Abstract
The prognosis of patients with cholangiocarcinoma historically has been poor, even after surgical resection. Although data from some single-institution series indicate improvement over historical results, survival after surgical therapy for cholangiocarcinoma has not been investigated in a population-based study. We used the Surveillance, Epidemiology, and End Results database to identify patients who underwent surgery for cholangiocarcinoma from 1973 through 2002. Multivariate modeling of survival after surgery for intrahepatic cholangiocarcinoma showed an improvement in survival only within the last decade studied, resulting in a cumulative 34.4% improvement in survival from 1992 through 2002. In contrast, multivariate modeling of survival after surgery for extrahepatic cholangiocarcinoma revealed a 23.3% increase in adjusted survival per each decade studied, resulting in a cumulative 53.7% improvement from 1973 through 2002. We conclude that survival after surgery for extrahepatic cholangiocarcinoma has dramatically improved since 1973. Patients with intrahepatic cholangiocarcinoma, however, have achieved an improvement in survival largely confined to more recent years. We suggest that these trends are largely caused by developments in imaging technology, improvements in patient selection, and advances in surgical techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cholangiocarcinoma is a malignancy arising from the ductal epithelium of the biliary tree. It is relatively uncommon, accounting for approximately 3% of all gastrointestinal cancers,1 but historically it has carried a very poor prognosis. Cholangiocarcinomas are classified by location as either intrahepatic or extrahepatic, and extrahepatic cholangiocarcinomas are often subclassified into those involving the hepatic duct bifurcation versus more distal lesions.2 Temporal trends in the population-based survival of patients diagnosed with cholangiocarcinoma have been studied, but in limited detail. For intrahepatic cholangiocarcinoma (ICC), the 5-year survival has not changed significantly and has remained below 5% from 1975 to 1999.3 In contrast, the 5-year survival of patients with extrahepatic cholangiocarcinoma (ECC) increased from 11.7% in 1973–1977 to 15.1% in 1983–1987.4 These figures represent the aggregate prognosis of all patients with cholangiocarcinoma, most of whom are unresectable at presentation.5 Importantly, they may not accurately describe the outcomes of those patients who receive surgical therapy. Trends in survival after surgical therapy for cholangiocarcinoma have not been investigated in a population-based study.
Data on long-term survival of patients after surgical resection are limited to single-institution case series. Reported 5-year survival rates in recent surgical series (irrespective of margin status) vary widely, from 17 to 40% for ICC6–14 and from 9 to 41% for ECC.10,14–27 These single-institution data may not offer generalizable information and may not reflect outcomes in the general population. To determine whether there have been improvements in survival after surgery for cholangiocarcinoma on a population level, we investigated trends in the survival of patients undergoing cancer-directed surgery for both ECC and ICC over the last 30 years using the Surveillance, Epidemiology, and End Results (SEER) database.
Methods
This study was a retrospective analysis of prospectively collected data from the SEER database maintained by the National Cancer Institute.28 The SEER database began in 1973 with data from seven cancer registries and today includes data from 17 cancer registries, representing 26.2% of the United States population. Compared to the general U.S. population, the SEER population is slightly more urban and has a slightly higher percentage of foreign-born individuals. Available data include patient demographics (e.g., age, gender, race), tumor data (histology, grade), SEER stage of disease, use of cancer-directed surgery, use of radiation therapy, and attributes of the patient’s county of residence (e.g., urban-rural continuum code). Other data elements (e.g., American Joint Committee on Cancer staging, details of surgical therapy, tumor size, lymph node involvement) are consistently available only in more recent time periods.
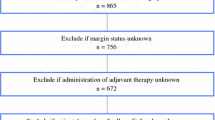
Patients with cholangiocarcinoma were identified by the International Classification of Diseases for Oncology (ICD-O-3)29 topography and histology codes that were chosen to minimize the possibility of inadvertently including metastatic lesions or non-cholangiocarcinoma hepatobiliary malignancies in the analysis (Table 1). Klatskin tumors that were coded as intrahepatic tumors were reclassified as extrahepatic, accounting for a known problem that erroneously cross-references Klatskin tumors to the topography code for intrahepatic tumors.30 The ICD-O-3 coding system does not allow perihilar tumors to be reliably distinguished from other tumors of the extrahepatic biliary tree, so all extrahepatic tumors were analyzed as one category. Only patients who were actively followed were included, and all patients diagnosed at autopsy or by death certificate were excluded. Those patients who underwent cancer-directed surgical procedures were identified using site-specific surgery codes 10–90 or surgery of primary site codes 10–90.
For descriptive analyses, crude survival statistics for ECC and ICC were generated using the Kaplan–Meier method31 and were then adjusted for expected death rates in SEER*Stat version 6.2.4 (Surveillance Research Program, National Cancer Institute, Silver Spring, MD). The resulting relative survival curves were compared using log-likelihood statistics.32 Differences in patient and tumor characteristics between decades were evaluated by Pearson’s chi-squared test or Cuzick’s nonparametric test for trend,33 as appropriate. Trends in survival were then further explored using Cox proportional hazards models.34 The SEER database codes cases with less than 1-month survival time as having zero survival time, an apparent truncation that would bias the survival analysis. To avoid this potential bias, we redefined survival times for these cases (81/2,107 for ECC and 15/591 for ICC), as 0.1 months. The variables considered in our analysis were age, gender, race, marital status at diagnosis, rural versus urban area of residence, SEER historic tumor stage, tumor grade, receipt of radiation therapy, SEER registry, and year of diagnosis.
Univariate and multivariate modeling of survival were performed using Cox proportional hazards models using the Efron method for ties. The appropriate functional forms of covariates were determined during exploratory data analysis using Martingale residuals. Entry of covariates into the multivariate models was generally determined by statistical significance in the univariate Cox models (using the likelihood ratio test). An exception was the variable for rural area of residence, which was force-entered in the model for ICC because of its significance in the multivariate model for ECC. Extensive sensitivity analyses of the final models were performed using likelihood ratio tests, Akaike information criteria, and stratified analyses to ensure that important variables or interaction terms had not been erroneously excluded. Adherence to the proportional hazards assumption was confirmed by Schoenfeld residuals and log–log plots.
The multivariate analyses were performed both by using complete records only and by including missing categories for covariates with missing data >5%. For ICC, these two approaches did not agree, so missing data were dealt with using multiple imputation.35–37 For ECC, these two approaches produced the same significant variables with <10% difference in the hazard ratios, so the results of the simpler model are reported. The final models included 591 of 591 ICC cases (with multiple imputation) and 1,529 of 2,107 ECC cases (using complete records only).
All tests of statistical significance were two-sided, and statistical significance was established at α = 0.05. Statistical analysis was performed using Stata/SE 9.2 for Windows (StataCorp, College Station, TX), and multiple imputation was performed using the ICE module for Stata.38 This study was approved by the Johns Hopkins University School of Medicine Institutional Review Boards.
Results
Our selection criteria identified 591 patients with ICC and 2,107 patients with ECC who were diagnosed from 1973 through 2002 and underwent a cancer-directed surgical procedure. The range of follow-up times was 0–323 months for ICC and 0–321 months for ECC. Five-year relative survival (RS) over the entire period of study was 20.6% (crude survival 17.7%) for ICC and 20.5% (crude survival 17.1%) for ECC. There was no significant difference in overall relative survival (RS) between ECC and ICC (P = 0.221) (Fig. 1).
Intrahepatic Cholangiocarcinoma
The only statistically significant trend in ICC patient and tumor characteristics (Table 2) was an increase in the proportion of male patients over this period (P = 0.046). Because the type of cancer-directed surgery was not specified for a high proportion of patients (122 of 591), we were not able to analyze trends in the type of surgical procedure performed. Comparison of ICC survival between decades (Fig. 2) showed no significant difference between 1973–1982 and 1983–1992 (P = 0.547), but survival improved between 1983–1992 and 1993–2002 (P = 0.015). Because there was no difference in survival between the first two decades, and because there were only 42 patients in the first decade, we combined the first two decades in further analysis. Comparison of ICC survival in 1973–1992 compared against 1993–2002 showed a significant improvement (P = 0.003), with 5-year RS rising from 16.5% to 22.9%. Comparisons of survival curves by stage at diagnosis (Fig. 3) were all highly significant (P < 0.001). As expected, more advanced disease conferred a worse prognosis, with 5-year RS of 37.4% for localized disease, 14.7% for regional disease, and 5.3% for distant disease.
Although our exploratory univariate analysis revealed better survival for patients undergoing surgery for ICC in the last decade versus previous decades, this benefit did not persist in initial multivariate models that adjusted for demographics, tumor characteristics, and receipt of radiation therapy. Having found no improvement in the aggregate survival of patients diagnosed in 1993–2002 versus 1973–1992, we explored the possibility that there has nevertheless been more recent incremental improvement by focusing on the year-to-year changes after 1992. Univariate Cox proportional hazards analysis for ICC (Table 3) showed the following variables to be significantly associated with decreased survival (P value for likelihood ratio test, percent of data missing): age per year over 80 years (P = 0.001, 0%), tumor stage (P < 0.001, 7.6%), tumor grade (P = 0.017, 34.4%), and year of diagnosis per year after 1992 (P < 0.001, 0%). These variables, together with rural area of residence (0.2% missing), were entered into the multivariate model for ICC. This approach revealed a year-to-year improvement in ICC survival over the years 1992–2002 that remained significant in multivariate analysis. In the final model of ICC survival (Table 3), age per year over 80 years and stage at diagnosis were strong predictors of worse survival, but the effect of tumor grade was not statistically significant. This analysis demonstrated a significant year-to-year improvement in ICC survival after 1992, corresponding to a cumulative 34.4% increase in adjusted survival from 1992 through 2002.
Extrahepatic Cholangiocarcinoma
Several ECC patient and tumor characteristics changed significantly over the period of this study (Table 4). On average, patients in later decades tended to be older (P = 0.021), and fewer came from rural areas (P < 0.001). They also had higher stages of disease (P = 0.008) and more aggressive tumor histology (P < 0.001). There was no significant association between stage of disease and rural area of residence. The proportion of patients surviving less than 1 month after diagnosis (a surrogate marker of perioperative mortality) decreased over the three decades studied from 6.7% to 2.7% (P < 0.001). Because the type of cancer-directed surgery was not specified for a high proportion of patients (771 of 2,107), we were not able to analyze trends in the type of surgical procedure performed.
Higher proportions of patients in later decades received radiation therapy (P < 0.001). Receipt of radiation therapy was not significantly associated with tumor grade, but it was associated with tumor stage. Overall, 31.1% of patients with regional disease received radiation therapy, significantly more than those with localized (21.8%) or distant (22.0%) disease (P < 0.001). Stratification by decade consistently demonstrated that patients with regional disease had the highest rate of radiation therapy, but this difference was statistically significant only in 1993–2002, when 39.2% of patients with regional disease received radiation therapy versus 23.6% of those with localized and 27.9% of those with distant disease (P < 0.001). Stratification by stage showed that patients with every stage of disease were more likely to receive radiation therapy in later decades.
Comparison of ECC survival between decades (Fig. 4) showed significant improvements between 1973–1982 and 1983–1992 (P = 0.004) and again between 1983–1992 and 1993–2002 (P = 0.001). These improvements corresponded to 5-year RS of 14.4%, 19.1%, and 24.5% in the three decades studied. Comparisons of survival curves by stage at diagnosis (Fig. 5) were all highly significant (P < 0.001). As with ICC, more advanced disease conferred a worse prognosis, with 5-year RS of 33.7% for localized disease, 17.7% for regional disease, and 16.6% for distant disease.
Univariate Cox proportional hazards analysis for ECC (Table 5) showed the following variables to be significantly associated with decreased survival (P value for likelihood ratio test, percent of data missing): age per year over 60 years (P < 0.001, 0%), male gender (P = 0.007, 0%), marital status (P = 0.006, 5.7%), rural area of residence (P < 0.001, 1.4%), tumor stage (P < 0.001, 3.2%), tumor grade (P < 0.001, 22.7%), radiation therapy (P = 0.003, 0%), and year of diagnosis per year after 1973 (P < 0.001, 0%). These variables were entered into the multivariate model for ECC. In the final model of ECC survival (Table 5), age over 60 years and rural area of residence were strong predictors of worse survival. Advanced stage of disease and histological de-differentiation also conferred a worse prognosis. Gender, marital status, and radiation therapy did not show statistically significant effects on survival in the multivariate model. In sharp contrast to ICC, there was a dramatic improvement in adjusted ECC survival over the entire 30-year period studied, corresponding to a 23.3% increase in adjusted survival per decade and a cumulative 53.7% improvement from 1973 through 2002. A sensitivity analysis that restricted the cohort to those patients surviving at least 1 month did not yield qualitatively different conclusions, suggesting that the observed improvement was not solely a result of decreasing perioperative mortality.
Discussion
Historically, analyses of patient survival after surgery for cholangiocarcinoma have been restricted to single-institution series. Although such institutional data may offer great depth of clinical information, they may be limited by poor generalizability and potential selection bias. In this population-based study, we analyzed long-term survival after cancer-directed surgery for cholangiocarcinoma using data derived from a national cancer registry. We found 5-year crude survival rates of 17.7% for ICC and 17.1% for ECC over the period 1973–2002. For ICC, recent single-institution surgical series have reported 5-year crude survival rates of 17–40%.6–14 Even the highest 5-year crude survival rate for ICC in our analysis, 19.7% in the decade 1993–2002, falls below all except one of these single-institution rates.6 For ECC (including perihilar tumors), recent single-institution surgical series have reported 5-year crude survival rates of 9–41%.10,14–27 Again, our analysis found 5-year crude survival rates for ECC that were at the lower end of this spectrum. These results are not surprising, as the results we report are not restricted to specialized centers, and single-institution series are susceptible to publication bias.
Our analysis offers a more generalizable assessment of the progress made in the surgical therapy of cholangiocarcinoma. In particular, we defined cancer-directed surgery as it is defined in the SEER database, including a range of procedures from cryoablation and enucleation to hepatectomy and pancreaticoduodenectomy. Some of these less aggressive practices might not be considered oncologically adequate at specialized centers, which may also explain the poorer survival seen in this analysis as compared to single-institution series. Importantly, however, our analysis reflects the full range of practice patterns in the treatment of cholangiocarcinoma in the United States, not just the results of specialized centers employing more aggressive surgical approaches.
We did not find an improvement in ICC survival until the last decade studied. During the period from 1992 through 2002, there was a cumulative 34.4% increase in adjusted survival after surgery. Unfortunately, the SEER data do not allow us to specifically identify the factors responsible for this improvement, but based on the substantial collective experience with cholangiocarcinoma at our institution there are several factors that we believe have likely played an important role. The improvement in ICC survival may reflect improving patient selection over time, likely as the result of improvements in imaging technology, such as multidetector computed tomography, that allow better preoperative assessments of resectability. Also, improvements in the safety of hepatic resection39 have likely led to the increased utilization of aggressive hepatic resection for ICC, contributing to improved oncologic results and increased long-term survival. Unfortunately, details of the type of surgical resection in the SEER database are inconsistently available, and margin status information is absent, preventing us from further investigating these hypotheses.
We noted improvements in ECC survival over the entire 30-year time period studied, corresponding to a 23.3% increase in adjusted survival per decade and a cumulative 53.7% improvement from 1973 through 2002. As with ICC, the improvement in ECC survival may reflect improvements in preoperative imaging and patient selection, as well advances in surgical techniques. Decreases in the morbidity and mortality of complex hepatobiliary procedures may have expanded the use of such operations in ECC patients. For example, advances in the safety of pancreaticoduodenectomy are well documented.40 Technical advances may also have resulted in a higher proportion of margin-negative resections, resulting in fewer patients undergoing inadequate resections. For example, concomitant hepatic resection for hilar cholangiocarcinoma has recently gained popularity as a strategy to achieve adequate margins.14,19,22,27 It is possible that the increased use of hepatic resection in hilar cholangiocarcinoma has resulted in better oncologic results. Again, the SEER data do not permit the identification of such specific reasons for the observed trends.
The proportion of surgical patients surviving less than 1 month after diagnosis of ECC has decreased from 6.7% in the first decade to 2.7% in the last. Although these figures are not, strictly speaking, measures of 30-day surgical mortality, this decrease in 1-month survival likely indicates decreasing perioperative mortality. This interpretation assumes that the interval from diagnosis to surgery has not lengthened over the last three decades. More likely, this interval has either not changed or has shortened, which would underestimate perioperative mortality in the early years and overestimate it in the later years, resulting in a bias toward the null. Furthermore, our analysis demonstrates that an improvement in long-term ECC survival persists even when the effect of decreasing perioperative mortality is removed.
Despite these overall improvements, patients from rural areas who undergo surgery for ECC experience a 43% decrease in adjusted survival compared with those who live in more metropolitan areas. Rural patients did not, in fact, present with more advanced disease, suggesting that differences in survival were not related to delayed diagnosis. Instead, such differences may be related to discrepancies in access to specialized care or adequate follow-up, although we note that a rural area of residence does not necessarily imply treatment at a rural hospital. Another possible explanation is that the effect of rural area of residence was confounded by socioeconomic status. Socioeconomic data are only available in later years of the SEER database, so we were unable to test this hypothesis.
The use of radiation therapy in ECC patients increased from 10.8% in the first decade to 34.7% in the last. Patients with regional disease were especially likely to receive radiation therapy. Most prior studies show that adjuvant radiation does not confer a survival benefit in cholangiocarcinoma,41–43 although some evidence suggests that higher doses of radiation and concurrent chemotherapy may be of benefit.44,45 In the present study, the increasing use of adjuvant radiation therapy demonstrated no independent survival benefit, underscoring the need for rigorous prospective evaluation of its efficacy in resected patients.
This study is limited primarily by the depth of surgical data in the SEER database. In addition to the lack of margin status data, the level of detail and completeness of data on tumor size, lymph node involvement, and details of resection have varied since 1973, such that comparisons that account for these factors over all 30 years are not possible. Although we did have some data on radiation therapy, we did not have any information on the use of chemotherapy. Finally, the ICD-O-3 coding scheme used in the SEER database did not allow us to separate perihilar tumors from other ECC, limiting comparisons with other studies.
Alternative explanations for the improvements we describe include the possibilities of lead time bias and stage migration. Even today, just as 30 years ago, patients with cholangiocarcinoma are typically diagnosed only after they develop symptoms of obstructive jaundice. Lead time bias is therefore unlikely to play a role in explaining these findings. Stage migration may have also played a role, but because we focused on a surgical population we would expect that patients would be appropriately upstaged at the time of surgery, even if their preoperative workups did not reveal the full extent of their disease. This would have resulted in more uniform coding of stage than in a nonsurgical population, for whom stage migration would be a more important issue.
In conclusion, this population-based analysis demonstrates that survival after surgery for extrahepatic cholangiocarcinoma has dramatically improved since 1973. Patients with intrahepatic cholangiocarcinoma, however, have achieved an improvement in survival largely confined to more recent years. We suggest that improvements in imaging technology, patient selection, and surgical techniques are largely responsible for these improvements. The discrepancies between the survival rates we report and those reported in single-institution series deserve further investigation to determine whether they are the result of publication bias, patient selection, disease characteristics, or disparities in access to adequate care. Finally, these population-based survival statistics demonstrate that extrahepatic and intrahepatic cholangiocarcinoma continue to carry very poor prognoses. Despite incremental advances in the surgical therapy of these biliary tract malignancies over the last three decades, there remains much opportunity for improvement.
References
Vauthey JN, Blumgart LH. Recent advances in the management of cholangiocarcinomas. Semin Liver Dis 1994;14:109–114.
Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, Hruban RH, Lillemoe KD, Yeo CJ, Cameron JL. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg 1996;224:463–473; discussion 473–475.
Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis 2004;24:115–125.
Carriaga MT, Henson DE. Liver, gallbladder, extrahepatic bile ducts, and pancreas. Cancer 1995;75:171–190.
Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet 2005;366:1303–1314.
Pichlmayr R, Lamesch P, Weimann A, Tusch G, Ringe B. Surgical treatment of cholangiocellular carcinoma. World J Surg 1995;19:83–88.
Jan YY, Jeng LB, Hwang TL, Wang CS, Chen MF, Chen TJ. Factors influencing survival after hepatectomy for peripheral cholangiocarcinoma. Hepatogastroenterology 1996;43:614–619.
Casavilla FA, Marsh JW, Iwatsuki S, Todo S, Lee RG, Madariaga JR, Pinna A, Dvorchik I, Fung JJ, Starzl TE. Hepatic resection and transplantation for peripheral cholangiocarcinoma. J Am Coll Surg 1997;185:429–436.
Lieser MJ, Barry MK, Rowland C, Ilstrup DM, Nagorney DM. Surgical management of intrahepatic cholangiocarcinoma: A 31-year experience. J Hepatobiliary Pancreat Surg 1998;5:41–47.
Madariaga JR, Iwatsuki S, Todo S, Lee RG, Irish W, Starzl TE. Liver resection for hilar and peripheral cholangiocarcinomas: A study of 62 cases. Ann Surg 1998;227:70–79.
Valverde A, Bonhomme N, Farges O, Sauvanet A, Flejou J, Belghiti J. Resection of intrahepatic cholangiocarcinoma: A western experience. J Hepatobiliary Pancreat Surg 1999;6:122–127.
Inoue K, Makuuchi M, Takayama T, Torzilli G, Yamamoto J, Shimada K, Kosuge T, Yamasaki S, Konishi M, Kinoshita T, Miyagawa S, Kawasaki S. Long-term survival and prognostic factors in the surgical treatment of mass-forming type cholangiocarcinoma. Surgery 2000;127:498–505.
Weber SM, Jarnagin WR, Klimstra D, DeMatteo RP, Fong Y, Blumgart LH. Intrahepatic cholangiocarcinoma: Resectability, recurrence pattern, and outcomes. J Am Coll Surg 2001;193:384–391.
Deoliveira ML, Cunningham SC, Cameron JL, Kamangar F, Winter JM, Lillemoe KD, Choti MA, Yeo CJ, Schulick RD. Cholangiocarcinoma: Thirty-one-year experience with 564 patients at a single institution. Ann Surg 2007;245:755–762.
Sugiura Y, Nakamura S, Iida S, Hosoda Y, Ikeuchi S, Mori S, Sugioka A, Tsuzuki T. Extensive resection of the bile ducts combined with liver resection for cancer of the main hepatic duct junction: A cooperative study of the keio bile duct cancer study group. Surgery 1994;115:445–451.
Su CH, Tsay SH, Wu CC, Shyr YM, King KL, Lee CH, Lui WY, Liu TJ, P'eng FK. Factors influencing postoperative morbidity, mortality, and survival after resection for hilar cholangiocarcinoma. Ann Surg 1996;223:384–394.
Nagino M, Nimura Y, Kamiya J, Kanai M, Uesaka K, Hayakawa N, Yamamoto H, Kondo S, Nishio H. Segmental liver resections for hilar cholangiocarcinoma. Hepatogastroenterology 1998;45:7–13.
Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Shimizu Y, Kato A, Nakamura S, Omoto H, Nakajima N, Kimura F, Suwa T. Aggressive surgical approaches to hilar cholangiocarcinoma: Hepatic or local resection? Surgery 1998;123:131–136.
Kosuge T, Yamamoto J, Shimada K, Yamasaki S, Makuuchi M. Improved surgical results for hilar cholangiocarcinoma with procedures including major hepatic resection. Ann Surg 1999;230:663–671.
Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, Wex C, Lobeck H, Hintze R. Extended resections for hilar cholangiocarcinoma. Ann Surg 1999;230:808–818; discussion 819.
Bortolasi L, Burgart LJ, Tsiotos GG, Luque-De Leon E, Sarr MG. Adenocarcinoma of the distal bile duct. A clinicopathologic outcome analysis after curative resection. Dig Surg 2000;17:36–41.
Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BSJ, Youssef BAM, Klimstra D, Blumgart LH. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 2001;234:507–517; discussion 517–519.
Yoshida T, Matsumoto T, Sasaki A, Morii Y, Aramaki M, Kitano S. Prognostic factors after pancreatoduodenectomy with extended lymphadenectomy for distal bile duct cancer. Arch Surg 2002;137:69–73.
Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, Katoh H. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: Results of a prospective study. Ann Surg 2004;240:95–101.
Rea DJ, Munoz-Juarez M, Farnell MB, Donohue JH, Que FG, Crownhart B, Larson D, Nagorney DM. Major hepatic resection for hilar cholangiocarcinoma: Analysis of 46 patients. Arch Surg 2004;139:514–523; discussion 523–525.
Nishio H, Nagino M, Nimura Y. Surgical management of hilar cholangiocarcinoma: The Nagoya experience. HPB 2005;7:259–262.
Liu CL, Fan ST, Lo CM, Tso WK, Lam CM, Wong J. Improved operative and survival outcomes of surgical treatment for hilar cholangiocarcinoma. Br J Surg 2006;93:1488–1494.
National Cancer Institute, DCCPS, Surveillance Research Program, Cancer Statistics Branch. Surveillance, epidemiology, and end results (SEER) program (http://www.seer.cancer.gov) SEER*Stat database: Incidence, SEER 17 regs public-use, Nov 2005 sub (1973–2003 varying), linked to county attributes, total U.S., 1969–2003 counties. Released April 2006, based on the November 2005 submission.
Fritz AG. International Classification of Diseases for Oncology: ICD-O, 3rd ed. Geneva: World Health Organization, 2000.
Welzel TM, McGlynn KA, Hsing AW, O’Brien TR, Pfeiffer RM. Impact of classification of hilar cholangiocarcinomas (klatskin tumors) on the incidence of intra- and extrahepatic cholangiocarcinoma in the united states. J Natl Cancer Inst 2006;98:873–875.
Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457–481.
Brown CC. The statistical comparison of relative survival rates. Biometrics 1983;39:941–948.
Cuzick J. A wilcoxon-type test for trend. Stat Med 1985;4:87–90.
Cox DR. Regression models and life-tables. J R Stat Soc B 1972;34:187–220.
Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley, 1987.
Rubin DB, Schenker N. Multiple imputation in health-care databases: An overview and some applications. Stat Med 1991;10:585–598.
Schafer JL. Multiple imputation: A primer. Stat Methods Med Res 1999;8:3–15.
Royston P. Multiple imputation of missing values: Update of ICE. Stat J 2005;5:527–536.
Kooby DA, Jarnagin WR. Surgical management of hepatic malignancy. Cancer Invest 2004;22:283–303.
Cameron JL, Riall TS, Coleman J, Belcher KA. One thousand consecutive pancreaticoduodenectomies. Ann Surg 2006;244:10–15.
Pitt HA, Nakeeb A, Abrams RA, Coleman J, Piantadosi S, Yeo CJ, Lillemore KD, Cameron JL. Perihilar cholangiocarcinoma. postoperative radiotherapy does not improve survival. Ann Surg 1995;221:788–797; discussion 797–798.
Hejna M, Pruckmayer M, Raderer M. The role of chemotherapy and radiation in the management of biliary cancer: A review of the literature. Eur J Cancer 1998;34:977–986.
Khan SA, Davidson BR, Goldin R, Pereira SP, Rosenberg WM, Taylor-Robinson SD, Thillainayagam AV, Thomas HC, Thursz MR, Wasan H, British Society of Gastroenterology. Guidelines for the diagnosis and treatment of cholangiocarcinoma: Consensus document. Gut 2002;51(6):7–9.
Alden ME, Mohiuddin M. The impact of radiation dose in combined external beam and intraluminal ir-192 brachytherapy for bile duct cancer. Int J Radiat Oncol Biol Phys 1994;28:945–951.
Czito BG, Anscher MS, Willett CG. Radiation therapy in the treatment of cholangiocarcinoma. Oncology (Williston Park) 2006;20:873–884; discussion 886–888, 893–895.
Acknowledgements
Dr. Nathan is supported by the Johns Hopkins-NIH Clinical Research Scholars Program (NIH K12RR017627). We are indebted to Richard E. Thompson, Ph.D., and Dorry L. Segev, M.D., for their advice on statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCUSSION
Bryan M. Clary, M.D. (Durham, NC): This is another very nice paper. I must admit when I read reports of this nature, I am not always sure what to do with them. Number one, I would like to commend you on your manuscript. This type of a study is all about the statistics, and in your manuscript’s methods section you very eloquently state the methods that you use, and you also include a number of very relevant references to help guide individuals such as myself as to what the statistics mean.
Again, the problem is what you gain from this. You in general get a look at how we are doing in certain eras, and trying to come up with the explanations as to why that is, is really pure speculation. One of the main concerns I have with the intrahepatic cholangio population is just the definition as to what is an intrahepatic cholangiocarcinoma during different eras. In eras past, including the ’70s and ’80s, this was essentially adenocarcinoma of unknown primary in the liver, and really it was a diagnosis of exclusion for cytokeratin staining was not as sophisticated as it is now. And so I would venture to guess that one of the problems that you have in this series is that a large proportion of your intrahepatic cholangiocarcinomas were adenocarcinomas metastatic from other sites such as occult pancreatic cancers which were very common with poor imaging back then, and possibly even gastric cancers and lung cancers, et cetera. I wonder if you might make some comment to that specific issue.
The thing that clearly isn’t brought out in this, which you already mentioned, is that of chemotherapy and the issue about rural populations not doing as well. Again, that explanation may not be a surgical issue but it instead that in their follow-up they don’t have medical oncologists who were offering chemotherapy, et cetera. But again, those types of things are pure speculation.
Hari Nathan, M.D. (Baltimore, MD): Dr. Clary, thank you very much for your review of our manuscript and your insightful questions. Your first question was whether the intrahepatic cholangiocarcinomas are truly cholangiocarcinomas. We specifically designed our selection criteria with that issue in mind. The SEER data allow the identification of tumors based on two codes: one is a topography code indicating the location of the tumor and the other is a histology code indicating the pathological diagnosis. For tumors that were located in the liver, the intrahepatic cholangiocarcinomas, we specifically excluded adenocarcinomas that were not otherwise specified and other lesions that we could not specifically identify as being cholangiocarcinomas. We were less stringent, for example, in the extrahepatic biliary tree, where we might accept a histological diagnosis of adenocarcinoma, not otherwise specified. But in the liver or at the ampulla we were much more strict about requiring a specific histological diagnosis of cholangiocarcinoma. So we feel very comfortable that we have excluded metastatic malignancies and other adenocarcinomas not arising from the bile ducts.
With regard to chemotherapy and rural patients, you are correct in pointing out that one of the weaknesses of the study is that we just don’t have the depth of data in this database that would be required to specifically identify what the reasons for the improvements are. But I think this study provides two important pieces of information.
One, it gives us a sense as to the generalizability of the results that we see reported from single institutions. In terms of prognostication for patients and to get a general sense of how we are doing in the country as a whole, it is important to have that reality check of not exclusively relying on reports from specialized centers to guide our impression of how we are doing across the entire country.
And the other contribution is that it points to a direction for future research. There are other data that are available that may help us to identify why exactly, for example, rural patients with ECC have worse survival. The SEER-Medicare data, for example, which we are currently trying to acquire, do include information on chemotherapy receipt. So as we investigate further why these disparities do exist in patient outcomes, not just with cholangiocarcinoma but with a variety of malignancies, I think that this study and others like it give us a starting point. In future work, we hope to move from describing the differences to identifying the reasons for these disparities and actually trying to do something about them.
Thanks again for your comments and questions.
Rights and permissions
About this article
Cite this article
Nathan, H., Pawlik, T.M., Wolfgang, C.L. et al. Trends in Survival after Surgery for Cholangiocarcinoma: A 30-Year Population-Based SEER Database Analysis. J Gastrointest Surg 11, 1488–1497 (2007). https://doi.org/10.1007/s11605-007-0282-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0282-0