Abstract
Background
It is commonly thought that colon cancer metastases to the lungs without involvement of the liver are rare.
Methods
We performed a retrospective review of all patients with colorectal cancer diagnosed between December 2003 and August 2007 in Singapore. Isolated lung metastases were determined as (1) Definite if there was confirmed histology or cytology of the lung lesion(s) in the absence of liver lesions on CT scan, and (2) Probable if there were only radiological evidence suggestive of lung metastases rather than lung primary also in the absence of liver lesions on CT scan.
Results
There were 196 patients with rectal and 558 patients with colon cancer (369 left-sided and 189 right-sided). There were 13 definite isolated lung metastases, and the remaining 43 were probable. Twenty-three (12%) patients with rectal cancer and 33 (6%) patients with colon cancer had isolated lung metastases (OR 2.11, 95% CI 1.21–3.70). Patients with ≥pT3 lesions (OR 1.92, 95% CI 0.75–4.93) and ≥pN1 (OR 1.56, 95% CI 0.86– 2.83) were more likely to have isolated lung metastases.
Conclusion
The true incidence of isolated lung without liver metastases in colorectal cancer is likely to lie between 1.7% and 7.2%. While the incidence of isolated lung metastases is twice as common in patients with rectal cancer, it is still significant in patients with colon cancer. The absence of liver involvement should not preclude a search for lung metastases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The incidence of colorectal cancers is rising worldwide. Surgical resection is the primary treatment modality for colorectal cancers, and its outcome is most closely related to the extent of disease at presentation. However, metastases are present in up to 30% of patients with colorectal cancers at the time of presentation.1 The commonest sites of involvement are the regional lymph nodes, liver, lungs, and peritoneum.2 Most deaths from cancer are still due to metastases.2
As the venous drainage of the colon is via the portal system, the first site of hematogenous spread of malignancy has always been regarded as the liver. But metastases bypassing the liver have been mentioned in several reports over the years, including to the lungs and thyroid.3–6
Lung metastases are seen in about 10–15% of all colorectal cancer metastases, but only 10% of these are isolated in the absence of liver metastases.3,4 The higher incidence of this isolated lung metastases in rectal compared to colonic carcinoma was attributed to the direct hematogenous spread into the systemic circulation via the inferior and middle rectal veins, bypassing the portal venous system.3,7
However, colon cancer with isolated metastases not involving the liver is considered very rare with only a few reports mentioning the existence of such an entity.3,4 Our study aims to review the incidence of isolated lung metastases in all patients with colorectal cancers and to identify clinical factors that could be associated with this phenomenon.
Methods
Study Population
Tan Tock Seng Hospital is a single 1,300-bed hospital, the second largest in Singapore and provides secondary and tertiary medical care for about 1.5 million people. A retrospective review of the records of all patients diagnosed with colorectal cancers in our institution between December 2003 and August 2007 was performed. Data for this study was derived from a database of de-identified patient information.
Definition of Isolated Lung Metastases and Colon and Rectal Cancers
All patients with evidence of lung metastases without liver involvement were included in the review. Isolated lung metastases were determined as (1) Definite if there was confirmed histology or cytology of the lung lesion(s) in the absence of liver lesions on CT scan, and (2) Probable if there were only radiological evidence suggestive of lung metastases rather than lung primary also in the absence of liver lesions on CT scan. The findings on the CT scans were agreed upon by two independent radiologists. All scans were performed with intravenous contrast using a Siemens SOMATOM Sensation 64-slice CT scanner (Siemens AG, Wittelsbacherplatz, Muenchen, Germany) for the past 3 years.
Our institution’s routine follow-up protocol for any patient with resected colorectal malignancy includes three monthly follow-up with CEA levels for the first 2 years and six monthly follow-up with CEA levels for the next 3 years with surveillance colonoscopy done 1 year after the surgery. CT scans of the abdomen and pelvis, and definitely thorax, is not routine and is only usually performed if there’s a high index of suspicion or for monitoring of response of metastatic disease undergoing adjuvant therapy. Some of the histological features of the lung lesions that were suggestive of colorectal primary would include the presence of histological immunological markers such as Cytokeratin 20 (CK-20) and Villin, and in the absence of CK-7 and thyroid transcription factor 1 (TTF-1). Synchronous lung metastases were described as lesions arising within 6 months of the diagnosis of the primary, while metachronous metastases were lesions arising after 6 months.
We defined patients with rectal cancer in our study group as those located up to 15 cm from the anal verge excluding the rectosigmoid region. The location of the primary lesion in the colon cancer group commenced from the cecum until the rectosigmoid junction. These patients were also further subdivided into right- and left-sided lesions. Right-sided cancers were regarded if the primary was located from the cecum until the transverse colon, while left-sided cancers was located from the splenic flexure till the rectosigmoid junction.
Exclusion Criteria
Patients were excluded if there were any liver lesions suggestive of metastases within 6 months of diagnosis of the isolated lung metastases, but patients with liver metastases after 6 months from diagnosis of isolated lung metastases were included as it would indicate the progression of the dissemination of the malignancy. Patients were also excluded if the lung lesion(s) did not grow in the absence of adjuvant chemotherapy, indicating a higher probability that they were of infective or scar origins.
Statistical Analysis
For all the colorectal cancer patients reviewed for possible isolated lung metastases, differences in the age, gender, ethnic differences, and site of primary malignancy were tested using Chi square. Other association between the presence of isolated lung metastases and the tumor staging, nodal status of the resected specimens and the location of primary colonic lesions were also tested using Chi square. All results were presented with their Odds ratios (OR) and their 95% confidence interval (CI). All analyses were performed using the SPSS 13.0 statistical package (Chicago, IL, USA).
Results
There were 754 patients diagnosed with colorectal cancers in our institution from December 2003 until August 2007. Their mean age was 67.8 [standard deviation (SD) 12.6] years. A total of 196 (26.0%) patients had rectal cancers, while 558 (74.0%) had colon cancers, with 189 (25.1%) right-sided lesions and 369 (48.9%) left-sided ones. Table 1 illustrates the characteristics of all the 754 patients who had colorectal cancers.
Surgery was performed in 730 (96.8%) patients. The remaining 24 (3.2%) patients declined surgery. Emergency operation was performed in 181 patients (24.0%), and their indications were intestinal obstruction (133, 17.4%), bleeding (25, 3.3%), and perforation (25, 3.3). Details of the histology of the resected specimens are shown in Table 2.
From the resected specimens, majority of the specimen showed an advanced T staging (T3/T4) in 83.6%, and positive nodal involvement (≥N1) in 54.8%, with a median of 17 (1–99) lymph nodes harvested. An overwhelming proportion of the malignancy were of moderate differentiation (n = 679, 92.3%). Distant metastases was already present in 168 (22.3%) patients at presentation, with liver the most common organ involved in 15.0% (n = 113). The median follow-up for all the patients was 21 (6–40) months.
There were a total of 56 patients with isolated lung metastases, 33 (59%) in patients with colon primary, and 23 (41%) in patients with rectal cancers. Of these 56 lung metastases, 13 (23.2%) were definite, (seven in colon cancers, six in rectal cancers) with the remaining 43 (76.8%) probable (26 in colon cancers, 17 in rectal cancers). Thirty (53.6%) patients had synchronous isolated lung metastases while the remaining 26 (46.4%) had metachronous lesions. The median time taken for isolated lung metastases to be diagnosed was 17 (4–36) months after diagnosis of the primary. Carcinoembryonic antigen (CEA levels) was only raised in 18 (32.1%) during follow-up. Table 3 shows the characteristics and details of the group of patients with isolated lung metastases.
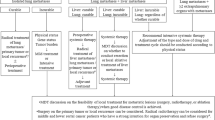
In the 13 patients with definite diagnosis, eight had cytological confirmation, while five had histological evidence, of which four underwent wedge resection of their lung metastases, while one had a core biopsy of the lesion. In these 13 patients, details of the immunohistochemistry were present in seven, for which all were positive for CK-20 and Villin and negative for CK-7 and TTF-1. Of all the patients who underwent chest X-ray preoperatively or during follow-up, only eight (14.3%) patients had features suggestive of lung metastases, and all underwent CT scans of the thorax subsequently. In the group of patients with probable lung metastases, 27 had bilateral lung lesions, while 16 had unilateral nodules. Figure 1 summarised the above findings.
In the 33 patients with colonic primary, 13 had adjuvant chemotherapy, whereas in the 23 patients with rectal primary, four had neoadjuvant chemoradiation therapy, four had adjuvant radiotherapy, while nine have adjuvant chemotherapy.
Patients with rectal cancers were strongly associated with the presence of isolated lung metastases (OR 2.11, 95% CI 1.21–3.70, p = 0.011) compared to colon cancer patients (Table 4). Analysis of the subgroup of patients with colonic primary showed that isolated lung metastases were slightly more commonly seen in left-sided colon cancers compared to right sided ones (OR 1.64, 95% CI 0.73–3.72, p = 0.260; Table 5), though not statistically significant. More advanced T-staging, ≥T3 lesions (OR 2.44, 95% CI 0.57–10.43, p = 0.291) seems to be associated with isolated lung metastases in colon cancers. Whereas in rectal cancers, the presence of nodal disease (OR 3.03, 95% CI 0.97–9.48, p = 0.055) appears to be more strongly associated with isolated lung metastases (Table 6).
Discussion
Reports decades ago showed that pulmonary parenchyma metastases happened in about 10–15% of all colorectal cancers with an approximately 10% of these cases being isolated to the lung.3,4 It has been reported that the lungs could be the only site of metastasis when the primary tumor is in the rectum, with incidence of up to 12%.4,8,9 The high incidence of systemic recurrence in rectal carcinoma was attributed to direct spread into the systemic circulation via the inferior and middle rectal veins.3,7,10
The present series supports this hypothesis as those patients with rectal cancers were shown to have a much higher incidence of isolated pulmonary metastases than those with colon cancers: 12% vs. 6%, respectively. This sizeable percentage rate of isolated lung metastases in rectal cancers has a rather serious implication in its management. CT scans of the thorax should be routinely carried out for patients with rectal cancers for staging and surveillance since around half of these lesions in the present series occurred at diagnosis or within 6 months of presentation. This is especially so as reports have shown favorable long-term results even after repeated surgical resection for lung metastases from colorectal primaries.11,12
However, there has never been any postulation for the rationale associating colon cancer with isolated lung metastases, unlike that of rectal cancer. As the venous drainage of the colon is via the portal system, the first site of hematogenous spread of malignancy has always been regarded as the liver. But metastases bypassing the liver have been mentioned in several reports over the years, involving the lungs and/or thyroid only.3–7 The incidence of isolated lung without liver metastases in colon cancer patients ranged from 1% to 3.8% and was only mentioned in a few reports over the decades3,4 compared to 5.9% in the present series.
The precise mechanism accounting for this phenomenon of skip metastasis bypassing the first draining solid organ or the sentinel node through the hematogenous and lymphatics route is unclear. Various reports cite nonanatomic spread to any draining lymph node or solid organ and nonsequential spread within the lymphatic bed or hematogenous sites as possible explanations. These features could be related to the differences in tumor biology among various patients, tumor types, or even within a given tumor,13–15 supporting the “seed and soil” hypothesis.
The authors feel that the increased presence of isolated lung metastases in patients with advanced T and N disease is not surprising and has been highlighted in other reports,16–19 even though the result was statistically not significant. This tendency may perhaps reflect the increased likelihood of skipped metastases through nonanatomical, nonsequential channels after surgery for locally advanced tumors, for which further studies would be required. But isolated lung metastases also occurred in a significant proportion of patients with T2 and N0 disease. These features reinforced a heightened awareness at all times in detecting metastatic disease during the management of all patients with colorectal malignancy regardless of the stage of their primary cancers.
CEA has not been used as a screening test for detecting primary colorectal malignancy due to its insufficient specificity or sensitivity.20 But its utilization as a tool to detect recurrent disease in patients following curative resection of colorectal cancers has been well documented.21–24 However, in this current series, only half of the patients with isolated lung metastases were found to have elevated CEA levels during follow-up after initial curative surgery. This was not surprising, as CEA levels were shown to be especially useful in the detection of recurrent disease in the liver with sensitivity of up to 80%, while CEA was much less reliable at predicting recurrent disease in other locations.23,25,26
Recent reports have recommended the regime of annual CT scan for the first 3 years after resection for AJCC stage II and III disease.27,28 But neither the role of CT scan nor CEA can be used alone. Evaluation of each patient must include a thorough clinical evaluation, colonoscopy, CEA, and the necessary imaging modalities.29,30
All the above points brought out an important message in the current practice. As we tend to focus only on patients with stage III or high risk stage II disease during the follow-up with the aid of CEA levels, we may have already missed several patients with resectable metastatic disease. In view of the unpredictability of metastatic potential in each colorectal malignancy in every patient, the authors feel that the role of tumor genetic profiling may help to predict the outcome and hopefully prognosticate the disease in the future.
In our series, only four patients (7.1%) with isolated lung metastasis underwent metastasectomy, for which two are still alive currently (>3 years since the lung surgery), while the other two have passed away since. It has been shown in the literature that early diagnosis of colorectal pulmonary metastases is of paramount importance, as several reports have highlighted the survival benefits of pulmonary metastasectomy.31–34 If the metastases could be completely removed, the cumulative 5- and 10-year (total) survival could be as high as 44% and 22%, respectively.
The majority of patients with isolated lung metastasis in our series were not suitable for resection due to several reasons. These included bilateral and multiple lung lesions, control of primary disease, inadequate pulmonary reserve after the planned resection, comorbid conditions, and patients’ decisions. These are similar to the criteria mentioned in the literature of suitability for resection of pulmonary metastases.31–34 After resection, improved survival was shown to be related to various factors such as smaller number and sizes of metastases, lower intrapulmonary tumor load, long disease-free interval, normal serum CEA level, and the absence of concomitant liver metastases and mediastinal lymph node spread. Pulmonary metastasectomy can even be performed effectively in patients with recurrent disease after prior hepatic resection for colorectal metastases, and prolonged survival can still be achieved.
As with most studies, there were several limitations in the present study. This series of patients was enrolled from a single institution, and the data was retrospectively reviewed. The small number of patients with isolated lung metastases may also mask several other important factors that could be accountable. Another significant point was that not all diagnosed lung metastases in this series were diagnosed through confirmed histology or cytology of the lung lesion(s). As such, some of the cases included may have had lung primaries or just post-infective lung scarring. We also do not use PET scan routinely, so some cases classified as isolated lung metastases may actually have other occult metastases as well. The fact that CT scan of the thorax was also not routinely performed for all patients was very significant, as it is possible that other patients with isolated lung metastases may be missed as a consequence, especially since rise in CEA was not present in half of the patients with isolated lung metastases during follow-up. Considering these limitations, the true incidence of isolated lung metastases may range from 3.1% to 11.7% in patients with rectal cancers, and from 1.3% to 5.9% in patients with colon cancers.
Although these limitations are significant, this study remains important in highlighting the presence and extent of isolated lung metastases in colorectal malignancy. It also attempted to identify factors that could aid in the detection of patients with isolated lung metastases earlier and perhaps allow proper interventions to be instituted.
Conclusion
The true incidence of isolated lung without liver metastases in colorectal cancer could lie between 1.7% and 7.2%. While the incidence of isolated lung metastases is twice as common in patients with rectal cancer, it is still significant in patients with colon cancer. Search for lung metastases should be included in the staging and surveillance of all patients with rectal cancer. The absence of liver involvement should not preclude a search for lung metastases.
References
Eisenberg B, Decosse JJ, Harford F, Michalek J. Carcinoma of the colon and rectum: the natural history reviewed in 1704 patients. Cancer 1982;49(6):1131–1134. doi:10.1002/1097-0142(19820315)49:6<1131::AID-CNCR2820490611>3.0.CO;2-T.
Galandiuk S, Wieand HS, Moertel CG, Cha SS, Fitzgibbons RJ Jr, Pemberton JH, Wolff BG. Patterns of recurrence after curative resection of carcinoma of the colon and rectum. Surg Gynecol Obstet 1992;174(1):27–32.
Pihl E, Hughes ES, McDermott FT, Johnson WR, Katrivessis H. Lung recurrence after curative surgery for colorectal cancer. Dis Colon Rectum 1987;30:417–419. doi:10.1007/BF02556487.
McCormack PM, Attiyeh FF. Resected pulmonary metastases from colorectal cancer. Dis Colon Rectum 1979;22:553–556. doi:10.1007/BF02587003.
Hanna WC, Ponsky TA, Trachiotis GD, Knoll SM. Colon cancer metastatic to the lung and the thyroid gland. Arch Surg 2006;141(1):93–96. doi:10.1001/archsurg.141.1.93.
Phillips JS, Lishman S, Jani P. Colonic carcinoma metastasis to the thyroid: a case of skip metastasis. J Laryngol Otol 2005;119(10):834–836. doi:10.1258/002221505774481273.
Scheele J, Altendorf-Hofmann A, Stangl R, Gall FP. Pulmonary resection for metastatic colon and upper rectum cancer. Is it useful? Dis Colon Rectum 1990;33(9):745–752. doi:10.1007/BF02052319.
Goya T, Miyazawa N, Kondo H, Tsuchiya R, Naruke T, Suemasu K. Surgical resection of pulmonary metastases from colorectal cancer. 10-year follow-up. Cancer 1989;64(7):1418–1421. doi:10.1002/1097-0142(19891001)64:7<1418::AID-CNCR2820640709>3.0.CO;2-N.
Wilkins EW Jr, Head JM, Burke JF. Pulmonary resection for metastatic neoplasms in the lung: experience at the Massachusetts Hospital. Am J Surg 1978;135:480–483. doi:10.1016/0002-9610(78)90023-5.
Akasu T, Yamaguchi T, Fujimoto Y, Ishiguro S, Yamamoto S, Fujita S, Moriya Y. Abdominal sacral resection for posterior pelvic recurrence of rectal carcinoma: analyses of prognostic factors and recurrence patterns. Ann Surg Oncol 2007;14(1):74–83. doi:10.1245/s10434-006-9082-0.
Welter S, Jacobs J, Krbek T, Krebs B, Stamatis G. Long-term survival after repeated resection of pulmonary metastases from colorectal cancer. Ann Thorac Surg 2007;84(1):203–210. doi:10.1016/j.athoracsur.2007.03.028.
Ishikawa K, Hashiguchi Y, Mochizuki H, Ozeki Y, Ueno H. Extranodal cancer deposit at the primary tumor site and the number of pulmonary lesions are useful prognostic factors after surgery for colorectal lung metastases. Dis Colon Rectum 2003;46(5):629–636. doi:10.1007/s10350-004-6623-0.
Merrie AE, Phillips LV, Yun K, McCall JL. Skip metastases in colon cancer: assessment by lymph node mapping using molecular detection. Surgery 2001;129(6):684–691. doi:10.1067/msy.2001.113887.
Herrera-Ornelas L, Justiniano J, Castillo N, Petrelli NJ, Stulc JP, Mittelman A et al. Metastases in small lymph nodes from colon cancer. Arch Surg 1987;122:1253–1256.
Tang R, Wang JY, Chen JS et al. Survival impact of lymph node metastasis in TNM stage III carcinoma of the colon and rectum. J Am Coll Surg 1995;180:705–712.
Read TE, Mutch MG, Chang BW, McNevin MS, Fleshman JW, Birnbaum EH, Fry RD, Caushaj PF, Kodner IJ. Locoregional recurrence and survival after curative resection of adenocarcinoma of the colon. J Am Coll Surg 2002;195(1):33–40. doi:10.1016/S1072-7515(02)01224-3.
Radespiel-Tröger M, Hohenberger W, Reingruber B. Improved prediction of recurrence after curative resection of colon carcinoma using tree-based risk stratification. Cancer 2004;100(5):958–967. doi:10.1002/cncr.20065.
Zlobec I, Baker K, Minoo P, Jass JR, Terracciano L, Lugli A. Node-negative colorectal cancer at high risk of distant metastasis identified by combined analysis of lymph node status, vascular invasion, and Raf-1 kinase inhibitor protein expression. Clin Cancer Res 2008;14(1):143–148. doi:10.1158/1078-0432.CCR-07-1380.
Park YJ, Park KJ, Park JG, Lee KU, Choe KJ, Kim JP. Prognostic factors in 2230 Korean colorectal cancer patients: analysis of consecutively operated cases. World J Surg 1999;23(7):721–726. doi:10.1007/PL00012376.
Hine KR, Leonard JC, Booth SN, Dykes PW. Carcinoembryonic antigen concentrations in undiagnosed patients. Lancet 1978;2:1337–1340. doi:10.1016/S0140-6736(78)91975-X.
Devesa JM, Morales V, Enriquez JM et al. Colorectal cancer. The bases for a comprehensive follow-up. Dis Colon Rectum 1988;31:636–652. doi:10.1007/BF02556803.
Beart RW, Metzger PP, O’Connell MJ, Schutt AJ. Postoperative screening of patients with carcinoma of the colon. Dis Colon Rectum 1981;24:585–589. doi:10.1007/BF02605750.
Rocklin MS, Senagore AJ, Talbott TM. Role of carcinoembryonic antigen and liver function tests in the detection of recurrent colorectal carcinoma. Dis Colon Rectum 1991;34:794–797. doi:10.1007/BF02051073.
Barillari P, Bolognese A, Chirletti P, Cardi M, Sammartino P, Stipa V. Role of CEA, TPA, and Ca 19-9 in the early detection of localized and diffuse recurrent rectal cancer. Dis Colon Rectum 1992;35(5):471–476. doi:10.1007/BF02049405.
Hine FR, Dyke PW. Serum CEA testing in the postoperative surveillance of colorectal carcinoma. Br J Cancer 1984;49:689–693.
McCall JL, Black RB, Rich CA, Harvey JR, Baker RA, Watts JM, Toouli J. The value of serum carcinoembryonic antigen in predicting recurrent disease following curative resection of colorectal cancer. Dis Colon Rectum 1994;37(9):875–881. doi:10.1007/BF02052591.
Desch CE, Benson AB 3rd, Somerfield MR, Flynn PJ, Krause C, Loprinzi CL, Minsky BD, Pfister DG, Virgo KS, Petrelli NJ, American Society of Clinical Oncology. Colorectal cancer surveillance: 2005 update of an American Society of Clinical Oncology practice guideline. J Clin Oncol 2005;23(33):8512–8519. doi:10.1200/JCO.2005.04.0063.
Chau I, Allen MJ, Cunningham D, Norman AR, Brown G, Ford HE, Tebbutt N, Tait D, Hill M, Ross PJ, Oates J. The value of routine serum carcino-embryonic antigen measurement and computed tomography in the surveillance of patients after adjuvant chemotherapy for colorectal cancer. J Clin Oncol 2004;22(8):1420–1429. doi:10.1200/JCO.2004.05.041.
Staib L, Schirrmeister H, Reske SN, Beger HG. Is (18)F-fluorodeoxyglucose positron emission tomography in recurrent colorectal cancer a contribution to surgical decision making? Am J Surg 2000;180(1):1–5. doi:10.1016/S0002-9610(00)00406-2.
Sarikaya I, Bloomston M, Povoski SP, Zhang J, Hall NC, Knopp MV, Martin EW Jr. FDG-PET scan in patients with clinically and/or radiologically suspicious colorectal cancer recurrence but normal CEA. World J Surg Oncol 2007;5:64. doi:10.1186/1477-7819-5-64.
Warwick R, Page R. Resection of pulmonary metastases from colorectal carcinoma. Eur J Surg Oncol 2007. 33(Suppl 2):S59–S63. doi:10.1016/j.ejso.2007.09.018.
Zink S, Kayser G, Gabius HJ, Kayser K. Survival, disease-free interval, and associated tumor features in patients with colon/rectal carcinomas and their resected intra-pulmonary metastases. Eur J Cardiothorac Surg 2001;19(6):908–913. doi:10.1016/S1010-7940(01)00724-2.
Joosten J, Bertholet J, Keemers-Gels M, Barendregt W, Ruers T. Pulmonary resection of colorectal metastases in patients with or without a history of hepatic metastases. Eur J Surg Oncol 2008;34(8):895–899. doi:10.1016/j.ejso.2008.01.009.
Labow DM, Buell JE, Yoshida A, Rosen S, Posner MC. Isolated pulmonary recurrence after resection of colorectal hepatic metastases–is resection indicated? Cancer J 2002;8(4):342–347. doi:10.1097/00130404-200207000-00011.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tan, K.K., Lopes Jr., G.d.L. & Sim, R. How Uncommon are Isolated Lung Metastases in Colorectal Cancer? A Review from Database of 754 Patients Over 4 Years. J Gastrointest Surg 13, 642–648 (2009). https://doi.org/10.1007/s11605-008-0757-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0757-7