Abstract
Background
Disorders involving the peripheral nervous system can have devastating impacts on patients’ daily functions and routines. There is a lack of consideration of the impact of injury on social/emotional well-being and function.
Methods
We performed a retrospective database and chart review of adult patients presenting between 2010 and 2012 with peripheral nerve compression, brachial plexus injury, thoracic outlet syndrome (TOS), or neuromas. At the initial assessment, patients completed a questionnaire used to obtain demographic and psychosocial variable data including the (1) average level of pain over the last month, (2) self-perceived depression, (3) how much pain impacts quality of life (QoL), (4) current level of stress, and (5) ability to cope with stress. Statistical analyses were used to assess the differences between the dependent variables and diagnostic and demographic groups.
Results
This study included 490 patients (mean age 50 ± 15 years); the most common diagnosis was single nerve compression (n = 171). Impact on QoL was significantly greater in patients with TOS, cutaneous peroneal compressions, and neuroma versus single site nerve compressions. Average pain, impact on QoL, and stress at home were significantly higher in females versus males. Impact on QoL was correlated with average pain, depression, stress at home, and ability to cope with stress at home.
Conclusions
Our study demonstrates that patients with single site nerve compression neuropathies experience fewer negative psychosocial effects compared to patients with more proximal upper extremity peripheral nerve disorders and neuromas. The impact on QoL was strongly correlated with pain and depression, where patients with neuromas and painful peroneal nerve entrapments reported greater detriments to QoL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disorders involving the peripheral nervous system can have devastating impacts on patients’ daily functions and routines [7, 15, 21, 25]. However, the literature lacks comprehensive descriptions of the psychosocial implications of peripheral nerve injuries and treatment outcomes. An understanding of the multiple factors that influence outcomes becomes increasingly important as hospitals and other health-care facilities progressively emphasize outcome-focused patient care. Valuation of the success of a treatment still often differs between patient and provider [19]. Historically, treatment outcomes have been assessed by a number of quantitative biomedical measures and postoperative measurements of sensibility, motor function, and strength. There is a lack of consideration of the impact of injury on social/emotional well-being and function [22, 30], despite the importance of these subjective measures to patients.
Previous studies have provided evidence that pain associated with nerve injuries can be severe and is associated with disability using self-report outcome measures (i.e., DASH, SF-36, CISS) [8, 13, 20, 22]. In addition, both increased pain and disability levels are predictive factors for poor quality of life (QoL) scores [12]. Similarly, studies of patients with either upper or lower extremity peripheral nerve disorders have shown that patient-reported QoL is significantly worse when compared to healthy control subjects [2, 4]. Using the SF-36 survey, which examines both physical and mental components of functional health and well-being, those who experience nerve-related pain experience more burden and poorer outcomes as a result of their injury compared to patients who experience little to no pain [12].
Stress and ability to cope with stress are also important yet underreported factors in the nerve-injured population [6]. Individuals are at increased risk for chronic pain and disability when using catastrophizing as a coping strategy [23]. In 2010, Cederlund et al. reported that patients with a low sense of coherence, defined as the capacity to cope in a stressful situation, were significantly less satisfied in daily occupations, had lower QoL scores, and reported more pain [10].
The objective of this study was to assess and compare patient-reported preoperative psychosocial impacts of various peripheral nerve diagnoses by examining specific subjective factors (pain, depression, stress, and QoL). We included a broad spectrum of nerve pathologies to determine the range and importance of psychosocial implications. We hypothesized that patients with single nerve compression neuropathies (i.e., carpal tunnel syndrome, cubital tunnel syndrome) would report lower pain, depression, and stress and higher QoL than would patients with multiple or other, more complex peripheral nerve diagnoses (i.e., brachial plexus injury, thoracic outlet syndrome (TOS), dual upper extremity nerve compression, lower extremity pathologies). We hypothesized that patients with neuromas would present with the highest negative ratings across outcome measures.
Materials and Methods
Approval was obtained from the university’s institutional review board for this study, and written informed consent was obtained from each patient for inclusion of routine clinic visit information into a patient database. A retrospective cross-sectional review was performed with eligible patients who were seen by the senior author for nerve-related diagnoses from December 2010 to October 2012. Records were retrieved from a database (n = 644), which included patients with nerve and musculoskeletal-related diagnoses. Only adult patients (>18 years) presenting with an upper or lower extremity peripheral single or dual nerve compression diagnosis were included.
Measures
At the initial assessment, all patients completed written health history and pain evaluation questionnaires (Fig. 1). Data were collected from the prospective database and chart review. Demographic and patient characteristic data included age, sex, hand dominance, smoking status, alcohol consumption, and height and weight (from which body mass index was computed). The health history form assessed past medical and surgical history, comorbidities, and medications. Subjective data from the pain evaluation questionnaire consisted of 20 pain-descriptive words, 21-item questionnaire, and 7 10-cm visual analogue scales (VASs) used to evaluate the (1) average level of pain experienced over the last month, (2) self-perceived depression, (3) impact of pain on QoL, (4) current level of stress at home, (5) current level of stress at work, (6) ability to cope with stress at home, and (7) ability to cope with stress at work. For the ability to cope with stress at home or at work, lower VAS values indicated better coping ability. For all other scales, higher values indicated increased severity of symptoms or impact of symptoms.
Pain questionnaire. Each patient fills out the questionnaire in its entirety at the initial evaluation. At each follow-up visit, pain description and visual analogue scale (10 cm) questions 1–10 are completed. (Reproduced with permission: Susan E. Mackinnon, MD). Entire Pain Evaluation Questionnaire can be found at www.nervesurgery.wustl.edu
Statistical Analysis
Patients were classified into seven groups according to their clinical diagnosis: (1) brachial plexus nerve injury; (2) TOS; (3) single nerve compressions (including carpal tunnel syndrome, cubital tunnel syndrome, radial nerve compression, or median nerve diagnosis other than carpal tunnel syndrome); (4) dual nerve compression diagnoses (carpal and cubital tunnel syndromes or carpal tunnel syndrome and ulnar nerve compression at Guyon’s canal); (5) ulnar nerve diagnosis other than cubital tunnel syndrome; (6) lower extremity compression (common peroneal nerve, superficial or deep peroneal nerve, and tarsal tunnel); and (7) neuroma. While compression of the common peroneal branch results in motor deficits, foot drop, patients with compression of the cutaneous superficial or deep branch of the peroneal nerve clinically present with sensory disturbances. Based on these distinct presentations, a subgroup containing only patients with compression of the superficial or deep peroneal nerve was formed for a post hoc analysis.
Descriptive statistics (means, standard deviations, and frequencies) were calculated for all variables by diagnosis. Differences in initial visit data between diagnostic groups were analyzed using the Kruskal–Wallis test for each continuous variable. For the post hoc analyses, Mann–Whitney U tests with Bonferroni correction were used. Bivariate analyses (Mann–Whitney U tests) were used to analyze the differences between smokers and nonsmokers, those who drink and those who do not drink, right versus left extremity affected, and males versus females. Nonparametric Spearman’s correlations were used to assess the associations among variables with continuous data. p values <0.05 were considered statistically significant.
Results
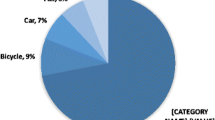
Patient demographic data are presented in Table 1. There were 490 patients included in this study, with a mean age of 50 years (SD = 15 years; range, 18–86 years). Single compression neuropathies accounted for 171 cases. The dominant extremity was involved in 58.5 % of the patient population. Table 2 presents the mean VAS scores for each variable included in the pain evaluation questionnaire. The most frequently reported pain descriptors for all diagnoses included tingling, numbing, and aching; however, for neuroma, stabbing, throbbing, and shooting were the three most reported pain descriptors.
There were significant main effect differences between diagnostic groups and QoL score (p < 0.001) and stress at home (p = 0.05) and stress at work (p = 0.05). Post hoc analysis revealed that pain-related impact on QoL scores was significantly greater in patients with TOS (p = 0.002), neuroma (p = 0.002), and superficial or deep peroneal compression (p = 0.001) compared to patients with upper extremity single nerve compressions. Compared to patients with single nerve compressions, both the level of stress at home and the level of stress at work were significantly higher in patients with neuromas (p = 0.002) (Table 2).
The impact on QoL was significantly greater in females versus males (p = 0.02), smokers versus nonsmokers (p = 0.03), and non-alcohol drinkers versus alcohol drinkers (p < 0.001) (Table 3). Pain intensity was significantly higher in females versus males (p = 0.003) and non-alcohol drinkers versus alcohol drinkers (p < 0.001). Significantly higher home stress levels were reported by females versus males (p = 0.002). Significantly lower abilities to cope at home and higher work stress levels were reported by non-alcohol drinkers versus alcohol drinkers (p = 0.02).
Correlation coefficients among VAS variables are shown in Table 4. Impact on QoL scores demonstrated moderate (0.3 to 0.5) to moderately strong (0.5 to 0.7) correlation with average pain, depression, stress at home, and the ability to cope with stress at home.
Discussion
Our study demonstrates that patients who present with distal single site nerve compression neuropathies, such as carpal or cubital tunnel, experience fewer negative psychosocial effects than patients with neuromas or more proximal upper extremity peripheral nerve disorders, including thoracic outlet syndrome and brachial plexus injury. Depending on the structure and site of injury, there is great variability in symptoms and patient presentation.
It is well established that upper extremity disorders affecting the peripheral nervous system have lasting implications on function [4, 8, 11, 22]. In our study, patients reported a moderate to large negative impact on QoL, regardless of diagnosis, indicating that nerve injury and compression have a considerable impact on overall well-being. Our findings are consistent with prior research suggesting that the psychosocial aspects following injury are associated with patient presentation and treatment outlook [3, 9, 26, 32]. Adogwa et al. [1] found that greater depression was associated with higher levels of disability and less satisfaction with treatment. This finding was observed in patients with similar diagnoses and surgical treatment, suggesting an interplay between intrinsic and extrinsic factors in recovery and outcomes [1, 4]. Because of the psychosocial influences that may impact outcomes in the presence of multiple site nerve compression, the identification and treatment of all nerve compressive sites is necessary for successful outcomes [18]. These findings support the ever-increasing emphasis on patient-centered outcome measures [28].
Psychosocial factors, such as depression, coping, and anxiety, influence many common patient outcomes, such as levels of pain, patient satisfaction, and disability [17, 23, 26, 31]. In our study, patient-reported depression was low when examined in the context of the poor QoL ratings. This score discrepancy could be attributed to the social stigma associated with mental illness [29]. A difference in ratings between men and women was also found for pain, impact on QoL, and stress at home. These findings are consistent with prior work reporting gender differences in neurogenic pain and psychosocial distress after injury [5, 14].
Carpal tunnel, cubital tunnel, and Guyon’s canal are common sites of nerve entrapment and are traditionally considered to be easily diagnosed and treated. By contrast, in this study, we found that dual compressions of these nerves resulted in higher stress and decreased ability to cope with stress at work. This finding may be important in counseling patients with respect to work performance and psychosocial issues.
Our study highlighted that those who consume alcohol reported significantly lower pain, greater ability to cope with stress at home, and lower work stress levels. Previous work has shown that coping is a frequent motive for the consumption of alcohol [16]. Forthcoming studies can evaluate alcohol consumption and its relationship to stressors and coping strategies as confounding factors. The lower extremity nerve compression group had a greater proportion of smokers and reported greater pain, more depressed feelings, and a greater negative impact on QoL in comparison to the upper extremity nerve compression group. Smoking can impair the vascular supply to the nerve. Therefore, prolonged distal ischemia may lead to increased susceptibility of peripheral nerve degeneration [24, 27]. Examining the influence of health behaviors on self-report factors is an important step moving forward to reduce the incidence of spurious relationships between these variables.
The strengths of this study include a large sample of patients with nerve-related diagnoses and a heterogeneous sample with comprehensive self-report evaluation. The limitations of this study include a cross-sectional study design, lack of a control group, and exclusion of physical impairment measures. This introductory study examined only data obtained at the participants’ initial visit with the surgeon, and therefore, we were unable to assess changes that occurred with recovery and/or treatment. Not having a control group limited potential comparative findings with healthy subjects or injuries not involving the peripheral nervous system. We did not explore the relationships between symptom duration and self-report ratings, and univariate data analysis cannot rule out the presence of confounding variables. Quantitative measures of strength and sensibility were not included, and we were unable to assess the relationship between physical impairment related to nerve function and subjective psychosocial variables. Disability and specific activity limitations were not evaluated in this study but may provide valuable information regarding relationships with psychosocial variables.
Our findings highlight the need for increased screening and assessment of factors that reach beyond the biomedical model. While measurements of range of motion and strength can help to determine levels of biomechanical function and physical impairments, they fail to assess the overall functional status in multiple life domains. Understanding the psychosocial and biomedical factors will allow physicians and other health-care professionals to focus on improvements in QoL and function.
References
Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung depression scale predicts patient satisfaction independent of the extent of improvement after revision lumbar surgery. Spine J. 2013;13:501–6.
Aprile I, Caliandro P, La Torre G, et al. Multicenter study of peroneal mononeuropathy: clinical, neurophysiologic, and quality of life assessment. J Peripher Nerv Syst. 2005;10:259–68.
Ayers DC, Franklin PD, Ring DC. The role of emotional health in functional outcomes after orthopaedic surgery: extending the biopsychosocial model to orthopaedics: AOA critical issues. J Bone Joint Surg Am. 2013;95:e165.
Bailey R, Kaskutas V, Fox I, et al. Effect of upper extremity nerve damage on activity participation, pain, depression, and quality of life. J Hand Surg [Am]. 2009;34:1682–8.
Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth. 2013;111:52–8.
Bear-Lehman J, Poole SE. The presence and impact of stress reactions on disability among patients with arm injury. J Hand Ther. 2011;24:89–93.
Becker SJ, Makanji HS, Ring D. Expected and actual improvement of symptoms with carpal tunnel release. J Hand Surg [Am]. 2012;37:1324–9. e1-5.
Boogaard S, De Vet HC, Faber CG, et al. An overview of predictors for persistent neuropathic pain. Expert Rev Neurother. 2013;13:505–13.
Calderon SA, Zurakowski D, Davis JS, et al. Quantitative adjustment of the influence of depression on the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire. Hand (N Y). 2010;5:49–55.
Cederlund RI, Ramel E, Rosberg HE, et al. Outcome and clinical changes in patients 3, 6, 12 months after a severe or major hand injury—can sense of coherence be an indicator for rehabilitation focus? BMC Musculoskelet Disord. 2010;11:286.
Choi PD, Novak CB, Mackinnon SE, et al. Quality of life and functional outcome following brachial plexus injury. J Hand Surg [Am]. 1997;22:605–12.
Ciaramitaro P, Mondelli M, Logullo F, et al. Traumatic peripheral nerve injuries: epidemiological findings, neuropathic pain and quality of life in 158 patients. J Peripher Nerv Syst. 2010;15:120–7.
Cocito D, Paolasso I, Pazzaglia C, et al. Pain affects the quality of life of neuropathic patients. Neurol Sci. 2006;27:155–60.
Edwards RR, Haythornthwaite JA, Sullivan MJ, et al. Catastrophizing as a mediator of sex differences in pain: differential effects for daily pain versus laboratory-induced pain. Pain. 2004;111:335–41.
Guse DM, Moran SL. Outcomes of the surgical treatment of peripheral neuromas of the hand and forearm: a 25-year comparative outcome study. Ann Plast Surg. 2013;71:654–8.
Kuntsche E, Gabhainn SN, Roberts C, et al. Drinking motives and links to alcohol use in 13 European countries. J Stud Alcohol Drugs. 2014;75:428–37.
Lozano Calderon SA, Paiva A, Ring D. Patient satisfaction after open carpal tunnel release correlates with depression. J Hand Surg [Am]. 2008;33:303–7.
Mackinnon SE, Novak CB. Clinical commentary: pathogenesis of cumulative trauma disorder. J Hand Surg [Am]. 1994;19:873–83.
Nisenzon AN, Robinson ME, Bowers D, et al. Measurement of patient-centered outcomes in Parkinson’s disease: what do patients really want from their treatment? Parkinsonism Relat Disord. 2011;17:89–94.
Novak CB, Anastakis DJ, Beaton DE, et al. Patient-reported outcome after peripheral nerve injury. J Hand Surg [Am]. 2009;34:281–7.
Novak CB, Anastakis DJ, Beaton DE, et al. Relationships among pain disability, pain intensity, illness intrusiveness, and upper extremity disability in patients with traumatic peripheral nerve injury. J Hand Surg [Am]. 2010;35:1633–9.
Novak CB, Anastakis DJ, Beaton DE, et al. Biomedical and psychosocial factors associated with disability after peripheral nerve injury. J Bone Joint Surg Am. 2011;93:929–36.
Pincus T, Burton AK, Vogel S, et al. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976). 2002;27:E109–20.
Pourmemari MH, Viikari-Juntura E, Shiri R. Smoking and carpal tunnel syndrome: a meta-analysis. Muscle Nerve. 2014;49:345–50.
Ring D. Symptoms and disability after major peripheral nerve injury. Hand Clin. 2013;29:421–5.
Ring D, Kadzielski J, Fabian L, et al. Self-reported upper extremity health status correlates with depression. J Bone Joint Surg Am. 2006;88:1983–8.
Rinker B, Fink BF, Barry NG, et al. The effect of cigarette smoking on functional recovery following peripheral nerve ischemia/reperfusion injury. Microsurgery. 2011;31:59–65.
Selby JV, Lopstein SH. PCORI at 3 years—progress, lessons, and plans. N Engl J Med. 2014;370:592–5.
Switaj P, Grygiel P, Anczewska M, et al. Loneliness mediates the relationship between internalised stigma and depression among patients with psychotic disorders. Int J Soc Psychiatry. 2013.
van Wilgen P, Beetsma A, Neels H, et al. Physical therapists should integrate illness perceptions in their assessment in patients with chronic musculoskeletal pain; a qualitative analysis. Man Ther. 2013.
Vranceanu AM, Barsky A, Ring D. Psychosocial aspects of disabling musculoskeletal pain. J Bone Joint Surg Am. 2009;91:2014–8.
Vranceanu AM, Jupiter JB, Mudgal CS, et al. Predictors of pain intensity and disability after minor hand surgery. J Hand Surg [Am]. 2010;35:956–60.
Conflict of Interest
Danielle M. Wojtkiewicz declares that she has no conflict of interest.
James Saunders declares that he has no conflict of interest.
Leahthan Domeshek declares that she has no conflict of interest.
Christine B. Novak declares that she has no conflict of interest.
Vicki Kaskutas declares that she has no conflict of interest.
Susan E. Mackinnon declares that she has no conflict of interest.
Statement of Animal and Human Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Wojtkiewicz, D.M., Saunders, J., Domeshek, L. et al. Social impact of peripheral nerve injuries. HAND 10, 161–167 (2015). https://doi.org/10.1007/s11552-014-9692-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-014-9692-0