Abstract
Purpose
This study aimed to evaluate the usefulness of a coaxial double balloon catheter for simplification of the balloon-occluded retrograde transcatheter obliteration (BRTO) procedure compared with a single-balloon catheter.
Materials and methods
Thirty-three patients who underwent BRTO with a single-balloon catheter (Single-balloon group, n = 15) or a coaxial double balloon catheter (Coaxial group, n = 18) were included, retrospectively. The frequency of additional procedures for stagnation of sclerosant including ethanol injection, coil embolization, and additional balloon occlusion for collateral draining veins; the dose of ethanolamine oleate (EO); and the complication rate and the success rate of sclerosant stagnation were evaluated.
Results
Additional procedures were needed in four patients in the Coaxial group, which was significantly lower than that in the Single-balloon group (nine patients, P = 0.038). The dose of EO in the Coaxial group (11.2 ± 6.6 g) was lower, but not significantly different than that in the Single-balloon group (14.4 g ± 6.1 g, P = 0.184). The complication rate and the success rate of sclerosant stagnation were not different between the two groups.
Conclusion
The use of a coaxial double balloon catheter can simplify the BRTO procedure compared with a single-balloon catheter.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric varices are one of the most important complications in patients with portal hypertension because bleeding from gastric varices is associated with high mortality [1]. Balloon-occluded retrograde transcatheter obliteration (BRTO) is an effective procedure for the treatment of gastric varices [2]; thus, it is the first-line treatment in the prevention of rebleeding from gastric varices [3]. To perform BRTO successfully, stagnation of the sclerosant in the gastro-renal shunt and/or gastric varices during occlusion of the gastro-renal shunt is essential; however, in many cases, collateral draining veins develop through which sclerosant flows into systemic circulation during occlusion. Therefore, preventing the outflow of the sclerosant into systemic circulation through collateral draining veins is necessary. The easiest way to avoid the outflow of sclerosant through the collateral draining veins is to advance a balloon catheter over the branch point of the collateral draining veins. However, since the gastro-renal shunt is tortuous, it is often difficult to advance the catheter to the proximal point. Therefore, additional procedures, such as embolization using a coil or ethanol, or occlusion using another balloon catheter, are necessary to prevent the outflow of the sclerosant [4], making the BRTO procedure more complex. To overcome these issues, Tanoue et al. developed a coaxial double balloon catheter system, which made it possible to advance to and occlude the proximal point of the gastro-renal shunt over the branch point of the collateral draining veins, and reduces the need of additional procedures to embolize or occlude collateral draining veins [5]. However, there is little evidence on the usefulness of a coaxial catheter to simplify BRTO procedures by reducing the necessity of embolization or occlusion for collateral draining veins compared with a conventional single catheter system.
Therefore, the aim of this study was to evaluate the effectiveness of the coaxial catheter system compared with the conventional single-balloon catheter in terms of frequency of additional procedures (including ethanol injection, coil embolization, and balloon occlusion with an additional balloon catheter) for stagnating the sclerosant in the gastro-renal shunt during BRTO.
Materials and methods
Patients
We retrospectively reviewed 40 consecutive adult patients who were admitted to our department and underwent BRTO from April 1, 2003 to March 31, 2019. Indications for BRTO were as follows: gastric varices with prior bleeding, enlarging gastric varices, and treatment-resistant hepatic encephalopathy [6]. One patient with inferior mesenteric vein-left gonadal vein shunt; one with gastrocaval shunt via the left inferior phrenic vein; one with duodenal varices; one in whom BRTO was not applicable due to a reversed blood flow in the portal vein; and one in whom foam sclerosant was used for BRTO were excluded. Furthermore, to minimize the learning curve effect on the outcomes, two patients in whom BRTO was performed by the operators who had the experience of performing the procedure less than three times were also excluded. Finally, 33 patients with gastro-renal shunt were enrolled for analysis. Informed consent was waived because of the retrospective nature of the study and the analysis used anonymous clinical data. The Local Ethics Committee approved this study, which proceeded according to the principles of the Declaration of Helsinki (1975). Patients’ characteristics are shown in Table 1. Fifteen patients underwent BRTO with a single-balloon catheter (Single-balloon group) and 18 patients underwent BRTO with a double balloon coaxial catheter (Coaxial group). The patients’ characteristics were not different between the two groups except for serum creatinine levels (Coaxial group, 0.61 ± 0.14 mg/dL; Single-balloon group, 0.83 ± 0.27 mg/dL; P = 0.005) (Table 1).
BRTO procedure
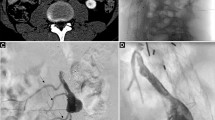
From April 1, 2003 to March 31, 2010, 15 patients underwent BRTO with a 6-Fr catheter and a 20-mm-diameter single balloon (Selecon MP or Selecon MP II catheter, Terumo Clinical Supply, Gifu, Japan). From April 1, 2010 to March 31, 2019, 18 patients underwent BRTO with a double balloon, coaxial catheter (except for one patient in whom the attending physician decided to use a single-balloon catheter) consisting of a 5 Fr catheter with a 10 mm balloon and a 9 Fr guiding catheter with a 20 mm balloon (Candis, Medikit Tokyo, Japan). BRTO was performed by operators who had more than eight years of experience in interventional radiology and were familiar with portal hypertension. BRTO procedures were as follows. First, the catheter was inserted via the femoral or internal jugular vein into the gastro-renal shunt, and venography with the balloon inflated was performed to evaluate the form of the gastro-renal shunt and collateral veins. The gastro-renal shunt is quite weak and can be easily damaged by contrast medium injection at high pressure. Therefore, contrast medium injection was performed manually and carefully. The form was classified into five grades based on a study by Hirota et al. [7]. Briefly, in grade 1, collateral draining veins were absent and the gastro-renal shunt and gastric varices were filled with contrast media; in grade 2, the amount of the contrast media outflow through the collateral draining veins was small and the contrast media stayed in the gastric varices for several minutes; in grade 3, the contrast media drained into the collateral draining veins and only a distal part of the gastric varices was filled with contrast media; in grade 4, large collateral draining veins developed and the gastric varices were not filled with any contrast media; and in grade 5, the gastro-renal shunt was too large to be occluded by a balloon catheter. Next, a 0.035 inch hydrophilic guidewire (Radifocus; Terumo, Tokyo, Japan) was advanced carefully to the proximal point and a balloon catheter was advanced over it. When using a coaxial system, a 10 mm balloon catheter was advanced to the proximal point, and inflated and hooked at the narrow part of the gastro-renal shunt. Then, a 20 mm balloon catheter was advanced over the 10 mm balloon catheter and inflated, and the 10 mm balloon catheter was deflated and advanced. After repeating these processes, both the 10 mm and 20 mm balloon catheters were advanced to the proximal point (Fig. 1). After the advancement of the catheters in both methods, venography was performed with the balloon inflated. In the Coaxial group, venography was performed with the 10 mm balloon inflated. With the 20 mm balloon, both inflation and deflation were acceptable. If the gastro-renal shunt was too large to be occluded by the 10 mm balloon catheter, the 20 mm balloon was advanced as much as possible to occlude the shunt, and venography was performed with the 20 mm balloon inflated. If the form was still Hirota’s grade 3 or 4, a microcatheter was selectively inserted into the collateral draining veins through the balloon catheter. If the collateral draining veins were narrow, ethanol was injected into them, and if they were considered to be difficult to embolize by ethanol, coils were inserted into them until they were occluded. If a microcatheter could not be selectively inserted into the collateral draining veins, another micro-balloon catheter was directly inserted into the collateral draining vein from the inferior vena cava and occluded. If the form changed to Hirota’s grade 1 or 2, the sclerosant was injected. A mixture of 10% ethanolamine oleate (EO; Oldamin, Fuji Chemical Industries, Toyama, Japan) with an equal amount of contrast medium was used as a sclerosant. The sclerosant was administered to fill the gastric varices and/or afferent veins until it did not spill out into the portal vein. The occlusion time was approximately 1 h from April 1, 2003 to March 31, 2010, except for one patient in whom the gastro-renal shunt was large. After April 1, 2010, overnight occlusion was introduced to increase the success rate of obstruction of the gastro-renal shunt [8], and all patients received overnight occlusion except for some patients in whom overnight rest was intolerable. In the cases of overnight occlusion, venography was reperformed the next day and, in cases where thrombus formation was insufficient, the sclerosant was additionally administered and the catheter was removed approximately 1 h later.
Representative venography using a coaxial double balloon catheter for a man in his 50 s who had gastric varices due to liver cirrhosis. a Venography with manual injection of sclerosant at the bottom of the gastro-renal shunt with a 10 mm balloon inflated and a 20 mm balloon deflated. The contrast media outflows into systemic circulation through retroperitoneal collateral veins (black arrows). The distal part of the gastro-renal shunt (outlined by grey line) is opacified with contrast media, but the proximal part is not filled with contrast media (outlined by grey dotted line) (Hirota’s grade 3). b Venography with manual injection of sclerosant after the advancement of a balloon catheter with a 10-mm-balloon inflated and a 20 mm balloon deflated. A 10 mm balloon is advanced to the proximal point over the branch point of the retroperitoneal collateral veins and the whole gastro-renal shunt and gastric varices are filled with contrast media (Hirota’s grade 1). The thick white arrow shows the tip of the 5 Fr catheter with a 10 mm balloon and thin white arrow shows the tip of the 9 Fr guiding catheter with a 20 mm balloon. White arrowheads show the inflated 10 mm balloon. A small retroperitoneal collateral vein (black arrow) and a posterior gastric vein (black arrowhead; main supply for the gastric varices) can also be observed. GV gastric varices
Data collection and definition
Clinical and laboratory data at the time of BRTO, and the cost of devices required for BRTO procedures, including the sheath, catheter, wire, and coil, were collected retrospectively. The form of the gastro-renal shunt at the time of catheter insertion and just before the injection of the sclerosant was assessed and classified according to Hirota’s grades. The maximum diameter of the gastro-renal shunt on contrast-enhanced computed tomography (CECT) was evaluated. Because occlusion time was different among patients and some patients underwent a hepatic venous pressure gradient (HVPG) measurement just before the BRTO procedure, the time of catheter insertion into the femoral or internal jugular vein to the time of sclerosant injection in patients who did not undergo HVPG measurement and from the time after HVPG measurement to the time of sclerosant injection in patients who underwent HVPG measurement, were used for analysis. Stagnation of sclerosant and obstruction of the gastric varices and/or the gastro-renal shunt were also evaluated. A successful obstruction was defined by the disappearance of blood flow in the gastric varices in patients who underwent BRTO to treat gastric varices or the disappearance of blood flow in the gastric-renal shunt in patients who underwent BRTO to treat hepatic encephalopathy based on the findings of CECT taken approximately 1 week after the last BRTO. Data regarding the amount of EO (g) used during BRTO were collected, and, in patients with overnight occlusion, data on the amount of EO used on the next day were also collected. We defined ethanol injection, coil embolization, and balloon occlusion by using another balloon catheter for collateral draining veins as additional procedures. For safety evaluation, we collected data on the frequency of development of acute renal failure, deterioration of ascites, thrombosis after BRTO, and vascular injury during BRTO. Acute renal failure was defined as an increase in serum creatinine levels by ≥ 0.3 mg/dL within 48 h [9]. A complication that needed specific treatment or influenced the clinical course, such as discontinuation of BRTO, was defined as a major complication [10].
Statistical analysis
Quantitative variables were compared using the Student’s t test and qualitative variables were evaluated using the Fisher’s exact test. Values with P < 0.05 were considered to be of statistical significance. The data were statistically analyzed using EZR on R commander (Version 1.38) [11] and R Statistical Software (Foundation for Statistical Computing, Vienna, Austria).
Results
Frequency of additional procedures
In the Coaxial group, 11 out of the 18 patients achieved a decrease in the Hirota’s grade after advancing a balloon catheter (grade 2, n = 2; grade 3, n = 4; grade 4, n = 5 at baseline; grade 1, n = 9; grade 2, n = 2 after advancing a catheter). In one patient, BRTO was discontinued due to vascular injury, and in two patients with grades 1 and 2 each at baseline, the grades remain unchanged after catheter advancement. The remaining four patients received additional procedures, including ethanol injection (n = 1) and coil embolization (n = 3) (Fig. 2). In the Single-balloon group, the grade was decreased by advancing a balloon catheter in three out of 15 patients (grade 3, n = 3 at baseline; grade 1, n = 3 after advancing the catheter). In one patient, BRTO was discontinued due to vascular injury, and two patients with grades 1 and 2 each did not show any improvement after advancing the catheter. The remaining 9 patients received additional procedures, including ethanol injection (n = 3), coil embolization (n = 5), and balloon occlusion (n = 3; of these, one patient received both coil embolization and balloon occlusion). The frequency of additional procedures was significantly lower in the Coaxial group (4/18) than in the Single-balloon group (9/15) (P = 0.038, Table 2).
Changes in the Hirota’s grade in each patient from when the catheter was inserted into the gastro-renal shunt to just before injection of the sclerosant. The numbers denoted in the grey bars are Hirota’s grade. In each group “●” on the left denote the Hirota’s grade in each patient when the catheter was inserted into the gastro-renal shunt and those on the right denote Hirota’s grades just before injection of the sclerosant; “○” shows the patient in whom stagnation of the sclerosant was not successful and the sclerosant was not injected; “×”denote the patients in whom vascular injury occurred and BRTO was discontinued; lines connected with marks show changes in the Hirota’s grade in each patient; solid lines show changes in Hirota’s grade obtained by the advancement of a catheter and dotted lines show those by additional procedures
Comparison of the dose of EO, required time until the injection of sclerosant, and the cost of devices required for the BRTO procedure between two groups
Five patients who underwent overnight occlusion in the Coaxial group received additional administration of EO on the next day. The mean dose of 10% EO used during BRTO without the dose of additional administration was 9.2 ± 3.8 g in the Coaxial group, which was significantly lower than that in the Single-balloon group (14.4 ± 6.1 g; P < 0.01). The total amount of 10% EO, including additional administration, was 11.2 ± 6.6 g in the Coaxial group, which was also lower, but not significantly different than that in the Single-balloon group (P = 0.184). The mean required time until the injection of sclerosant was 83.8 ± 49.8 min in the Coaxial group, which was almost similar to that in the Single-balloon group (85.3 ± 42.6 min, P = 0.946). The cost of devices required for the BRTO procedure was 25.0 ± 14.2 × 104 yen in the Coaxial group, which was not significantly different from that in the Single-balloon group (18.4 ± 18.3 × 104 yen, P = 0.288) (Table 3).
Success rate of sclerosant stagnation and obstruction of the gastric varices and/or the gastro-renal shunt
The success rate of sclerosant stagnation, which is essential for successful obstruction, was 94.4% (17/18) in the Coaxial group and 86.7% (13/15) in the Single-balloon group. There was no significant difference between the two groups (P = 0.579). Successful obstruction was seen in all the patients in whom the sclerosant was successfully stagnated except for one patient in each group. One patient in the Coaxial group who discontinued BRTO due to vascular injury showed a disappearance of blood flow in the gastric varices on CECT one week after BRTO. Therefore, the successful obstruction rate was 94.4% (17/18) in the Coaxial group and 80.0% (12/15) in the Single-balloon group.
Safety
Major complications were seen in two patients in the Coaxial group and one patient in the Single-balloon group (Table 4). BRTO had to be discontinued due to vascular injury that occurred during 0.035-inch guidewire manipulation to advance a balloon catheter in one patient in each group. In one patient in the Coaxial group, increased ascites was seen that was probably be due to the elevation of portal vein pressure caused after BRTO and required additional diuretics. In both groups, no one showed acute renal failure. There was no significant difference in the frequency of complications between the two groups (P = 1.00).
Discussion
The present study showed that the frequency of additional procedures (including embolization with coil or ethanol injection, or occlusion using an additional balloon catheter for collateral draining veins) for sclerosant stagnation during a BRTO could be reduced using a coaxial double balloon catheter as compared to using a single-balloon catheter.
BRTO is a very effective procedure for preventing gastric varices and hepatic encephalopathy caused by portosystemic shunt [12], but obstruction of the gastric varices and/or the gastro-renal shunt failed in approximately 10% of the patients [13]. The causes of technical failure in BRTO procedures were reviewed and classified into five types: (1) inability to insert the balloon catheter into the gastro-renal shunt, (2) inability to occlude the gastro-renal shunt due to undersized balloon, (3) inability to stagnate sclerosant sufficiently in the gastric varices due to the outflow of sclerosant through collateral draining veins, (4) vascular injury during the procedure, and (5) balloon rupture during BRTO. Among them, the inability to stagnate the sclerosant was the most common cause of technical failure [13]; therefore, to improve the rate of successful obstruction by BRTO, preventing the outflow of sclerosant through collateral draining veins is important. Advancement of a balloon catheter over the branch point of the collateral draining veins is an easy and effective way to prevent the outflow of the sclerosant; however, it is often difficult due to the complex form of the gastro-renal shunt. In a large cohort study, the advancement of the balloon catheter could be performed in only 16.5% of the patients [14], and other patients needed additional procedures including embolization of the collateral draining veins using ethanol or coil, and balloon occlusion of the collateral draining vein by using another balloon catheter. In the current study, only 22.2% (4/18) of patients in the Coaxial group needed additional procedures, which is significantly lower than that in the Single-balloon group. A previous study showed almost similar results with 2 of 8 patients needing additional procedures during BRTO with a coaxial balloon catheter [5]. In cases with Hirota’s grade 1 or 2, BRTO can be easily performed without additional procedures even using a single-balloon catheter. However, in cases with Hirota’s grade 3 or 4, the use of a coaxial balloon catheter can reduce the frequency of additional procedures and make the BRTO procedure simpler. As the gastro-renal shunt was tortuous, it took time to advance the balloon catheter to the proximal part of the gastro-renal shunt when using a coaxial double balloon catheter; therefore, the required time until the injection of the sclerosant in the Coaxial group was almost the same as that in the Single-balloon group. Further, the cost of a coaxial double balloon catheter is almost nine times higher than a single-balloon catheter. Therefore, although the frequency of costly additional procedures such as occlusion by using coils or a micro-balloon catheter was lower in the Coaxial group than in the Single-balloon group, the total cost of the devices required for the BRTO procedure was not significantly different. However, the simplification of the BRTO procedure using a coaxial double balloon catheter is clinically significant. Although BRTO is an effective treatment for gastric varices, the procedures involved are complex; therefore, endoscopic treatment is applied as an alternative treatment for gastric varices in hospitals that lack the expertise [3]. However, the efficacy of endoscopic treatment is lower than that of the BRTO [15]. Our study shows that a coaxial balloon catheter is useful for the simplification of the BRTO procedure, especially in patients with complex gastro-renal shunt. Therefore, using coaxial balloon catheter, practicing clinicians can perform BRTO more easily in patients with gastric varices and expect better clinical outcomes.
Although there is no evidence, a study suggested that a coaxial balloon catheter could possibly have an additional advantage of reducing the required amount of EO to fill the gastric varices and/or gastro-renal shunt because of the capability of balloon of the guiding catheter to occlude the collateral vessels [5]. The current study showed that the required amount of EO in the Coaxial group was lower, but not significantly different than that in the Single-balloon group.
The successful obstruction of gastric varices using the coaxial method was 94.4%. The occlusion time was one of the important factors for obtaining successful obstruction of the gastric varices and/or the gastro-renal shunt [8]. In the current cohort, overnight occlusion was applied at the same time as the introduction of the coaxial balloon catheter. Therefore, the superiority or inferiority of the treatment efficacy between the two groups could not be concluded from the results. However, at least, the success rate of obstruction using a coaxial double balloon catheter was proved to be almost equivalent to that using a single-balloon catheter in the current study and a previous study [2]. For safety, the rate of complications was not different between the Coaxial and the Single-balloon groups. The rate of major complications was reported to be 4.7% for BRTO in a previously published meta-analysis [2]. In this study, a major complication occurred in 2 of 18 patients (11.1%) in the Coaxial group and 1 of 15 (6.7%) patients in the Single-balloon group. The rate in coaxial group of the present study was relatively higher than that by Tanou et al. who reported no procedure-related complication in the eight patients during BRTO with a coaxial balloon catheter system [5]. The complication rate in the Coaxial group in this study was relatively higher than the study by Tanoue et al. However, the number of patients was small in both the studies; therefore, further investigations are needed to evaluate the safety of the coaxial catheter.
There are several limitations to the current study. First, the present study is retrospective; therefore, selection bias cannot be excluded. However, after the introduction of a coaxial method, all but one patient was treated with the coaxial balloon; thereby, weakening the selection bias. Second, there is a possibility of the influence of the learning curve effect on the outcome. To minimize this influence, two cases in whom BRTO was performed by the operators who had the experience of performing procedures less than three times were excluded. There has been no report on the learning curve effect in the BRTO procedure; therefore, the number of procedures an operator should perform before achieving the efficiency to perform BRTO skillfully with clinically reasonable outcomes is unknown. Because the success and complication rate of BRTO were not much different irrespective of the number of cases [2], the learning curve is considered to be steep. However, the learning curve effect could not be excluded completely. To confirm our results, a prospective randomized study is needed. Third, venography was performed by manual injection of contrast medium gently and slowly, which resulted in a different injection speed in each patient.
Conclusion
Using a coaxial, double balloon catheter, the frequency of additional procedures required to stagnate the sclerosant during BRTO could be reduced as compared to that using a single-balloon catheter.
References
Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–9.
Park JK, Saab S, Kee ST, Busuttil RW, Kim HJ, Durazo F, et al. Balloon-occluded retrograde transvenous obliteration (BRTO) for treatment of gastric varices: review and meta-analysis. Dig Dis Sci. 2015;60:1543–53.
Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310–35.
Kobayakawa M, Kokubu S, Hirota S, Koizumi J, Nishida N, Yasumoto T, et al. Short-term safety and efficacy of balloon-occluded retrograde transvenous obliteration using ethanolamine oleate: results of a prospective, multicenter. Single-Arm Trial J Vasc Interv Radiol. 2017;28:1108–15.
Tanoue S, Kiyosue H, Matsumoto S, Hori Y, Okahara M, Kashiwagi J, et al. Development of a new coaxial balloon catheter system for balloon-occluded retrograde transvenous obliteration (B-RTO). Cardiovasc Intervent Radiol. 2006;29:991–6.
Saad WEA, Kitanosono T, Koizumi J, Hirota S. The conventional balloon-occluded retrograde transvenous obliteration procedure: indications, contraindications, and technical applications. Tech Vasc Interv Radiol. 2013;16(2):101–51.
Hirota S, Matsumoto S, Tomita M, Sako M, Kono M. Retrograde transvenous obliteration of gastric varices. Radiology. 1999;211:349–56.
Kakutani H, Sanada J, Nakayama D, Moriyasu F. Catheter-retaining balloon-occluded retrograde transvenous obliteration for gastric varices. J Nippon Med Sch. 2014;81:298–304.
Khwaja A. KDIGO Clinical practice guidelines for acute kidney injury. Nephron. 2012;120(4):c179-184.
Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of interventional radiology clinical practice guidelines. J Vasc Interv Radiol. 2003;14:S199-202.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Fukuda T, Hirota S, Sugimura K. Long-term results of balloon-occluded retrograde transvenous obliteration for the treatment of gastric varices and hepatic encephalopathy. J Vasc Interv Radiol. 2001;12:327–36.
Saad WEA, Sabri SS. Balloon-occluded retrograde transvenous obliteration (BRTO): technical results and outcomes. Semin Intervent Radiol. 2011;28(3):333–8.
Imai Y, Nakazawa M, Ando S, Sugawara K, Mochida S. Long-term outcome of 154 patients receiving balloon-occluded retrograde transvenous obliteration for gastric fundal varices. J Gastroenterol Hepatol. 2016;31:1844–50.
Hong CH, Kim HJ, Park JH, Park DI, Cho YK, Sohn CI, et al. Treatment of patients with gastric variceal hemorrhage: endoscopic N-butyl-2-cyanoacrylate injection versus balloon-occluded retrograde transvenous obliteration. J Gastroenterol Hepatol. 2009;24:372–8.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Ethics Committee at Nagoya University Hospital approved this study (approval no. 2019-0086), which proceeded according to the principles of the Declaration of Helsinki (1975). Due to the retrospective nature of the study, the need for obtaining informed consent was waived off by the Ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Ishizu, Y., Ishigami, M., Honda, T. et al. Simplification of balloon-occluded retrograde transcatheter obliteration procedure using a coaxial double balloon catheter compared with a single-balloon catheter. Jpn J Radiol 39, 296–302 (2021). https://doi.org/10.1007/s11604-020-01060-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-020-01060-x