Abstract
Background
Recently, it has been demonstrated that surgical treatment of hemorrhoids in a day-care basis is possible and safe. The aim of this study was to compare the Longo stapled hemorrhoidopexy (SH) and the Milligan–Morgan hemorrhoidectomy (MMH).
Methods
One hundred seventy one patients (95 cases in SH group and 76 cases in MMH group) entered the study: 83 cases were III degree hemorrhoids, 88 IV degree. A priori and a post hoc power analysis were performed. Results, prospectively collected, were compared using chi squared test and student t test. Visual analog scale was used for pain evaluation. Postoperative pain, duration of pain, wound secretion, bleeding, resumption of a normal lifestyle, and postoperative complication were evaluated.
Results
Surgical time was 28.41 ± 10.78 for MMH and 28.30 ± 13.28 min in SH (P = 0.94). Postoperative pain was not different between MMH and SH during the first two postoperative days (4.73 ± 2.91 vs 5.1 ± 3.048; P = 0.4), during the following 6 days, patients treated with SH had less pain (4.63 ± 2.04 in MMH vs 3.60 ± 2.35 in SH; P = 0.006). In the SH group, seven patients needed further hospital stay for complicated course. SH showed higher incidence of anal fissure compared with MMH (6.3% vs 0%; P = 0.025) but no differences in urinary retention, anal stricture, urgency, or anal hemorrhage.
Conclusions
This study confirms that SH is associated with less postoperative pain and shorter postoperative symptoms, compared with MMH. SH may be a viable addition to the therapy for hemorrhoids with some advantages in early postoperative pain and some disadvantages in postoperative complications and costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemorrhoids are one of the most common anorectal disorders. The Milligan–Morgan open hemorrhoidectomy (MMH) is the most common surgical technique used for the treatment of hemorrhoids. Circular stapled hemorrhoidopexy (SH) was described by Longo in 1998 as an alternative surgical technique for grade III and IV hemorrhoids. Early small studies comparing SH with standard hemorrhoidectomy have shown that SH is less painful and associated with quicker recovery.1–4 Driven by this early success, SH has achieved rapid popularity as an alternative to excisional surgery in many centers. Later on, several authors reported severe complications, such as pelvic sepsis, rectal obstruction, rectal perforation, and stapled line dehiscence following SH.5–7 Doubts about the adequacy of SH in managing concomitant external hemorrhoids were raised together with the fact that this technique carries a postoperative bleeding rate higher than that of excisional hemorrhoidectomy and has an early reoperation rate of more then 5%.5 A severe postdefecation pain syndrome and fecal urgency have also been reported.6 Moreover, in the past 2 years, a few randomized clinical trials comparing SH with Milligan–Morgan have been published with a higher number of cases and a longer follow-up.8–10 Conclusions from these studies are that SH may be at least as safe as the Milligan–Morgan technique. SH in most studies causes significantly less postoperative pain and earlier resumption of normal activities than MMH. Despite this evidence in support of SH, controversy still exists due to rare but occasionally life-threatening complications, and also due to significant chronic pain experienced by a small subset of patients. More recently, a large meta-analysis study on the safety and efficacy of SH compared to MMH in the treatment of hemorrhoids has concluded that SH may be at least as safe as MMH. However, the efficacy of SH compared with MMH could not be determined absolutely, and the conclusion was that further, more rigorous studies with longer follow-up periods and larger sample sizes need to be conducted.11 In the past few years, some studies have demonstrated that surgical treatment of hemorrhoids on a day-care basis is possible and safe. The aim of this study was to compare two surgical techniques, the SH and the MMH, in day surgery.
Materials and Methods
Between January 2002 and June 2006, 200 consecutive patients were enrolled in this study to be treated on a day-care basis in our University Hospital. Two groups were created: a SH group (100 patients) operated on using the PPH-01 kit (Ethicon Endo-Surgery) with the technique described by Longo,12 and a MMH group (100 patients) operated on using a standard open hemorrhoidectomy technique.13 Patients were enrolled in the study after an office visit and a rigid proctoscopy. All patients over 40 years old underwent colonoscopy. After the patients had given their written consent, they were informed of the result of the randomization. Seven patients rejected the result of the randomization and six others refused surgery thereafter. Inclusion criteria were third- and fourth-degree symptomatic hemorrhoids that could be treated by either surgical technique. A further criterion was that the patients had to be classified ASA I or ASA II to fulfill the day-care anesthesiology standard. Exclusion criteria were acute thrombosis, concomitant anal fissure, previous surgical treatment of hemorrhoids, Crohn’s disease, and ASA classification over II. All patients were operated on in the lithotomy position under local anesthesia by local injection of 20 ml of naropine 0.75% in the anal verge and submucosa of the anal canal, 1 mg of i.v. Midazolam was administered in all patients, and general anesthesia was provided when required. All patients were operated on by two certified colorectal surgeons with a previous experience of over 100 SH procedures and hundreds of MMH procedures. The protocol was approved by an ethics committee. In the comparison of the two groups, we considered the following parameters: postoperative pain, relevant pain duration (in days), duration of wound secretion, bleeding duration, and resumption of a normal lifestyle. Postoperative pain was assessed using a visual analog scale (VAS) in which zero corresponds to no pain and ten to maximum experienced pain. The VAS score was recorded by the patient daily for 8 days starting the day of surgery. The analgesic regimen included Ketorolac 30 mg 1 h after surgery and at the moment of discharge from the day care. At home, the patients were given oral Ketorolac 20 mg up to three times a day. All patients were given daily postoperative laxative (lactulose 30 ml q.d.) for 1 week. Antibiotic prophylaxis was administered using Ciprofloxacine 400 mg i.v. intraoperatively and 250 mg p.o. bid for 3 days. Starting January 2003, antibiotic profilaxis was revised using intravenous cephalosporin (1 g) and Metronidazole (500 mg). A high-fiber diet was recommended together with adequate oral fluid intake. Patients were encouraged to take sit baths two or thee times a day. Patient follow up was 8 days after surgery, 1 month, 3 months, and then every 6 months. Mean follow up was 34.8 ± 15.6 months. Patients were asked at follow up to fill out a questionnaire about symptoms, continence, defecation, and quality of life. Patients were also asked to express a score on the quality of care and assistance received. Randomization was stratified at the moment of the first diagnosis. Two different groups were compared with the following assumptions: independent samples from normal population having equal variances. Then, we compared the results with a chi-squared test for qualitative variables and a parametric T test to compare means for quantitative variables. Statistical test was carried out, choosing a bilateral test and a first type α-error risk of 0.05 (α = 5%). A priori power analysis was performed as a component of the design experiment to estimate required total sample size as a function of power 1-β (at least 0.80) with medium effect size (μ1 − μ2/σ = 0.5),14 and α = 0.05 (Fig. 1). We also considered a post hoc power analysis to decide how likely it would be that our statistical test would detect the specified effect with the observed samples. Power analysis was carried out both for the two independents means under investigation and for the difference between two independents proportions (Table 1). With regard to the chi square test between two independent proportions, power analysis performed a priori required a sample size of 82 patients (pts) equal for the two groups to detect a difference of 0.2 in the proportion of the two population with a power of 0.80 (α = 0.05). Although one of the two samples was slightly less (MMH = 76 pts) the achieved power was 0.81. Some of the results are expressed as a mean ± standard deviation (sd). The software used was SPSS version 11.0 for Windows. The power calculation was computed using G*Power 3.15
Results
A total of 200 patients, 109 males and 91 females, all affected by III- and IV-degree hemorrhoids, were included and randomized for SH (100 patients) and MMH (100 patients) in the study, and there were no significant differences with respect to mean age, weight, history, or risk factors. Thirteen patients refused randomization or did not undergo surgery and 16 were lost at follow up; therefore, 171 patients were considered in the results of the study, 102 male and 69 female. Among these patients, 95 underwent SH and 76 MMH. Eighty three patients had III-degree hemorrhoids, while 88 had IV-degree hemorrhoids.
Clinical data were comparable in both groups; the most common problems reported from the patients before the operation were the impression of a mass at the anus (85%), rectal bleeding (77%), pain (65%), itching (32%), and discharge and soiling (20%). The same anesthesia protocol was used in all patients, and no intraoperative complications were observed. Surgical time was not significantly different: 28.41 ± 10.78 min for MMH and 28.30 ± 13.28 min for SH (P = 0.94). In the Longo prolassectomy group, 88 patients (92.6%) were managed in a day-care setting, 4 (4.2%) were in 1-day surgery (they were discharged the day after) and three required further admission for complicated course (3.2%). All of the 76 patients operated on with MMH were treated in day care. The necessity of prolonged hospital stay was significantly higher in SH than MMH (P = 0.014): in the SH group, four patients required observation overnight for pain or urinary retention and three patients required admission for 2 to 4 days for postoperative complication, vs none of the patients treated by MMH. The mean follow up period was 34.8 ± 15.6 months; a total of 16 patients (12 MMH and 4 SH) failed to come back for follow up.
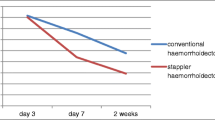
There were no significant differences between MMH and SH related to postoperative pain in the first 2 days (5.13 ± 2.98 vs 5.10 ± 3.04; P = 0.959), but during the following 6 days, patients treated with Longo technique had significantly less pain (4.71 ± 21.94 vs 3.60 ± 2.35; P = 0.002) (Fig. 2, Table 2). The statistical evaluation among the whole period considered (8 days) was significantly less in SH compared to MMH (P = 0.016). The duration of postoperative pain, (in days) secretion, and bleeding are significantly less in the Longo group then in the Milligan–Morgan group, as is shown in Table 2.
Among postoperative complications, SH showed a significantly higher incidence of anal fissure compared with MMH (6.3% vs 0%; P = 0.025). In both groups, few cases of urinary retention (3 pts in SH vs none in MMH), anal stricture (2 pts in each group), urgency (5 pts in SH group vs 2 pts in MMH group), or anal hemorrhage (3 pts in SH group vs 1 pts in MMH group) were observed, but there was no significant difference (Table 3). Despite the difference in pain, bleeding, and soiling duration, the resumption of a normal lifestyle was not different between the two techniques (17.28 ± 11.32 days in SH group vs 18.37 ± 9.65 days in MMH group; P = 0.550) (Tables 2 and 3). Recurrence was based on the physical examination of the surgeon 1 and 2 years after the procedure. In SH, recurrence of prolapse was 7.4% (7 cases) and 2.6% in MMH (2 cases); the difference was not significant (P = 0.17). All patients were either satisfied or very satisfied and considered themselves cured by both surgical techniques.
Discussion
Hemorrhoids are one of the most common afflictions in the populations of industrialized countries, probably promoted by bipedal ambulation (gravity), lack of fiber in the diet, and the habit of squatting on a commode for relatively long periods of time. All these factors combine to increase pressure in the submucosal venous plexus in the anal canal, leading to venous and capillary distension and breakdown of the supporting submucosal connective tissue. Many surgical operations have been advocated for hemorrhoids over the centuries, with some from as far back as the time of Hippocrates (500 B.C.). During the past few decades, the favored operation has been the MMH and the Ferguson hemorrhoidectomy because of the relatively simple technique and reliable outcome observed. Complication rates are relatively low in experienced hands and are simple to manage.16 In 1998, Longo proposed a technique of SH for the treatment of hemorrhoids whereby a cylinder strip of mucosa and submucosa at the top of the hemorrhoids is removed by a 33-mm circular stapler, which creates an anastomosis between the proximal and distal mucosa and submucosa.12 The staple line is created approximately 4 cm above the dentate line. The procedure does not excise hemorrhoids. The purpose of the procedure is to pexy the anal canal in a more cranial position and to divide the terminal branches of the superior hemorrhoidal arteries, decreasing the blood supply to the hemorrhoidal venous plexus. Several prospective randomized controlled trials have been published comparing SH with MMH, diathermy excision, Ferguson hemorrhoidectomy, etc.,8–10 and few meta-analyses.4,11 The results of these studies suggested that SH may be at least as safe as standard open or closed hemorrhoidectomy including the MMH, but the efficacy could not be determined absolutely. The results of the published studies tend to show reasonable evidence in favor of SH for operating time, length of hospital stay, pain, anal discharge, and patient satisfaction. Skin tags and relapse of prolapse were more frequent after SH. Moreover, hemorrhoidopexy was not superior to MMH with regard to postoperative bleeding, urinary retention, difficulty in defecating, anal fissure, anal stenosis, sphincter damage, resumption of normal activity, incontinence, itching, anal resting, and squeezing pressures and analgesia. Recurrence rates are controversial; in some studies, they seem to be higher in SH than MMH;17 in other studies, there is no significant difference.9 Longo SH remains somewhat controversial despite the popularity that it has gained largely to the highly publicized “decreased pain” compared to traditional hemorrhoidectomy, although not all studies report this advantage. The reason for the controversy is due to many serious, and sometimes devastating, complications after the use of the PPH instrument including retroperineal sepsis,7 rectovaginal fistula, life-threatening stapled line hemorrhage, and severe and long-lasting pain reported in a small subset of patients.6,18,19 This catastrophic report of devastating and life-threatening complications, including a few deaths, has led to a consensus conference in which indications, contraindications, and even the surgical training necessary to be proficient in the technique are thoroughly addressed.20 The results of our study confirm that SH, when performed by trained specialists, is at least as safe as MMH. We had no life-threatening complications in this study, and the difference in postoperative complications such as anal stricture, urgency, urinary retention, postoperative hemorrhage, and the persistence of skin tags, was not significant. The occurrence of postoperative anal fissure, not present preoperatively, was significantly more frequent after SH than after MMH (6.3% vs 0%, P = 0.025) (Tables 2 and 3). This may be partially due to the technique itself, with the anal insertion of the large bore operating anoscope CAD used in SH. With regard to operating time, we did not find significant differences between the two techniques. Both surgeons who participated to the study are certified colorectal surgeons with a long learning curve on PPH use of more than 100 procedures done before the beginning of this study. The meticulous attention paid to surgical technique combined with a long learning curve probably contributed to minimizing complications both in SH and in MMH. In our study, the overall assessment of pain during the first eight postoperative days, considered as a whole, showed significantly less pain in SH compared to MMH (P = 0.016). In contrast to what other investigators have shown,1,2,21–24 we detected little difference in pain between the two groups on days 1 and 2 (Fig. 2); although, if we consider the period between the third and the eight postoperative days, the group of patients treated by SH experienced significantly less pain than the group treated with MMH (P = 0.002). In a prospective randomized study, a similar phenomenon was observed, with no difference in pain between the two groups on day 1.9 In most centers, hemorrhoids are not treated in a day-care setting. In our hospital, since 2002, a choice has been made to treat hemorrhoids in day care, and the population of our hospital district has been educated over the years to accept the method so well that, nowadays, most people would refuse to undergo hemorrhoidectomy with a regular hospital admittance and a hospital stay of 2 or 3 days, as most patients are subjected to in other hospitals in our town. Also, to our surprise, the great majority of patients treated for hemorrhoids regardless of the technique did not require further hospital stay; in fact, in the SH group, four patients required observation overnight for pain or urinary retention and three patients required admission for 2 to 4 days for postoperative complication, vs none of the patients treated by MMH. Postoperative symptoms such as pain, soiling, and anal bleeding lasted significantly less in SH than in MMH, as reported in several studies.1,9,21,22 It was interesting to observe that, regardless of the longer duration of postoperative symptoms related to surgery, there was no significant difference in resumption of normal activities between the two groups, although MMH patients complained about the length of time it took for anal wounds to heal. Both types of treatment were equally effective in curing the symptoms, with no patient declaring him\herself less than satisfied of the cure received. Among early postoperative complications, such as urgency of defecation, urinary retention, and postoperative hemorrhage, there is no difference between the two groups (Table 3) as shown in other studies,9 while postoperative anal fissure not present preoperatively was significantly more frequent after SH (P = 0.025) and usually persisted for several weeks or months, being a major complaint for the patients affected. Late complications such as skin tags and anal stricture did not show differences in the two groups, contrary to several other studies.1,2,9,21–23,25 There was a low rate of recurrence 2 years after surgery that was not different in the two groups (P = 0.17). Recurrence was assessed by the surgeon at physical examination and anoscopy and generally was asymptomatic. With regard to costs, in our experience, SH surgery is more expensive than MMH because of the cost of the stapler device, which is not offset by other costs such as operation time, shorter hospital stay, and earlier resumption of normal activities.
Conclusions
This prospective randomized study with a 3-year medium follow up confirms that SH is associated with less postoperative pain and shorter postoperative symptoms, compared with MMH. The technical component of the operation is straightforward and is feasible with local anesthesia, with very little sedation in a day care setting, the same as the MMH. Long-term outcome is good, and long- and short-term complications are low and comparable to those of MMH. SH in our study was not superior to MMH with regard to postoperative bleeding, urinary retention, anal stenosis, sphincter damage, and resumption of normal activities. Longo SH may be a viable addition to the therapy options available for hemorrhoids with advantages in early postoperative pain and some disadvantages in postoperative complications and costs.
References
Mehigan BJ, Monson JR, Hartley JE. Stapling procedure for haemorrhoids versus Milligan–Morgan haemorrhoidectomy: randomised controlled trial. Lancet 2000;355(9206):782–785. Mar 4.
Rowsell M, Bello M, Hemingway DM. Circumferential mucosectomy (stapled haemorrhoidectomy) versus conventional haemorrhoidectomy: randomised controlled trial. Lancet 2000;355(9206):779–781. Mar 4.
Boccasanta P, Capretti PG, Venturi M, Cioffi U, De Simone M, Salamina G, Contessini-Avesani E, Peracchia A. Randomised controlled trial between stapled circumferential mucosectomy and conventional circular hemorrhoidectomy in advanced hemorrhoids with external mucosal prolapse. Am J Surg 2001;182(1):64–68. Jul.
Jayaraman S, Colquhoun PH, Malthaner RA. Stapled versus conventional surgery for hemorrhoids (Review). The Cochrane Collaboration Oct. 18; (4). New York: Wiley.
Pescatori M. Stapled hemorrhoidectomy: a word of caution. Int J Colorectal Dis 2002;17(5):362–363. Sep.
Cheetham MJ, Mortensen NJ, Nystrom PO, Kamm MA, Phillips RK. Persistent pain and faecal urgency after stapled haemorrhoidectomy. Lancet 2000;356(9231):730–733. Aug 26.
Maw A, Kong-Weng E, Seow-Cohen F. Retroperitoneal sepsis complicating stapled haemorrhoidectomy. Dis Colon Rectum 2002;45(6):826–828. June.
Ortiz H, Marzo J, Armendariz P, De Miguel M. Stapled haemorrhoidopexy vs diathermy excision for fourth- degree haemorrhoids: a randomized, clinical trial and review of the litterature. Dis Colon Rectum 2005;48:1837–1845.
Gravie JF, Lehur PA, Huten N, Papillon M, Fantoli M, Descottes B, Pessaux P, Arnaud JP. Stapled hemorrhoidopexy versus milligan–morgan hemorrhoidectomy: a prospective, randomized, multicenter trial with 2-year postoperative follow up. Ann Surg 2005;242(1):29–35. Jul.
Senagore AJ, Singer M, Abcarian H, Fleshman J, Corman M, Wexner S, Nivatvongs S. Procedure for Prolapse and Hemmorrhoids (PPH) Multicenter Study Group A prospective, randomized, controlled multicenter trial comparing stapled hemorrhoidopexy and Ferguson hemorrhoidectomy: perioperative and one-year results. Dis Colon Rectum 2004;47(11):1824–1836. Nov.
Lan P, Wu X, Zhou X, Wang J, Zhang L. The safety and efficacy of stapled hemorrhoidectomy in the treatment of hemorrhoids: a systematic review and meta-analysis of ten randomized control trials. Int J Colorectal Dis 2006;21(2):172–178. Epub 2005 Jun 22 Mar.
Longo A. Treatment of hemorrhoids disease by reduction of mucosa and hemmoroidal prolapse with a circular suturing device: a new procedure. Proceedings of the 6th Wold Congress of Endoscopic Surgery. Monduzzi Editore. 1998;777–784.
Milligan ETC, Morgan CN, Jones LE. Surgical anatomy of the anal canal and operative treatment of haemorrhoids. Lancet 1937;1:1119–1124.
Cohen J. Statitical Power Analysis for the Behavioural Sciences. 2nd ed. Hillsdale: Lawrence Erlbaum, 1988.
G*Power; Erdfelder, Faul and Buchner. Behaviour research methods, Intruments and Computers 1996 (Last improvement G*Power 3 2006)
Stamos MJ. Stapled hemorrhoidectomy. J Gastrointest Surg 2006;10(5):627–628. May.
Nisar PJ, Scholefield JH. Clinical review: managing haemorroids. BMJ 2003;327:845–851.
Thaha MA, Irvine LA, Steele RJ, Campbell KL. Postdefaecation pain syndrome after circular stapled anopexy is abolished by oral nifedipine. Br J Surg 2005;92(2):208–210. Feb.
Brusciano L, Ayabaca SM, Pescatori M, Accarpio GM, Dodi G, Cavallari F, Ravo B, Annibali R. Reinterventions after complicated or failed stapled hemorrhoidopexy. Dis Colon Rectum 2004;47(11):1846–1851. Nov.
Corman ML, Gravie JF, Hager T, Loudon MA, Mascagni D, Nystrom PO, Seow-Choen F, Abcarian H, Marcello P, Weiss E, Longo A. Stapled haemorrhoidopexy: a consensus position paper by an international working party—indications, contra-indications and technique. Colorectal Dis 2003;5(4):304–310. Jul.
Ganio E, Altomare DF, Gabrielli F, Milito G, Canuti S. Prospective randomized multicentre trial comparing stapled with open haemorrhoidectomy. Br J Surg 2001;88(5):669–674. May.
Ho YH, Cheong WK, Tsang C, Ho J, Eu KW, Tang CL, Seow-Choen F. Stapled hemorrhoidectomy—cost and effectiveness. Randomized, controlled trial including incontinence scoring, anorectal manometry, and endoanal ultrasound assessments at up to three months. Dis Colon Rectum 2000;43(12):1666–1675. Dec.
Shalaby R, Desoky A. Randomized clinical trial of stapled versus Milligan–Morgan haemorrhoidectomy. Br J Surg 2001;88(8):1049–1053. Aug.
Kairaluoma M, Nuorva K, Kellokumpu I. Day-case stapled (circular) vs. diathermy hemorrhoidectomy: a randomized, controlled trial evaluating surgical and functional outcome. Dis Colon Rectum 2003;46(1):93–99. Jan.
Boccasanta P, Stuto A, Naldini G, Caviglia A, Carriero A. Opinions and facts on reinterventions after complicated or failed stapled hemorrhoidectomy. Dis Colon Rectum 2006;49(5):690–691. author reply 691–693. May.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stolfi, V.M., Sileri, P., Micossi, C. et al. Treatment of Hemorrhoids in Day Surgery: Stapled Hemorrhoidopexy vs Milligan–Morgan Hemorrhoidectomy. J Gastrointest Surg 12, 795–801 (2008). https://doi.org/10.1007/s11605-008-0497-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0497-8