Abstract
Introduction
Despite several meta-analyses and randomized controlled trials showing no benefit to patients, mechanical bowel preparation (MBP) remains the standard of practice for patients undergoing elective colorectal surgery.
Methods
We performed a systematic review of the literature of trials that prospectively compared MBP with no MBP for patients undergoing elective colorectal resection. We searched MEDLINE, LILACS, and SCISEARCH, abstracts of pertinent scientific meetings and reference lists for each article found. Experts in the field were queried as to knowledge of additional reports. Outcomes abstracted were anastomotic leaks and wound infections. Meta-analysis was performed using Peto Odds ratio.
Results
Of 4,601 patients (13 trials), 2,304 received MBP (Group 1) and 2,297 did not (Group 2). Anastomotic leaks occurred in 97(4.2%) patients in Group 1 and in 81(3.5%) patients in Group 2 (Peto OR = 1.214, CI 95%:0.899–1.64, P = 0.206). Wound infections occurred in 227(9.9%) patients in Group 1 and in 201(8.8%) patients in Group 2 (Peto OR = 1.156, CI 95%:0.946–1.413, P = 0.155).
Discussion
This meta-analysis demonstrates that MBP provides no benefit to patients undergoing elective colorectal surgery, thus, supporting elimination of routine MBP in elective colorectal surgery.
Conclusion
In conclusion, MBP is of no benefit to patients undergoing elective colorectal resection and need not be recommended to meet “standard of care.”
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mechanical bowel preparation (MBP) is the standard of practice for patients undergoing elective colorectal surgical resection despite growing evidence that it may not be of benefit to the patient. Several trials have been run to address this issue, including two large multicenter-randomized controlled trials performed in Europe. The aims of this paper are to review the history and advances made surrounding this common practice, review all the published prospective randomized controlled trials, and perform a meta-analysis to evaluate the impact of mechanical bowel preparation on anastomotic leak and wound infection rates.
History of Mechanical Bowel Preparation
When anesthesia and antisepsis permitted surgeons to safely enter the peritoneal cavity, more and more challenging procedures were performed, including operations on the biliary tract, urinary tract, and the gastrointestinal tract. At the beginning of the 20th Century, intestinal resections were fraught with many infectious complications that resulted from contamination of the operating field, lack of antibiotics, and poor or nonexistent postoperative support. Surgeons started prescribing specialized “elemental diets” and laxatives in order to maintain an empty bowel. Fewer complications were noted in patients treated in this fashion, thus, starting the era of mechanical bowel preparation. With advances in pharmacotherapy, the use of antibiotics perioperatively for intestinal surgery became commonplace. The landmark studies regarding the use of antibiotics and MBP compared the use of preoperative oral and intravenous antibiotics combined with MBP to MBP alone. These studies showed a significant decrease in the rate of infectious complications.1 Preoperative prophylactic antibiotics became a mainstay of therapy along with MBP. This combination of oral and intravenous antibiotics with mechanical bowel preparation continues to be the combination most commonly used by surgeons in the United States.2 Currently, the correct and timely administration of antibiotics have become performance measures for quality improvement projects nationwide.3 The role of mechanical bowel preparation in the era of prophylactic antibiotic administration has never been addressed separately and, thus, remains one of the cornerstones of safe colorectal surgery.4
Goals of Mechanical Bowel Preparation
The stated goal of MBP is to completely empty the bowel before surgery in order to decrease the risk of infectious complications. This is conventional wisdom and is theoretically accomplished by decreasing the bacterial load in the intestinal lumen and by decreasing the risk of spillage of feces in the operative field. MBP also purportedly makes manipulation of the bowel easier for the surgeon. However, existing evidence does not support these tenets.
When MBP is performed alone, the bacterial load does not decrease significantly in the lumen or in the bowel wall.5–7 The intervention that affects changes in bacterial flora is the use of antibiotics, not the bowel preparation.8 Mucosal-associated bacteria are still found within the bowel wall with an increasing gradient from the distal rectum to the proximal colon after MBP with polyethylene glycol solution (PEG).9 Thus, the bacteriologic benefit of mechanical bowel preparation is not readily apparent.
The reduction in the risk of fecal spillage in the operative field is also questionable. In a chart review of 333 patients who underwent various colorectal procedures, spillage of bowel contents occurred in 26 (17%) patients who underwent MBP compared to 22 (12%) patients who underwent no MBP (p = 0.21). Interestingly, patients who had spillage during surgery compared to those that did not have higher anastomotic leak rates and wound infection rates, 6.2% versus 3.8% (p = 0.39) and 12.5% versus 6.7% (p = 0.23), respectively.10 These differences did not reach statistical significance, but a trend that favored no MBP was apparent. Sometimes, MBP does not completely empty the bowel, and the remaining liquid effluent is harder to control, thus, potentially increasing the risk of spillage. Poor MBP has already been shown to increase the rate of anastomotic leak compared to patients with adequate MBP.11 Lastly, it is logical to assume that an empty bowel is easier to manipulate than a full one. However, a recent single-blind randomized trial that compared MBP to no MBP in women undergoing laparoscopic gynecologic surgery found no difference in ease of bowel handling or differences in operative field visualization.12
Complications of Mechanical Bowel Preparation
MBP is not an innocuous procedure. There are many choices for preparation of the bowel before elective surgery, which include various preparations of PEG, bisacodyl tablets, aqueous and tablet sodium diphosphate (NaP), and saline laxatives.13 However, the most popular among surgeons in the United States are PEG and NaP.14 Traditional PEG is given to patients as a 4-L solution. Those patients unable to drink the solution are admitted the night prior to surgery and are given the PEG solution per nasogastric tube, thus, adding the discomfort associated with tube placement and the potential risk of aspiration.15 NaP is more convenient for patients, as it is given as a 90-mL solution. Patients have less difficulty drinking the solution, have less gastrointestinal symptoms (pain and bloating), and less fatigue.16,17 However, NaP is associated with more electrolyte disturbances, including changes in sodium, potassium, calcium, and phosphorus. Changes in calcium and phosphorous levels are markedly increased in patients 60 years or older, leading some to suggest that NaP not be provided without a prescription.17 There have also been case reports of near-fatal and fatal complications associated with the use of NaP.18–20
On a survey of 105 patients who underwent elective colorectal resection, 65 underwent MBP and 45 underwent no MBP. The authors found that patients would prefer not to undergo MBP. The time to first bowel movement was shorter in the no MBP group (p = 0.04). However, this group had more discomfort on postoperative day 4.21 They attributed this difference in discomfort (pain was not different) to the decreased time to the first bowel movement.
Effects of Mechanical Bowel Preparation on Intestinal Mucosa
At the histologic level, MBP is associated with certain architectural changes, including loss of superficial mucus and epithelial cells, inflammatory changes, and polymorphonuclear cell infiltration.22 Other changes, such as aphtoid-like lesions, have been reported with NaP.23 The clinical significance of these histologic changes is unknown and requires further investigation but suggests possible changes in bowel wall homeostasis that may impact anastomotic structural integrity.
Initial Experience Without Mechanical Bowel Preparation
Challenges to the use of MBP arose in the 1960s from surgeons who started performing primary repair of injuries to the colon in trauma, with good results in selected cases.24 This, then, led to a flurry of single-institution or single-surgeon series in which MBP was omitted. These authors consistently found rates of wound infections and anastomotic leaks comparable to the literature that used MBP leading to the conclusion that the benefits of MBP might be overstated.25
Initial Randomized Controlled Trials
The first randomized controlled trials comparing MBP to no MBP were performed in Europe and South America in the early 1990s.26–29 Since then, several trials have been performed.30–37 All studies are slightly different in their methodology, with some studies including patients who also underwent procedures in which intestinal continuity was not restored, and others including procedures in both the right and left colon. Anastomotic leak rates for all studies are summarized in Table 1. The difficulty in interpretation and application in practice derives from the variability in methodology in these studies. For example, anastomotic leak rates range from 0.6% to 20.8% in patients who underwent MBP. Wound infection rates for all studies are summarized in Table 2.
Cochrane Review
Given the small number of patients in the aforementioned randomized controlled trials and the variability among these, several meta-analyses have been performed, including a Cochrane Review.38,39 The latest iteration of the Cochrane Review included nine trials with a total of 1,592 patients. Anastomotic leaks were significantly higher in the MBP group (6.2% versus 3.2%, Peto OR 2.03, 95% CI:1.276–3.26, p = 0.003). However, when subgroup analysis was performed for leakage for low anterior resection and leakage for colonic surgery (only four studies could be included), the analysis still favored no MBP, but the statistical significance was lost. The authors found a statistically significant difference favoring no MBP for a decrease in the rate of peritonitis. Elimination of MBP was associated with a statistically significant decreased anastomotic leak rate when sensitivity analyses for studies that were completed and papers published (abstracts excluded), studies that only included adults (children excluded), and in studies that only included creation of an anastomosis. No MBP was also favored in all other analyses (decreased mortality, decreased rate of reoperation, decreased rate of wound infection, decreased noninfectious extra-abdominal complications, and decreased rate of surgical site infections), but these differences did not reach statistical significance. These analyses are limited by the small number of studies that could be included. The authors concluded that MBP before colorectal surgery does not add any value for patients and that it might lead to an increase in anastomotic leak rate.39
Results of Latest Randomized Controlled Trials
In light of the Cochrane Review findings, two large multicenter-randomized controlled trials were performed and the results published in the past year; one was performed in Sweden and another in the Netherlands.40,41 The Swedish trial randomized 686 patients to MBP and 657 to no MBP.40 Patients in the MBP arm were prepped with PEG (47.2%), NaP (48.5%), or enemas (4.3%). Antibiotic prophylaxis was appropriate for colorectal surgery and similar in both arms. The indications for surgery, patient demographics, type of anastomosis (site and technique) were similar for both groups. The results showed no statistically significant difference in cardiovascular complication rates, general infectious rates, or surgical site infection rates. Anastomotic dehiscence occurred in 13 (2.3%) patients in the MBP arm and in 17 (2.6%) patients in the no MBP arm (p = 0.46). No mid- to low-anterior resections were performed in either group.
The study from the Netherlands randomly assigned 670 patients to mechanical bowel preparation and 684 to no mechanical bowel preparation for elective bowel resection.41 The authors found that those patients that did not undergo MBP had an anastomotic leak rate of 5.4% compared to 4.8% in those that did undergo MBP, but the difference was not statistically significant (p = 0.69). However, in the group of patients who did not undergo MBP, there was a statistically significant increased risk for anastomotic leak associated with a pelvic abscess (p = 0.001). The authors did not explicitly state the complications for each type of anastomosis for each group. However, multivariate analysis did show that type of anastomosis (ileocolic, colocolic, and colorectal), ASA classification, and intraoperative blood-loss correlated with an increase in anastomotic leaks in general.
Meta-analysis
Methods
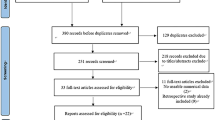
We performed a systematic review of the literature of all trials that prospectively compared mechanical bowel preparation with no mechanical bowel preparation for patients undergoing elective colorectal surgical resection. We performed a search in MEDLINE using the following search terms: (1) “Surgical Procedures, Elective” [Mesh] AND “Colorectal Surgery” [Mesh] AND mechanical bowel preparation; (2) mechanical bowel preparation AND elective AND surgery; (3) mechanical bowel preparation AND surgery AND colon AND rectum. We also performed a search in LILACS and SCISEARCH using the following terms: mechanical bowel preparation AND elective surgery. This was followed by a manual search of the reference lists for each article found, as well as abstracts of pertinent scientific meetings. Experts in the field were queried as to knowledge of additional reported trials. There were no limits on dates or language and all searches were performed up to January 2008. Studies had to be prospective, have two groups (one with mechanical bowel preparation and one without mechanical bowel preparation), and have the two outcomes of interest clearly stated in their results section. The outcomes we abstracted were anastomotic leaks and wound infections. Retrospective studies and studies that only evaluated either mechanical bowel preparation or no mechanical bowel preparation were excluded from meta-analysis. Meta-analysis was performed using Comprehensive Meta-Analysis version 2 (Englewood, NJ, 2005, USA) applying the Peto-Odds ratio (fixed effects model). We also ran a test of statistical heterogeneity for each category.
Results
Of a total of 4,601 patients (13 trials), 2,304 were allocated to mechanical bowel preparation (Group 1) and 2,297 were allocated to no mechanical bowel preparation (Group 2). Anastomotic leaks (Table 1) occurred in 97 (4.2%) patients in Group 1 and in 81 (3.5%) patients in Group 2 (Peto OR = 1.214, CI 95%:0.899–1.64, P = 0.206). Wound infections (Table 2) occurred in 227 (9.9%) patients in Group 1, and in 201 (8.8%) patients in Group 2 (Peto OR = 1.156, CI 95%:0.946–1.413, P = 0.155). Forest plots for anastomotic leaks and wound infections are shown in Figs. 1 and 2, respectively.
Discussion
Initial challenges to mandatory MBP first arose in the 1960s surrounding primary colon repairs in traumatic injuries to the colon. This led to single-institution and single-surgeon series where MBP was eliminated and ultimately to prospective randomized controlled trials comparing MBP to no MBP. A Cochrane review in 2005 suggested that MBP does not add value, but the number of patients evaluable were still small. Two more large trials have been performed since the Cochrane analysis, and now a total of 4,601 patients have been studied in a prospective fashion. Our meta-analysis suggests that MBP is of no benefit to patients undergoing elective colon and rectal surgery.
Based on the earlier small trials and Cochrane review many surgeons have abandoned routine MBP for elective “right-sided” surgeries, where the proximal extent of the resection will involve the small bowel and, therefore, theoretically be associated with a decreased risk for anastomotic and wound complications. More recently, some have questioned the need for MBP where a colocolonic or colorectal anastomosis is anticipated. Because of continued concerns for the role of MBP in rectal surgery and the exclusion of this population from most of the prospective trials, a retrospective review was performed on 144 patients who underwent anterior resection for cancer without MBP or a diverting stoma demonstrated an excellent anastomotic leak rate of only 4.9%.42 In a French case-control study of an unselected group of patients with rectal cancer, the authors found an increased morbidity associated with MBP and no difference in the anastomotic leak rates.43
However, even with the growing body of evidence that suggests that mechanical bowel preparation should be abandoned, many groups have yet to change their practice. One of the main reasons is that even with several randomized controlled trials and meta-analyses, many practitioners feel that the right question has not been asked and, thus, the right trial has not been run. The ideal trial would recruit the number of patients necessary to show a difference in outcome. Power calculations by our statistics department resulted in over 2,400 patients, thus, requiring collaboration among many institutions. Because the rate of anastomotic leak is low in ileocolic anastomoses, these should be excluded from the study, allowing a focus on colocolonic and colorectal anastomoses. The study should compare the same type of anastomosis, report the height of anastomosis, and use a similar operative technique. More importantly, the endpoints (anastomotic leaks and wound infections) must be unambiguously defined. These requirements become difficult as it is hard to minimize variability in studies that require participation of various surgeons and centers. Other possible reasons why a change in practice has not taken place include the influence of training programs on practice patterns, the inability to work “comfortably” with a bowel filled with feces, and the persistent yet unrealized fear of increased risk of fecal spillage during surgery when MBP is eliminated.
In modern surgical practice, the use of prophylactic antibiotics and the rate of surgical site wound infections have become, for better or worse, performance measures used to rank, reward, and penalize institutions and physicians as part of national and institutional quality improvement projects.3 Since MBP may or may not increase the rate of infectious complications, it will become imperative to define its place in clinical practice in order to justify its continued use. MBP should not be completely abandoned, as it is necessary for those procedures in which intraoperative colonoscopy is necessary. Even though the ideal study has not yet been performed, this meta-analysis does point to the fact that MBP is not a prerequisite of safe colorectal surgery, as suggested by others. Some of our European counterparts have embraced these findings and changed their practice patterns, yet we remain static, either as cautious observers or as laggards.
As individual-practicing surgeons, one can argue to remain cautious. In fact, the individual-practicing surgeon relies on national societies to provide guidelines that are based on best available evidence.44 This is also true for medicolegal proceedings, where practice guidelines serve as key elements that establish the standard of care.45 As thought leaders, however, we should have the courage to expose unsubstantiated dogmas and encourage discontinuation of unfounded practices. Thus, our meta-analysis represents an opportunity for respected national societies, like the Society for Surgery of the Alimentary Tract, to lead by publicly endorsing the abandonment of routine MBP in elective colon and rectal surgery.
Conclusion
MBP has remained a dogmatic practice in surgery of the alimentary tract. This updated meta-analysis demonstrates that MBP is of no benefit to patients undergoing elective colon and rectal surgery, thus, supporting elimination of routine MBP. It should not be considered as a prerequisite to meet the “standard of care.”
References
Nichols RL, Broido P, Condon RE, Gorbach SL, Nyhus LM. Effect of preoperative neomycin-erythromycin intestinal preparation on the incidence of infectious complications following colon surgery. Am Surg 1973;178:453–62. doi:10.1097/00000658-197310000-00008.
Zmora O, Wexner SD, Hajjar L, Park T, Efron JE, Noqueras JJ, Weiss EG. Trends in preparation for colorectal surgery: survey of the members of the American Society of Colon and Rectal Surgeons. Am Surg 2003;69:150–4.
McCahill LE, Ahern JW, Gruppi LA, Limanek J, Dion GA, Sussman JA, McCaffrey CB, Leary DB, Lesaqe MB, Single RM. Enhancing compliance with Medicare guidelines for surgical infection prevention: experience with a cross-disciplinary quality improvement team. Arch Surg 2007;142:355–61. doi:10.1001/archsurg.142.4.355.
Nichols RL, Choe EU, Weldon CB. Mechanical and antibacterial bowel preparation in colon and rectal surgery. Chemotherapy 2005;51(Suppl 1):115–21. doi:10.1159/000081998.
Nichols RL, Gorbach SL, Condon RE. Alteration of intestinal microflora following preoperative mechanical preparation of the colon. Dis Colon Rectum 1971;14:123–7. doi:10.1007/BF02560057.
Lindsey JT, Smith JW, McClugage SG Jr, Nichols RL. Effects of commonly used bowel preparations on the large bowel mucosal-associated and luminal microflora in the rat model. Dis Colon Rectum 1990;33:554–60. doi:10.1007/BF02052206.
Smith MB, Baliga P, Sartor WM, Goradia VK, Holmes JW, Nichols RL. Intraoperative colonic lavage: failure to decrease mucosal microflora. South Med J 1991;84:38–42. doi:10.1097/00007611-199104000-00017.
Bornside GH, Cohn I Jr. Intestinal antisepsis. Stability of fecal flora during mechanical cleansing. Gastroenterology 1969;57:569–573.
Bleday R, Braidt J, Ruoff K, Shellito PC, Ackroyd FW. Quantitative cultures of the mucosal-associated bacteria in the mechanically prepared colon and rectum. Dis Colon Rectum 1993;36:844–9. doi:10.1007/BF02047381.
Mahajna A, Krausz M, Rosin D, Shabtai M, Hershko D, Ayalon A, Zmora O. Bowel preparation is associated with spillage of bowel contents in colorectal surgery. Dis Colon Rectum 2005;48:1626–31. doi:10.1007/s10350-005-0073-1.
Irvin TT, Goligher JC. Aetiology of disruption of intestinal anastomoses. Br J Surg 1973;60:461–4. doi:10.1002/bjs.1800600612.
Muzii L, Bellati F, Zullo MA, Manci N, Angioli R, Panici PB. Mechanical bowel preparation before gynecologic laparoscopy: a randomized, single-blind, controlled trial. Fertil Steril 2006;85:689–93. doi:10.1016/j.fertnstert.2005.08.049.
Wexner SD, Beck DE, Baron TH, Fanelli RD, Hyman N, Shen B, Wasco KE. A consensus document on bowel preparation before colonoscopy: prepared by a task force from the American Society of Colon and Rectal Surgeons (ASCRS), the American Society for Gastrointestinal Endoscopy (ASGE), and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES). Surg Endosc 2006;20:1147–60. doi:10.1007/s00464-006-0152-y.
Nichols RL, Smith JW, Garcia RY, Waterman RS, Holmes JW. Current practices of preoperative bowel preparation among North American colorectal surgeons. Clin Infect Dis 1997;24:609–19.
de Graaf P, Slagt C, de Graaf JL, Loffeld RJ. Fatal aspiration of polyethylene glycol solution. Neth J Med 2006;64:196–8.
Oliveira L, Wexner SD, Daniel N, DeMarta D, Weiss EG, Noqueras JJ, Bernstein M. Mechanical bowel preparation for elective colorectal surgery. A prospective, randomized, surgeon-blinded trial comparing sodium phosphate and polyethylene glycol-based oral lavage solutions. Dis Colon Rectum 1997;40:585–91. doi:10.1007/BF02055384.
Mathus-Vliegen EM, Kemble UM. A prospective randomized blinded comparison of sodium phosphate and polyethylene glycol-electrolyte solution for safe bowel cleansing. Aliment Pharmacol Ther 2006;23:543–52. doi:10.1111/j.1365-2036.2006.02777.x.
Gonlusen G, Akgun H, Ertan A, Olivero J, Truong LD. Renal failure and nephrocalcinosis associated with oral sodium phosphate bowel cleansing: clinical patterns and renal biopsy findings. Arch Pathol Lab Med 2006;130:101–6.
Ullah N, Yeh R, Ehrinpreis M. Fatal hyperphosphatemia from a phosphosoda bowel preparation. J Clin Gastroenterol 2002;34:457–8. doi:10.1097/00004836-200204000-00017.
Aydogan T, Kanbay M, Uz B, Kaya A, Isik A, Bozalan R, Erkman M, Akcay A. Fatal hyperphosphatemia secondary to a phosphosoda bowel preparation in a geriatric patient with normal renal function. J Clin Gastroenterol 2006;40:177. doi:10.1097/01.mcg.0000196408.60851.cf.
Jung B, Lannerstad O, Pahlman L, Arodell M, Unosson M, Nilsson E. Preoperative mechanical preparation of the colon: the patient’s experience. BMC Surg 2007;7:5. doi:10.1186/1471-2482-7-5.
Bucher P, Gervaz P, Egger JF, Soravia C, Morel P. Morphologic alterations associated with mechanical bowel preparation before elective colorectal surgery: a randomized trial. Dis Colon Rectum 2006;49:109–12. doi:10.1007/s10350-005-0215-5.
Zwas FR, Cirillo NW, El-Serag HB, Eisen RN. Colonic mucosal abnormalities associated with oral sodium phosphate solution. Gastrointest Endosc 1996;43:463–6.
LoCicero J 3rd, Tajima T, Drapanas T. A half-century of experience in the management of colon injuries: changing concepts. J Trauma 1975;15:575–9. doi:10.1097/00005373-197507000-00003.
Duthie GS, Foster ME, Price-Thomas JM, Leaper DJ. Bowel preparation or not for elective colorectal surgery. J R Coll Surg Edinb 1990;35:169–71.
Brownson P, Jenkins SA, Nott D, Ellenbogen S. Mechanical bowel preparation before colorectal surgery: results of a prospective randomized trial. Br J Surg 1992;79:461–2.
Burke P, Mealy K, Gillen P, Joyce W, Traynor O, Hyland J. Requirement for bowel preparation in colorectal surgery. Br J Surg 1994;81:907–10. doi:10.1002/bjs.1800810639.
Santos JC Jr, Batista J, Sirimarco MT, Guimaraes AS, Levy CE. Prospective randomized trial of mechanical bowel preparation in patients undergoing elective colorectal surgery. Br J Surg 1994;81:1673–6. doi:10.1002/bjs.1800811139.
Fillmann EEP, Fillmann HS, Fillmann LS. Elective colorectal surgery without prepare [Cirugia colorretal eletiva sem preparo]. Rev Bras Colo-Proct 1995;15:70–1.
Miettinen RP, Laitinen ST, Makela JT, Paakkonen ME. Bowel preparation with oral polyethylene glycol electrolyte solution vs. no preparation in elective open colorectal surgery: prospective, randomized study. Dis Colon Rectum 2000;43:669–75. discussion 75–77. doi:10.1007/BF02235585.
Tabusso FY, Zapata JC, Espinoza FB, Meza EP, Figueroa ER. Mechanical preparation in elective colorectal surgery, a useful practice or need. Rev Gastroenterol Peru 2002;22:152–8. Preparación mecánica en cirugía electiva colo-rectal ¿Costumbre o necesidad?
Zmora O, Mahajna A, Bar-Zakai B, Rosin D, Hershko D, Shabtai M, Krausz MM, Ayalon A. Colon and rectal surgery without mechanical bowel preparation: a randomized prospective trial. Ann Surg 2003;237:363–7. doi:10.1097/00000658-200303000-00010.
Bucher P, Gervaz P, Soravia C, Mermillod B, Erne M, Morel P. Randomized clinical trial of mechanical bowel preparation versus no preparation before elective left-sided colorectal surgery. Br J Surg 2005;92:409–14. doi:10.1002/bjs.4900.
Fa-Si-Oen P, Roumen R, Buitenweg J, van de Velde C, van Geldere D, Putter H, Verwaest C, Verhoef L, de Waard JW, Swank D, D’Hoore A, Croiset van Uchelen F. Mechanical bowel preparation or not? Outcome of a multicenter, randomized trial in elective open colon surgery. Dis Colon Rectum 2005;48:1509–16. doi:10.1007/s10350-005-0068-y.
Ram E, Sherman Y, Weil R, Vishne T, Kravarusic D, Dreznik Z. Is mechanical bowel preparation mandatory for elective colon surgery? A prospective randomized study. Arch Surg 2005;140:285–8. doi:10.1001/archsurg.140.3.285.
Zmora O, Mahajna A, Bar-Zakai B, Hershko D, Shabtai M, Krausz MM, Ayalon A. Is mechanical bowel preparation mandatory for left-sided colonic anastomosis? Results of a prospective randomized trial. Tech Coloproctol 2006;10:131–5. doi:10.1007/s10151-006-0266-1.
Pena-Soria MJ, Mayol JM, Anula-Fernandez R, Arbeo-Escolar A, Fernandez-Represa JA. Mechanical bowel preparation for elective colorectal surgery with primary intraperitoneal anastomosis by a single surgeon: interim analysis of a prospective single-blinded randomized trial. J Gastrointest Surg 2007;11:562–7. doi:10.1007/s11605-007-0139-6.
Bucher P, Mermillod B, Gervaz P, Morel P. Mechanical bowel preparation for elective colorectal surgery: a meta-analysis. Arch Surg 2004;139:1359–64. discussion 65. doi:10.1001/archsurg.139.12.1359.
Guenaga KF, Matos D, Castro AA, Atallah AN, Wille-Jorgensen P. Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev 2005, CD001544.
Jung B, Pahlman L, Nystrom PO, Nilsson E. Multicentre randomized clinical trial of mechanical bowel preparation in elective colonic resection. Br J Surg 2007;94:689–95. doi:10.1002/bjs.5816.
Contant CM, Hop WC, van’t Sant HP, Oostvoqel HJ, Smeets HJ, Stassen LP, Neijenhuis PA, Idenburg FJ, Dijkhuis CM, Heres P, van Tets WF, Gerritsen JJ, Weidema FF. Mechanical bowel preparation for elective colorectal surgery: a multicentre randomised trial. Lancet 2007;370:2112–7. doi:10.1016/S0140-6736(07)61905-9.
Vlot EA, Zeebregts CJ, Gerritsen JJ, Mulder HJ, Mastboom WJ, Klaase JM. Anterior resection of rectal cancer without bowel preparation and diverting stoma. Surg Today 2005;35:629–33. doi:10.1007/s00595-005-2999-2.
Bretagnol F, Alves A, Ricci A, Valleur P, Panis Y. Rectal cancer surgery without mechanical bowel preparation. Br J Surg 2007;94:1266–71. doi:10.1002/bjs.5524.
Eagle KA, Garson AJ Jr, Beller GA, Sennett C. Closing the gap between science and practice: the need for professional leadership. Health Aff (Millwood) 2003;22:196–201. doi:10.1377/hlthaff.22.2.196.
Feld AD. Medicolegal implications of colon cancer screening. Gastrointest Endosc Clin N Am 2002;12:171–9. doi:10.1016/S1052-5157(03)00065-5.
Author information
Authors and Affiliations
Corresponding author
Additional information
Grant support and other assistance: none received.
Rights and permissions
About this article
Cite this article
Pineda, C.E., Shelton, A.A., Hernandez-Boussard, T. et al. Mechanical Bowel Preparation in Intestinal Surgery: A Meta-Analysis and Review of the Literature. J Gastrointest Surg 12, 2037–2044 (2008). https://doi.org/10.1007/s11605-008-0594-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0594-8