Abstract
Improvements in positron emission tomography (PET) technology have contributed to increased diagnostic accuracy in patients with large-vessel vasculitis (LVV) over the last decades. Many systematic reviews and meta-analyses were conducted, and earlier diagnosis by 18F-FDG PET can be made in patients suspected of having LVV. Two subtypes, Takayasu arteritis and giant cell arteritis, will progress when poorly responding to corticosteroids and augmented immunosuppression. In most patients, disease activity cannot be monitored by laboratory tests alone; therefore, glucose metabolism may be a source for possible biomarkers. In this review, we present current concepts regarding 18F-FDG PET/CT imaging standards.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vasculitis is a heterogeneous group of disorders characterized by inflammation and fibrinoid necrosis of blood vessel walls. Large vessel vasculitis (LVV) is a disease predominantly affecting the large arteries and main branches. Pathologic specimens from patients show granulomatous infiltration of various inflammatory cells within the vessel walls of the thoracic and abdominal aorta and their branches. Patients with LVV often present with nonspecific clinical symptoms including fatigue, malaise, weight loss, anorexia, fever, and night sweats. Two subtypes, Takayasu arteritis (TA) and giant cell arteritis (GCA), are known. In most patients, the development of LVV is a progressive process that is an inefficient and impermanent response to treatment. Diagnostic procedures including ultrasound, computed tomography, magnetic resonance imaging, and angiography often give inconclusive results in patients with LVV [1,2,3,4]. 18F-FDG PET/CT can detect the activated inflammatory process within the arterial wall and may be valuable for initial diagnosis, monitoring of disease activity, and evaluating response to treatment in LVV [5, 6]. In this review, we present current concepts regarding the 18F-FDG PET/CT of LVV.
Pathogenesis and cellular mechanism of LVV
LVV is regarded as two pathologic conditions: GCA and TA. GCA is the most common reason for idiopathic LVV in patients aged greater than 50 years and affects mainly the thoracic, abdominal aorta, and its primary branches. Its etiology and pathogenesis are still unknown. Classic cranial manifestations consist of headache, scalp tenderness, jaw claudication, and vision loss. Temporal artery biopsy remains the gold standard for diagnosis. Steroid treatment is the standard of care, though not curative. Genes in HLA type 2 region affect GCA’s development. An imbalance among CD4 + T helper (Th)1, Th17, and regulatory T cells contribute to the pathogenesis of GCA. Tocilizumab, a monoclonal antibody against the IL-6 receptor, exerts its effects through increasing Treg cell number.
TA is a rare granulomatous pan-arteritis with female predominance and an estimated incidence of 2 per 1 million persons. The mean age of onset is 35 years and regions of highest prevalence are in Asia. TA can cause late complications including stenoses, occlusions, and aneurysms and can be life-threatening, with mortality rates reaching 35% at 5 years after diagnosis.
The realization that arterial wall inflammation results in LVV has led to a search for inflammatory mediators. M1 macrophages activated by IFN-γ produce inflammatory cytokines, and a dominant subset of M1 macrophages in lesions play a role in the inflammatory amplification loop in LVV. M2 macrophages, recognized as the anti-inflammatory and tissue-repair macrophage subtype, consist of four subtypes. Of these, the M2d subset induced by IL-6 is considered to be important in the pathogenesis of LVV, because the serum level of IL-6 is high in patients with LVV [7]. Both of M1 and M2 macrophages are significantly expanded in inflamed arteries in LVV.
Diagnostic accuracy and staging
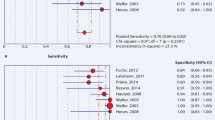
Activated macrophages and lymphocytes within the arterial wall overexpress the transporters (Glut-1 and Glut-5) of glucose destined to undergo glycolysis. 18F-FDG is readily taken up by these cells. 18F-FDG PET/CT has proven to be an efficient tool for LVV diagnosis. The diagnosis of LVV can be made histologically, but the histologic proof is usually difficult to obtain. Although 18F-FDG is nonspecific because it is taken up by other proliferating cells, 18F-FDG PET/CT can detect increased metabolism and functional changes before morphological transformations become apparent. It has been shown that baseline 18F-FDG PET/CT performed prior to the initiation of steroid therapy can be used to render an accurate diagnosis [8,9,10,11]. Similarly, the performance of baseline 18F-FDG PET/CT provides a means of staging LVV. This strategy may eventually prove useful for LVV diagnosis prior to treatment. Therefore, the cost of FDG-PET imaging was covered by insurance since March 2018 in Japan. Two studies, a systematic review and meta-analysis, have been published on the diagnostic accuracy of FDG PET and the diagnostic accuracy of PET/CT [8, 9]. The results of each study are summarized in Table 1. Populations in most studies were patients with GCA or GCA/TA. The pooled sensitivity and specificity for diagnostic purposes were 87–90% and 73–98%, respectively. When stratified by TA, the diagnostic performance was similar.
18F-FDG PET/CT protocol
Procedurally, it is recommended that patients fast for at least 6 h prior to 18F-FDG administration and have serum glucose levels below 7 mmol/L (126 ml/dL) [10, 11]. Glucocorticoid treatment results in attenuation of 18F-FDG uptake in patients with LVV. However, Nielsen BD and colleagues demonstrated in a prospective cohort study that 18F-FDG PET/CT is not compromised by a 3-day course of 60 mg glucocorticoid treatment [12]. They concluded that the sensitivity of 18F-FDG PET/CT is higher in glucocorticoid-naïve than in treated patients with LVV, but within 3 days of glucocorticoid treatment, the attenuation effect is limited. For adequate biodistribution, the acquisition should be started 60 min after intravenous administration of 18F-FDG. For the purpose of discrimination from atherosclerotic plaque accumulation, a 120-min interval is recommended [10, 11]. Contrast-enhanced 18F-FDG PET/CT is reported useful for identifying stenosis in patients with TA, but the data are insufficient to support routine use [13]. Resolution of the PET scanner limits detection in the large vascular system. Therefore, time-of-flight (TOF) reconstruction and digital PET/CT are preferable for high-resolution images. Although many meta-analyses of the diagnostic accuracy of 18F-FDG PET/CT for LVV have been published, most of the data are from analog PET/CT scanners. Digital PET/CT can provide us with better image quality, more precise SUV, and improved tracer detectability as compared to analog PET/CT. Since digital PET/CT allows faster TOF technology and coupling between the scintillation crystal and detector and digital photon counting on a one-to-one basis, this technique results in better spatial resolution and sensitivity gain to enable detection of subtle differences in vascular uptake. On the other hand, better sensitivity also results in false-positive findings on digital PET/CT. The difference between the diagnostic performance of digital PET/CT should be addressed on the basis of comparative study with analog PET/CT and cost-effectiveness.
18F-FDG PET/CT interpretation
In 2016, a committee sponsored by the American Heart Association proposed an LVV visual grading scale based on the comparison between vascular uptake and liver uptake [14]. The use of a single visual grading scale is helpful for comparisons between several different institutions because many criteria have been proposed for visual analysis [0, no uptake (≤ mediastinum); 1, low-grade uptake (< liver); 2, intermediate-grade uptake (= liver), 3, high-grade uptake (> liver)]. Grade 2 and grade 3 indicate “possible” and “definite” active inflammation, respectively (Fig. 1). On the basis of visual analysis, 18F-FDG PET and PET/CT have high accuracy, with a meta-analytic pooled sensitivity of 84% and meta-analytic pooled specificity of 84% for TA and 89% and 98% for GCA [8]. When the visual scale is applied, type of uptake including linear, segmental, and focal should be taken into account.
Assessment of 18F-FDG PET images by using the visual scoring grade system. The visual grading scale consists of 4 grades: 0, no uptake (≤ mediastinum); 1, low-grade uptake (< liver); 2, intermediate-grade uptake (= liver), and 3, high-grade uptake (> liver). Grade 2 and grade 3 indicate “possible” and “definite” active inflammation, respectively (arrows)
A reproducible metric of 18F-FDG accumulation in the vascular wall has been introduced. Semiquantitative analysis includes basic SUV parameters and target-to-background ratio (TBR) (Fig. 2). However, simple SUV metrics are not preferable because of the overlap between LVV and atherosclerosis. TBR is calculated as the ratio between SUVmax of the vascular wall and SUVmean of the blood pool in the inferior vena cava or internal jugular vein. Arterial wall uptake normalized to the background activity of the blood pool is a good reference for assessing vascular inflammation. Liver and lung are known to be favorable target organs for normalization using TBRs. The sensitivity and specificity are 90% and 94% for liver and 82% and 73% for lung, respectively [15].
Versari and colleagues introduced the total vascular score (TVS), which they measured in seven vascular districts (carotid, subclavian, axillary, iliac, femoral, thoracic aorta, and abdominal aorta) [3, 16]. Uptake is scored from 0 to 3 in each district based on intensity, and uptake is maximum when the score is 21. A TVS greater than or equal to 6 is specific for the presence of disease.
Grayson PC and colleagues created the PET Vascular Activity Score (PETVAS) which can be used to qualitatively assess vascular uptake in arterial territories [17]. Four segments of the aorta (ascending, arch, descending thoracic, and abdominal) and 11 branch arteries (innominate, carotid, subclavian, axillary, iliac, and femoral) are evaluated from the degree of 18F-FDG accumulation relative to liver uptake (0, no uptake; 1, less than liver uptake; 2, same as liver uptake; 3, greater than liver uptake). The summary score is the total of the qualitative scores in specific arterial territories. Other reproducible metrics to quantify 18F-FDG uptake within arterial walls have been developed; however, the summation of all vascular districts or territories is complicated without any standardization of volumetry [18, 19].
Although 18F-FDG PET/CT is valuable for initial diagnosis, monitoring of disease activity, and for evaluating treatment response in LVV, the atherosclerotic vascular uptake may complicate interpretation in elderly patients. Distinction between LVV and atherosclerosis is difficult, but some characteristics can be distinguished from the pathological background. Atherosclerotic lesions are typically skip lesions that show a patchy uptake pattern, while inflammatory lesions of LVV demonstrate a smooth linear pattern. Surgical intervention is needed when there are complications of LVV including aneurysm and severe stenosis. Graft stenting is a possible procedure for such complications. However, significant 18F-FDG uptake confined to arterial graft sites in patients with LVV does not reflect clinically relevant disease activity or progression. When heterogeneous and focal 18F-FDG uptake are identified, it may indicate infected grafts. Visual assessment of 18F-FDG uptake compared with that of inactive muscle and fat, or that of the liver, are shown to be useful for detection of infected grafts.
Polymyalgia rheumatica (PMR) and GCA frequently overlap. 18F-FDG uptake in extravascular regions should be carefully examined. PMR patients often show FDG uptake in glenohumeral synovia, subacromial-subdeltoid bursa, supraspinatus tendinitis and biceps synovitis (shoulder), trochanteric/ischial bursa, hip synovia, interspinous regions of the cervical and lumbar vertebrae, or the synovial tissue of the knees [20]. 18F-FDG uptake of extravascular regions also reflect disease activity.
Response evaluation as biomarker
Current treatment of LVV consists primarily of augmenting immunosuppression by changing or adding medications. Several medications and immune-modulating treatments have been introduced to stabilize the inflammatory reaction in LVV. Glucocorticoid is the initial choice of treatment in most cases, but relapse happens commonly and adverse effects including diabetes mellitus, osteoporosis, and infection are often observed. Methotrexate and cyclophosphamide are possible medications to switch to, and seem to be associated with a lower risk of relapse albeit with treatment-related adverse events. Tocilizumab, the IL-6 receptor directed monoclonal antibody, is a milestone in the induction and maintenance of remission in patients with GCA. 18F-FDG PET/CT is currently used for monitoring LVV as a biomarker. Vitiello G and colleagues evaluated 12 patients with GCA receiving glucocorticoid and tocilizumab (8 mg/kg/month) [21]. All patients achieved complete remission after initiation of tocilizumab and mean SUV decreased significantly on 18F-FDG PET/CT. Although encouraging, the results were from a limited number of patients enrolled at a single institution, and the time to post-treatment 18F-FDG PET/CT varied widely; therefore, 18F-FDG PET/CT might be useful for monitoring treatment response because it can detect metabolic changes even if asynchronous with levels of several laboratory parameters.
The presence of significant 18F-FDG uptake on post-treatment PET/CT images is an accurate indicator of disease activity in LVV. From the previous results of a case–control study, the sensitivity and specificity of active vasculitis detection by 18F-FDG PET/CT were 85% (95%CI: 69–94%) and 83% (71–91%), respectively [22]. Most patients with LVV in clinical remission showed significant 18F-FDG uptake on PET/CT and these findings are suggestive of future clinical relapse. The results from recent prospective studies in large populations are summarized in Table 2.
Prognostic implication
Patients with LVV have an increased risk of aortic dilatation, aortic aneurysm, and aortic dissection, which have a close relationship with mortality (Fig. 3). Prediction of disease course by 18F-FDG PET/CT has not been fully elucidated to date. Dellavedova et al. demonstrated that 18F-FDG PET/CT can predict favorable progress in patients with LVV [23]. Total lesion glycolysis (TLG) was significantly higher in patients with complicated progress than in those with favorable progress. Muratore F and colleagues conducted a longitudinal case–control study using 18F-FDG PET/CT follow-up with a mean time of 35 months [24]. Diameters of ascending, descending, and suprarenal abdominal aortas showed a significant increase compared to control. A notable predictor of aortic dilatation was significant 18F-FDG uptake at baseline on PET/CT scans in patients with GCA. However, this trend was not observed in patients with TA. Although 18F-FDG PET/CT can predict prognosis in patients with LVV, important limitations of these previous studies include the retrospective nature of the analyses, mixed population of patients with LVV, and duration of follow-up that was too short to observe aortic dilatation or dissection. It will therefore be necessary to conduct a prospective study using a homogeneous treatment regimen with longer follow-up.
Conclusion
8F-FDG PET/CT has an important role to play in the diagnosis, response assessment, and prognosis of LVV. Distinction between LVV and other conditions with significant vascular uptake should be considered for initial diagnosis. The optimization of 18F-FDG PET/CT procedures is necessary before a reproducible metric can be used to quantify 18F-FDG accumulation in the vascular wall.
References
Myklebust G, Gran JT. A prospective study of 287 patients with polymyalgia rheumatic and temporal arteritis: clinical and laboratory manifestations at onset of disease and at the time of diagnosis’. Br J Rheumatol. 1996;35:1161–8.
Treglia G, Mattoli MV, Leccisotti L, et al. Usefulness of whole body fluorine-18-fluorodeoxyglucose positron emission tomography in patients with large-vessel vasculitis: a systematic review. Clin Rheumatol. 2011;30(10):1265–75.
Versari A, Pipitone N, Casali M, Jamar F, et al. Use of imaging techniques in large vessel vasculitis and related conditions. Q J Nucl Med Mol Imaging. 2018;62(1):34–9.
Duftner C, Dejaco C, Sepriano A, Falzon L, Schmidt WA, Ramiro S. Imaging in diagnosis, outcome prediction and monitoring of large vessel vasculitis: a systematic literature review and meta-analysis informing the ULAR recommendations. RMD Open. 2018;4:e000612.
Incerti E, Tombetti E, Fallanca F, Baldissera EM, Alongi P, Tombolini E, et al. (18)F-FDG PET reveals unique features of large vessel inflammation in patients with Takayasu’s arteritis. Eur J Nucl Med Mol Imaging. 2017;44(7):1109–18.
Barra L, Kanji T, Malette J, Pagnoux C. CanVasc. Imaging modalities for the diagnosis and disease activity assessment of Takayasu’s arteritis: A systematic review and meta-analysis. Autoimmun Rev. 2018;17:175–87.
Jiemy WF, Heeringa P, Kamps JAAM, van der Laken CJ, Slart RHIJ, et al. Positron emission tomography (PET) and single photon emission computed tomography (SPECT) imaging of macrophages in large vessel vasculitis: current status and future prospects. Autoimmun Rev. 2018;17:715–26.
Soussan M, Nicolas P, Schramm C, Katsahian S, Pop G, Fain O, et al. Management of large-vessel vasculitis with FDG-PET: a systematic literature review and meta-analysis. Medicine (Baltimore). 2015;94(14):e622.
Lee SW, Kim SJ, Seo Y, Jeong SY, Ahn BC, Lee J. F-18 FDG PET for assessment of disease activity of large vessel vasculitis: a systematic review and meta-analysis. J Nucl Cardiol. 2019;26(1):59–67.
Slart RHJA, Glaudemans AWJM, Chareonthaitawee P, Treglia G, Besson FL, Bley TA, Blockmans D, et al. FDG-PET/CT(A) imaging in large vessel vasculitis and polymyalgia rheumatica: joint procedural recommendation of the EANM, SNMMI, and the PET Interest Group (PIG), and endorsed by the ASNC. Eur J Nucl Med Mol Imaging. 2018;45:1250–69.
Dejaco C, Ramiro S, Duftner C, Besson FL, Bley TA, Blockmans D, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis. 2018;77:636–43.
Nielsen BD, Gormsen LC, Hnsen T, Keller KK, Therkildsen P, Hauge EM. Three days of high-dose glucocorticoid treatment attenuates large-vessel 18F-FDG uptake in large-vessel giant cell arteritis but with a limited impact on diagnostic accuracy. Eur J Nucl Med Mol Imaging. 2018;45:1119–28.
Olthofa SC, Krumma P, Henesb J, Nikolaoua K, la Fougèrec C, Pfannenberga C, et al. Imaging giant cell arteritis and aortitis in contrast enhanced 18F-FDG PET/ CT: Which imaging score correlates best with laboratory inflammation markers? Eur J Radiol. 2018;99:94–102.
Buttgereit F, Dejaco C, Matteson EL, Dasgupta B. Polymyalgia rheumatica and giant cell arteritis: a systematic review. JAMA. 2016;315:2442–58.
Hautzel H, Sander O, Heinzal A, Schneider M, Muller HW. Assessment of large-vessel involvement in giant cell arteritis with 18F-FDG PET: introducing an ROC-analysis-based cutoff ratio. J Nucl Med. 2008;49:1107–13.
Soriano A, Pazzola G, Boiardi L, Casali M, Muratore F, Pipitone N, et al. Distribution patterns of 18F-fluorodeoxyglucose in large vessels of Takayasu’s and giant cell arteritis using positron emission tomography. Clin Exp Rheumatol. 2018;36:S99–106.
Grayson PC, Alehashemi S, Bagheri AA, Civelek AC, Cupps TR, Kaplan MJ, et al. 18F-Fluorodeoxyglucose-positron emission tomography as an imaging biomarker in a prospective, longitudinal cohort of patients with large vessel vasculitis. Arthritis Rheumatol. 2018;70:439–49.
Emsen B, Benalia K, Mahidaa B, Larivièreb D, Le Guludeca D, Papob T, et al. Comparison between visual and numerical metrics for the evaluation of patients with Takayasu arteritis with 18F-FDG-PET. Nucl Med Commun. 2018;39:779–88.
Rodríguez IM, Alonso M, Quirce R, Bonilla JJ, Amador NM, Pha MT, et al. 18F-FDG PET/CT in the follow-up of large-vessel vasculitis: a study of 37 consecutive patients. Semin Arthritis Rheum. 2018;47:530–7.
Yuge S, Nakatani K, Yoshino K, Koyama T. Diagnosing polymyalgia rheumatica on 18 F-FDG PET/CT: typical uptake patterns. Ann Nucl Med. 2018;32:573–5677.
Vitiello G, Battaglini CO, Carli G, Radice A, Matucci A, Vultaggio A, et al. Tocilizumab in giant cell arteritis: a real-life retrospective study. Angiology. 2018;69:763–9.
Banerjee S, Quinn KA, Gribbons KB, Rosenblum JS, Civelek AC, Novakovich E, et al. Effect of treatment on imaging, clinical, and serologic assessments of disease activity in large-vessel vasculitis. J Rheumatol. 2020;47:99–107.
Dellavedova L, Carletto M, Faggioli P, Sciascera A, Del Sole A, Mazzone A, et al. The prognostic value of baseline 18F-FDG PET/CT in steroid-naïve large-vessel vasculitis: introduction of volume-based parameters. Eur J Nucl Med Mol Imaging. 2016;43:340–8.
Muratore F, Crescentini F, Spaggiari L, Pazzola G, Casali M, Boiardi L, et al. Aortic dilatation in patients with large vessel vasculitis: a longitudinal case control study using PET/CT. Semin Arthritis Rheum. 2019;48:1074–82.
Acknowledgements
We gratefully appreciate the cooperation of the following members, Jun Isogai, MD, PhD, Asahi General Hospital and Yoichi Machida, MD, PhD, Kameda Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Tateishi, U., Tsuchiya, J. & Yokoyama, K. Large vessel vasculitis: imaging standards of 18F-FDG PET/CT. Jpn J Radiol 39, 225–232 (2021). https://doi.org/10.1007/s11604-020-01059-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-020-01059-4