by monoclonal neoplastic cells and gaining K-ras mutations as the tumor progresses.
The aim of our current study was to explore the genetic alterations responsible for tumor development in IPMN by screening the different histological grades of IPMN for the presence of oncogenic mutations and by evaluating whether genetic alterations present in invasive IPMN coexist in the adjacent precancerous cells. Towards this end, we based our methods on the hypothesis that gain-of-function mutations do not occur randomly in most known oncogenes and tumor suppressor genes. Instead, changes affecting a small number of “hotspot” codons often account for the majority of somatic mutations. Therefore, a limited number of genetic assays could effectively deal with a large proportion of known mutations. A high-throughput genotyping analysis could provide an effective means to screen for major known cancer mutations in IPMN tissue. Here, we performed a high-throughput analysis of multiple oncogenic mutations in the different histological grades of IPMN using a chip-based matrix-assisted laser desorption time-of-flight (MALDI-TOF) mass spectrometer (Sequenom, San Diego, CA, USA).
Materials and Methods
Patients and Tissue Samples
We used a prospective database of all patients identified as having IPMN in our institutional database between February 2002 and May 2008. Additionally, all pathological results of pancreatic resections performed in our department from 1995 to 2002 (350 specimens) were reviewed. These latter patient data were derived from pathology reports and therefore subject to the pathologist’s diligence. We are aware that some IPMN cases that were operated before February 2002 were probably missed and therefore not included in our analysis. A pathologist experienced in pancreatic pathology (E.B.) reviewed the histological slides in all cases suspected of being IPMN according to the pathological report. The selected cases were reviewed again by another pathologist (S.M.), and following confirmation of a diagnosis of IPMN, the specimens were entered into the study. Histological typing of the tumors was performed according to the classification recommended in the revised WHO classification in 20002 as having tall, columnar, mucin-containing epithelium with or without papillary proliferations and involving the pancreatic ducts. Tumors were graded as low-, moderate-, and high-grade dysplasia and as invasive carcinomas. High-grade dysplasia was differentiated from invasive carcinoma according to the presence of stromal invasion.
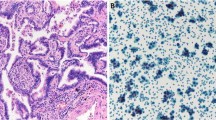
DNA Samples
Paraffin-embedded tumor samples were reviewed by one pathologist (S.M.) who marked tissue margins of invasive and noninvasive tumor and also confirmed that more than 90% of cells in the marked area were of tumor origin. Microdissection was then performed by hand. Eight micrometer-thick sections were cut from the paraffin-embedded tumor block and transferred onto glass slides, one of which was stained with hematoxylin and eosin, and the tissue margins were marked. The tumor within the marked margins was carefully removed by means of a sharp scalpel. The retrieved material was then transferred in a 1.5-mL Eppendorf tube. Eight to 12 sections were harvested for each case. Deparaffinization was performed using xylene. Genomic DNA was extracted using a classical DNA extraction technique.14
Selection of Oncogenic Mutations
Selection of oncogenic mutations was based on the methods of Thomas et al.15 who designed a245 genotyping assays of 238 somatic mutations in 17 human oncogenes. We added more mutations after we conducted searches of two databases of known somatic oncogenic mutations, Cosmic (catalogue of somatic mutations in cancer) and PubMed. The resulting list (supplementary Table 1) contained 323 genotyping assays of known somatic mutations involving 22 human oncogenes and tumor suppressor genes. Mutations with high prevalence in other cancers (e.g., P53, BRAF, K-ras family mutations) and genes with proven clinical implications (e.g., KIT and EGFR) were given preference.
MALDI-TOF Assay Outline
Genotyping assays were designed using the Sequenom MassARRAY Assay Design 3.0 software with a maximum of six multiplexed assays per well. Assays were designed manually for complex mutations. Specific primers flanking the mutation site and extension primers that bind adjacent to the mutation site were designed. A primer extension reaction was carried out following the amplification of the region of interest. The extension reaction included sequence-specific hybridization and sequence-dependent termination that generated different products for the mutated and wild-type alleles, each with its unique mass values. Genotyping was terminated by spotting the extension products onto silicone chips preloaded with proprietary matrices (SpectroChip; Sequenom) that were subsequently read by the MALDI-TOF mass spectrometer (Figs. 1, 2, 3, and 4).
Direct sequencing of the same patient of Fig. 1 demonstrating concurrent wild-type and mutant K-ras (G12V mutation)
Mass Spectrometric Genotyping
PCR amplifications were carried out in standard 384-well plates in a 5-μL final volume containing 40 ng of template DNA, 0.1 U of Taq polymerase (Hotstar Taq, Quiagen, Valencia, CA, USA), 0.2 mM of each deoxyribonucleotide triphosphate (dNTP), 200 nmol of each primer, 1 mM MgCl2, and Hotstar buffer. The primers are listed in Supplementary Table 2. The PCR thermal cycling was carried out in an ABI-9700 instrument with the following conditions: 15 min at 95°C, 30 s at 65°C, and 60 s at 72°C; and 38 cycles of 20 s at 95°C, 30 s at 53°C, and 60 s at 72°C. The PCR products were incubated with shrimp alkaline phosphatase (0.3 U in a total volume of 7 μL; 20 min at 37°C and 5 min at 85°C) in order to remove the non-incorporated dNTPs. The massEXTEND® (Sequenom) analysis was then conducted in a total volume of 9 μL containing 1 μL extension primer (Supplementary Table 2), 0.2 μL termination mix (list of specific termination mix for each assay in Supplementary Table 2), and 1.25 U ThermoSequenase (Sequenom) in 0.22× PCR buffer. The cycling conditions were: incubation for 2 min at 94°C followed by 99 cycles of 5 s at 94°C, 5 at 52°C, and 5 s at 72°C. Following this step, 6 mg of massEXTEND® cleanup resin (Sequenom) and 25 μL of H2O were added to remove extraneous salts. A Samsung nanodispenser was used to apply 15 nL of the extension products from each well of the sample plate onto the SpectroChips. Mass spectra were recorded on a Bruker Biflex MALDI-TOF mass spectrometer operated on the linear mode and finally analyzed by MassARRAY Typer Software (Sequenom).
Additional Assays
All assays found positive for mutation in the multiplex assay were repeated using a singleplex assay for the identified mutation. Singleplex assays for mutations found in adenocarcinoma specimens were also performed on the DNA extracted from microdissected IPMN dysplastic cells found in the background of the adenocarcinoma. The protocol followed for the singleplex assay was similar to that of the multiplex assay, with different reagent concentrations for the first PCR reaction (supplementary Table 2). Three milligrams of massEXTEND® cleanup resin (Sequenom) was used with 16 μL of H2O for salt removal.
Sequencing of K-ras Oncogene
Sequencing of the K-ras exon 2 was performed in 18 specimens in order to verify the results of the Sequenom assays. Following DNA extraction, genomic DNA (60 ng per sample) was amplified with primers covering the coding region and exon/intron border. DNA sequencing was performed with ABI’s automated sequencer at a commercial laboratory. The results were blindly compared with the results obtained from the Sequenom assays.
Ethical Considerations
The study protocol was approved by the Human Ethics Review Committee of the Ministry of Health and of the Tel Aviv Sourasky Medical Center.
Results
The 323 assays of 22 tumor-related genes were performed on 27 specimens, including 14 low-grade IPMNs, 6 moderate-grade IPMNs, and 7 invasive cancers arising on the background of IPMN. The clinical and molecular findings are summarized in Table 1. Additional singleplex assays of 2 K-ras mutations in codon 12 (G12D, G12V) were performed in another 7 specimens of invasive IPMN.
K-ras Mutations
K-ras mutations in codon 12 were found in 2 of 14 patients with low-grade IPMN (14.3%), in 1 of 6 patients with moderate-grade IPMN (14.3%), and in 6 of 7 patients with invasive IPMN (85.7%). No other mutations in K-ras oncogene were found. The two singleplex K-ras codon 12 mutation assays performed on two additional specimens of invasive IPMN revealed another two mutations. In the eight patients with invasive IPMN and a K-ras mutation, analysis of the background noninvasive IPMN demonstrated the same K-ras mutation in four patients, and no K-ras mutation in the other four patients (Table 2). A single patient with invasive carcinoma negative for K-ras mutation had a codon 12 mutation in the background IPMN. The other five patients with invasive IPMN and no K-ras mutation had no mutation in the background IPMN. The Sequenom results were fully matched with the direct sequencing results, including six assays with K-ras mutations and seven assays negative for K-ras mutations.
P53 Mutations
P53 mutations were found in three patients, including two patients with invasive IPMN (28%) and one patient with low-grade IPMN (5%). One patient with invasive IPMN had two mutations in the p53 gene. Analysis of the DNA from the adjacent noninvasive IPMN cells demonstrated the presence of one of these mutations (p53_20), but not the other (p53_8). The other patient with invasive IPNM had the same p53 mutation (p53_20) present in the background noninvasive IPMN (Table 2). The patient with noninvasive IPMN and p53 mutations had additional mutation in the PIK3CA gene.
PIK3CA Mutations
PIK3CA mutations were found in two patients, one of whom had noninvasive IPMN and another who had invasive IPMN. The patient with noninvasive IPMN had additional mutation in the p53 gene. Analysis of the DNA from the adjacent noninvasive IPMN cells failed to demonstrate any PIK3CA mutation in the patient with invasive IPMN (Table 2).
Patient Outcome
The relevant clinical data and long-term outcome of the patients are listed in Table 1. All patients with invasive cancer had at least one mutation in either K-ras (n = 6), PIK3CA (n = 1), or p53 (n = 2) genes. Only patients with K-ras mutations and no additional or other mutations experienced long-term disease-free survival. Five of the patients had positive surgical margins, all five with benign IPMN. The pathology of the main specimen of these patients was low-grade IPMN (n = 3), borderline IPMN (n = 1), and malignant IPMN (n = 1). Two of these patients experienced recurrence of IPMN and both had recurrence of noninvasive IPMN. Both of these patients did not have an oncogenic mutation. No clear clinical–molecular correlations could be demonstrated, possibly due to the small number of patients included in this study.
Discussion
We performed a high-throughput analysis of 323 hotspot mutations in 22 tumor-related genes in order to characterize the specific mutations in various grades of IPMN. Much of the comparative analysis depends on tumor differentiation determined by microscopic evaluation, which is subjective and user-dependent. We attempted to minimize this drawback by ensuring that all slides were re-evaluated by two independent pathologists who confirmed the diagnosis of IPMN as well as the specific grades of all the included slides. We identified 9 K-ras mutations (low grade in 2/14, borderline in 1/6, and invasive in 6/7), 3 p53 mutations (low grade in 1/14 and invasive in 2/7), and 2 PIK3CA mutations (low grade in 1/14 and invasive in 1/7). We based our mutation screening assays on a recently described MALDI-TOF-based assay of 238 mutations,15 to which we added 85 other mutations. The assay involves PCR amplification of the region containing the mutation, a primer extension reaction through the mutation site, generation of allele-specific extension products, and analysis using the MALDI-TOF mass spectrometer. This assay was compared to both Sanger sequencing and a highly sensitive pyrosequencing by a synthesis method15 for EGFR and K-ras mutations and was proved to be highly sensitive for mutation detection. In previous studies, we have shown that this method is capable of mutant detection down to 1% mutant allele for JAK2 mutations,16 and BCR ABL kinase domain mutations.17 In the current study, we also verified the assay’s results for the K-ras mutations using direct sequencing, and all assays that were found to be positive for mutations were repeated using singleplex assays.
The progression of pancreatic adenocarcinoma is strongly associated with the presence of K-ras mutations found in close to 100% of lesions.18–20 K-ras mutations have been shown to occur at a relatively early stage of carcinogenesis in the pancreas.21,22 The frequency of K-ras mutations in pancreatic adenocarcinoma evolving from IPMN is lower, reportedly between 14% and 86%.7,23–25 We found K-ras mutations significantly less frequently in early lesions than in invasive IPMN cancers. It is hypothesized that IPMN is a precursor lesion of pancreatic carcinoma and that a sequenced grade-continuum from low-grade dysplasia exists, leading eventually to invasive cancer development. To date, there are no reliable tools to enable a clear identification of invasive component or to predict the time frame for cancer transformation in IPMN patients. This results in delayed cancer diagnoses as well as unnecessary operations performed for noninvasive benign tumors. According to the consensus guidelines, patients with small asymptomatic branch type IPMN are not offered surgery due to the low risk of having invasive cancer.26 However, the long-term outcome of these patients is unknown, and some of them may eventually develop invasive cancer. Moreover, a reliable surveillance protocol to diagnose early cancer or imminent transformation within IPMN does not exist. Previous studies have demonstrated that the presence of K-ras mutation in IPMN cyst fluid does not assist in distinguishing benign from malignant IPMN.27 Our data demonstrate that most patients with invasive IPMN have a K-ras mutation, whereas only 15% of patients with benign IPMN patients have this mutation. The p53 and PIK3CA mutations were also more common in invasive IPMN. This may imply that patients that have noninvasive IPMN with K-ras mutation (and perhaps p53 and PIK3CA mutations as well) will develop invasive cancer faster than patients without these mutations. More studies are needed to evaluate whether the presence of specific oncogenic mutations is associated with higher likelihood for future malignant transformation in patients with small, branch duct IPMN treated conservatively according to current guidelines.
Higher rates of K-ras mutations were found in studies that examined multiple sections from the same subject,7,23 possibly pointing to a heterogeneous nature of IPMN cells. Analysis of the invasive cancer cells and the adjacent noninvasive IPMN tissue in our patients with invasive IPMN demonstrated a lack of uniformity of the mutational status of the K-ras, PIK3CA, and p53 genes (Table 2). These results may also be explained by a heterogeneous precursor lesion that contains different clones of neoplastic cells, only some of which continue and develop into malignant cells as they acquire additional mutations. These results are different from those of a previous report by Wada et al.,12 which showed an identical K-ras sequence in the precursor and invasive lesions in most cases of IPMN.
Much attention has been recently given to the significance of the PIK3CA gene mutations identified in several human cancers.13 Mutations usually occur in exons 9 and 20, affecting functionally important domains of this protein.13 While mutations in the PIK3CA gene are not infrequent in several types of cancers, e.g., colon, gastric, breast, brain, ovarian, and lung,13,28–30 no mutations have been described in pancreatic cancer, and a negative finding was reported in at least two studies.13,31 In contrast, Schönleben et al.8 reported that 11% (4/36) of the IPMNs they evaluated had PIK3CA mutations. One of these mutations was a previously described missense hotspot mutation in exon 20 H1047R,13 and the others were novel mutations. They observed that mutations seemed to be a rather late event in the development of IPMN cancer. They found mutations in borderline tumor (n = 1), in situ cancer (n = 1), and invasive cancer (n = 2). The H1047R mutation was found in invasive cancer. This is the first gene that had been found to be mutated in IPMN but not reported in ductal adenocarcinoma. In the present study, two of the 27 specimens contained an H1047R mutation of the PIK3CA gene. This mutation was found in one patient with invasive cancer and another patient with low-grade IPMN (which also had a p53 mutation). This finding is compatible with that of the previous study8 and confirms a 10% mutation rate for the PIK3CA gene in IPMN.
Several studies have demonstrated overexpression of p53 among IPMNs, with an increasing expression level during progression from adenoma to invasive cancer.32–35 Abe et al.34 reported overexpression of p53 on immunohistochemical analysis in 0% of cases in low-grade adenoma and in 23% of cases of carcinoma in situ. This was significantly lower than the overexpression rate in PanIN lesions. Sasaki et al.35 reported nuclear p53 expression in 38% of invasive IPMN tissue, but not in premalignant low-grade or borderline tissues. The profile of specific p53 mutations and their role in the carcinogenesis of IPMN have not been studied. We found p53 mutations in one patient with low-grade IPMN and in two patients with invasive IPMN, one of whom had two concurrent mutations. Both patients with invasive IPMN had the hotspot R248Q mutation, which is the most common p53 mutation reported in human cancer, and the second most common mutation in pancreatic cancer (Universal Mutation Database, www.umd.necker.fr). Interestingly, the same mutation was found in the adjacent nonmalignant IPMN in both of these cases. The R248Q mutation was present while the other (H179R) was not present in the adjacent premalignant tissue in the patient with two p53 mutations. This may point to a dominant role of the specific R248Q mutation in IPMN tumor evolution. Larger studies are needed to explore the possible role of specific p53 mutations on tumor evolution in IPMN, as well as their prognostic significance.
In summary, the MALDI-TOF-based assay is an effective means by which to screen neoplastic tissue for a large number of oncogenic mutations. Of the 22 screened tumor-related genes, only K-ras, p53, and PIK3CA mutations were found in IPMN. Oncogenic mutations, especially in K-ras, are significantly more prevalent in invasive IPMN than in low-grade and borderline IPMN. The variable existence of mutations present in the invasive cancer in the adjacent precursor cells and the presence of a K-ras mutation in the precursor lesion but not in the adjacent malignancy in one patient may point to a heterogeneous nature of this tumor. More studies are needed to determine the role of specific oncogenic mutations as molecular markers for future progression in non-resected tumors and their value as prognostic markers in resected tumors.
References
Ohhashi K, Murakami Y, Maruyama M, et al. Four cases of “mucin producing” cancer of the pancreas on specific findings of the papilla Vater. Prog Dig Endosc 1982;20:348–51.
Kloppel G, Solcia E, Longnecker DS et al. Histological typing of tumors of the exocrine pancreas. In: World Health Organization international classification of tumors, 2nd ed. Berlin: Springer 1996:11–20.
Salvia R, Fernandez-Castillo F, Bassi C, et al. Main-duct intraductal papillary mucinous neoplasm of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg 2004;239:678–87.
Sohn TA, Yeo CJ, Cameron JL, et al. Intraductal papillary mucinous neoplasm of the pancreas: an updated experience. Ann Surg 2004;239:788–799.
D’Angelica M, Brennan M, Suriawinata A, Klimstra D, Conlon KC. Intraductal papillary mucinous neoplasm of the pancreas: an analysis of clinicopathologic features and outcome. Ann Surg 2004;239:400–8.
Lubezky N, Ben-Haim M, Nackache R, Barazovsli E, Santo M, Klausner J. The natural course of intraductal papillary mucinous neoplasm of the pancreas: clinical–pathological correlation. World J Surg 2010 Jan;34(1):126–32.
Z’Graggen K, Rivera JA, Compton CC, et al. Prevalence of activating K-ras mutations in the evolutionary stages of neoplasia in IPMT. Ann Surg 1997;226:491–8.
Schonleben F, Qiu W, Ciau NT, et al. PIK3CA mutations in intraductal papillary mucinous neoplasm/carcinoma of the pancreas. Clin Cancer Res 2006;12:3851–5.
Schönleben F, Qiu W, Bruckman K, et al. BRAF and K-ras gene mutations in intraductal papillary mucinous neoplasm/carcinoma (IPMN/IPMC) of the pancreas. Cancer Lett 2007;249:242–8.
Sessa F, Solcia E, Capella C, et al. IPMT presents a distinct group of pancreatic neoplasms: an investigation of tumour cell differentiation and K-ras, P-53 and c-erbB2 abnormalities in 26 patients. Virchows Arch 1994;425:357–67.
Moriya T, Kimura W, Semba S, et al. Biological similarities and differences between pancreatic intraepithelial neoplasias and IPMN. Int J Gastroinest Cancer 2005;35:111–9.
Wada K, Takada T, Yasuda H, et al. Does “clonal progression” relate to the development of intraductal papillary mucinous tumors of the pancreas? J Gastrointest Surg 2004;8:289–96.
Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science 2004;304:554.
Goelz SE, Hamilton SR, Vogelstein B. Purification of DNA from formaldehyde fixed and paraffin embedded human tissue. Biochem Biophys Res Commun 1985;30:118–26.
Thomas R, Baker A, DeBiasi R, et al. High throughput oncogene mutation profiling in human cancer. Nat Genet 2007;39:347–52.
Koren-Michowitz M, Shimoni A, Vivante A, et al. A new MALDI-TOF based assay for monitoring JAK2 V617F mutation level in patients undergoing allogeneic stem cell transplantation for classic myeloproliferative disorder. Leuk Res 2008;32:421–7.
Vivante A, Amariglio N, Koren-Michowitz M, et al. High throughput, sensitive and quantitative assay for the detection of BCR-ABL kinase domain mutations. Leukemia 2007;21:1318–21.
Almoguera C, Shibata D, Forrester K, Martin H, Arnheim N, Perucho M. Most human carcinomas of the exocrine pancreas contain mutant K-ras genes. Cell 1988;53:549–54.
Smit VT, Boot AJ, Smits AM, Fleuren GJ, Cornelisse CJ, Bos HL. K-ras codon 12 mutations occur very frequently in pancreatic adenocarcinoma. Nucleic Acids Res 1988;16:7773–82.
Grunewald K, Lyons J, Frohlich A, et al. High frequency of Ki-ras codon 12 mutations in pancreatic adenocarcinomas. Int J Cancer 1989;43:1037–41.
Pellegata NS, Sessa F, Renault B, et al. K-ras and p53 gene mutations in pancreatic cancer: ductal and nonductal tumors progress through different genetic lesions. Cancer Res 1994;54:1556–60.
Luttges J, Schilehe B, Menke MA, Vogel I, Henne-Bruns D, Klöppel G. The K-ras mutation pattern in pancreatic ductal adenocarcinoma usually is identical to that in associated normal, hyperplastic, and metaplastic ductal epithelium. Cancer 1999;85:1703–10.
Satoh K, Shimosegawa T, Moriizumi S, et al. K-ras mutation and p53 protein accumulation in intraductal mucin-hypersecreting neoplasms of the pancreas. Pancreas 1996;12:362–8.
Lemoine NR, Jain S, Hughes CH, et al. Ki-ras oncogene activation in preinvasive pancreatic cancer. Gastroenterology 1992;102:230–6.
Satoh K, Sawai T, Shimosegawa T, et al. The point mutation of c-Ki-ras at codon 12 in carcinoma of the pancreatic head region and in intraductal mucin hypersecreting neoplasm of the pancreas. Int J Pancreat 1993;14:135–41.
Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 2006;6:17–32.
Sawhney MS, Devarajan S, O’Farrel P, et al. Comparison of carcinoembryonic antigen and molecular analysis in pancreatic cyst fluid. Gastrointest Endosc 2009;69:1106–10.
Broderick DK, Di C, Parrett TJ, et al. Mutations of PIK3CA in anaplastic oligodendrogliomas, high grade astrocytomas, and medulloblastomas. Cancer Res 2004;64:5048–50.
Li VS, Wong CW, Chan TL, et al. Mutations of PIK3CA in gastric adenocarcinoma. BMC Cancer 2005;5:29.
Wang Y, Helland A, Holm R, Kristensen GB, Borresen-Dale AL. PIK3CA mutations in advanced ovarian carcinomas. Hum Mutat 2005;25:322.
Gallmeier E, Calhoun E, Kern SE. No mutations in PIK3CA identified in pancreatic carcinoma. NOGO 2004;8:2.
Abe K, Suda K, Arakawa A, et al. Different patterns of p16INK4A and p53 protein expressions in intraductal papillary-mucinous neoplasms and pancreatic intraepithelial neoplasia. Pancreas 2007;34:85–91.
Furukawa T, Fujisaki R, Yoshida Y, et al. Distinct progression pathways involving the dysfunction of DUSP6/MKP-3 in pancreatic intraepithelial neoplasia and intraductal papillary-mucinous neoplasms of the pancreas. Mod Pathol 2005;18:1034–42.
Jinfeng M, Kimura W, Sakurai F, et al. Histopathological study of intraductal papillary mucinous tumor of the pancreas: special reference to the roles of Survivin and p53 in tumorigenesis of IPMT. Int J Gastrointest Cancer. 2002;32:73–81.
Sasaki S., Yamamoto H., Kaneto H, et al. Differential roles of alterations of p53’ p16, and SMAD4 expression in the progression of intraductal papillary mucinous tumors of the pancreas. Oncol Rep 2003;10:21–5.
Acknowledgment
This paper was supported by a grant from the Israeli Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table 1
(XLS 62.5 kb)
Supplementary Table 2
(DOC 28.4 kb)
Rights and permissions
About this article
Cite this article
Lubezky, N., Ben-Haim, M., Marmor, S. et al. High-Throughput Mutation Profiling in Intraductal Papillary Mucinous Neoplasm (IPMN). J Gastrointest Surg 15, 503–511 (2011). https://doi.org/10.1007/s11605-010-1411-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-010-1411-8