Abstract
Gastrojejunostomy stricture after Roux-en-Y gastric bypass occurs in 3 to 27% of morbidly obese patients in the USA. We questioned whether preoperative patient characteristics, including demographic attributes and comorbid disease, might be significant factors in the etiology of stricture. In this study from November 2001 to February 2006 (51 months), at a high-volume bariatric center, of the 1,351 patients who underwent laparoscopic gastric bypass, 92 developed stricture (6.8%). All but two were treated successfully by endoscopic dilation. All patients stopped nonsteroidal anti-inflammatory medications 2 weeks prior to surgery and did not restart them. The operative procedure included the use of a 21-mm transoral circular stapler to create the gastrojejunostomy; the Roux limb was brought retrogastric, retrocolic. In an effort to reduce our center’s stricture rate, late in the study, U-clips used at the gastrojejunostomy were replaced by absorbable sutures, and postoperative H2 antagonists were added to the treatment protocol. The change to absorbable polyglactin suture proved to be significant, resulting in a lower stricture rate. The addition of H2 antagonists showed no significant effect. Following the retrospective review of the prospective database, univariate and multivariate logistic regression analyses identified factors associated with the development of stricture. Gastroesophageal reflux disease and age were each shown to be statistically significant independent predictors of stricture following laparoscopic gastric bypass.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery, particularly Roux-en-Y gastric bypass (RYGB), has been proven safe1,2 and effective in achieving long-term weight loss,3,4 comorbidity reduction,3,5 and enhancement of quality of life.6 Since its introduction by Wittgrove et al. in 1994,7 laparoscopic Roux-en-Y gastric bypass (LRYGB) has been shown to be as reliable as open RYGB8–10 and less traumatic, requiring a briefer recovery time and shorter duration of stay.11 It is effective in achieving comparable weight loss at 1 year3,12–15 and is successful in reducing the comorbidities of morbid obesity.3,9,13 Laparoscopic RYGB has surpassed other weight-loss methods for the morbidly obese in frequency of use in the USA.14
Laparoscopic RYGB is a technically demanding procedure with a lengthy learning curve of approximately 100 cases.16,17 Gastrojejunostomy stricture following RYGB has been reported variously in 3 to 27% of patients.12,16–19 Actual incidence of this complication is a function of the accuracy of its diagnosis and reporting19 and has been shown to be relative to operative technique and surgeon experience.20 Other known etiologies of stricture following LRYGB are tension on the anastomosis, foreign body reaction, technical error in creation of the anastomosis, marginal ulcer, and leak with associated scarring.19
In 2003, Perugini and colleagues published an analysis of preoperative predictors of complications.20 They reported a 14.4% rate of gastrojejunostomy stricture (N = 27/188), greater than half of all complications. With multivariate analysis by stepwise logistic regression, they found that surgeon experience was the most significant predictor of complications in general (not of stricture specifically) and that sleep apnea and hypertension were also significant independent predictors of complications.20 Perugini et al. cautioned that the factors they identified (experience, sleep apnea, hypertension) as predictive of complications in general might, in fact, “ be specific for the complication of gastrojejunal stenosis”.20 Our study took up this question and, by univariate and multivariate logistic regression, analyzed preoperative predictors specifically for stricture.
Patients and Methods
Patients
A consecutive series of morbidly obese patients underwent LRYGB between November 12, 2001, and February 28, 2006 (51 months), in a dedicated, community-based, bariatric program awarded Center-of-Excellence status by the Surgical Review Corporation in 2005.
Institutional review board approval and informed consent were obtained prior to prospective data collection. In a retrospective analysis, preoperative patient characteristics, including whether the patient was taking any nonsteroidal anti-inflammatory medications on a chronic basis prior to surgery, were compared for two groups: those who developed gastrojejunostomy stricture (N = 17/92, 6.8%) and those who did not (N = 311/1,259, 93.2%). No patients were excluded from the study.
Patients where tested for Helicobacter pylori and treated if positive. Anti-inflammatory medications were withheld 2 weeks preoperatively and not resumed postoperatively. Procedures were performed by four bariatric surgeons. Stenosis, or stricture, indicated by progressive dysphagia, nausea, and vomiting, was diagnosed by endoscopy.
Surgical Technique
The procedure was performed using the transoral end-to-end anastomotic (EEA) technique similar to the Wittgrove technique.10 Using a Veress needle to an intra-abdominal pressure of 15 mm Hg, abdominal insufflation was performed. The patient was placed supine, in the reverse Trendelenburg position, and six abdominal trocars were introduced. The angle of His was dissected, and a 15-ml balloon was passed transorally and placed at the esophagogastric junction. The lesser sac was entered just below the balloon on the lesser curve of the stomach. A 15- to 20-ml gastric pouch was created with the Endo GIA 45-mm stapler (Ethicon Endo-Surgery, Cincinnati, OH, USA), using an average of three firings. A guidewire was introduced through the anterior abdominal wall and an endoscope was passed transorally. Cautery was used to pass the snare through the pouch and grasp the guidewire. The anvil of the 21-mm EEA Stealth stapler (Ethicon Endo-Surgery) was attached to the guidewire and brought down through the mouth. The ligament of Treitz was identified, and, approximately 20 cm distally, the jejunum was divided. A 100-cm Roux limb was created for patients with BMI < 55 kg/m2, and a 150-cm Roux limb was created for patients with BMI ≥ 55 kg/m2. The jejunojejunostomy was stapled side to side, and closed with the Endo GIA stapler. The Roux limb was brought retrocolic, retrogastric through the lesser curve of the stomach. The EEA circular stapler was introduced through the abdominal wall and the gastrojejunostomy was stapled end to end. The posterior wall of the gastrojejuostomy lays on soft tissue that holds the left gastric and vagus nerve and does not need reinforcement. All techniques for reinforcing the gastrojejunostomy were instituted only in the anterior wall of the anastamosis as a second layer. The initial technique was to sew a continuous second layer of the gastrojejunostomy anteriorly with 3–0 polyglactin absorbable suture. The angle is often technically demanding. In October 2005, the procedure was modified to one in which the gastrojejunostomy was oversewn with two Nitinol “U” clips that revert to preformed circular memory when placed, without additional suture. In October of 2005, these U-clips were replaced with two interrupted 3–0 polyglactin absorbable sutures. Finally, in January 2006, the addition of H2 antagonists for 90 days to the postoperative regimen was made. These technical changes were instituted in an attempt to lessen the stricture rate, which is followed monthly in our database.
Patients who experienced persistent postoperative nausea, vomiting, and intolerance to solid food were referred for upper gastrointestinal studies, followed by referral to the gastroenterologist for upper endoscopy. Patients with stricture were treated endoscopically with balloon dilation to a maximum of 15 mm.
Statistical Methods
Patient data were collected prospectively and included preoperative patient demographics and comorbidities, as well as postoperative complications extracted to identify potential influences on stricture rates. Variables included in the univariate logistic regression analysis are listed in Table 1.
The SPSS™ software package (version 14.0, SPSS, Chicago, IL, USA) was used to perform all statistical analyses. Statistical significance was set at P < 0.05. Binary logistic regression analysis was used in both univariate and multivariate modeling to identify independent preoperative variables associated with the development of gastrojejunostomy stricture following LRYGB surgery. Univariate analysis using logistic regression was applied to identify significant associations with the dichotomous outcome variable (stricture). For comparison, Pearson chi-square test for categorical variables and Student’s t test for continuous variables were used. A priori preoperative factors of research interest (P < 0.21), as well as those found to be significantly associated with stricture (P < 0.05), were entered into multivariate analysis using forward stepwise logistic regression. Likelihood ratio tests were used for variable selection.
In the initial analysis of preoperative characteristics by univariate logistic regression, age, number of comorbidities, number of medications, BMI, fasting blood sugar, HbA1C, and previous abdominal surgeries were classified as continuous variables. With the exception of sex and ethnicity (dichotomized to male/female and Caucasian/non-Caucasian, respectively), all remaining variables were dichotomized (yes/no). In the final multivariate forward stepwise logistic regression model, both age and BMI were redefined as categorical variables: age was coded to reflect four levels (≤35, 36 to 45, 46 to 55, and ≥55 years) and BMI was coded to reflect two levels (<50 and ≥50).
Results
From November 12, 2001, to February 28, 2006 (51 months), 1,351 patients underwent LRYGB at a single institution. Mean preoperative patient age was 44 years, mean BMI was 49 kg/m2, 83% of patients were female, and mean preoperative weight was 305 lb. Patients were predominantly Caucasian (89%); 7% were Hispanic; 3% were African American; and 1% were of Native American, Asian/Pacific, and other ethnicities.
Operative technique was the same in all procedures, namely, a retrocolic, retrogastric, transoral, 21-mm, circular stapled gastrojejunostomy. Mean intraoperative time was 96 min and length of stay averaged 2.8 days; 97.6% of operations were accomplished laparoscopically and 2.4% were conversions to open procedures. There were two reoperations with revision of the gastrojejunostomy in the “stricture group.” The first was in a patient who developed a leak immediately postoperatively and returned to the OR for definitive management. The patient developed a stricture that was not amenable to dilation and, at 7 months, underwent a revision of her gastrojejunostomy. The second patient had a stricture that was dilated to 12–15 mm. Subsequent endoscopy showed no recurrent stricture. She continued to eat very large portions in multiple meals, developing recurrent bezoars that had to be cleared endoscopically. The pouch dilated over time, and even though the gastrojejunostomy was shown to be only large enough to pass an endoscope, we were obliged to revise the pouch to a smaller size. Since that time she has had no further problem with bezoars.
There were no deaths in the stricture group. In the “nonstricture group,” early mortality was 0.2% (two deaths <31 days postoperatively); intermediate mortality, 0.3% (four deaths between 31 and 90 days postoperatively); and late mortality, 0.4% (five deaths >90 days postoperatively). Ninety-two patients (6.8%) were diagnosed with stricture and underwent subsequent endoscopic dilation. Seventeen of 92 stricture patients (18.5%) were on nonsteroidal anti-inflammatory medications prior to surgery, whereas 294 of the 1,259 (23.4%) nonstricture patients were on nonsteroidal anti-inflammatory medications prior to surgery (Table 1). The difference in stricture rates between these two groups was not significant.
Our rate of stricture (92/1,351, 6.8%) was in the range of rates previously reported by Higa et al. (5.3%), Schauer et al. (4.7%), and DeMaria et al. (6.6%), as compiled by Perugini20, at the lower end of the national range of stricture prevalence. Other complications with the highest incidence were cholecystectomy (6.5% stricture group vs 3.0% nonstricture group), small bowel obstruction secondary to internal hernia (4.4 vs 1.9%), and intra-abdominal abscess (3.3 vs 2.0%). In the stricture and nonstricture groups, respectively, leakage occurred in 1.1 and 1.0% of patients, and port site infection occurred in 2.2 and 3.6% of patients. Peripheral neuropathy was 5.4% in the stricture group and 0.5% in the nonstricture group (Table 2).
Mean percent excess weight loss at 1 year following surgery was the same for both groups (−103.1 lb, 82.6% stricture group vs −115.8 lb, 82.0% nonstricture group). Mean numbers of medications were reduced from 4.6 to 1.6 and from 4.2 to 1.5 in the stricture and nonstricture groups, respectively, at the most recent postoperative examination.
By univariate logistic regression analysis, two preoperative characteristics were identified as factors associated significantly (P < 0.05 level) with stricture: gastroesophageal reflux disease (GERD) (P = 0.035) and age (P = 0.039) (Table 1). In addition to GERD and age, BMI (P = 0.202) and gender (P = 0.208) were incorporated into the final multivariate analysis. In the first multivariate model (Table 3), with age defined as a continuous variable, forward stepwise multivariate logistic regression confirmed GERD (P = 0.006, OR = 1.917, CI = 1.200–3.062) and age (P = 0.010, OR = 0.973, CI = 0.953–0.993) to be independent factors associated with stricture. Seventy-two percent of all stricture patients were diagnosed with GERD prior to surgery, and the mean age was 41 years, whereas, in the preoperative nonstricture group, 57% were diagnosed with GERD and the mean age was 44 years.
In the second multivariate model (Table 3), age was classified as a categorical variable to refine our understanding of the impact of age on stricture. Using age group 1 (≤35 years) as the reference category, age groups 2 (36–45 years) and 3 (46–55 years) were significant at the 0.05 level [group 2, P = 0.015 (OR = 0.508, CI = 0.294–0.877); group 3, P = 0.004 (OR = 0.431, CI = 0.244–0.760)]. GERD remained significant (P = 0.005; OR = 1.963, CI = 1.227–3.141).
Three postoperative complications were found to be associated significantly with the presence of stricture by univariate logistic regression, including readmissions within 30 days of surgery (P = 0.000), peripheral neuropathy (P = 0.000), and pneumonia (P = 0.031). The postoperative multivariate model determined readmissions within 30 days of surgery (P = 0.000, OR = 4.381, CI = 2.666–7.197) and peripheral neuropathy (P = 0.000, OR = 11.979, CI = 3.423–41.929) to be statistically significant covariates of stricture.
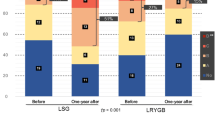
Decreasing our rate of stricture by a protocol change to oversewing the gastrojejunostomy with polyglactin was shown, by chi square analysis, to be a significant decrease, with the rate of 6.8% diminishing to 2.8% (P = 0.028, OR = 0.358, CI = 0.143–0.895). The second protocol adjustment, administration of an H2 antagonist (prevacid) postoperatively, had no effect.
Discussion
Strictures contribute to almost half of all readmissions in the early perioperative period and require instrumentation and rehydration. They can also be associated with the development of a more serious complication, peripheral neuropathy, as is demonstrated by these data.
Specific intraoperative factors (e.g., surgeon experience) associated with stricture have been identified as causal by prior studies. Isolating preoperative factors that may be causally related to stricture may aid in minimizing this complication. In their study, Perugini et al. showed preoperative hypertension and obstructive sleep apnea to be predictive of complications in general; yet, they cautioned that their findings might have been confounded by their high rate of stricture.20 By logistic regression analysis, our study found the variables of GERD and age to be significantly associated with a complication with one of the highest incidences—stricture. Our results are supportive of Perugini’s findings, in that we did not find the same preoperative predictors of complications (hypertension, obstructive sleep apnea) significantly associated with stricture and the overall rate was significantly less.
The odds of developing stricture in patients with preoperative GERD were found to be nearly two times higher than those for patients without GERD. GERD is a known inflammatory condition of the upper gastrointestinal tract that specifically affects the lower esophagus and fundus. If present, this inflammation may predispose patients to more vigorous scarring of the gastrojejunostomy. During the period of the study, we began testing patients preoperatively for H. pylori. Patients who tested positive were treated preoperatively. In general, the micropouch used to create the gastrojejunostomy has been assumed to be almost devoid of acid-producing cells, and the rate of ulceration at the anastomosis at the time of endoscopy is low. It is clear, though, that adding H2 antagonists for 30 days following surgery helps to decrease inflammation, and in addition, the polyglactin stitch may be less inflammatory in nature. Data were insufficient at study summary to demonstrate the statistical significance of administering H2 antagonists; however, we are encouraged by the trend of fewer strictures.
Finding that younger rather than older age was associated with the development of stricture seems clinically counterintuitive. One reason for this is that age affects the small vessels’ ability to provide necessary oxygenation to the anastomosis, and older patients are more likely overall to have diminished capability to oxygenate. In our center, maintenance on oxygen the night of surgery is standard; patients who require continuous positive airway pressure are started in the anesthesia recovery unit and are kept on supplemental oxygen until they can oxygenate in ambulating and resting modes at greater than 92%. However, as stated, in our first multivariate model, older age was shown to be slightly protective with respect to stricture. In the second multivariate model, designed to refine the interpretation of age effects on stricture, we found that the odds of developing stricture in those 35 years or younger were two times greater than those aged 36–45 years, and 2.32 times greater than those aged 46–55 years. The trend of age being protective against stricture leveled off and was not significant in those older than 55 years. More study of this finding is indicated.
Our original assumption that higher rates of central fat distribution in males might place greater tension on the anastomosis predisposing male patients, particularly those with higher BMIs, toward stricture, may be in error. The effect of increased central fat on the anastomosis may not be injurious if meticulous technique is used to ensure a tension-free anastomosis. Also, the ischemic effects of diabetes, sleep apnea, and chronic respiratory disease at the gastrojejunostomy site may be insufficient, in themselves, to cause stricture.
It has been well documented that operative technique can contribute to increased stricture rates. Previous studies have reported fewer strictures with hand-sewn anastomoses than with stapled ones. Some authors have demonstrated that the 25-mm EEA stapler may be associated with fewer strictures that the 21-mm EEA stapler; we have a 6.8% stricture rate with the 21-mm EEA stapler. Further studies of stapling methodologies are warranted.
It has been proposed that stricture rates may be lessened by the creation of a larger gastrojejunostomy anastomosis. The effect on the restrictive element of the bypass and subsequent effect on weight loss long term has not been evaluated. We avoided excessive dilation to allow the patient to maintain as much restriction as possible. Using a protocol of minimal dilation to between 12.5 and 15 mm resulted in only one perforation and acceptable weight loss. In our study and those of others,21,22 weight loss at 1 year is not hindered by dilation.
A limitation of this study is that is was retrospective. A prospective trial in which comorbidities were not controlled would not be feasible, although a prospective trial of H2 antagonists may be of value. It is difficult to discern the effect of absorbable suture on stricture rates vs the effect of H2 antagonists as their introduction to the protocol occurred in close proximity. The finding that readmissions within 30 days of surgery and postoperative peripheral neuropathy were statistically significant covariates of stricture most likely relates to the frequency of readmissions for peripheral neuropathy secondary to vitamin deficiencies following bariatric surgery.
The objective of this study was to reach back in the causal continuum, prior to the intraoperative effects of technique and surgeon experience, to identify other potentially salient contributors to postoperative stricture. This analysis of a large series of patients undergoing RYGB identified GERD and age as factors associated with gastrojejunostomy stricture.
Conclusions
Using absorbable suture at the gastrojejunostomy anastomosis appears to decrease stricture rates. As identified via multivariate logistic regression analysis, GERD and age are independent predictors of gastrojejunostomy stricture.
References
Flancbaum L, Choban PS. Surgical implications of obesity. Annu Rev Med 1998;49:215–234.
MacLean LD, Rhode BM, Sampalis J, Forse RA. Results of the surgical treatment of obesity. Am J Surg 1993;165:155–159.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and metaanalysis. JAMA 2004;292:1724–1737.
Yale CE. Gastric surgery for morbid obesity: complications and long-term weight control. Arch Surg 1989;124:941–946.
Christou NV, Sampalis JS, Liberman M, Look D, Auger S, McLean AP, MacLean LD. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 2004;240(3):416–423; discussion 423–424.
Choban PS, Onyejekwe J, Burge JC, Flancbaum L. A health status assessment of the impact of weight loss following Roux-en-Y gastric bypass for clinically severe obesity. J Am Coll Surg 1999;188(5):491–497.
Wittgrove AC, Clark GW, Tremblay CJ. Laparoscopic gastric bypass, Roux-en-Y: preliminary report of five cases. Obes Surg 1994;4:353–357.
Nguyen NT, Lee SL, Goldman C, Fleming N, Arango A, McFall R, Wolfe B. Comparison of pulmonary function and postoperative pain after laparoscopic versus open gastric bypass: a randomized trial. J Am Coll Surg 2001;192(4):469–476; discussion 476–477.
Higa KD, Boone KB, Ho T, Davies OG. Laparoscopic Roux-en-Y gastric bypass for morbid obesity: technique and preliminary results of our first 400 patients. Arch Surg 2000;135:1029–1034.
Wittgrove AC, Clark GW. Laparoscopic gastric bypass, Roux-en-Y- 500 patients: technique and results, with 3–60 month follow-up. Obes Surg 2000;10(3):233–239.
El Shobary H, Christou N, Backman SB, Gvocdic B, Schricker T. Effect of laparoscopic versus open gastric bypass surgery on postoperative pain and bowel function. Obes Surg 2006;16(4):437–442.
Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J. Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Ann Surg 2000;232(4):515–529.
Westling A, Gustavsson S. Laparoscopic vs open Roux-en-Y gastric bypass: a prospective, randomized trial. Obes Surg 2001;11:284–292.
Nguyen NT, Silver M, Robinson M, Needleman B, Hartley G, Cooney R, Catalano R, Dostal J, Sama D, Blankenship J, Burg K, Stemmer E, Wilson SE. Result of a national audit of bariatric surgery performed at academic centers: a 2004 University HealthSystem Consortium Benchmarking Project. Arch Surg 2006;141(5):445–449; discussion 449–450.
Puzziferri N, Austrheim-Smith IT, Wolfe BM, Wilson SE, Nguyen NT. Three-year follow-up of a prospective randomized trial comparing laparoscopic versus open gastric bypass. Ann Surg 2006;243(2):181–188.
Matthews BD, Sing RF, DeLegge MH, et al. Initial results with a stapled gastrojejunostomy for the laparoscopic isolated Roux-en-Y gastric bypass. Am J Surg 2000;179:476–481.
Schauer P, Ikramuddin S, Hamad G, Gourash W. The learning curve for laparoscopic Roux-en-Y gastric bypass is 100 cases. Surg Endosc 2003;17(2):212–215.
Sanyal AJ, Sugerman HJ, Kellum JM, et al. Stomal complications of gastric bypass: incidence and outcome of therapy. Am J Gastroenterol 1992;87:1165–1169.
Schirmer BD. Strictures and marginal ulcers in bariatric surgery. In: Buchwald H, Pories WJ, Cowan GSM, eds. Surgical Management of Morbid Obesity. New York: Elsevier, 2006, in press.
Perugini RA, Mason R, Czerniach DR, Novitsky YW, Baker S, Litwin DE, Kelly JJ. Predictors of complication and suboptimal weight loss after laparoscopic Roux-en-Y gastric bypass: a series of 188 patients. Arch Surg 2003;138(5):541–545; discussion 545–546.
Goitein D, Papasavas PK, Gagne D, Ahmad S, Caushaj PF. Gastrojejunal strictures following laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Endosc 2005;19(5):628–632.
Rossi TR, Dynda DI, Estes NC, Marshall JS. Stricture dilation after laparoscopic Roux-en-Y gastric bypass. Am J Surg 2005;189(3):357–360.
Acknowledgments
We want to thank our Gastroenterology colleagues, Jay Mellen, MD, and Leon Rigberg, MD, who have worked with our team in the treatment of our gastric bypass patients with a collaborative demeanor and flawless technique. We must also thank the nursing staff at Scottsdale Healthcare and the office staff of Scottsdale Bariatric Center for their kind and considerate care of patients who are struggling with life after surgery. We acknowledge J. N. Buchwald, M.A., for her consultation and editing of the manuscript. Finally, our thanks go to all our family and friends who endure us during our efforts to communicate our research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Blackstone, R.P., Rivera, L.A. Predicting Stricture in Morbidly Obese Patients Undergoing Laparoscopic Roux-en-Y Gastric Bypass: A Logistic Regression Analysis. J Gastrointest Surg 11, 403–409 (2007). https://doi.org/10.1007/s11605-007-0135-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0135-x