Abstract
Purpose
The risk of malignancy after solid-organ transplantation is well documented. However, the incidence and specific risk for colorectal adenocarcinoma, although previously proposed, has been difficult to calculate. We reviewed the University of Wisconsin transplant database for all cases of colorectal adenocarcinoma to assess the risk of this malignancy, as well as the need for improved screening in this population.
Methods
The transplant database was queried using diagnosis codes for colorectal adenocarcinoma to configure a list of eligible patients. Exclusion criteria included: age less than 18 years at the time of transplant, diagnosis of colorectal cancer or patient death less than 12 months posttransplant, and pretransplant history of colorectal cancer or proctocolectomy. Statistical analysis determined overall incidence, age-specific incidence, and survival for this population.
Results
A total of 5,603 kidney, liver, or combination transplants were eligible for analysis from 1966 through 2004. The mean follow-up was 9.3 years. We identified 40 cases of colorectal adenocarcinoma. Twenty-five of these cases (62%) occurred in kidney transplant recipients, 13 after liver transplant, and two after kidney–pancreas combination. Twenty-seven patients (68%) diagnosed with cancer have died, 12 of metastatic disease. The median survival postcancer diagnosis was 2.3 years. These results were compared to the National Cancer Institute Survival, Epidemiology, and End Results (SEER) database for colon and rectal cancer. The current age-adjusted annual incidence based on year 2000 census data is 0.053% (52.9/100,000), and the extrapolated 10-year incidence is 0.27%. The 10-year incidence in the transplanted cohort is 0.71% (incidence ratio = 2.6). The 5-year survival postcancer diagnosis is 63.5% in the general population (SEER), vs. 30.7% in the transplant cohort. The SEER median age at diagnosis of colorectal adenocarcinoma is 72.0 years. Of the transplant recipients who developed cancer, the median age at diagnosis was 58.7 years (32.4 to 78.2), and 11 patients (27%) were diagnosed at or before age 50. In the U.S. population, the annual incidence of colorectal adenocarcinoma below the age of 50 is 0.0055% (5.52/100,000) and the 10-year extrapolated incidence is 0.11%. The 10-year incidence in the under-50 transplant cohort is 0.33% (incidence ratio = 3.0). In this under-50 cohort, median time from transplant to cancer diagnosis was 7.8 years.
Conclusion
The incidence of and 5-year survival after diagnosis of colorectal adenocarcinoma in transplant recipients is markedly different than the general population. Patients are often diagnosed at a younger age. With current screening guidelines, over 25% of at-risk patients would not be screened. We propose modifying these guidelines to allow earlier detection of colorectal cancer in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The solid-organ transplant population has a well-documented risk for certain malignancies. The first reports of soft-tissue and lymphoproliferative malignancy among renal transplant recipients date back to the late 1960s.1,2 As the variety of transplanted organs has grown and long-term survival is now expected, the range and severity of neoplasms have become a formidable medical challenge. The reported lifetime incidence of posttransplant malignancy varies, but overall the risk appears to be three to five times that of the general population.3,4 The majority of these neoplasms are nonmelanoma skin and lymphoproliferative cancers, which differs significantly from the predominant tumors presenting in the general population.5 However, the incidence of several other neoplasms, excluding cutaneous and lymphoproliferative disease, is also significantly increased.6,7
Included in these other neoplasms has been colorectal adenocarcinoma, although the true risk is less well characterized. European data, including Swedish and Danish studies, have documented an increased risk among solid-organ recipients, especially those post-liver transplant.7,8 Australian and New Zealand transplant registries have confirmed these findings.9 Interestingly, the data for American patients are less clear, with some studies demonstrating no increased risk.5 Previous attempts to calculate colorectal cancer risk in the U.S. have utilized databases that include only transplant patients with cancer, and a true incidence therefore cannot be calculated.5 Because the transplant database at the University of Wisconsin is prospective and includes data from over 5,000 transplant recipients, a more accurate calculation of the incidence, age at presentation, and survival of solid-organ transplant recipients diagnosed with colorectal cancer is possible and is the primary aim of this study. In addition, as a secondary aim, the information gained by this assessment allows further insight to the need for future screening alterations, because current guidelines are the same for transplant recipients and the general population.
Materials and Methods
The University of Wisconsin organ transplantation program has existed since 1966. A prospective database for these patients has evolved significantly since that time. In its current computerized form, it contains pre- and posttransplant information for abdominal solid organ and small bowel transplant recipients, as well as diagnosis codes for all types of secondary diagnoses and related follow-up. Approval for this review was granted by the University of Wisconsin Institution Review Board. The database was queried for all cases of colorectal adenocarcinoma among transplant recipients who were greater than 18 years of age at the time of transplant. The age at diagnosis, time from first transplant to cancer diagnosis, time from cancer diagnosis to death, and cause of death were subsequently identified. These variables were then used to calculate a 10-year colorectal cancer incidence and survival in this patient population.
To properly identify the population at risk, several exclusion criteria were utilized. Patients were excluded from the analysis if they: 1) were under the age of 18 at the time of their transplant, 2) did not have their first transplant at the University of Wisconsin (to properly calculate the length of time from first transplant to cancer diagnosis), 3) were diagnosed with colorectal cancer within the first 12 months of transplant (as this likely represented a pretransplant condition rather than a result of the transplant itself), 4) died within 12 months of transplant, 5) had a known preoperative diagnosis of colorectal cancer, prior adenomatous polyps, inflammatory bowel disease (IBD), and/or prior proctocolectomy, or 6) underwent combined heart or intestine solid-organ transplant.
These results were compared to the most appropriate data available from the National Cancer Institute’s Survival, Epidemiology, and End Results (SEER) database. This database is composed of multiple epidemiologic reporting centers throughout the U.S., which were selected based on the region’s ability to maintain a high-quality cancer reporting system. The total SEER population consists of approximately 26% of the total U.S. population and is assumed comparable in composition to the U.S. population overall. The database collects information from each reporting center on patient demographics, primary tumor site, stage at diagnosis, and follow-up. It is currently the best estimate of cancer incidence, age, and survival statistics for the U.S. population.
Because the incidence data in the SEER database is reported per year, it is difficult to compare the number of transplant patients who developed cancer during the follow-up period with the incidence in the general population. However, the 10-year risk by age group (decade) is available for the general population.12 These data were plotted and the specific 10-year incidence was extrapolated from the graph using the mean age at the time of transplant. Similarly, this approach was repeated for comparison between the U.S. population and the transplant cohort under the age of 50. An incidence ratio was calculated as the Kaplan–Meier estimate of the 10-year cancer incidence in the transplant group divided by an estimate of the 10-year incidence from the SEER database.10,11
Statistics
All statistics were reviewed by a senior statistician (G.E.L.) Patient survival rates and free-of-colorectal-adenocarcinoma rates were estimated using the methods of Kaplan and Meier. The increase in risk of patient death associated with the posttransplant development of colorectal adenocarcinoma was estimated by employing a Cox proportional hazards model with a time-varying covariate. Continuous variables were summarized by reporting means ± standard deviations and discrete variables were summarized by reporting percentages. All analyses were performed using SAS statistical software version 6.12, SAS Institute, Inc. (Cary, NC, USA).
Results
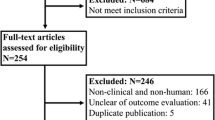
The University of Wisconsin transplant database includes 6,771 transplant recipients from 1966 through 2004. This population includes patients whose first recorded transplant was performed at the University of Wisconsin, as well as patients who had a subsequent transplant at UW after receiving their first organ at a different institution. After excluding 253 patients whose first transplant was not performed at the University of Wisconsin, 6,518 patients remained. An additional 26 patients were excluded who received combination heart or intestine solid-organ transplants, leaving 6,492 patients eligible for analysis. An additional 889 patients met our exclusion criteria as described in Materials and Methods (Table 1). These included 396 patients younger than 18 years of age and 477 patients who died within the first year after transplantation. Finally, 14 patients had a known preoperative diagnosis of adenocarcinoma, adenomatous polyps, inflammatory bowel disease (IBD), or prior proctocolectomy. However, the total number of patients in the transplant population who had either IBD or a history of colectomy was 101; all but 14 were previously excluded because of one of the other criteria listed above. Two patients were censored because of a diagnosis of colorectal adenocarcinoma within 12 months of transplant. Therefore, a total of 5,603 patients remained for inclusion in this analysis.
In the transplant recipient population overall, the mean age at transplant was 43.4 years, and the percentage of patients transplanted before age 50 was 67.6%. The mean length of follow-up was 9.3 years. Sixty percent of UW transplant recipients were male. The majority of patients were cadaveric kidney recipients (2,400 patients, 42.8%), with living-related kidney (1,249, 22.3%), living-unrelated kidney (303, 5.4%), kidney–pancreas (798, 14.2%), kidney–liver (17, 0.3%), and liver (836, 14.9%) comprising the remaining transplant types (Table 2). The overall survival for transplant recipients at the University of Wisconsin, including those patients with colorectal cancer, is 87.8% at 5 years and 71.0% at 10 years.
Among the 5,603 patients, a total of 40 cases of colorectal adenocarcinoma were identified. Of those who developed cancer, the median age at diagnosis was 58.7 years. Twenty-five of these cases (62%) occurred in kidney transplant recipients, 13 (32.5%) after liver transplant, and two (5%) after kidney–pancreas combination (Table 2). The median time from transplant to cancer diagnosis was 6.6 years, and 12 patients (30%) were diagnosed less than 5 years post transplant (Fig. 1). In the liver transplant population specifically, 103 patients (out of 836) were transplanted for primary sclerosing cholangitis (PSC); two of these patients were eventually diagnosed with colorectal adenocarcinoma, although they were screened aggressively preoperatively and were not found to have evidence of active ulcerative colitis or polyps. According to the SEER database, in the U.S. general population from 1998 to 2002, the median age at colorectal cancer diagnosis was 72.0 years. The age-adjusted annual incidence for the general population based on year 2000 census data is 0.053% (52.9/100,000). Based on the plot of 10-year risk by decade of life in the U.S. population, the 10-year incidence for a 43-year-old (mean age of transplant) is 0.27%. The 10-year incidence in the transplanted cohort is 0.71%. Therefore, the incidence ratio for cancer diagnosis in this group compared to the general population is 2.6. Twenty-seven patients (68%) diagnosed with cancer have died, 12 of metastatic disease. The median survival after colorectal cancer diagnosis was 2.3 years (Fig. 2). In the UW transplant recipient population overall, the diagnosis of colorectal adenocarcinoma results in a relative risk of death of 6.6 (4.3–9.3). The 5-year survival for all stages of colon cancer is 63.5% in the general population (SEER) compared to 30.7% in the transplant cohort (Table 3).
The length of time from transplant to cancer diagnosis was calculated for each of the 40 transplant recipients who developed colorectal adenocarcinoma. This was plotted in years post transplant and grouped into 2-year increments. Patients who developed cancer within 1 year of transplant were excluded from the total eligible patient pool due to the likelihood of a pre-existing condition. A total of 13 patients developed cancer 10 or more years post transplant (range 10.1–33.8).
Considering only those patients under the age of 50, the mean age at transplant was 36.5 years. Among the 40 transplant recipients with colorectal adenocarcinoma, 11 patients (27.5%) were 50 years old or younger (Fig. 3). In this subgroup of patients, the median age at cancer diagnosis was 42.4 years. In the U.S. general population (SEER), the age-adjusted annual incidence of colorectal adenocarcinoma in patients under 50 years old is 0.0055% (5.52/100,000). The 10-year risk for a 36-year-old in the general population is 0.11%. The estimated 10-year incidence in this 50-and-under transplanted group is 0.29% (11/3794). Therefore, the incidence ratio for transplant recipients under the age of 50 compared to people under 50 in the general population is 3.0. The median time from transplant to cancer diagnosis in this subgroup was 7.8 years, and the median survival post cancer diagnosis was 2.4 years. In all, 23/40 patients (58%) were either 50 years old or younger at the time of diagnosis, or were diagnosed with cancer within 5 years of their transplant.
The age of each transplant recipient at the time of cancer diagnosis was determined for each of the 40 patients who developed colorectal adenocarcinoma. Note that 11/40 (27.5%) of patients were age 50 or less at the time of cancer diagnosis and would have been missed by current cancer screening guidelines.
Discussion
A significantly higher risk of developing neoplasia is noted in transplant recipients when compared with age-matched controls. The first such report dates back to 1968.1 Since then numerous studies have documented this correlation, with estimates of three to five times the overall risk for malignancy, and a lifetime incidence of 6%.3–5,7 Interestingly, most of these neoplasms differ from the predominant tumor types seen in the general population and are comprised mainly of nonmelanoma skin and lymphoproliferative cancers.5,7,13 However, even after excluding these common posttransplant malignancies, the incidence of other neoplasia is also increased, with an overall relative risk of up to 3.4 times that of the general population.9
An increased risk for the development of colorectal cancer after solid organ transplantation has been previously suggested, primarily by European data. The Swedish cancer registry, which followed 5,931 solid organ recipients for an average of 6.8 years, identified 34 cases of colorectal adenocarcinoma.7 Compared with the Swedish population overall, the incidence of colon and rectal cancer using standardized incidence ratios was approximately twofold higher in the transplanted group. In addition, they noted a predilection for right-sided cancers, with a standardized incidence ratio of 3.3 vs. 1.8 for left-sided colon tumors.7 Other studies have determined the overall lifetime risk for colon cancer to be two to three times that of the general European population, especially more than 10 years post transplant.14,15 Similarly, Birkeland et al. reviewed 5,692 renal transplant patients transplanted between 1964 and 1982 in Scandinavia and calculated male and female standardized incidence ratios of 3.2 and 3.9 for colon cancer compared to the general population.4
The combined New Zealand and Australian tumor registries also reported an increased risk for posttransplant colon cancer. The authors identified 38 cases of colorectal cancer among 6,641 renal transplant recipients, with a calculated risk ratio of 2.6 compared to the general population.16,17 In contrast, conflicting evidence for this risk comes from a multinational database including more than 300 transplant centers worldwide. From this Collaborative Transplant Study, over 76,000 patients post heart or kidney transplant have been followed since 1983. In this analysis, a modest but not statistically significant increased incidence in colon cancer was observed.18
The incidence of colorectal cancer among transplant recipients within the U.S. is less clear. Previous estimates of this risk have utilized the Israel Penn International Transplant Tumor Registry, which is comprised of solid-organ transplant recipients with a diagnosis of malignancy. Early reports from this database did not specifically address colorectal cancer incidence, although 386 cases of colorectal cancer were identified among 10,667 transplant recipients.5,19 As this database is comprised exclusively of transplant recipients with malignancy, a true cancer incidence is difficult to calculate. Because the University of Wisconsin transplant database is prospective for transplant recipients overall, a more reliable estimate of the incidence in this population is possible. Although a comparison of this incidence to that of the general population is difficult, our efforts to do so based on SEER database statistics for a similarly matched age group reveal an appreciably higher incidence in the transplanted cohort.
Additional U.S. studies include a work by Agraharkar et al., who compared the risk of colorectal malignancy among 1,739 U.S. renal transplant recipients to the SEER database in a single institution retrospective review. A total of six cases of colorectal cancer were identified, and a standardized incidence ratio (SIR) of 1.5 was calculated.6 Similarly, a single institution review of 556 U.S. renal transplant recipients identified three cases (0.5%) of colorectal cancer. All cases occurred in male patients over the age 50 without a history of prior screening colonoscopy. The mean time from transplant to cancer diagnosis in this study was 11 years. The authors concluded that there did not appear to be an increased risk of colorectal cancer when compared to the general population, although a more aggressive phenotype was observed.20
Regardless of the incidence, the behavior of these neoplasms does appear different in this immunosuppressed population. It has been previously noted in transplant recipients that squamous cell skin cancers act more aggressively and are diagnosed at a younger age.5,21–26 Similarly, Papaconstantinou et al. found that transplant recipients developed de novo colorectal cancer at a younger age (58 vs. 70 years) and had a worse 5-year survival (43.5% vs. 62.3%), compared with NCI/SEER database statistics.27 Our data also suggest that the behavior of colorectal cancer is more aggressive in this population. Of those with cancer, the median age at diagnosis in our population was 58.7 years, compared to 72.0 for the U.S. population in general. The 5-year survival post cancer diagnosis was just 30.7% vs. 63.5% in the SEER database. In addition, more than 25% of transplant recipients diagnosed with colorectal adenocarcinoma in our database were younger than 50 years old. It is unclear whether this apparently more aggressive phenotype is a result of immunosuppression, later stage at diagnosis secondary to screening issues, or a combination of these and other factors.
Several theories have been proposed to explain the association between immunosuppression and malignancy. Immunosuppressive agents themselves have been identified as possible factors. For example, metabolites of azathioprine are known to sensitize the skin to sunlight and may increase the risk of skin cancer, and some agents such as azathioprine, cyclophosphamide, and cyclosporine may directly damage DNA.5,22 Agents like cyclosporine and T-cell specific inhibitors such as OKT3 and ATG, while rescuing the patient from graft loss also create dysregulation of the body’s natural antineoplastic defenses. Although the type or degree of immunosuppression was not the focus of this study, the most likely mechanism relating to the development of colorectal cancer is the body’s inability to respond against natural carcinogens.22 The degree of immunosuppression has been found to be an independent risk factor in the development of carcinoma, and in some cases the reduction in immunosuppression has been utilized as treatment after cancer diagnosis.5 Similarly, it has been noted that chronic disease states requiring immunosuppression, such as rheumatoid arthritis and systemic lupus erythematosis, have higher rates of malignancy as well.28
If indeed immunosuppression is the reason for these findings, one would expect a greater risk in patient cohorts requiring higher doses of antirejection medication. Heart recipients, for example, have generally been maintained on stronger immunosuppressive regimens because allograft loss would result in death and several studies have found a higher cancer incidence in this transplant cohort.7,29 However, if immunosuppression is the only factor, we would expect the incidence of all cancer types to be equally more common. Clearly, additional risk factors such as genetics, geography, and premalignant conditions are also important considerations. Finally, the time from transplant to diagnosis (duration of immunosuppression) may also be a significant factor. In European studies, the cumulative risk for developing any malignancy posttransplant was recorded as 13.6% at 10 years and 31.8% at 20 years.7 In 124 cardiac transplant recipients, the cumulative cancer risk was 2.7 % at 1 year and 25.6% at 5 years.30 In liver transplant patients, the overall risk of de novo malignancy was 6%, 20% and 55% at 5, 10, and 15 years of follow-up, respectively.8 Although the prevalence of cancer increases with age in the general population as well, the incidence among transplant patients is clearly much higher.
Liver transplant recipients have been previously identified as being at risk for developing colorectal cancer. Proposed mechanisms have included liver dysfunction, which may expose the colon to carcinogens, or premalignant conditions such as ulcerative colitis often noted in patients transplanted for primary sclerosing cholangitis. Haagsma et al. found 21 malignancies among 174 liver transplant recipients, followed for a mean of 5.1 years in the Netherlands. Three cases of colon cancer were found with a calculated relative risk of 12.5 times that of the general Dutch population. Their series included 29 patients transplanted for primary sclerosing cholangitis (PSC) and 18 patients with ulcerative colitis, although a subgroup analysis did not find these patients at increased risk when compared to the remaining liver transplant recipients.8 A recent review of the Pittsburgh liver transplant registry revealed 50 malignancies among 1,657 patients. Colon adenocarcinoma was identified in 3.1%, although premalignant conditions were not specified.31 Bleday et al. discovered colon cancer or high-grade dysplasia in 3 of 27 patients who underwent liver transplantation for PSC. These patients all had negative pretransplant colonoscopies and developed neoplasia within 13 months of transplantation.32 Similar findings were published by Loftus et al., who noted a 1% per person per year incidence of colorectal neoplasia in liver recipients transplanted for PSC.33 Trotter et al. suggested that aggressive posttransplant surveillance, including annual colonoscopy with biopsy in patients with inflammatory bowel disease, and colonoscopy every 3 years in patients with adenomatous polyps, may improve disease-free survival in liver transplant recipients.33,34 It seems likely that a correlation between PSC and ulcerative colitis places these patients at increased risk for eventual colorectal cancer development. In our analysis, we specifically excluded patients with known inflammatory bowel disease to more clearly demonstrate the direct association between transplantation and colorectal cancer risk. Even with this exclusion, our liver transplant recipients comprised 32.5% of the patients with cancer, but only 15% of the total transplant population. Out of 103 liver recipients in our series transplanted for PSC, two patients were eventually diagnosed with colorectal adenocarcinoma, although they were screened aggressively pre transplant and were not found to have polyps or active IBD. Therefore, we found no clear association between a history of PSC without IBD and eventual colorectal cancer.
In the present study, we identified a significant cohort of patients diagnosed with colorectal cancer at an age less than 50. Based on the mean age of all transplant recipients under age 50, we extrapolated a 10-year incidence from the SEER database. Upon comparison, transplant recipients under the age of 50 were found to have a threefold greater risk of developing colorectal cancer. Because the current recommendations for screening transplant recipients does not differ from that of the general population, it is likely that several of these younger patients would be excluded from current colorectal cancer screening guidelines.34,35 Most transplant centers, including the University of Wisconsin, now administer a preoperative colonoscopy to patients over age 50 and subsequent postoperative surveillance colonoscopy based on standard U.S. screening guidelines.34,36 Unfortunately, most transplant registries seldom report whether aggressive or standard postoperative surveillance was administered. Similarly, our database does not record which of these patients received screening or surveillance colonoscopy appropriately. On the other hand, some might argue that many of these patients are actually screened more aggressively, and the higher rates of colorectal cancer are the result of selection bias. Current recommendations from the American Society of Transplantation are not different from that of the general population.35 Therefore, there is little reason to believe that patients without documented prior disease or risk factors such as inflammatory bowel disease are screened differently than the general population.
Conclusion
Our data would suggest that the incidence of and 5-year survival after diagnosis of colorectal adenocarcinoma in transplant patients is markedly different from the general population. Although the median age at cancer diagnosis was 58.7 years of age, there is a significantly higher risk in those less than age 50 as well. In addition, it appears that these malignancies may behave more aggressively. Based on our findings, we would propose the following posttransplantation screening colonoscopy recommendations. Initial screening in existing transplant recipients should be performed within 2 years of the first transplant. For those not yet transplanted and older than age 50, a baseline pretransplant screening colonoscopy should be obtained (if not already done) along with a follow-up surveillance exam 2 years after transplant. In patients not yet transplanted and under the age of 50, a preoperative screening colonoscopy could also be considered, although more importantly, initial screening should begin within 2 years post transplant. Clearly, prospective, multiinstitutional data are needed to further clarify the ideal regimen and better define the time interval after initial screening. However, it seems a relatively short interval between screenings may be necessary. The impact of colorectal screening in the general population has been significant to date, and although this malignancy may present earlier and act more aggressively in transplant recipients, one may be comforted by the fact that more aggressive screening may continue to preserve this most precious gift in an at-risk population.
References
Doak PB, Montgomerie JZ, North JD, Smith F. Reticulum cell sarcoma after renal homotransplantation and azathioprine and prednisone therapy. BMJ 1968;4(633):746–748.
Penn I, Hammond W, Brettschneider L, Starzl TE. Malignant lymphomas in transplantation patients. Transplant Proc 1969;1:106–112.
Birkeland SA, Lokkegaard H, Storm HH. Cancer risk in patients on dialysis and after renal transplantation. Lancet 2000;355(9218):1886–1887.
Birkeland SA, Storm HH, Lamm LU, Barlow L, Blohme I, Forsberg B, Eklund B, Fjeldborg O, Friedberg M, Frodin L. Cancer risk after renal transplantation in the Nordic countries, 1964–1986.[see comment]. Int J Cancer 1995;60(2):183–189.
Penn I. Tumors after renal and cardiac transplantation. (Review; 24 refs). Hematol/Oncol Clin N Am 1993;7(2):431–445.
Agraharkar ML, Cinclair RD, Kuo YF, Daller JA, Shahinian VB. Risk of malignancy with long-term immunosuppression in renal transplant recipients. Kidney Int 2004;66(1):383–389.
Adami J, Gabel H, Lindelof B, Ekstrom K, Rydh B, Glimelius B, Ekbom A, Adami HO, Granath F. Cancer risk following organ transplantation: a nationwide cohort study in Sweden.(See comment). Br J Cancer 2003;89(7):1221–1227.
Haagsma EB, Hagens VE, Schaapveld M, van den Berg AP, de Vries EG, Klompmaker IJ, Slooff MJ, Jansen PL. Increased cancer risk after liver transplantation: a population-based study.(See comment). J Hepatol 2001;34(1):84–91.
Shiel AGR. Cancer in dialysis and transplant patients. In Morris PJ, ed. Kidney Transplantation: Principles and Practice, 4th ed. Philadelphia: WB Saunders, 1994, pp 390–400.
National Cancer Institute SEER Database. Available at http://seer.cancer.gov 2005.
Hankey BF, Ries LA, Edwards BK. The surveillance, epidemiology, and end results program: a national resource. (Review; 43 refs). Cancer Epidemiol Biomark Prev 1999;8:1117–1121.
SEER Cancer Statistics Review 1975–2002, Table VI-13 Colon and Rectum Cancer (Invasive) 2005.
Tremblay F, Fernandes M, Habbab F, deB E, Loertscher R, Meterissian S. Malignancy after renal transplantation: incidence and role of type of immunosuppression. Ann Surg Oncol 2002;9:785–788.
Kyllonen L, Salmela K, Pukkala E. Cancer incidence in a kidney-transplanted population. Transpl Int 2000;13(Suppl 1):S394–S398.
Brunner FP, Landais P, Selwood NH. Malignancies after renal transplantation: the EDTA-ERA registry experience. European Dialysis and Transplantation Association-European Renal Association. Nephrol Dial Transplant 1995;10(Suppl 1):74–80.
Sheil AGR. Cancer in dialysis and transplant patients. In Morris PJ, ed. Kidney Transplantation: Principles and Practice, 4th ed. Philadelphia: WB Saunders, 1994, pp 390–400.
Sheil A. Cancer report. In Disney APS, ed. Fourteenth Report of the Australia and New Zealand Dialysis and Transplant Registry. Woodville, South Australia: Queen Elizabeth Hospital, 1991.
Stewart T, Henderson R, Grayson H, Opelz G. Reduced incidence of rectal cancer, compared to gastric and colonic cancer, in a population of 73,076 men and women chronically immunosuppressed. Clin Cancer Res 1997;3(1):51–55.
Trivedi MH, Agrawal S, Muscato MS, Metzler MH, Marshall JB. High grade, synchronous colon cancers after renal transplantation: were immunosuppressive drugs to blame? (Review: 11 refs). Am J Gastroenterol 1999;94(11):3359–3361.
Saidi RF, Dudrick PS, Goldman MH. Colorectal cancer after renal transplantation. Transplant Proc 2003;35:1410–1412.
Mullen DL, Silverberg SG, Penn I, Hammond WS. Squamous cell carcinoma of the skin and lip in renal homograft recipients. Cancer 1976;37(2):729–734.
Penn I. Why do immunosuppressed patients develop cancer? (Review; 271 refs). Crit Rev Oncog 1989;1(1):27–52.
Euvrard S, Kanitakis J, Pouteil-Noble C, Disant F, Dureau G, Finaz d, V, Claudy A, Thivolet J. Aggressive squamous cell carcinomas in organ transplant recipients. Transplant Proc 1995;27(2):1767–1768.
Adamson R, Obispo E, Dychter S, Dembitsky W, Moreno-Cabral R, Jaski B, Gordon J, Hoagland P, Moore K, King J, Andrews J, Rich M, Daily PO. High incidence and clinical course of aggressive skin cancer in heart transplant patients: a single-center study. Transplant Proc 1998;30(4):1124–1126.
Pollard JD, Hanasono MM, Mikulec AA, Le QT, Terris DJ. Head and neck cancer in cardiothoracic transplant recipients. Laryngoscope 2000;110(8):1257–1261.
Veness MJ, Quinn DI, Ong CS, Keogh AM, Macdonald PS, Cooper SG, Morgan GW. Aggressive cutaneous malignancies following cardiothoracic transplantation: the Australian experience. (Review; 21 refs). Cancer 1999;85(8):1758–1764.
Papaconstantinou HT, Sklow B, Hanaway MJ, Gross TG, Beebe TM, Trofe J, Alloway RR, Woodle ES, Buell JF. Characteristics and survival patterns of solid organ transplant patients developing de novo colon and rectal cancer. Dis Colon Rectum 2004;47(11):1898–1903.
Morath C, Mueller M, Goldschmidt H, Schwenger V, Opelz G, Zeier M. Malignancy in renal transplantation. (Review; 76 refs). J Am Soc Nephrol 2004;15(6):1582–1588.
Jensen P, Hansen S, Moller B, Leivestad T, Pfeffer P, Geiran O, Fauchald P, Simonsen S. Skin cancer in kidney and heart transplant recipients and different long-term immunosuppressive therapy regimens.(See comment). J Am Acad Dermatol 1999;40(2 Pt 1):177–186.
Krikorian JG, Anderson JL, Bieber CP, Penn I, Stinson EB. Malignant neoplasms following cardiac transplantation. JAMA 1978;240(7):639–643.
Frezza EE, Fung JJ, van Thiel DH. Non-lymphoid cancer after liver transplantation. Hepato-gastroenterology 1997;44(16):1172–1181.
Bleday R, Lee E, Jessurun J, Heine J, Wong WD. Increased risk of early colorectal neoplasms after hepatic transplant in patients with inflammatory bowel disease. (Review; 23 refs). Dis Colon Rectum 1993;36(10):908–912.
Loftus EV, Jr, Aguilar HI, Sandborn WJ, Tremaine WJ, Krom RA, Zinsmeister AR, Graziadei IW, Wiesner RH. Risk of colorectal neoplasia in patients with primary sclerosing cholangitis and ulcerative colitis following orthotopic liver transplantation. Hepatology 1998;27(3):685–690.
Trotter JF. Cancer surveillance following orthotopic liver transplantation. (Review; 65 refs). Gastrointest Endosc Clin N Am 2001;11(1):199–214.
Kasiske BL, Vazquez MA, Harmon WE, Brown RS, Danovitch GM, Gaston RS, Roth D, Scandling JD, Singer GG. Recommendations for the outpatient surveillance of renal transplant recipients. American Society of Transplantation. J Am Soc Nephrol 2000;11(Suppl 15):S1–S86.
Winawer S, Fletcher R, Rex D, Bond J, Burt R, Ferrucci J, Ganiats T, Levin T, Woolf S, Johnson D, Kirk L, Litin S, Simmang C, Gastrointestinal Consortium. Colorectal cancer screening and surveillance: clinical guidelines and rationale—update based on new evidence. Gastroenterology 2003;124:544–560.
Acknowledgments
We appreciate the capable assistance of Barbara Voss and Delores Robillard in data analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Johnson, E.E., Leverson, G.E., Pirsch, J.D. et al. A 30-Year Analysis of Colorectal Adenocarcinoma in Transplant Recipients and Proposal for Altered Screening. J Gastrointest Surg 11, 272–279 (2007). https://doi.org/10.1007/s11605-007-0084-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0084-4