Abstract
Background
Colorectal cancer is one of the commonest malignancies in the elderly and, as such, is a major cause of morbidity and mortality. There is no consensus yet if age itself is a risk factor for adverse outcome after colectomy. The aims of the study were to evaluate the impact of age on operative results of right colectomy for cancer and to define factors that influence the postoperative mortality in octogenarians.
Methods
Data of all patients who underwent right colectomy for colon cancer between January 2001 and December 2006 were collected retrospectively. Patients were divided into two groups: those who were 80 years and older and those who were less than 80 years old. Analysis included patients’ demographics, comorbidities, American Society of Anesthesiologists class, functional status, mode of presentation, stage of disease, length of hospital stay, postoperative morbidity, and mortality.
Results
A total of 124 consecutive patients with right colon cancer were operated. Control group included 84 patients less than 80 year old. Study group included 40 patients 80 years or older. In Cox multivariate regression analysis, poor functional status and emergent surgery were independent factors for postoperative mortality.
Conclusions
There was no significant difference in the outcome of elective right colectomy between elderly patients and their younger counterparts. Operative mortality of emergency surgery was significantly higher in octogenarians. Emergent setting and poor functional status are major risk factors for postoperative mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Life expectancy in Western world is increasing and as a result, the elderly represent a rapidly growing sector in industrialized countries.1,2
Colorectal cancer (CRC) is one of the commonest malignancies in the elderly and, as such, is a major cause of morbidity and mortality. The proportion of elderly patients undergoing surgery for CRC is rising steadily, as surgical resection remains the primary therapy whenever possible, either for cure or to avoid late complications, such as obstruction or perforation.
Elderly patients are considered to be a different population group compared to younger patients because of higher incidence of comorbidity, poorer functional status, and increased likelihood to present with more advanced disease and as emergency.
Some authors have shown that the effectiveness of treatment of colonic cancer in the elderly is similar to that of younger patients.3–6 Nevertheless, there is no consensus yet if age itself is a risk factor for adverse outcome after colectomy.
In this study, we attempted to decrease the surgical variability by limiting our study population only to patients who had right colectomy as a procedure that anatomically is well defined. The phenomenon of proximal migration in the distribution of colon cancer is consistent with recent literature,7,8 and as a result, right colectomy is one of the most common types of resection. However, there are no studies addressed the outcome of right-side colonic resection in elderly.
The aims of the study were (a) to evaluate clinical manifestations of right-side colon cancer as compared to younger patients, (b) to evaluate the impact of age on operative results of right colectomy for cancer, and (c) to define factors that influence the postoperative mortality in elderly patients.
Patients and Methods
Data of all patients who underwent right colectomy for colon cancer at the Department of Surgery, Kaplan Medical Center between January 2001 and December 2006 were collected retrospectively.
Patients were divided into two groups: a study group of those who were 80 years and older and a control group of patients who were less than 80 years old. Analysis included patients’ demographics, comorbidities, American Society of Anesthesiologists (ASA) class,9 functional status, mode of presentation, stage of disease, length of hospital stay, and postoperative morbidity and mortality.
Right colectomy was defined as any resection extending from the cecum to, but without, the splenic flexure. Resections were designated as emergent in patients who had been admitted with obstructed or perforated right colon cancer and were operated within 24 h of admission. Primary anastomosis was performed in all patients. Postoperative complications were classified as major surgical complications and major general complications, including infectious complications. Major surgical complications were defined as anastomotic leakage or any complication required relaparotomy. Major general complications included cardiovascular complications (myocardial infarction, cardiac rhythm disturbances, heart failure, cerebral infarction, or pulmonary embolism), respiratory failure, or renal failure. Infectious complications included pneumonia and sepsis.
Postoperative mortality was defined as any in-hospital death or death occurring within 30 days after operation. Patients preoperative functional status was assessed using Karnofsky Performance Status Scale10 and defined as poor when Karnofsky score was equal or below 40, i.e., patient who is unable to care for himself; requires equivalent of institutional or hospital care.
Data was analyzed using an “Statistical Package for the Social Sciences” (version 11 for Windows) statistical program. All statistical evaluations were carried out in an explorative sense. The chi-square or Fisher exact tests were used for comparison of categorical variables between the groups. Cox multivariate analysis was used to identify independent factors for postoperative mortality.
Results
A total of 124 consecutive patients with right colon cancer were operated.
Study group included 40 patients who were 80 years or older (median age 83.4, range 80–94). Control group included 84 patients who were less than 80 year old (median age of 68.6, range 39–79).
A comparison of preoperative data of both groups is summarized in Table 1.
The incidence of comorbidities was significantly higher among the elderly patients (80% and 55% respectively, p < 0.01). Nine patients (23%) in the elderly group were classified as ASA score 3–5 as compared to six patients (7%) in the younger patients’ group (p < 0.01). Thirty-two percent of patients in the elderly group had poor functional status as compared to 8% in the younger group (p < 0.05). Emergency surgery was performed in 30% of elderly patients compared to 9.5% in the younger group (p < 0.01). There was no difference between the groups in tumor stage at presentation.
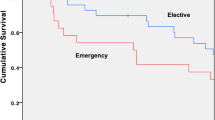
The overall postoperative mortality rate was 10% in the elderly group and 3.5% in the younger cohort (p < 0.01). In the elderly group, all mortality cases were in emergency setting. In the younger cohort, two mortality cases were in emergency setting and one death occurred after elective surgery because of acute myocardial infarction.
Postoperative major complications were recorded in 27.5% in the elderly cohort compared with 17.8% in the younger group (NS), although general complications (pulmonary, cardiovascular, and urinary infection) were more frequent in the elderly (Table 2). There was no anastomotic leak requiring reoperation or demonstrated on CT scan.
The influence of age, tumor stage, ASA grade, comorbidities, emergency operation, and functional status on postoperative mortality were evaluated using multivariate Cox analysis. Emergent setting and poor functional status, but not age by itself, have been identified as independent risk factors for postoperative mortality (Table 3).
Discussion
CRC, the third leading cause of cancer death worldwide, represents 10% of cancer diagnoses and deaths.11 CRC is primarily a disease of the elderly.12 Age is a major risk factor for the development of CRC, with the incidence of carcinomas increasing with advanced age.13
Western population is aging, and as a result, there is a rapidly expanding cohort of octogenarians. Therefore, the medical and societal burdens of CRC will only worsen over the coming decades.
Elderly patients form a highly heterogeneous group. Their general physical status varies, and numerous comorbidities are common. Some studies report age to be an independent predictor of poor outcome in patients with CRC.14,15 As a matter of fact, the relationship of age to outcome after surgery for CRC is complex and multifactorial.
Previous studies have demonstrated an age-related right shift of CRC.7,13,16 Thus, the incidence of right-side colon cancer is increasing with age.
Current studies designated to evaluate outcome of colorectal surgery in aged population include patients undergoing operations for both right and left colon malignancies. Our study is dedicated solely to outcome of right colectomy.
Some studies have found that the older the patient at the time of surgery, the more advanced the tumor stage is likely to be.17 This study has not revealed any significant difference in tumor’s stage between the groups. However, acute presentation because of obstruction or perforation was more frequent in the elderly group, with emergency surgery performed in 30% of elderly patients compared to 9.5% in younger cohort, similar to previous studies reports.18,19 This may be attributed to the shift of cancers to the right in older patients, which might contribute to delay in presentation and diagnosis. This speculation along with the observation from other studies that the elderly apply late for medical help20,21 only emphasizes the importance of screening colonoscopy. Other CRC tests, such as virtual colonoscopy or stool-based molecular testing, have the potential to become important screening tests for elderly in the future.22
Although ASA class is an important predictor of perioperative morbidity and mortality, our study has not found chronologic age or high ASA score to be an independent risk factor of mortality. These data come in line with other studies that found the functional status of the patient to be a better predictor of outcome after surgery for CRC, making ASA scoring alone too imprecise as an instrument for treatment decisions.
Postoperative morbidity rate was higher in the elderly group (27.5% vs. 17.8%), but there was no statistical significance. Although major general complications were observed more frequently among the elderly group, specific surgical postoperative complications did not differ according to age. Primary anastomosis was done in all patients including those in emergent setting. As there was no evidence of anastomotic leak in our study, it appears that the present management of emergency right colectomy with primary anastomosis should continue to be the treatment of choice for obstructing or perforated carcinomas of the right colon. Thus, in surgical treatment of CRC in the elderly, the main problem is not surgery itself, but rather the preoperative and postoperative care which should be optimized to reduce the rate of postoperative complications and mortality. Furthermore, thanks to advances made in surgical technique, anesthetic procedures, and postoperative medical care, modern surgery carries less risk for elderly patient.
Emergency surgery because of obstructed or perforated CRC in the elderly is associated with clearly higher postoperative morbidity and mortality rates than elective surgery.
Overall mortality was 10% in the elderly group, compared to 3.5% in younger patients. All mortality cases in the elderly group were in emergent setting. This finding comes in concordance with results of other studies that emphasize the strong negative influence of emergency surgery on the outcome.23–25 The reason for this is the diminished physical status of the patient, and nonoptimal preoperative preparation of the patient. Therefore, physicians should see the uttermost importance in bringing the elderly patient to elective surgery.
Numerous studies have shown that the age-corrected survival rate of elderly patients is comparable with that of younger ones.26–28 Thus, despite concomitant diseases that elderly patients may have, the cancer-specific survival after surgery seems to be similar to that of younger patients.
We recognize that there are limitations to this study design because of its retrospective nature, which may affect the validity of the conclusions. Our study is single institution, and therefore, the total number of patients is rather small, but we reduced some of the bias by choosing a homogenous group of right-side colon cancer only. Further prospective multi-center studies will provide a stronger validity to these findings.
Conclusions
There was no significant difference in the outcome of elective right colectomy between the elderly patients and their younger counterparts:
-
Operative mortality of emergency surgery was significantly higher in octogenarians.
-
Emergent setting and poor functional status are major risk factors for postoperative mortality.
References
Etzioni D, Liu J, Maggard M, Ko C. The aging population and its impact on the surgery workforce. Ann Surg 2003;238:170–177.
Parker SL, Tong T, Bolden S, Wingo PA. Cancer statistics. CA Cancer J Clin 1997;47:5–27. doi:10.3322/canjclin.47.1.5.
Chiappa A, Zbar AP, Bertani E, Biella F, Audisio RA, Staudacher C. Surgical outcomes for colorectal cancer patients including the elderly. Hepatogastroenterol 2001;48:440–444.
Kashtan H, Werbin N, Wasserman I, Stadler Y, Wiznitzer T. Colorectal cancer in patients over 70 years old. A prospective study of operative results. Isr J Med Sci 1992;28:861–864.
Irvin T. Prognosis of colorectal cancer in the elderly. Br J Surg 1988;75:419–421. doi:10.1002/bjs.1800750508.
Smith J, Lee J, Burke C, Dawson P. Major colorectal cancer resection should not be denied to the elderly. Eur J Surg Oncol 2002;28:661–666. doi:10.1053/ejso.2002.1265.
Obrand DI, Gordon PH. Continued change in the distribution of colorectal carcinoma. Br J Surg 1998;85:246–248. doi:10.1046/j.1365-2168.1998.00507.x.
Cheng X, Chen VW, Steele B, Ruiz B, Fulton J, Liu L, et al. Sub-site specific incidence rate and stage of disease in colorectal cancer by race, gender, and age group in the United States, 1992–1997. Cancer 2001;92:2547–2554. doi:10.1002/1097-0142(20011115)92:10<2547::AID-CNCR1606>3.0.CO;2-K.
Dripps RD, Echenhoff JE, Vandom D. Introduction to anesthesia: the principles of safe practice. Philadelphia: WB Saunders Co, 1988, p 17.
Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: Reliability, validity, and guidelines. J Clin Oncol 1984;2:187–193.
Jemal A, Siegel R, Ward E, Hao A, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin 2008;58:71–96.
Ries L, Wingo PA, Miller DS, Howe HL, Weir HK, Rosenberg HM, et al. The annual report to the nation on the status of cancer 1973–1997 with a special section on colorectal cancer. Cancer. 2000;88:2398–2424. doi:10.1002/(SICI)1097-0142(20000515)88:10<2398::AID-CNCR26>3.0.CO;2-I.
Marusch F, Koch A, Schmidt U, et al. The impact of the risk factor “age” on the early postoperative results of surgery for colorectal carcinoma, and its significance for perioperative management. World J Surg 2005;29:1013–1022. doi:10.1007/s00268-005-7711-6.
Edna TH, Bjerkeset T. Colorectal cancer in patients over 80 years of age. Hepatogastroenterol 1998;45:2142–2145.
Damhuis RA, Wereldsma JC, Wiggers T. The influence of age on resection rates and postoperative mortality in 6457 patients with colorectal cancer. Int J Colorectal Dis 1996;11:45–48.
Zhang B, Fattah A, Nakama H. Characteristics and survival rate of elderly patients with colorectal cancer detected by immunochemical occult blood screening. Hepatogastroenterol 2000;47:414–418.
Payne JE, Chapius PH, Pheilsy MT. Surgery for large bowel cancer in people aged 75 years and older. Dis Colon Rectum 1986;29:733–737. doi:10.1007/BF02555321.
Waldron R, Donovan I, Drumm J, Mottram S, Tedman S. Emergency presentation and mortality from colorectal cancer in the elderly. Br J Surg 1986;73:214–216. doi:10.1002/bjs.1800730320.
Edwards RT, Bransom CJ, Crosby DL, Pathy MS. Cotorectal carcinoma in the elderly: a geriatric and surgical practice compared. Age Ageing 1983;12:256–262. doi:10.1093/ageing/12.3.256.
Kemppainen M, Raiha I, Rajala T, Sourander L. Delay in diagnosis of colorectal cancer in elderly patients. Age Ageing 1993;22:260–264. doi:10.1093/ageing/22.4.260.
Wagner JL, Herdman RC, Wadhwa S. Cost effectiveness of colorectal cancer screening in the elderly. Ann Intern Med 1991;115(10):807–817.
Walsh J, Terdiman J. Colorectal cancer screening. JAMA 2003;289:1288–1296. doi:10.1001/jama.289.10.1288.
Smothers L, Hynan L, Fleming J, Turnage R, Simmang C, Anthony T. Emergency surgery for colon carcinoma. Dis Colon Rectum 2003;46:24–30. doi:10.1007/s10350-004-6492-6.
Biondo S, Marti-Rague J, Kreisler E, Pares D, Martin A, Navarro M, et al. Prospective study of outcomes of emergency and elective surgeries for complicated colonic cancer. Am J Surg 2005;189:377–383. doi:10.1016/j.amjsurg.2005.01.009.
Jestin P, Nilsson J, Heurgren M, Pahlman L, Glimelius B, Gunnarsson U. Emergency surgery for colonic cancer in a defined population. Br J Surg 2005;92:94–100. doi:10.1002/bjs.4780.
Arnaud JP, Schloegel M, Ollier JC, Adloff M. Colorectal cancer in patients over 80 years of age. Dis Colon Rectum 1991;34:896–898. doi:10.1007/BF02049704.
Puig-La Calle J, Quayle J, Thaler HT, Shi W, Paty PB, Quan SH, et al. Favorable short-term and long-term outcome after elective radical rectal cancer resection in patients 75 years of age or older. Dis Colon Rectum 2000;43:1704–1709. doi:10.1007/BF02236854.
Agarwal N, Leighton L, Mandile MA, Cayten CG. Outcomes of surgery for colorectal cancer in patients aged 80 years and older. Am J Gastroenterol 1990;85:1096–1101.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented in part at the Biennial Meeting of the Israel Surgical Association, Jerusalem, Israel, June 6–7, 2007.
Rights and permissions
About this article
Cite this article
Gurevitch, A.J., Davidovitch, B. & Kashtan, H. Outcome of Right Colectomy for Cancer in Octogenarians. J Gastrointest Surg 13, 100–104 (2009). https://doi.org/10.1007/s11605-008-0643-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0643-3