Abstract
Background
The aim of this study is to compare the outcomes of platelet-rich plasma (PRP) injections to surgical release and decortication for lateral elbow tendinosis within a similar patient population.
Methods
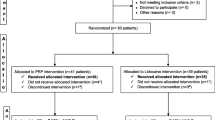
A retrospective chart review was performed on two groups of patients, receiving either PRP injections (n = 28) or surgery (n = 50). Patient demographics, clinical presentation, pain score, worker’s compensation status, and previous steroid injections were recorded. Primary outcomes included pain and symptom improvement, range of motion, return to work, and postoperative complications.
Results
Demographics, duration of symptoms, and exam findings were similar between the PRP and surgical patients. There was no significant difference in pain and symptom improvement. Pain improvement was reported in 89.3 % of PRP patients and 84 % of surgical patients, with a reported percent reduction in pain of 61.1 and 55 %, respectively. Symptoms other than pain improved in 85.7 and 88 % of the PRP and surgical patients, respectively. Tenderness to palpation at the lateral epicondyle (64.3 % PRP, 44 % surgical), pain with resisted wrist extension (35.7 % PRP, 30 % surgical), or residual symptoms other than pain (14.3 % PRP, 10 % surgical) were not significantly different between groups at last follow-up. Eighty-two percent of patients in both the PRP and surgical groups returned to work. No complications were reported. Mean follow-up was 315 vs. 352 days for the PRP and surgical groups, respectively.
Conclusions
Similar outcomes in pain improvement and return to work may be achievable with either PRP injections or surgery in recalcitrant lateral elbow tendinosis. PRP injections may be a reasonable alternative for patients apprehensive to proceed with surgery or poor surgical candidates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral elbow tendinosis, also known as lateral epicondylitis or “tennis elbow,” is a common condition resulting from a noninflammatory tendinopathy along the extensor origin of the lateral epicondyle. Multiple etiologies have been proposed, including chronic overexertion or sudden forceful extension. Ultimately, it is the accumulation of microtears between the tendon origin of extensor carpi radialis brevis (ECRB) and the periosteum of the lateral epicondyle that leads to the clinical signs and symptoms [1]. Histological analysis demonstrates the presence of angiofibroblastic hyperplasia, vascular ingrowth, and abnormal collagen production [2]. This condition is more accurately described as lateral elbow tendinosis, as only a minimal presence of inflammatory cells has been found on surgical pathology specimens [3].
Pain and tenderness over the extensor origin with associated weakness in gripping or lifting are common presenting signs and symptoms. Initial treatment of lateral elbow tendinosis is conservative with rest, activity modification, and a 10–14-day course of NSAIDs. Counterforce bracing and strengthening with physical therapy are additional effective therapeutic modalities. Nearly 85–95 % of patients obtain complete relief with conservative measures at 1-year follow-up [4–6].
There are a number of options available to patients with persistent symptoms who fail conservative therapy. Historically, corticosteroid injections were considered first-line therapy for recalcitrant cases. Recent literature suggests that corticosteroid injections may be effective in the short term but have minimal long-term benefit [5, 7–9]. Extracorporeal shock wave therapy has also been proposed as a potential option, but a recent systematic review of 1006 patients showed that it has no significant long-term benefit [10].
In recent years, alternative injections including autologous blood and platelet-rich plasma (PRP) have become more prevalent for those patients not responsive to conservative therapy. In 2006, Mishra et al. reported a 93 % pain reduction in 15 patients following PRP injections [11]. Another randomized controlled trial of 100 patients comparing injections of PRP to corticosteroid injections for lateral tendinosis demonstrated better outcomes in pain and function with use of PRP at both 1- and 2-year follow-up [12, 13]. A recent meta-analysis of 17 randomized studies reported significantly superior outcomes in PRP injections for lateral elbow tendinosis compared to a saline placebo. No significant difference was reported between steroid injections and placebo at long-term follow-up [14]. PRP injections have also shown better pain scores and long-term efficacy over corticosteroids in cases of chronic plantar fasciitis [15].
A number of other studies have suggested that PRP injections lack long-term efficacy. A recent double-blinded controlled trial randomizing 60 patients to PRP, glucocorticoid, or saline injections showed greater pain reduction in the steroid group at 1 month, but no significant difference was reported between the groups at 3-month follow-up [16]. A separate double-blinded study comparing these same three injection modalities found no significant difference in the mean reduction of pain [17].
Surgical treatment is often considered for patients whose symptoms persist after 6–12 months. Previous studies have shown comparable outcomes between percutaneous and open approaches [18]. Open methods vary depending on the surgeon and degree of tendon release or excision, with successful outcomes in 85–94 % of patients [2, 19, 20].
Although studies have suggested that PRP injections have significantly better long-term outcomes than steroid injections, there is limited data comparing the outcomes of PRP injections with surgery. The purpose of this study was to examine outcomes regarding pain and function in a two-surgeon practice over 5 years in a patient population treated with either PRP injections or surgery for recalcitrant lateral elbow tendinosis.
Methods
A retrospective chart review was performed on all adult patients presenting to the two senior authors’ office from January 1, 2006, through July 26, 2011, for chronic lateral elbow tendinosis recalcitrant to conservative therapy (e.g., activity modification, bracing, physical therapy, and NSAIDs) who received either PRP injections or surgery. Injection of corticosteroids may have been attempted prior to intervention. Inclusion criteria were symptomatic lateral tendinosis for a minimum of 6 months and clinical follow-up of at least 3 months. PRP injections were offered to patients predicted to be less than optimal surgical candidates (health status, apprehension to surgery, or require early return to work). Patients who had received previous surgical interventions were excluded from the study.
The study proposal was approved by the local institutional review board on December 6, 2011, at Mercy Health Hospital, Grand Rapids, MI. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Verbal informed consent was obtained from all patients included in the study.
PRP Preparation and Injection
All patients were asked to stop taking any NSAIDs 2 weeks prior to injections. The injection of PRP was performed in an outpatient surgical center under local anesthesia. The inner syringe from the Double Syringe Arthrex ACP® system (Arthrex Inc., Naples, FL) was first primed, followed by withdrawal of 1 mL of Anticoagulant Citrate Dextrose, Solution A (ACD-A). Approximately 10 mL of venous blood was then withdrawn from the contralateral antecubital fossa using a 21-G needle. The syringe was then gently rotated to mix the blood with the ACD-A. The syringe was then placed into the rotor and centrifuged at 1500 rpm for 5 min. Approximately 3–5 mL of concentrated plasma supernatant was then withdrawn into the inner syringe and removed from the outer syringe.
The lateral epicondyle was identified by palpation, prepped, and anesthetized with approximately 5 mL of 1 % lidocaine. Approximately 3–4 mL of PRP was injected into the extensor tendon origin in a peppered pattern. A sterile dressing was then placed.
Stretching protocols were initiated 48 h after injection and continued for 2 weeks. Patients were restricted from lifting >20 lbs until the 2-week follow-up appointment, at which time physical therapy strengthening was initiated. Avoidance of repetitive activities was recommended until 6 weeks following injection. Sports activities were restricted for 3 months postoperatively.
Surgical Release
The surgical release of the extensor tendon origin was performed in an outpatient surgical center under MAC sedation and local anesthesia. The affected extremity was prepped in a sterile fashion. An upper arm tourniquet was insufflated to 250 mmHg, and approximately 10 mL of 1 % lidocaine was injected over the lateral epicondyle. An oblique incision was made just proximal to the lateral epicondyle and continued distally toward the radial head. Dissection was then carried out through the subcutaneous layer until the extensor aponeurosis was identified. A longitudinal incision was made to visualize the extensor group (Fig. 1). The extensor carpi radialis longus was retracted to reveal the extensor radialis brevis tendon. A small V-shaped incision with 1–2-cm arms was made through the superficial ECRB tendon origin, exposing the deeper portions with degenerative changes. Excision of the affected region and decortication of the exposed lateral epicondyle were performed to bleeding bone. Once adequate decortication had been achieved, the tendon incision was closed with simple interrupted 2-0 nonabsorbable braided polyester sutures in a V-Y fashion, followed by dermal and subcuticular closure with absorbable monofilament sutures.
Stretching protocols were initiated 48 h postoperatively and continued for 2 weeks. Full active and passive range of motion exercises were started at 2–6 weeks. Repetitive activities were minimized for 6 weeks. Isometric and resistance strengthening exercises were initiated at 6–12 weeks. Sports activities were restricted for 3 months postoperatively.
Data Analysis
Demographics, duration of symptoms, previous attempts at conservative therapy, prior corticosteroid injections, timing of intervention (PRP injection or surgical release and decortication), and follow-up were included. Preoperative pain at rest was reported using a standard visual analog scale (VAS, 1–10), in addition to other symptoms such as numbness, paresthesias, and weakness with gripping (Y/N). Tenderness to palpation over the lateral epicondyle (Y/N), pain with resisted wrist extension (Y/N), and mean grip strength (kg) were recorded. Primary outcomes included the following: pain and symptom improvement (Y/N), subjective percent reduction in pain (0–100 %), residual symptoms other than pain (numbness, paresthesias, weakness in gripping), tenderness to palpation over the lateral epicondyle (Y/N), persistent pain with resisted wrist extension (Y/N), elbow range of motion (none, partial, full), return to work (Y/N), failure requiring secondary intervention (surgical release or injection), and postoperative complications (infection, hematoma, dehiscence). Differences for quantitative variables were analyzed using the t test. Differences for nominal variables were determined using the χ 2 test. Significance was assessed at p < 0.05.
Results
A total of 28 (PRP group) and 50 (surgical group) patient charts were retrospectively reviewed. There was no statistical difference in average age (45.4 and 44.6 years), gender (67.9 and 52 % female), BMI (29.4 and 28.4), hand dominance, or affected side between the PRP and surgical groups, respectively (Table 1). Worker’s compensation was involved in 67.9 and 88 % of PRP and surgical cases, respectively. The mean duration of symptoms prior to intervention was 416 and 394 days for the PRP and surgical groups, respectively. Mean follow-up was 315 days (range 99–1345 days) for PRP and 352 days (range 106–2757 days) for surgery.
No significant difference was found in clinical presentation and examination between the PRP and surgical treatment groups prior to intervention. The mean VAS pain score (1–10) reported was 6.45 ± 2.49 (PRP) and 6.32 ± 2.10 (surgical). Tenderness to palpation over the lateral epicondyle was detected preoperatively in 92.9 and 98 % of PRP injection or surgery groups, respectively. Pain with resisted wrist extension was found in 95.8 and 98 % of the PRP and surgery groups, respectively (Table 2). The unsupported mean grip strength was similar between treatment groups (27.9 and 31.1 kg for PRP and surgery, respectively). Of the PRP injection and surgical groups, 100 and 98 % had tried conservative therapy prior to intervention, respectively. One patient from the surgical group did not attempt NSAID therapy due to untoward side effects. A significantly larger percent of the surgical patients received steroid injections prior to intervention (56 vs. 29.6 % of PRP patients, respectively, p = 0.033).
No statistical difference in measured outcomes was found between the two treatment groups (p > 0.05). Both groups reported comparable rates of pain improvement following intervention, 89.3 % for the PRP group and 84 % for the surgical group (Table 3). The mean percent reduction in pain was 61.1 and 55 % in the PRP and surgical groups, respectively. Patients reported similar improvements in other symptoms, such as numbness, paresthesias, and weakness with gripping (85.7 % PRP and 88 % surgical).
No significant difference was found on clinical exam following intervention between the two groups. Persistent tenderness with palpation over the lateral epicondyle was detected in 64.3 % of PRP and 44 % of surgical patients. Pain with resisted wrist extension was found in 35.7 % of PRP patients and 30 % of surgical patients. All patients in both groups had full elbow range of motion following intervention. Eighty-two percent of patients in both the PRP and surgical groups returned to work. No postoperative complications (infection, dehiscence, or hematoma) were reported in either group. Two patients failed PRP injection (7.2 %) and underwent surgical release and decortication. Three patients failed surgical therapy (6 %); two patients had further debridement and release of the extensor origin, and one had additional steroid injections.
Discussion
Various injection modalities have been proposed as suitable alternatives to surgical intervention for lateral elbow tendinosis. In a systematic review, Assendelft et al. (1996) showed that the injection of triamcinolone improved pain and function in 2–6 weeks but was inconclusive on long-term efficacy [21]. Randomized trials have shown that the efficacy of steroids is greatest in the acute setting as success rates decrease from 92 to 68 % at 6 and 52 weeks, respectively. In the same study, physical therapy resulted in the highest success rate long term (91 %) at 52 weeks [5]. Furthermore, steroid injections have been shown to suppress tendon healing and collagen synthesis and are no longer the recommended treatment modality in cases of recalcitrant lateral elbow tendinosis [22].
Autologous blood injections have shown some success in the treatment of lateral tendinosis with minimal risk of complications [23]. One study reported pain relief in 79 % (22/28) of patients after one to three injections [24]. The efficacy of autologous blood has been attributed to the delivery of growth factors, leading to the reactivation of tendon healing through complex signaling pathways and transcription factors [25]. In vitro studies have shown increased proliferation and collagen synthesis in animal fibroblasts when cultured with growth factors, such as platelet-derived growth factor (PDGF) and FGF-β [26]. In addition, the same adverse changes to collagen synthesis associated with steroids have not been observed with autologous blood injections [27].
Platelets play a central role by releasing a variety of growth factors essential for the recruitment of macrophages and fibroblasts, ultimately leading to soft tissue healing [28]. In vivo studies have confirmed that the addition of concentrated PRP to a transected rat Achilles tendon had 30 % increase in tendon strength at 1 week and more rapid maturation [29]. Understanding the essential role of platelets in the healing process has led to clinical applications in chronic injuries as an alternative to surgical intervention. PRP injections have been safely used in orthopedics, wounds, and cardiothoracic and maxillofacial surgery [30]. It has also shown some success in chronic cases of plantar fasciitis and nonhealing injuries of the patellar tendons [31–33]. The efficacy of PRP injections may be related to the release of platelet-activating factors that promote an earlier and more vigorous healing response at the degenerated tendon origin. Studies have suggested that this healing cascade is initiated by the release of thrombin during the injection process, which activates platelets to release their growth factors, such as TGF-β, PDGF, and VEGF [34].
Evidence supporting the efficacy of PRP injections for lateral elbow tendinosis has been presented in the literature. Mishra et al. (2006) evaluated 15 patients who received PRP injections for recalcitrant lateral elbow tendinosis. Patients reported a 93 % pain reduction and 99 % return to daily activities at long-term follow-up (12–38 months) [11]. A randomized controlled trial of 100 patients compared the use of PRP to corticosteroid injections in patients with lateral elbow tendinosis. Results demonstrated less improvement in symptoms and pain at 4 weeks in the PRP group. However, the opposite was found at long-term follow-up, with the PRP group showing significantly higher improvement in symptoms and pain resolution at 26, 52, and 104 weeks compared to the corticosteroid group [12, 13]. A recent systematic review and meta-analysis compared the effectiveness of various treatment modalities. Results showed that both autologous blood and PRP injections were statistically superior to placebo at 8 weeks, whereas glucocorticoids were no more effective than placebo [14]. Two additional randomized controlled trials have suggested that PRP injections are beneficial for both pain and function in chronic cases at 6-month follow-up [35, 36].
However, there have been other studies that have refuted the proposed efficacy of PRP injections in long-term follow-up. A trial of 60 patients randomized to steroid, PRP, or saline placebo injections showed no significant difference in pain relief at 3-month follow-up between PRP and saline injections. Although there was a significant reduction in pain with the steroid group at 1 month, no significant reduction was noted at 3 months for either the PRP or steroid group compared to the placebo [16]. Further double-blinded randomized trials have also shown no significant difference in mean reduction of pain between these injection modalities in the long-term [17].
As several studies have investigated the efficacy of PRP injections to steroids, the purpose of this study was to compare outcomes in pain and symptom resolution using PRP injection or surgical release and decortication in a similar patient population. The preoperative data analysis showed similar demographics and clinical history between the two groups. There was no significant difference in age, BMI, duration of symptoms, and location and quality of pain. Pain scores and clinical exam were similar in both groups prior to intervention. All patients had attempted and failed conservative therapy, except for one surgical patient who had not tried NSAID therapy due to gastrointestinal side effects. A significantly greater proportion of surgical patients did receive steroid injections prior to intervention (56 %) compared to the PRP group (29.6 %, p = 0.033). This is likely related to the timing of the patient’s presentation during the study time frame. The majority of patients that underwent surgical release and debridement presented at earlier dates when corticosteroid injections were a more common treatment modality for the surgeons’ practice. Fewer percentage of patients in the PRP group received steroid injections due to a transition away from steroid use. This was driven by evidence-based studies reporting minimal long-term benefit to steroids [5, 7–9, 11–15], in addition to difficulties with insurance coverage.
Following intervention, both groups reported similar pain improvement (89.3 % PRP, 84 % surgical, p > 0.05) and percent pain reduction (61.1 % PRP, 55 % surgical, p > 0.05). Patients reported similar improvements in associated symptoms other than pain, such as paresthesia, numbness, and weakness with gripping (85.7 % PRP, 88 % surgical, p > 0.05). These outcomes in pain and symptom resolution are comparable to those reported in previous literature [2, 19, 20].
Any residual tenderness to palpation at the lateral epicondyle was observed in 64.3 % of PRP compared to 44 % of surgical patients, and approximately one third of patients from each group showed some residual pain with resisted wrist extension. The difference between the two groups was not statistically significant. This discomfort was not severe enough to interfere with work or daily activities. Overall improvement in pain was still 89 and 84 % for the PRP and surgical patients, respectively, and 82 % of patients in both groups returned to full work duties.
There was no significant difference in failure rates between the two groups at last follow-up. Two patients did fail PRP therapy (7.2 %) and went on to have surgical release and decortication. Three patients failed surgical therapy (6 %); two patients had further debridement and release of the extensor origin and one had additional steroid injections.
These results suggest that PRP injections may be an equally suitable, although not a significantly superior, substitute for surgical intervention in similar patient populations. This study shows that comparable outcomes in pain resolution, symptom improvement, and return to work may be achieved with PRP injections instead of surgery. PRP injections may offer an additional advantage by reducing the potential risks associated with operative intervention, anesthesia, potential costs to the patient, and shorter recovery time.
Although the two treatment groups showed similar demographics and clinical presentations, the predictive power of this study is limited by the small sample size, lack of randomization, and absent control group. A controlled study of a larger sample of patients randomized to either PRP injections or surgical release may improve the validity of these conclusions. In addition, even though the mean follow-up was over 300 days for both groups, the range was quite variable. In some instances, patients were last seen only at a 3-month follow-up appointment. As lateral epicondylitis commonly follows a chronic course, it is entirely possible that any of these patients may still have some degree of residual discomfort or limitation.
Conclusions
As lateral elbow tendinosis is a common problem affecting a large population annually, it is important to understand the options available to physicians if conservative measures fail to resolve symptoms. As steroids have been shown to have poor long-term benefit, other nonsurgical modalities, such as PRP injections, have been investigated, often with successful outcomes in pain and function. As a first-line therapy, PRP injections may be a suitable alternative to promote activation of tendon healing, remodeling, and, ultimately, recovery. Patients who fail conservative measures, including activity modification, NSAIDs, bracing, and physical therapy, followed by PRP injections, may benefit from surgical therapy.
References
Johnson GW, Cadwallader K, Scheffel SB, Epperly TD. Treatment of lateral epicondylitis. Am Fam Physician. 2007;76(6):843–8.
Nirschl RP, Pettrone FA. The surgical treatment of lateral epicondylitis. J Bone Joint Surg Am. 1979;61(6A):832–9.
Scher DL, Wolf JM, Owens BD. Lateral epicondylitis. Orthopedics. 2009;32(4):276–82.
Struijs PA, Kerkhoffs GM, Assendelft WJ, et al. Conservative treatment of lateral epicondylitis: brace versus physical therapy or a combination of both—a randomized clinical trial. Am J Sports Med. 2004;32(2):462–9.
Smidt N, van der Windt DA, Assendelft WJ, et al. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: a randomized controlled trial. Lancet. 2002;359(37):657–62.
Budoff JE. Tendinopathies of the hand, wrist, and elbow. In: Trumble TE, Rayan GM, Budoff JE, Baratz ME, editors. Principles of hand surgery and therapy. Saunders/Elsevier: Philadelphia; 2010. p. 337–51.
Solveborn A, Buch F, Mjallmin H, Adalberth G. Cortisone injection with anesthetic additive for radial epicondylagia (tennis elbow). Clin Orthop Relat Res.1995;316:99–105
Newcomer KL, Laskowski ER, Idank DM, McLean TJ, Egan KS. Corticosteroid injection in early treatment of lateral epicondylitis. Clin J Sport Med. 2001;11:214–22.
Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B. Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. JAMA. 2013;309(5):461–9.
Buchbinder R, Green SE, Youd JM. Systematic review of the efficacy and safety of shock wave therapy for lateral elbow pain. J Rheumatol. 2006;33(7):1351–63.
Mishra A, Pavelko T. Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med. 2006;10(10):1–5.
Peerbooms JC, Sluimer J, Bruijn DJ, Gosens T. Positive effect of an autologous platelet concentrate in lateral epicondylitis in a double-blind randomized controlled trial: platelet-rich plasma versus corticosteroid injection with a 1-year follow-up. Am J Sports Med. 2010;38(2):255–62.
Gosens T, Peerbooms JC, van Laar W, et al. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis. Am J Sports Med. 2011;39(6):1200–8.
Krogh TP, Bartels EM, Ellingsen T, et al. Comparative effectiveness of injection therapies in lateral epicondylitis: a systematic review and network meta-analysis of randomized controlled trials. Am J Sports Med. 2013;41(6):1435–46.
Monto RR. Platelet-rich plasma efficacy versus corticosteroid injection treatment for chronic severe plantar fasciitis. Foot Ankle Int. 2014;35(4):313–8.
Krogh TP, Fredberg U, Stengaard-Pedersen K, et al. Treatment of lateral epicondylitis with platelet-rich plasma, glucocorticoid, or saline: a randomized, double-blind, placebo-controlled trial. Am J Sports Med. 2013;41:625–35.
Shiple BJ. How effective are injection treatments for lateral epicondylitis? Clin J Sport Med. 2013;23(6):502–3.
Dunkow PD, Jatti M, Muddu BN. A comparison of open and percutaneous techniques in the surgical treatment of tennis elbow. J Bone Joint Surg (Br). 2004;86(5):701–4.
Dunn JH, Kim J, Nirschl RP, et al. Ten- to 14-year follow-up of the Nirschl surgical technique for lateral epicondylitis. Am J Sports Med. 2008;36(2):261–6.
Coleman B, Quinlan JF, Matheson JA. Surgical treatment for lateral epicondylitis: a long-term follow-up of results. J Shoulder Elbow Surg. 2010;19(3):363–7.
Assendelft WJ, Hay EM, Adshead R, et al. Corticosteroid injections for lateral epicondylitis: a systematic review. B J Gen Prac. 1996;46(405):209–16.
Wong MN, Tang YN, Lee SN, et al. Effect of dexamethasone on cultured human tenocytes and its reversibility by platelet-derived growth factor. J Bone Joint Surg Am. 2003;85(10):1914–20.
Connell DA, Ali KE, Ahmad M, et al. Ultrasound guided autologous blood injection for tennis elbow. Skeletal Radiol. 2006;35(6):371–7.
Edwards SG, Calandruccio JH. Autologous blood injections for refractory lateral epicondylitis. J Hand Surg Am. 2003;28(2):272–8.
Molloy T, Wang Y, Murrel G. The roles of growth factors in tendon and ligament healing. Am J Sports Med. 2003;33(5):381–94.
Thomopoulus S, Harwood F, Silva M, et al. Effect of several growth factors on canine flexor tendon fibroblast proliferation and collagen synthesis in vitro. J Hand Surg Am. 2005;30(3):441–7.
Taylor MA, Norman TL, Clovis NB, et al. The response of rabbit patellar tendons after autologous blood injection. Med Sci Sports Exerc. 2002;34(1):70–3.
Anitua M, Sanchez E, Nurden A, et al. New insights into and novel applications for platelet-rich fibrin therapies. Trends Biotechnol. 2006;24(5):227–34.
Aspenberg P, Virchenko O. Platelet concentrate injection improves Achilles tendon repair in rats. Acta Orthop Scand. 2004;75(1):93–9.
Fufa D, Shealy B, Jacobson M, et al. Activation of platelet-rich plasma using soluble type I collagen. J Oral Maxillofac Surg. 2008;66(4):684–90.
Barrett S, Erredge S. Growth factors for chronic plantar fasciitis. Podiatry Today. 2004;17:37–42.
Kajikawa Y, Morihara T, Sakamoto H, Matsuda K, Oshima Y, Yoshida A, et al. Platelet-rich plasma enhances the initial mobilization of circulation-derived cells for tendon healing. J Cell Physiol. 2008;215(3):837–45.
Taylor M, Norman T, Clovis N, Blaha D. The response of rabbit patellar tendons after autologous blood injection. Med Sci Sports Exerc. 2002;34(1):70–3.
Sampson S, Gerhardt M. Platelet rich plasma injection grafts for musculoskeletal injuries: a review. Curr Rev Musculoskeletal Med. 2008;1:165–74.
Creaney L, Wallace A, Curtis M, Connell D. Growth factor-based therapies provide additional benefit beyond physical therapy in resistant elbow tendinopathy: a prospective, single-blind, randomized trial of autologous blood injections versus platelet-rich plasma. Brit J Sports Med. 2011;45(12):966–71.
Thanasas C et al. Platelet-rich plasma versus autologous blood for the treatment for chronic lateral elbow epicondylitis: a randomized controlled clinical trial. Am J Sports Med. 2011;39(10):2130–4.
Conflict of Interest
Ronald D. Ford, William P. Schmitt, Kyle Lineberry, and Paul Luce declare that they have no conflict of interest.
Statement of Human and Animal Rights
RF, WS, KL, and PL all declare that all procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008, and that this study was approved by the IRB on December 6, 2011. Informed consent was obtained from all patients for being included in this study. This article does not contain any studies on animal subjects.
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper was part of an oral presentation at the Michigan Academy of Plastic Surgeons, Mackinac, MI, on July 2012.
About this article
Cite this article
Ford, R.D., Schmitt, W.P., Lineberry, K. et al. A retrospective comparison of the management of recalcitrant lateral elbow tendinosis: platelet-rich plasma injections versus surgery. HAND 10, 285–291 (2015). https://doi.org/10.1007/s11552-014-9717-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9717-8