Abstract
Purpose
Our aim was to assess computed tomography (CT) features of Mycobacterium kansasii pulmonary infection (M. kansasii infection).
Materials and methods
A total of 29 cases confirmed to have M. kansasii infections were analyzed. The main locations of pulmonary changes, incidence, and various imaging features of the cavity (location, maximum diameter, wall thickness, satellite nodules, intracavitary fluid), and other imaging findings such as nodules, consolidation, and bronchiectasis, were visually assessed on CT images.
Results
Locations of the main abnormalities were as follows: right S2 41%; right S1 31%; left S1+S2 2: 21%. A total of 49 cavities were observed in 24 (83%) cases. The mean maximum diameter, wall thickness, and ratio of wall thickness to the maximum diameter were 33.0 mm, 4.7 mm, and 0.19, respectively. Shapes of the cavities were round in nine (18.4%), oval in 17 (34.7%), and tubular/meandering in 23 (47%). Satellite nodules were found in only 30.6% of patients (n = 15). Small nodules were found in 26 (89.7%) patients, and most of them showed a centrilobular distribution.
Conclusion
The characteristic CT findings suggestive of M. kansasii infection include cavities located in the right posterior or apical segment with a tubular/meandering shape and a thin wall.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Mycobacterium kansasii is the second most common nontuberculous mycobacterium after M. avium–intracellulare complex [1–5]. The incidence of M. kansasii is largely dependent on geographical factors and the highest incidence in the southern and central USA, the UK, and western Europe [2–4, 6, 7]. Clinical symptoms of M. kansasii are similar to those of M. tuberculosis; however, patient handling is completely different because M. kansasii is not contagious and there is no need for patient isolation [2–5]. Although M. kansasii is considered most virulent among the nontuberculous mycobacteria, its sensitivity to antibiotics is high, and the prognosis is good with appropriate treatment [3, 5, 7, 8]. Therefore, early and correct diagnosis of M. kansasii is clinically important.
Imaging has a major role in diagnosing M. kansasii infection; however, previous reports have dealt mainly with radiographic findings [2–6, 8, 9]. To our knowledge, computed tomography (CT) findings of M. kansasii infection have seldom been comprehensively reported [10, 11]. The purpose of this study was to review the CT findings in 29 patients with M. kansasii pulmonary infection and to validate the classic radiographic appearances on CT images.
Materials and methods
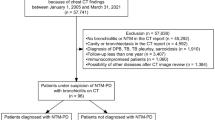
This retrospective study assessed 37 consecutive patients with a diagnosis of M. kansasii lung infection from December 2001 to November 2009 at the two regional referral centers for pulmonary diseases. The diagnosis of M. kansasii infection was based on guidelines from The Nontuberculous Mycobacteriosis Control Committee of the Japanese Society for Tuberculosis, which were revised in 2008 [12] to comply with the guidelines of the American Thoracic Society published in 2007 [13]. Among the 37 cases, eight were excluded from this study because CT images were missing (n = 4), co-infection was established within 6 months from the time of the CT examinations (two M. tuberculosis, one Pneumocystis jirovecii), or advanced bronchogenic carcinoma coexisted (n = 1). Finally, 29 patients (25 men, 4 women) were included. The average patient age at the time of diagnosis was 57 (range 28–79) years. Chief complaints were abnormal finding on chest radiograph at regular health checkup (n = 14), cough/sputum (including hemosputum) (n = 11), chest pain (n = 2), dyspnea (n = 1), and fever (n = 1). Smoking histories were current smokers n = 20, mean pack-year 47; ex-smokers n = 2, mean pack-year 26; and never smokers n = 7. Although two cases were complicated with localized bronchogenic carcinoma at the time of CT, there were no clinical and radiological findings suggesting metastases either in the lung or lymph nodes, which were confirmed by the follow-up examinations. One patient had a history of radiation therapy for bronchogenic carcinoma; however, there was no clinical or radiological evidence suggesting local recurrence or metastasis at the time of CT. Three patients also had histories of extrathoracic malignancy; however, there was no clinical and radiological evidence suggesting local recurrences or metastases at the time of CT. Three patients had histories of exposures to silica and three of treatment for M. tuberculosis; however, there were no clinical and bacteriological findings suggesting active tuberculosis. Two patients had diabetes mellitus and one had chronic hepatitis. Eleven patients had two or more sputum specimens that yielded positive cultures for M. kansasii. Fourteen cases had bronchial lavage specimens obtained via fiberoptic bronchoscopy that yielded cultures positive for M. kansasii. In three cases, specimens were obtained by percutaneous fine-needle aspirations. In one case, the specimen was obtained by video-assisted thoracic biopsy. All patients underwent chest radiographs and CT scans. The interval between sample collection and initial CT examinations ranged from 0 to 129 (mean 20.4) days, and no patients performed CT scans before treatment for M. kansasii. Our institutional review board approved the execution of this study. Informed consent from each patient was waived because this was a retrospective analysis.
Imaging technique
Chest CT examinations were performed with the following scanners: HiSpeed Dxi, ProSpeed F1 (both General Electric Healthcare, Milwaukee, WI, USA), Aquilion 16, or Aquilion 64 (both Toshiba Medical Systems, Otawara, Tochigi). Contiguous 7- or 10-mm-thick slices of the entire thorax were obtained in a single breath-hold at the end of full inspiration (120 kVp, 110–300 mA, 0.4–1.0 s/rotation). Reconstruction kernels for the lung were “bone” or “FC 52,” and those for the mediastinum were “standard” or “FC14.” In 16 patients, additional high-resolution CT (HRCT) images (2-mm thick with an interval of 2–10 mm) were obtained. The reconstruction kernels for HRCT were “bone” or “FC 52.” Images were obtained with lung window settings [width 1,500–1,800 Hounsfield units (HU); level −500 to −700 HU] and with mediastinal window settings (width 350–500 HU; level 20–40 HU).
Review of CT scans
All CT scans were reviewed by two experienced chest radiologists (27 and 23 years of experience) who were aware that all patients had proven M. kansasii infection; the final decision on the findings was reached by consensus. Measurement analysis on CT images was performed by one chest radiologist.
Most severely affected segment
Observers identified the segment that was most severely involved. If multiple segments were involved to a similar extent, all of those segments were recorded as the most strongly involved. Pulmonary changes included cavities, nodules, consolidation. and bronchiectasis. Observers assessed the following morphological changes in the thorax and the associated condition of the lung.
Cavity
The number and location of cavities were assessed. A cavity was defined as a gas-filled space, seen as a lucency or low-attenuation area, within pulmonary consolidation; a mass; or a nodule with a wall thicker than 1 mm. The shape of the cavity was classified as round, oval, or tubular/meandering (Figs. 1, 2, 3, 4). This classification was determined at the transverse level of the maximum diameter. If the ratio of two orthogonal diameters was <1.2, it was classified as round; if it was >1.2, it was classified as oval. If the shape of the cavity was irregularly extended or displayed a twisted tubular-like structure, it was classified as tubular/meandering. The appearance of the cavity wall was subjectively classified as even or uneven. The presence of fluid in the cavity was also assessed. Whether the satellite nodules were present or not was assessed. Satellite nodules were defined as multiple small nodules concentrically surrounding the cavity and found within an area with a length equivalent to the diameter of the cavity. The morphometry of the cavity, including maximum diameter, maximum wall thickness, and ratio of maximum wall thickness to maximum diameter, was also evaluated.
Nodules
The existence of the nodular lesions was assessed. The nodules were classified as large (>1 cm in diameter) or small (<1 cm in diameter) (Fig. 5). For the small nodules, measurements were taken to determine whether or not the distribution was centrilobular (Fig. 6).
Consolidation, bronchiectasis, pleural effusion, and mediastinal lymphadenopathy
The presence of consolidation and bronchiectasis was evaluated visually (Figs. 7, 8). Bronchiectasis was defined as bronchial dilation greater than that of the accompanying pulmonary artery. Pleural effusion and mediastinal lymphadenopathy were also evaluated. Mediastinal lymphadenopathy was determined to be present if the shortest diameter was >1.5 cm for subcarinal station and 1.0 cm for other stations.
Condition of the background lung
Associated lung abnormalities such as interstitial pneumonitis and pulmonary emphysema were assessed. Interstitial abnormality was defined as ground-glass opacity with intralobular reticulation or architectural distortion, such as honeycombing of traction bronchiectasis. The degree of pulmonary emphysema in the background lung was assessed using a modified Goddard score [14]. Lung parenchyma was assessed to determine the extent of emphysema based on three levels of CT (at the level of the aortic arch, the carina, and the inferior pulmonary vein). The three CT slices were graded and scored separately for the left and right lungs, yielding a total of six lung fields. The extent of emphysema using this visual assessment method was scored on a 4-point scale. The extent score was 1 if <25% of the lung field was involved, 2 if there was 25–50% involvement, 3 for 50–75% involvement, and 4 for >75% involvement. The sum of the extent scores for the six lung fields had a possible maximum value of 24.
Statistical analysis
The correlation between the number of cavities and the size of each cavity was tested by Student’s t test. MedCalc version 11.5.1.0 (MedCalc Software, Mariakerke, Belgium) was used for these statistical analyses. A P value <0.05 was judged to be statistically significant.
Results
Most severely affected segment
The right upper lobe was involved most frequently [posterior segment (12/29: 41.4%) and the apical segment (9/29: 31.0%)]. The left apical posterior segment was the third most commonly predicted site (6/29: 20.7%).
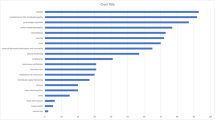
Cavity
A total of 49 cavities was observed in 24 cases (82.8%). The number of cavities varied from one to eight (average 2.04): 1 (n = 13, 54.2%), 2 (n = 7, 29.2%), 3 (n = 1, 4.2%), 5 (n = 1, 4.2%), 6 (n = 1, 4.2%), and 8 (n = 1, 4.2%). Locations of cavities are reported in Table 1. Locations involved in order of frequency were the posterior segment of the right upper lobe (29.1%), the apical segment of the right upper lobe (21.8%), and the apical posterior segment of the left upper lobe (16.4%).
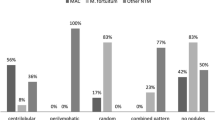
Cavity shape was categorized as follows: round 18.4% (n = 9); oval 34.7% (n = 17); tubular/meandering 47% (n = 23). In cases with tubular/meandering cavities, the course of this tubular structure had no relationship with bronchial branching and was usually observed running parallel to the chest wall. Appearance of the cavity wall was even in 69.4% (n = 34) and uneven in 30.6% (n = 15) of cases. Intracavitary fluid collection was observed in 14.3% (n = 7). In these patients, there were no clinical or bacteriological findings suggesting superinfections. Satellite nodules were observed in 30.6% (n = 15) of cavities. Maximum cavity diameter ranged from 7.1 to 100.4 mm (average 33.3 mm). Cavity size was compared with the number of cavities. Mean cavity size in the small-number group (one to two cavities) was smaller than that of the large-number group (three to eight cavities); sizes were 30.5 and 36.8 mm, respectively (P = 0.001, independent samples t test). Maximum wall thickness ranged from 0.6 to 14.6 mm (average 4.7 mm). The ratio of maximum thickness to maximum diameter ranged from 0.03 to 0.62 (average 0.19).
Nodules
Nodules were observed in 79.3% (n = 23) of cases. Small nodules were observed in 89.7% (n = 26); a centrilobular distribution was observed in 80.8%. In one case, CT showed diffusely distributed centrilobular nodules with upper lung predominance as well as the calcified hilar and mediastinal lymph nodes, which were consistent with silicosis.
Consolidation, bronchiectasis, pleural effusion, mediastinal lymphadenopathy
Consolidation and bronchiectasis were observed in 31.0% (n = 9) and 27.6% (n = 8) of patients, respectively. Consolidation was observed in a segmental or subsegmental fashion in seven cases and in a nonsegmental fashion in two cases. The presence of consolidation was not related to immune status, such as diabetes mellitus. There was no case with pleural effusion. Mediastinal lymphadenopathy was observed in only one case (3.4%). This case was considered to be silicosis, as described above.
Condition of the background lung
Interstitial abnormality was observed in 10.3% (n = 3). Pulmonary emphysema was observed in 62.0% (n = 18), and mean Goddard score was 12.3 (/24).
CT findings of the noncavitary cases
CT findings of cases without cavity formation (n = 5) were as follows: macronodule 80% (4/5), micronodule 60% (3/5), consolidation 40% (2/5), and bronchiectasis 20% (1/5). Three cases showed pulmonary emphysema; mean Goddard score was 14.
Discussion
Based on this study, CT findings related to M. kansasii infection can be summarized as follows:
-
1.
The main abnormalities were exclusively observed in the posterior and apical segments of the upper lobe; the right side was involved much more frequently than the left side.
-
2.
A cavity was observed in the majority of cases (82.8%). The shape of the cavity tended to be ovoid or tubular/meandering, and the cavity walls tended to be thin and even. Intracavitary fluid collection and satellite nodules were not frequently observed.
-
3.
Centrilobular small nodules were observed in the majority of cases.
-
4.
Incidences of bronchiectasis and consolidation were low.
-
5.
More than half of the cases had moderate or severe pulmonary emphysema.
As described above, location of pulmonary abnormalities was similar to that reported previously using radiographs [2–9]. Christensen et al. [6] reported that the disease almost always involves the upper lobes and involves the right side (72%) more often than the left (50%). Shitrit et al. [4] also reported the propensity for involvement of the right upper lobe compared with the left upper lobe in 56 cases: 86 vs. 61%. Although laterality was not mentioned, Maliwan and Zvetina [2] described that only 1% of patients (n = 3/302) had lesions that spared the upper lobes. These radiographic observations are consistent with our CT results, in which almost all lesions were located in the posterior and apical segment of the right upper lobe, followed by the posterior–apical segment of the left upper lobe. This propensity of the pulmonary lesions to affect the upper lobe in M. kansasii infection may be similar to that of M. tuberculosis [15]. Both mycobacteria are classified into the group of obligate aerobes; high oxygen tension in the apex helps M. kansasii to be preferentially localized [15]. The implication with respect to the pathogenesis of right-side predominance is still not clear.
The incidence of cavities has been considered characteristically high in M. kansasii pulmonary infection, varying from 75% [7] to 96% [6]. Our result (82.8%) was consistent with these reports. However, a recent study reported that the incidence varied from 32% [16] to 54% [4]. On CT assessment, Hollings et al. [10] reported 44% (4/9) patients had upper-lobe cavities. Several researchers have stated that this discrepancy might be explained by recent improvements in diagnosis and microbiological isolation of the organism [4, 16]. However, as shown in our results, cavities could be observed even within small nodules. Therefore, the incidence is probably not related to disease stage. There was no specific tendency of CT findings in cases without cavity formation. In such cases, it is extremely difficult to include M. kansasii in the list of differential diagnosis.
It was recently reported that patients with M. kansasii pulmonary infection can present with noncavitary or nodular/bronchiectatic lesions as major features of M. avium complex lung diseases [5, 16]. Park et al. [16] emphasized that the clinician should be aware of the various radiographic manifestations of M. kansasii lung disease. Although the incidence of bronchiectasis was low in our cases, it was reported to be high (54.5–100%) by several researchers based on CT observations [10, 11]. Up to now, the exact reason for this variation has not been clarified. Phylogenetic and molecular analyses have demonstrated that M. kansasii is a heterogeneous species with several distinct subtypes [1]. However, there have been no reports in which the relationship between species heterogeneity and imaging findings were discussed.
Among the imaging features of M. kansasii infection, cavity size and number are controversial issues. Zvetina et al. [9] stated that a single cavity <2 cm in diameter is a characteristic finding of M. kansasii pulmonary infection in comparison with M. tuberculosis. Evans et al. [7] reported that the frequency of cavity number varied, as follows: 1, 33% (n = 7/28); 2–3, 19% (4/28); 4–5, 10% (2/28); >5: 38% (8/28). Additionally, 66% (14/28) of cavities were <2 cm in diameter [7]. However, Christensen et al. [6] reported that multiple cavities were found in 88% of cases; in 69%, cavities were >2 cm in diameter. In our cases, the size of the cavity varied from 7.1 to 100.4 mm (mean 33.3 mm), and 65.5% demonstrated one or two cavities. Additionally, cavity size was significantly related to cavity number. Cavity size in the large-number group (three to eight cavities) was statistically greater than that of the group with fewer cavities (one to two cavities). Therefore, it was concluded from our study that most patients infected with M. kansasii displayed few cavities; the cavities tended to be larger in cases with multiple cavities. However, it should be noted that direct comparison between our results and previous data is impossible because our measurements were based on CT images, whereas previous measurements were derived from chest radiographs.
In this study, we measured cavity thickness and the ratio of wall thickness to cavity size using CT images. Results confirmed that cavity walls associated with M. kansasii infection tend to be thin. This is consistent with the classic description of the cavitary lesion in M. kansasii infection. Zvetina et al. [9] reported that cavity wall thickness was thin (<4 mm) in a single-cavity case. However, Christensen et al. [6] reported that thin-walled cavities were found in only 33% of patients. These authors stated that so-called classic radiographic pictures of a thin-walled cavity were not sufficient to distinguish M. kansasii from other cavitary lung diseases. The exact reason for this discrepancy is not clear; however, one possibility is the different approach to measurement: chest radiograph vs. CT. Fluid collection within the cavity was extremely rare in our cases, and this observation is in agreement with previously published descriptions [3, 6, 7].
Cavity shape was not studied previously because past observations were based on radiographic observations. Cavity shape tended to be ovoid or tubular/meandering. Although we did not compare these results with those for M. tuberculosis or other nontuberculous mycobacteria, the information can be used to characterize cavities observed in patients infected with M. kansasii. Kim et al. [17] studied the HRCT images of cavitary lesions due to M. avium–intracellulare complex infection. These authors found that 75% (18/24) of cavities had patent bronchi running into cavitary lesions [17]. They speculated that peribronchial nodules of M. avium–intracellulare complex infection evolve into inflamed focal cystic bronchiectasis and manifest as cavitary lesions [17]. In our study, this type of relationship between cavity and bronchus was not significant. Additionally, the tubular/meandering structure did not correspond to the airway course. Therefore, the mechanism of cavity formation in M. kansasii is speculated to be different from that of the M. avium–intracellulare complex. The low incidence of bronchiectasis in our study supports this speculation. However, CT images in our study were not all HRCT images; therefore, the small connections between cavities and bronchi may have been missed.
Satellite nodules were rare in our study, which is a characteristic radiographic finding related to M. kansasii infection [9]. Satellite nodules have been considered evidence for the benign nature of the solitary pulmonary nodule and are frequently observed in cases with M. tuberculosis. However, there have been no CT reports regarding the incidence of satellite nodules for various Mycobacterium infections. Therefore, it is still controversial whether this finding is a characteristic CT finding for M. kansasii infection.
Several reports have explored whether there are differences between the radiological appearances of M. kansasii and M. tuberculosis infection [2, 3, 9]. According to Evans et al. [7], radiographic abnormalities in patients with M. kansasii infection were more frequently unilateral and right-side predominant, whereas cases with tuberculosis more frequently involved the apical segment of the lower lobe. Air-space shadows including more than one bronchopulmonary segment and pleural effusions were seen less frequently in M. kansasii infection. In addition, cavitation was seen to a similar extent in patients with M. kansasii infection and in those with tuberculosis. Zvetina et al. reported on a subset of unilateral lesions with cavities <2 cm in diameter. The authors stated that a single thin-walled cavitated opacity and minimal adjacent parenchymal disease are characteristic radiographic findings related to M. kansasii pulmonary infection [9]. Although we did not compare CT findings of M. kansasii infection with those of M. tuberculosis, most of our results are consistent with previous descriptions regarding differentiation from M. tuberculosis.
The association with pulmonary emphysema was relatively high in this study, and it was also demonstrated that the degree of emphysema was usually moderate or severe. This probably reflected the high pack-year indices (current smokers 47, ex-smokers 26) of the cohort. Christensen et al. [6] and other researchers [18, 19] stated that the most important associated disease of M. kansasii pulmonary infection is chronic obstructive pulmonary disease.
There are several limitations in this study. First, results are based on a limited number of cases. This study focused mainly on validating the radiographic findings of M. kansasii using CT images and did not focus on differentiation of M. kansasii infection from other mycobacterial diseases. Statistical comparison among various mycobacterial infections should be performed on a large number of cases. It is especially important to analyze the differences between CT images of M. kansasii and M. tuberculosis infections because there are many similarities in radiographic presentations in these infections, and different patient handling is required. Second, CT images used in this study were not essentially HRCT images because the study was based on a retrospective collection of CT images. Third, some cases in this study had several factors that might influence or alter pulmonary findings, such as past history of M. tuberculosis infection or silica exposure. To clarify whether observed CT findings were purely related to M. kansasii infection or not, it is necessary to assess sequential changes of each CT finding during chemotherapy.
In conclusion, classic radiographic findings, including preference tendency for involvement of the posterior or apical segment of the right upper lobe, significantly higher prevalence of cavity formation in association with a thin wall, limited intracavitary fluid collection, and a limited number of satellite nodules were reconfirmed upon assessment of CT images. A limited number of oval and tubular/meandering shaped cavities represent additional characteristics of CT images of M. kansasii pulmonary infection.
References
Taillard C, Greub G, Weber R, Pfyffer GE, Bodmer T, Zimmerli S, et al. Clinical implications of Mycobacterium kansasii species heterogeneity: Swiss National Survey. J Clin Microbiol. 2003;41(3):1240–4.
Maliwan N, Zvetina JR. Clinical features and follow up of 302 patients with Mycobacterium kansasii pulmonary infection: a 50 year experience. Postgrad Med J. 2005;81(958):530–3.
Shitrit D, Priess R, Peled N, Bishara G, Shlomi D, Kramer MR. Differentiation of Mycobacterium kansasii infection from Mycobacterium tuberculosis infection: comparison of clinical features, radiological appearance, and outcome. Eur J Clin Microbiol Infect Dis. 2007;26(10):679–84.
Shitrit D, Baum GL, Priess R, Lavy A, Shitrit AB, Raz M, et al. Pulmonary Mycobacterium kansasii infection in Israel, 1999–2004: clinical features, drug susceptibility, and outcome. Chest. 2006;129(3):771–6.
Griffith DE. Management of disease due to Mycobacterium kansasii. Clin Chest Med. 2002;23(3):613–21, vi.
Christensen EE, Dietz GW, Ahn CH, Chapman JS, Murry RC, Hurst GA. Radiographic manifestations of pulmonary Mycobacterium kansasii infections. AJR Am J Roentgenol. 1978;131(6):985–93.
Evans AJ, Crisp AJ, Hubbard RB, Colville A, Evans SA, Johnston ID. Pulmonary Mycobacterium kansasii infection: comparison of radiological appearances with pulmonary tuberculosis. Thorax. 1996;51(12):1243–7.
Shitrit D, Peled N, Bishara J, Priess R, Pitlik S, Samra Z, et al. Clinical and radiological features of Mycobacterium kansasii infection and Mycobacterium simiae infection. Respir Med. 2008;102(11):1598–603.
Zvetina JR, Demos TC, Maliwan N, Van Drunen M, Frederick W, Lentino J, et al. Pulmonary cavitations in Mycobacterium kansasii: distinctions from M. tuberculosis. AJR Am J Roentgenol. 1984;143(1):127–30.
Hollings NP, Wells AU, Wilson R, Hansell DM. Comparative appearances of non-tuberculous mycobacteria species: a CT study. Eur Radiol. 2002;12(9):2211–7.
Okada F, Ando Y, Yoshitake S, Ono A, Tanoue S, Matsumoto S, et al. Clinical/pathologic correlations in 553 patients with primary centrilobular findings on high-resolution CT scan of the thorax. Chest. 2007;132(6):1939–48.
Guideline for the diagnosis of pulmonary nontuberculous mycobacterial diseases—2008. The Nontuberculous Mycobacteriosis Control Committee of the Japanese Society for Tuberculosis, The Scientific Assembly for Infection and Tuberculosis of the Japanese Respiratory Society. Kekkaku. 2011;86(1):37–9.
Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007;175(4):367–416.
Goddard PR, Nicholson EM, Laszlo G, Watt I. Computed tomography in pulmonary emphysema. Clin Radiol. 1982;33(4):379–87.
Gurney JW, Schroeder BA. Upper lobe lung disease: physiologic correlates. Review. Radiology. 1988;167(2):359–66.
Park HK, Koh WJ, Shim TS, Kwon OJ. Clinical characteristics and treatment outcomes of Mycobacterium kansasii lung disease in Korea. Yonsei Med J. 2010;51(4):552–6.
Kim TS, Koh WJ, Han J, Chung MJ, Lee JH, Lee KS, et al. Hypothesis on the evolution of cavitary lesions in nontuberculous mycobacterial pulmonary infection: thin-section CT and histopathologic correlation. AJR Am J Roentgenol. 2005;184(4):1247–52.
Gorse GJ, Fairshter RD, Friedly G, Delamaza L, Greene GR, Cesario TC. Nontuberculous mycobacterial disease. Experience in a southern California hospital. Arch Intern Med. 1983;143(2):225–8.
Ahn CH, Wallace RJ, Steele LC, Murphy DT. Sulfonamide-containing regimens for disease caused by rifampin-resistant Mycobacterium kansasii. Am Rev Respir Dis. 1987;135(1):10–6.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Takahashi, M., Tsukamoto, H., Kawamura, T. et al. Mycobacterium kansasii pulmonary infection: CT findings in 29 cases. Jpn J Radiol 30, 398–406 (2012). https://doi.org/10.1007/s11604-012-0061-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-012-0061-z