Abstract
Background
Survival for patients with unresectable cholangiocarcinoma is reported to range from only 5–8 months without treatment. Systemic chemotherapy has not been shown to significantly improve survival, but newer regimens involving gemcitabine have shown increased response rates. Transcatheter arterial chemoembolization (TACE) has been shown to prolong survival in hepatocellular carcinoma patients, but experience using TACE in the treatment of cholangiocarcinoma is limited. We report our experience treating cholangiocarcinoma with TACE using chemotherapeutic regimens based on the well-tolerated drug gemcitabine.
Methods
Forty-two patients with unresectable cholangiocarcinoma were treated with one or more cycles of gemcitabine-based TACE at our institution. Chemotherapy regimens used for TACE included: gemcitabine only (n = 18), gemcitabine followed by cisplatin (n = 2), gemcitabine followed by oxaliplatin (n = 4), gemcitabine and cisplatin in combination (n = 14), and gemcitabine and cisplatin followed by oxaliplatin (n = 4).
Results
Patients were 59 years of age (range 36–86) and received a median of 3.5 TACE treatments (range 1–16). Thirty-seven patients (88%) had central cholangiocarcinoma, and five (12%) had peripheral tumors. Nineteen patients (45%) had extrahepatic disease. Grade 3 adverse events (AEs) after TACE treatments were seen in five patients, whereas grade 4 AEs occurred in two patients. No patients died within 30 days of TACE. Median survival from time of first treatment was 9.1 months overall. Results did not vary by patient age, sex, size of largest initial tumor, or by the presence of extra-hepatic disease. Treatment with gemcitabine–cisplatin combination TACE resulted in significantly longer survival (13.8 months) compared to TACE with gemcitabine alone (6.3 months).
Conclusions
Our report represents the largest series to date regarding hepatic-artery-directed therapy for unresectable cholangiocarcinoma and provides evidence in favor of TACE as a promising treatment modality in unresectable cholangiocarcinoma. Our results suggest that gemcitabine-based TACE is well tolerated and confers better survival when given in combination therapy (with cisplatin or oxaliplatin) for patients with unresectable cholangiocarcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cholangiocarcinoma (CC) is a primary adenocarcinoma of the bile ducts. It is the second most common primary hepatic malignancy in the world, but is a rare neoplasm in the USA, with an incidence of only 0.5–2 per 100,000 population.1 In other parts of the world, however, particularly in East and Southeast Asia, rates are much higher, and overall global incidence is increasing.2–4
Cholangiocarcinoma historically has an extremely poor prognosis. Patients who present symptomatically usually have advanced disease which is not amenable to surgical resection. Mortality results from progressive liver failure or biliary obstruction and resulting cholangitis and sepsis.5
Survival for patients with unresectable cholangiocarcinoma is reported to be only 5–8 months. Intrahepatic CC generally presents in a more advanced state than extrahepatic CC, so prognosis is often even worse.6 Curative treatment is only possible with surgical resection, but less than 30% of patients are resectable at presentation.7 Of those resected, 5-year survival is reported as only 20–40%.8 Overall survival for all patients at 5 years from diagnosis is less than 5%.9
Systemic chemotherapy has been disappointing in regard to its efficacy, with most regimens resulting in a median survival of 6–12 months.10 No randomized studies have shown a significant improvement in overall survival compared to observation alone.11 Side effects are common and often limit patients’ tolerance of the therapy and their quality of life. Because of the poor results with standard systemic therapy, there has been a great interest in other modalities for treatment of cholangiocarcinoma. These have included chemoradiation,12 external beam radiation,13 radiofrequency ablation,14 photodynamic therapy (PDT),15,16 brachytherapy,17 hepatic artery infusion chemotherapy,18 and transcatheter arterial chemoembolization.6
Transcatheter arterial chemoembolization (TACE) is a promising, minimally invasive treatment modality for unresectable liver tumors. TACE allows delivery of high doses of chemotherapeutic drug directly to the tumor with very little systemic drug exposure.
TACE has been shown to be a useful treatment modality in hepatocellular carcinoma (HCC), with two randomized trials showing an improved survival over supportive care alone.19,20
Experience with TACE for biliary malignancies is limited, but recently, several small series have shown promising survival in CC patients treated with TACE.6,21,22 In addition, there have been numerous reports of intra-arterial delivery of chemotherapy drugs, in varied forms, in an attempt to maximize therapy to CC while limiting systemic side effects.18,23–25
Recently, patients receiving systemic chemotherapy for cholangiocarcinoma have benefited from the approval of gemcitabine, a nucleoside analogue drug which has shown promising response rates (up to 30–40%) in systemic treatment of CC.26 Gemcitabine has become the most commonly recommended first-line drug for systemic treatment of CC. It is well tolerated, and combination therapy with drugs such as 5-FU, cisplatin, and oxaliplatin offers potential synergistic tumoricidal effects.11 Because gemcitabine is rapidly deaminated to the inactive metabolite 2′2′ difluorodeoxyuridine (dFdU), it has an exceedingly high total body clearance (CLtb). The liver serves as a primary source for deamination on first pass.27 This should allow high intrahepatic gemcitabine concentrations to be achieved with little systemic exposure. Based on its promising antitumor activity and favorable pharmacokinetic and safety profiles, we selected gemcitabine as the basis for liver-directed TACE treatments in cholangiocarcinoma.
At the University of Pittsburgh Medical Center (UPMC) Liver Cancer Center, a significant experience with CC exists.28 Multidisciplinary therapeutic options include: surgery, radiofrequency ablation, hepatic artery infusional chemotherapy, systemic chemotherapy, and TACE. In this report, we describe our experience treating unresectable cholangiocarcinoma with TACE using regimens based on the well-tolerated drug gemcitabine.
Methods
Study Design
We performed a retrospective review of medical records for all patients treated with gemcitabine-based TACE at the UPMC Liver Cancer Center between June 2001 and February 2007. Data for the current study were extracted from an institutional database designed specifically to track outcomes of liver cancer patients. All data evaluation was done under a protocol approved by the University of Pittsburgh Institutional Review Board.
Once qualifying patients were identified, all patient data were de-identified through the use of an approved Honest Broker. Data variables included demographic, pre-procedure, procedure, and post-procedure data as well as long-term follow-up of all patients. Data were retrospectively gathered from patient charts, electronic medical records, and review of available imaging and pathology. In addition, the Social Security Death Index (SSDI) was queried to determine date of death for any patients not captured by our records. Morbidity was graded on a 1–5 scale according to criteria established by the National Cancer Institute’s Cancer Therapy Evaluation Program.29
Patients
During the study period (June 2001 to February 2007), 42 patients, all with unresectable intrahepatic cholangiocarcinoma, were treated with one or more cycles of gemcitabine-based TACE.
Initial Evaluation
Initial evaluation consisted of a complete history and physical at the UPMC Liver Cancer Center. All patients had biopsy-proven cholangiocarcinoma. Staging workup included a triphasic chest/abdomen/pelvis computed tomography (CT) scan or magnetic resonance imaging. Patients who were deemed to be unresectable but had acceptable laboratory values and performance status were considered for TACE. Contraindications to TACE included total bilirubin >3 mg/dl, serum creatinine >2× baseline, and ECOG performance status >1. Patients with biliary obstruction were treated with ERCP-based or percutaneous transhepatic biliary stents before administration of TACE.
TACE Procedures
All TACE procedures were performed by interventional radiologists at the University of Pittsburgh Medical Center using standard protocols. The day of the procedure, patients had screening laboratory studies and received intravenous fluid before treatment. Based on the results of the laboratory studies and recent imaging, a decision was made about the segment(s) of the liver to receive TACE and the drugs to be given.
After intravenous hydration was given for 2–3 h, patients were taken to the interventional radiology angiographic suite. Cannulation of the femoral artery was performed, and an arterial catheter was advanced under fluoroscopy to catheterize the celiac and superior mesenteric arteries. At the initial treatment session, complete diagnostic arteriography was performed to determine the hepatic arterial anatomy and to map all arterial vessels supplying the tumor. Therapeutic chemoinfusion was then performed, usually into the right or left hepatic artery, over a 30- to 45-min time period. If treatment included two drugs, each was given separately for a total infusion time of 60–90 min. After delivery of the drug(s) to the tumor, embolization was accomplished with Embospheres (Biosphere Medical, Inc., Rockland, MA, USA) until moderate to marked stasis of antegrade flow was seen in the artery.
Chemotherapeutic drug choice was made based on the patient’s previous therapy history, laboratory profile, and functional status. Generally, patients were given one drug or combination of drugs until signs that the patient’s tumor was progressing. At that point, if deemed clinically suitable, the patient’s regimen was altered to add a drug or change drugs. In the case of bilateral liver tumors, therapy was given to the side of the dominant tumor(s) until progression occurred on the contralateral side. At this point, the contralateral side was treated. Intra-arterial gemcitabine treatments were conducted with dose escalation starting from 1,250 mg/m2 up to 2,250 mg/m2 as tolerated. Intra-arterial cisplatin and oxaliplatin doses were 100–125 mg/m2 and 85–100 mg/m2, respectively.
Patients were observed overnight after the procedure for control of pain and nausea, administration of intravenous fluids, and monitoring of systemic side effects. Patients were routinely discharged home the following morning after laboratory studies were evaluated. All patients were prescribed anti-emetic and pain medications for home management of post-embolization syndrome (low-grade fever, pain, nausea).
Follow-up
After discharge, laboratory values were checked weekly on an outpatient basis. Follow-up imaging was performed on all patients 6–8 weeks after each TACE procedure. Decisions regarding further TACE therapy were made based on the patients’ tolerance of previous TACE as well as their tumor response to therapy.
Statistical Analysis
Overall survival was determined for all patients from the date of first TACE procedure to death. The Kaplan–Meier (product-limit) method was used to determine estimates of survival. The log-rank test was performed to assess overall survival and test differences in survival among TACE regimens. Survival plots and statistical analyses were performed using GraphPad Prism 5.0 software for Windows (GraphPad Software, Inc., San Diego, CA, USA). Statistical significance was assigned for a p value of ≤0.05.
Results
Patient and Tumor Details
During the study time period from June 2001 to February 2007, 42 patients underwent TACE with gemcitabine-based chemotherapy regimens for unresectable cholangiocarcinoma. The study included 21 men and 21 women. Patients’ median age was 59 years (range 36–87). All patients had mass-forming intrahepatic cholangiocarcinoma proven by biopsy. All patients’ ECOG performance status was 0 or 1. Thirty-seven patients (88%) had central cholangiocarcinoma, and five (12%) had peripheral tumors.
Median size of the largest single tumor nodule at presentation was 9.8 cm (range 1.3–17.0 cm). The median Ca 19-9 level for the group was 134 U/ml (<4–140,460). Nineteen of 42 patients (45%) had extrahepatic disease at time of presentation. Of these, four had disease confined to the porta hepatis lymph nodes, eight had intra-abdominal disease, and seven had distant metastasis (Table 1).
TACE Treatments
Forty-two patients underwent 199 TACE procedures, with a median of 3.5 TACE treatments per patient (range 1–16). Patients received one of five different chemotherapy-TACE regimens: gemcitabine alone, gemcitabine followed by cisplatin, gemcitabine followed by oxaliplatin, gemcitabine–cisplatin combination, and gemcitabine-cisplatin followed by oxaliplatin (Table 2).
Morbidity
TACE treatments were generally well tolerated. All patients were admitted overnight for observation after TACE. Ninety-six percent of patient admissions resulted in discharge on post-TACE day no. 1 (23-h admission), with the remaining 4% going home on post-TACE day no. 2.
Grade 4 adverse events (AEs) were seen in two patients. One patient developed crescendo angina 1 day after his first TACE and was diagnosed with an acute myocardial infarction. He underwent cardiac catheterization with angioplasty and coronary stent placement and made a full recovery. The patient went on to have nine further TACE cycles over the next 18 months. A second patient developed a hepatic abscess 1 week after his second TACE treatment. This patient required admission for drainage of the abscess and intravenous antibiotics. The patient developed grade 4 thrombocytopenia and sepsis associated with the abscess. This adverse event resulted in a hospitalization for 7 days with resolution of the sepsis, and the patient was discharged home with a percutaneous hepatic drain in place.
Five additional patients developed grade 3 AEs after TACE. One patient was over-sedated with narcotic pain medication and developed mild respiratory distress on the evening after TACE. When the patient’s mental status changes were reported, naloxone was administered with immediate resolution. Two patients developed grade 3 hyperbilirubinemia, and two developed grade 3 thrombocytopenia.
Minor morbidity was seen in nine patients who developed grade 2 adverse events and seven who developed grade 1 AEs (Table 3). In addition, most patients did experience “post embolization syndrome” consisting of low-grade fever, nausea, and abdominal pain. These symptoms were easily managed with antiemetics and narcotic medications. As evidenced by the high discharge rate on post-TACE day no. 1, these symptoms were generally not prolonged.
Morbidity did not vary significantly by patient age, TACE regimen, or by the presence of extrahepatic disease.
Tumor Response to TACE
Tumor response to TACE was gauged using the response evaluation criteria in solid tumors (RECIST) guidelines.30 Attempts were made to gauge response after three cycles of TACE if possible. Those receiving fewer TACE treatments were evaluated after the last TACE performed. Based on this evaluation, 20 patients were found to have stable disease, 15 patients had progressive disease, and seven were not evaluable.
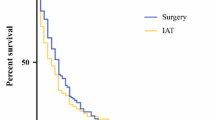
Survival
Median overall survival from the date of first TACE treatment was 9.1 months (Fig. 1). Survival did not vary by patient age, sex, size of largest initial tumor, or by presence of extrahepatic disease. Patients with peripheral cholangiocarcinoma, however, had better median survival (18.7 vs 8.2 months) than those with central tumors (p = 0.012 by log-rank test).
Survival did vary by response to TACE as measured by RECIST criteria. Patients who had stable disease by RECIST criteria underwent a median of six TACE cycles and had median survival of 13.1 months post-TACE, whereas patients who had progressive disease were able to have three TACE cycles and had post-TACE median survival of 6.9 months (p = 0.017).
Survival varied significantly by TACE regimen (Table 4). When comparing the survival curves for the two most frequently used TACE regimens, there was a statistically significant increase in survival for patients receiving TACE treatments with the gemcitabine-cisplatin combination over those receiving gemcitabine alone (13.8 vs 6.3 months, p = 0.0005; Fig. 2).
Discussion
Cholangiocarcinoma is a deadly disease with a very poor prognosis. Most patients who are diagnosed with CC are not candidates for surgical resection, which is the only treatment with potential for cure. Currently, therapeutic options for unresectable cholangiocarcinoma afford little or no improvement in survival over supportive therapy alone. Thus, there is a strong incentive to explore newer therapeutic options in an attempt to improve the outcome in this difficult disease. In this paper, we present promising results for treatment of unresectable cholangiocarcinoma using gemcitabine-based TACE.
Treatment of cholangiocarcinoma with chemotherapy or chemoradiation has proven to have little benefit in improving survival. Most published studies using these modalities for cholangiocarcinoma are small, phase I or phase II single-institution trials with a wide variation in outcomes. The few larger scale studies published have involved multiple tumor types, often including both intrahepatic and extrahepatic CC as well as sometimes pancreatic cancer and hepatocellular cancer.31 No randomized study has shown a significant benefit of systemic chemotherapy or chemoradiation over supportive care alone.9
The University of Pittsburgh Medical Center is a high volume center for the treatment of liver cancer.28 Approximately 11% of our new liver cancer patients have cholangiocarcinoma. We favor an aggressive surgical approach to CC, with surgical resection as the goal.32,33 Each patient is seen and discussed by a multidisciplinary team which offers the full range of treatment options from transplant and resection to systemic therapy, regional therapy, or palliative care. We offer special expertise in regional therapy strategies for treatment of liver tumors, performing a high volume of TACE (>400 treatments per year) and selective internal radiation with Yttrium-90 microspheres (>200 treatments to date) treatments in the setting of unresectable disease.
In the case of patients with unresectable disease, our primary goal of therapy is palliation: we aim to prolong survival while maintaining an acceptable quality of life. For these patients, we often choose a regional therapy as an attempt to maximize treatment delivered to the tumor while minimizing systemic side effects.
TACE is a modality widely used in patients with primary liver cancer (hepatoma). TACE is minimally invasive and can be performed on an outpatient or short-stay basis. Combining intra-arterial delivery of chemotherapy via the hepatic artery with embolization takes advantage of the fact that liver tumors receive 90–100% of their blood flow from the hepatic artery.34 Thus, TACE provides targeted delivery of a chemotherapeutic agent directly to the tumor. Delivery of chemotherapy is followed by arterial embolization, which causes further necrosis of the tumor by eliminating its predominant blood supply. In addition, by reducing blood flow through the tumor, embolization may prevent washout of the chemotherapeutic agent, resulting in higher concentrations of the drug remaining in the tumor cells while also reducing systemic exposure.35 TACE has been shown in two randomized controlled clinical trials,19,20 to improve survival in patients with unresectable HCC, and these results have been confirmed in two meta-analyses.36,37
Our data reveal a median survival of 9.1 months after gemcitabine-based TACE. The survival provided by TACE is significant, especially in light of the fact that many of our patients had already failed other treatment modalities before undergoing TACE. More important, combination regimens utilizing gemcitabine as first-line therapy followed by cisplatin or oxaliplatin or using the gemcitabine–cisplatin combination showed significantly greater response and survival, reaching up to 13–18 months. Although some of the survival difference may be due to selection bias in our retrospective review, our results do imply a benefit from combination chemotherapy regimens.
Of note, median survival in our overall cohort of 42 patients was not significantly different in patients with liver-only disease as compared to those with extrahepatic disease. This supports the belief that in patients with liver-predominant disease, the liver tumors determine eventual survival rather than the extrahepatic disease, and therefore, we favor regional treatment in these patients.
Tumor response to TACE treatments, using RECIST criteria, predicted improved survival (median survival 13.1 months in patients with stable disease vs 6.9 months in patients with progressive disease), but many authors have questioned whether size-based criteria are the best measure of the effectiveness of TACE.38,39 Although by RECIST criteria TACE treatments did not result in significant tumor shrinkage in any of our patients, several had evidence of tumor necrosis or decrease in tumor vascularity post-TACE (Fig. 3).
Gemcitabine-based TACE treatment proved to be well tolerated, with minimal significant side effects (only 17% of patients had grades 3 or 4 AEs). This tolerability profile fits with the goals of palliative therapy—to prolong life while maintaining quality of life. Although we did not specifically measure quality of life in this study, most patients were home 24 h post-TACE and did not suffer debilitating side effects. The limitations on their lifestyle consisted mainly of a post-embolization syndrome the few days after administration of TACE and the need for several outpatient laboratory studies obtained weekly after treatment. In contrast, systemic combination chemotherapy regimens using gemcitabine have grades 3–4 toxicities in over 40% of patients in recent phase II trials.40,41
In addition to our work, the results of two recent studies lend credence to the concept of intra-arterial treatment for unresectable cholangiocarcinoma. In a report from Burger et al.,6 TACE was performed in 17 patients with unresectable intrahepatic cholangiocarcinoma. Their group utilized varying TACE chemotherapy regimens, mostly including cisplatin, doxorubicin, and mitomycin-C. Although they report a median survival of 23 months, their survival was measured from the time of diagnosis rather than initiation of TACE treatment, making direct comparison difficult. Also, there may be differences in the patient populations being treated with TACE, as ten of the patients in the Burger study had only stage II disease.
Tanaka et al.,18 published promising results using a protocol of arterial chemoinfusion through an implanted port system in 11 patients. Their regimens of intra-arterial chemotherapy included various combinations of 5-FU, doxorubicin, cisplatin, and mitomycin-C and resulted in mean survival of 26 months in patients. Again, differences in reporting (mean survival rather than median) and patient characteristics (mean tumor size of 7 cm) make direct comparisons difficult.
As mentioned earlier, we selected gemcitabine as our drug of choice for liver-directed TACE therapy based on its in vivo and in vitro activity against CC, its pharmacokinetics, and its record of safety.10,11,26,42 With similar considerations in mind, Vogl et al.43 previously determined the maximum tolerated dose for intra-arterial treatment of cholangiocarcinoma and pancreatic cancer liver metastases with gemcitabine. In their study, 17 patients with intrahepatic cholangiocarcinoma were treated with transcatheter arterial gemcitabine (with or without starch microsphere embolization) in increasing doses from 200 to 2,000 mg/m2. Chemotherapy infusions were given twice during an 8-day treatment cycle, with cycles repeated every 2 weeks. The maximum tolerated dose found in this study was 1,400 mg/m2 without microspheres or 1,800 mg/m2 with microspheres. This dose is similar to that used in our study and confirms that higher doses than those given systemically can be given intrahepatic with an acceptable toxicity profile.
Future investigations will be important to clarify the role of TACE in the treatment of unresectable cholangiocarcinoma. In particular, because of its excellent toxicity profile, TACE may be safely combined with other modalities of treatment to produce complementary or synergistic effects. Several authors have explored combinations of intra-arterial treatments with systemic chemotherapy,21,24 radiation,25,44 or biliary drainage22 in small studies. Combinations of these therapies with gemcitabine-based TACE could potentially result in increased survival with minimal side effects.
In addition, as biliary obstruction is so often the eventual cause of mortality in patients with intrahepatic cholangiocarcinoma, it will be important to consider combinations of TACE with bile-duct-based therapeutic interventions such as PDT or brachytherapy. Brachytherapy or PDT lack adequate depth of tissue penetration to significantly affect large, mass-forming CC tumors, but the combination of these treatments with TACE may be beneficial.
The use of hepatic arterial infusion of Yttrium-90 microspheres for the treatment of inoperable CC is also a potential treatment modality. This technology is already approved by the United States Food and Drug Administration for selective internal radiation treatment in metastatic colorectal cancer (in combination with intra-arterial Floxuridine)45 and hepatocellular cancer.46 The treatment of other types of intrahepatic tumors is a current interest, and this treatment may represent a useful option for cholangiocarcinoma in the future.47–50
Conclusion
Our report represents the largest series to date describing hepatic-artery-directed therapy for unresectable cholangiocarcinoma. These results provide evidence in favor of gemcitabine-based TACE as a promising mode of therapy for palliation in unresectable cholangiocarcinoma. TACE regimens utilizing gemcitabine, especially in combination with cisplatin or oxaliplatin, may offer equivalent or improved survival when compared to traditional modalities such as systemic chemotherapy or chemoradiation.
We report gemcitabine-based TACE as a useful modality even in patients with minimal extrahepatic disease, offering similar survival outcomes to patients with liver-only disease. Our results demonstrate that gemcitabine-based TACE is well tolerated and suggest that it may offer acceptable quality of life. In a disease with limited treatment options and a dismal prognosis, we believe that this treatment modality warrants further investigation.
References
Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis 2004;24(2):115–125.
Malhi H, Gores GJ. Cholangiocarcinoma: modern advances in understanding a deadly old disease. J Hepatol 2006;45(6):856–867.
Patel T. Increasing incidence and mortality of primary intrahepatic cholangiocarcinoma in the United States. Hepatology 2001;33(6):1353–1357.
Patel T. Worldwide trends in mortality from biliary tract malignancies. BMC Cancer 2002;2:10.
Farley DR, Weaver AL, Nagorney DM. “Natural history” of unresected cholangiocarcinoma: patient outcome after noncurative intervention. Mayo Clin Proc 1995;70(5):425–429.
Burger I, Hong K, Schulick R, et al. Transcatheter arterial chemoembolization in unresectable cholangiocarcinoma: initial experience in a single institution. J Vasc Interv Radiol 2005;16(3):353–361.
Khan SA, Davidson BR, Goldin R, et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: consensus document. Gut 2002;51(Suppl 6):VI1–9.
Jarnagin WR, Shoup M. Surgical management of cholangiocarcinoma. Semin Liver Dis 2004;24(2):189–199.
Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet 2005;366(9493):1303–1314.
Thongprasert S. The role of chemotherapy in cholangiocarcinoma. Ann Oncol 2005;16(Suppl 2):ii93–96.
Mazhar D, Stebbing J, Bower M. Chemotherapy for advanced cholangiocarcinoma: what is standard treatment? Future Oncol 2006;2(4):509–514.
Crane CH, Macdonald KO, Vauthey JN, et al. Limitations of conventional doses of chemoradiation for unresectable biliary cancer. Int J Radiat Oncol Biol Phys 2002;53(4):969–974.
Zeng Z-C, Tang Z-Y, Fan J, et al. Consideration of the role of radiotherapy for unresectable intrahepatic cholangiocarcinoma: a retrospective analysis of 75 patients. Cancer J 2006;12(2):113–122 (see comment).
Slakey DP. Radiofrequency ablation of recurrent cholangiocarcinoma. Am Surgeon 2002;68(4):395–397.
Berr F. Photodynamic therapy for cholangiocarcinoma. Semin Liver Dis 2004;24(2):177–187.
Wiedmann M, Berr F, Schiefke I, et al. Photodynamic therapy in patients with non-resectable hilar cholangiocarcinoma: 5-year follow-up of a prospective phase II study. Gastrointest Endosc 2004;60(1):68–75.
Chen Y, Wang X-L, Yan Z-P, et al. HDR-192Ir intraluminal brachytherapy in treatment of malignant obstructive jaundice. World J Gastroenterol 2004;10(23):3506–3510.
Tanaka N, Yamakado K, Nakatsuka A, et al. Arterial chemoinfusion therapy through an implanted port system for patients with unresectable intrahepatic cholangiocarcinoma—initial experience. Eur J Radiol 2002;41(1):42–48.
Llovet JM, Real MI, Montana X, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 2002;359(9319):1734–1739.
Lo C-M, Ngan H, Tso W-K, et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 2002;35(5):1164–1171.
Kirchhoff T, Zender L, Merkesdal S, et al. Initial experience from a combination of systemic and regional chemotherapy in the treatment of patients with nonresectable cholangiocellular carcinoma in the liver. World J Gastroenterol 2005;11(8):1091–1095.
Qian X-J, Zhai R-Y, Dai D-K, et al. Treatment of malignant biliary obstruction by combined percutaneous transhepatic biliary drainage with local tumor treatment. World J Gastroenterol 2006;12(2):331–335.
Melichar B, Cerman J, Jr., Dvorak J, et al. Regional chemotherapy in biliary tract cancers-a single institution experience. Hepato-Gastroenterology 2002;49(46):900–906.
Cantore M, Mambrini A, Fiorentini G, et al. Phase II study of hepatic intraarterial epirubicin and cisplatin, with systemic 5-fluorouracil in patients with unresectable biliary tract tumors. Cancer 2005;103(7):1402–1407.
Ben-Josef E, Normolle D, Ensminger WD, et al. Phase II trial of high-dose conformal radiation therapy with concurrent hepatic artery floxuridine for unresectable intrahepatic malignancies. J Clin Oncol 2005;23(34):8739–8747.
Dingle BH, Rumble RB, Brouwers MC, Cancer Care Ontario’s Program in Evidence-Based Care’s Gastrointestinal Cancer Disease Site G. The role of gemcitabine in the treatment of cholangiocarcinoma and gallbladder cancer: a systematic review. Can J Gastroenterol 2005;19(12):711–716.
Dedrick RL, Forrester DD, Ho DH. In vitro-in vivo correlation of drug metabolism—deamination of 1-β-d-arabinofuranosylcytosine. Biochem Pharmacol 1972;21(1):1–16.
Geller DA, Tsung A, Marsh JW, et al. Outcome of 1000 liver cancer patients evaluated at the UPMC Liver Cancer Center. J Gastrointest Surg 2006;10(1):63–68.
NCI-CTEP. Common Terminology Criteria for Adverse Events v3.0 (CTCAE). Available Online at http://ctep.cancer.gov. 2003.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European organization for research and treatment of cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 2000;92(3):205–216.
Leonard GD, O’Reilly EM. Biliary tract cancers: current concepts and controversies. Exp Opin Pharmacother 2005;6(2):211–223.
Iwatsuki S, Todo S, Marsh JW, et al. Treatment of hilar cholangiocarcinoma (Klatskin tumors) with hepatic resection or transplantation. J Am Coll Surg 1998;187(4):358–364.
Casavilla FA, Marsh JW, Iwatsuki S, et al. Hepatic resection and transplantation for peripheral cholangiocarcinoma. J Am Coll Surg 1997;185(5):429–436.
Lau WY, Yu SCH, Lai ECH, Leung TWT. Transarterial chemoembolization for hepatocellular carcinoma. J Am Coll Surg 2006;202(1):155–168.
Ramsey DE, Kernagis LY, Soulen MC, Geschwind J-FH. Chemoembolization of hepatocellular carcinoma. J Vasc Interv Radiol 2002;13(9 Pt 2):S211–221.
Camma C, Schepis F, Orlando A, et al. Transarterial chemoembolization for unresectable hepatocellular carcinoma: meta-analysis of randomized controlled trials. Radiology 2002;224(1):47–54.
Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 2003;37(2):429–442.
Kamel IR, Bluemke DA, Ramsey D, et al. Role of diffusion-weighted imaging in estimating tumor necrosis after chemoembolization of hepatocellular carcinoma. AJR Am J Roentgenol 2003;181(3):708–710.
Tuma RS. Sometimes size doesn’t matter: reevaluating RECIST and tumor response rate endpoints. J Natl Cancer Inst 2006;98(18):1272–1274.
Lee G-W, Kang JH, Kim H-G, et al. Combination chemotherapy with gemcitabine and cisplatin as first-line treatment for immunohistochemically proven cholangiocarcinoma. Am J Clin Oncol 2006;29(2):127–131.
Alberts SR, Al-Khatib H, Mahoney MR, et al. Gemcitabine, 5-fluorouracil, and leucovorin in advanced biliary tract and gallbladder carcinoma: a North Central Cancer Treatment Group phase II trial. Cancer 2005;103(1):111–118.
Scheithauer W. Review of gemcitabine in biliary tract carcinoma. Semin Oncol 2002;29(6 Suppl 20):40–45.
Vogl TJ, Schwarz W, Eichler K, et al. Hepatic intraarterial chemotherapy with gemcitabine in patients with unresectable cholangiocarcinomas and liver metastases of pancreatic cancer: a clinical study on maximum tolerable dose and treatment efficacy. J Cancer Res Clin Oncol 2006;132(11):745–755.
Matsumoto S, Kiyosue H, Komatsu E, et al. Radiotherapy combined with transarterial infusion chemotherapy and concurrent infusion of a vasoconstrictor agent for nonresectable advanced hepatic hilar duct carcinoma. Cancer 2004;100(11):2422–2429.
FDA. SIR-Spheres®-P990065. Available Online at http://www.fda.gov/cdrh/pdf/p990065.html. 2002.
FDA. H980006-TheraSphere®. Available Online at http://www.fda.gov/cdrh/ode/H980006sum.html. 1999.
Garrean S, Joseph Espat N. Yttrium-90 internal radiation therapy for hepatic malignancy. Surg Oncol 2005;14(4):179–193.
Lim L, Gibbs P, Yip D, et al. Prospective study of treatment with selective internal radiation therapy spheres in patients with unresectable primary or secondary hepatic malignancies. Intern Med J 2005;35(4):222–227.
Salem R, Thurston KG. Radioembolization with yttrium-90 microspheres: a state-of-the-art brachytherapy treatment for primary and secondary liver malignancies: part 3: comprehensive literature review and future direction. J Vasc Interv Radiol 2006;17(10):1571–1593.
Jakobs TF, Hoffmann R-T, Poepperl G, et al. Mid-term results in otherwise treatment refractory primary or secondary liver confined tumours treated with selective internal radiation therapy (SIRT) using (90)Yttrium resin-microspheres. Eur Radiol 2007;17(5):1320–1330.
Acknowledgment
This work was supported by the NIH Roadmap Multidisciplinary Clinical Research Career Development Award Grant (K12 HD049109) from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gusani, N.J., Balaa, F.K., Steel, J.L. et al. Treatment of Unresectable Cholangiocarcinoma with Gemcitabine-Based Transcatheter Arterial Chemoembolization (TACE): A Single-Institution Experience. J Gastrointest Surg 12, 129–137 (2008). https://doi.org/10.1007/s11605-007-0312-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0312-y