Abstract
Introduction
Fractures of the distal radius are among the most common fractures seen. They encompass a myriad of presentations and fracture patterns that often benefit from various open reduction and internal fixation techniques—including volar plating, dorsal plating, radial plating, intramedullary nailing, and fragment-specific fixation. In order to obtain optimal reduction of these fractures, surgeons require a thorough understanding of the anatomy and various surgical exposures.
Anatomy
The distal radius is surrounded by a soft tissue envelope rich in vascularity and cutaneous innervation. The osseous surface consists of two articular surfaces and three cortical sides covered almost entirely by soft tissue.
Surgical approaches
Approaches to the distal radius can be broadly divided into volar, radial, and dorsal. Visualization of the articular surface can be accomplished best arthroscopically. Arthroscopy can be performed alone or in conjunction with other open approaches to the distal radius.
Summary
This article will review the pertinent anatomy and various surgical approaches in order to facilitate the surgeon’s ability to safely expose a distal radius fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fractures of the distal radius are among the most common fractures seen [1, 2]. As our population ages, the prevalence of these injuries is expected to increase. Similarly, over the past several years, we have observed a dramatic increase in the surgical management of distal radius fractures [3]. This increase in surgical intervention can be attributed to the development of new plating systems and the potential clinical benefits of more precise fracture reduction and early mobilization [4, 5].
Surgical implants for the management of distal radius fractures have also dramatically grown in number and include dorsal plates, volar plates, radial plates, fragment-specific fixation, and intramedullary nails [6–13] (see Fig. 1). Each implant can offer different advantages in the management of distal radius fractures. In order to obtain the best fracture reduction, various surgical approaches may be required. This article will review the regional anatomy of the distal radius and the various relevant surgical approaches.
Anatomy
Exposure of the distal radius and its fracture fragments is complicated by the close proximity of surrounding muscle, ligaments, tendons, and neurovascular structures. The individual alignment of various articular fracture fragments of the distal radius is affected by these soft tissue attachments [14]. When studying the distal radius, it is helpful to consider its five “surfaces”: (1) the volar surface, (2) the radial surface, (3) the dorsal surface, (4) the distal radiocarpal articular surface, and (5) the distal radioulnar articular surface (see Fig. 2). Understanding the anatomy and position of each surface is important for adequate exposure and subsequent reduction in the management of distal radius fractures.
Superficial Anatomy
The surface and superficial anatomy about the distal radius includes a soft tissue envelope that enjoys a rich blood supply and dense cutaneous innervation. Incisions can be placed liberally as long as the principles of maintaining longitudinal or oblique incisions are honored, underlying cutaneous nerves protected, and subcutaneous veins preserved whenever feasible. Branches of the radial sensory nerve reside in the subcutaneous tissue over the radial surface and provide sensation to the radial aspect of the wrist and the first web space dorsally. The radial sensory nerve emerges from below the brachioradialis tendon approximately 8–9 cm proximal to the radial styloid and on average divides into four branches [15, 16]. The dorsal cutaneous branch of the ulnar nerve provides sensation to the ulnar aspect of the wrist. It arises approximately 3–5 cm proximal to the ulnar styloid, and it typically crosses volar to the head of the ulna before traveling dorsally to the ulnar hand [17]. Although there is much variability as to when the dorsal cutaneous branch of the ulnar nerve branches, there is little variability in the branching pattern with most branches traveling dorsally and the remaining traveling volarly over the hypothenar eminence [18]. In addition, the dorsal aspect of the hand is also supplied by a consistent contribution from the lateral and posterior antebrachial cutaneous nerves [19]. In a detailed study of the dorsal innervations of the hand, Mok et al. noted that the dorsal hand and wrist were equally divided and innervated the sensory branch of the radial nerve and dorsal ulnar sensory branch of the ulnar nerve [18]. The palmar cutaneous branch of the median nerve provides sensation to the volar wrist and palm of the hand. It arises approximately 3.2 cm proximal to the wrist crease from the radial side of the median nerve and typically runs along the radial border of the palmaris longus tendon [20]. At the level of the wrist crease, the nerve travels approximately 5 mm radial to the inter-thenar depression [21].
Deep Anatomy
Excluding the two articular surfaces, the remaining three surfaces of the distal radius are covered almost entirely by soft tissue. Only Lister’s tubercle and the radial styloid maintain a subcutaneous osseous surface free of direct soft tissue attachments. The dorsal surface and radial surface are otherwise covered by the six traversing extrinsic dorsal extensor compartments of the wrist. The radial surface is covered by the first dorsal compartment and its abductor pollicis longus and extensor pollicis brevis tendons. Further proximally and deeper, the radial styloid is covered by the lone tendinous insertion onto the distal radius, the brachioradialis. It inserts approximately 17 mm proximal to the radial styloid under the base of the first dorsal compartment [22]. The brachioradialis can act as a deforming force with distal radius fractures. Moving further ulnarward, the distal radius is covered by the second dorsal compartments and its extensor carpi radialis longus and extensor carpi radialis brevis tendons. The second dorsal compartment is separate by the third dorsal compartment by Lister’s tubercle, which acts as a pulley for the extensor pollicis longus tendon running within the third dorsal compartment. The fourth dorsal compartment covers the remaining dorsal surface of the distal radius and contains the extensor indicis proprius and the extensor digitorum comminis tendons. Deep to the fourth dorsal compartment lies the posterior interosseous nerve and vessels on the dorsal surface of the distal radius. The fifth and sixth compartments with the extensor digiti minimi and extensor carpi ulnaris tendons, respectively, cover the distal radioulnar joint and ulnar head also, respectively.
The volar surface of the distal radius is relatively flat and broad but is covered by multiple layers of soft tissue. Superficially, the volar anatomy of the wrist includes, from radial to ulnar: the radial artery, flexor carpi radialis tendon, palmaris longus tendon, and the flexor carpi ulnaris tendon. Deep to the palmaris longus tendon lies the Median nerve and the finger flexor tendons. The flexor pollicis longus tendon lies deep to the flexor carpi radialis tendon. The deepest volar soft tissue structure is the pronator quadratus as it completely covers the flat volar surface of the distal radius. However, the very distal margin slopes volarly in the form of a ridge from which the volar radiocarpal ligaments take origin. The junction between the distal extent of the pronator quadratus and the origin of the volar radiocarpal ligaments represents the “watershed line” [23] (see Fig. 3). A plate positioned distally beyond this point may risk flexor tendon irritation. The ulnar volar margin of the lunate facet slopes volarly from a proximal to distal direction. Thus, the volar lunate facet extends approximately 3 mm more distally than expected, and an effective support of this area with a plate can be challenging [24, 25]. The short radiolunate ligament originates from the volar margin of the lunate facet and attaches to the volar surface of the lunate. It is proposed that this ligament plays a vital role in the volar stability of the radiocarpal articulation [26]. Similarly, the radioscaphocapitate ligament takes its origin from the volar surface of the radial styloid and provides an important restraint to ulnar translocation of the carpus [27].
Osseous Anatomy
The distal end of the radius should be viewed as the anatomic foundation of the wrist joint. Beginning 2 to 3 cm proximal to the radiocarpal joint at the metaphyseal flare, the distal end of the radius is uniquely designed to maintain the capacity to transmit axial load and provide mobility [28]. In the coronal plane, the distal radius assumes an inclination of 22° to 23°. In the sagittal plane, the distal radius assumes a tilt angled volarly approximately 11° to 12° (see Fig. 3a).
The distal radiocarpal articular surface is both biconcave and triangular in shape. The apex of the triangle points toward the radial styloid process, and the base of the triangle forms the sigmoid notch which articulates with the distal end of the ulna. Viewed from the lateral side, the radial styloid sits volar to the mid-axis of the radius. The articular surface is separated into two distinct concave facets known as the scaphoid and lunate facets, with the latter having a larger radius and extending volarly into the lunate facet [25] (see Fig. 3b). Standard compressive articular fracture lines commonly propagate between these facets. Additional compressive force will split the fragments in the coronal plane or cause central fragmentation and impaction [14]. In addition, there is often an associated inter-carpal ligament injury with radial styloid fractures that exit at the level of the scapholunate ligament [29].
The volar aspect of the lunate facet is approximately 5 mm thick and projects approximately 3 mm anteriorly to the flat volar surface of the distal radius, making it relatively vulnerable to injury and difficult to fix internally [25] (see Fig. 3). The articular surface exhibits an overall volar and ulnar slope which is essential in helping the wrist to deviate ulnarly for power grasp, but at the same time causing the carpus to assume a natural tendency to slope in this direction. Ligamentous restraints resist this natural tendency. The distal radiocarpal articular surface facilitates flexion/extension and radial/ulnar deviation of the wrist. In addition, it supports the majority of longitudinal stress across the wrist joint.
The distal radioulnar articular surface, or sigmoid notch, is semi-circular and articulates with the ulnar head. The sigmoid notch has a greater radius of curvature than the ulnar head, and motion at the distal radioulnar joint is a combination of rotation and translation. This articulation facilitates forearm rotation, along with the interosseous membrane and proximal radioulnar joints, as the radius and hand rotate about the fixed ulna. The triangular fibrocartilage complex (TFCC) arises from the ulnar aspect of the lunate facet of the radius, above the sigmoid notch, and extends on to the base of the ulnar styloid process. It functions as an additional stabilizer of the distal radioulnar joint and to increase the relative articulating area of the wrist. A large fracture of the ulnar styloid or peripheral tear of the TFCC can theoretically destabilize the distal radioulnar joint.
Volar Approach
The volar approach to the distal radius can be used for both volar plate and fragment specific fixation [8, 10, 11, 30]. Volar plate application provides the advantage of placing the plate on the tensile side of the radius while also utilizing greater soft tissue coverage to decrease hardware prominence and irritation [7–9]. The volar approach can be accomplished through three different intervals: (1) the Henry approach, (2) the trans-FCR approach, and the (3) volar-extensile approach (see Fig. 4). Both the Henry and trans-FCR approaches provide excellent exposure to the volar surface of the distal radius for the reduction and internal fixation of distal radius fractures [8, 10, 29, 31]. In contrast, the volar-extensile approach incorporates a carpal tunnel release and affords direct visualization and fracture reduction of the volar–ulnar corner of the distal radius, maximum volar visualization of the distal radioulnar joint, and expanded exposure of the radiocarpal and mid-carpal joints [30, 32]. Superficial landmarks should be noted and include the radial artery pulse, flexor carpi radialis tendon, and the ulnar artery pulse. In patients with greater girth, the flexor carpi radialis may be difficult to identify and can be located over the distal pole of the scaphoid at the wrist crease.
The Henry and Trans-FCR Approach
Although similar in the location of the incision and the deep surgical dissection, the Henry approach and trans-FCR approach utilize different superficial intervals prior to exposure of the deep volar compartment, or the space of Parona. The classic Henry interval describes the volar forearm approach to the radius but did not specifically describe exposure of the wrist [31]. It has been extrapolated to be understood that as the Henry approach is taken distally to the level of the wrist the interval will lie between the flexor carpi radialis tendon and the radial artery. In contrast, the trans-FCR approach involves opening the tendon sheath of the flexor carpi radialis tendon and through its floor entry into the deep volar compartment is achieved. Both provide reliable approaches to the volar surface of the distal radius, but the trans-FCR approach affords the benefit of not requiring direct radial artery dissection and isolation. The palmar cutaneous branch of the median nerve is potentially at risk for injury but can be prevented by avoiding any dissection ulnar to the flexor carpi radialis tendon.
The incision is placed longitudinally in line with the flexor carpi radialis tendon. For volar plate insertion, the incision should measure approximately 7–8 cm, but can be extended proximally as needed. If necessary, the wrist crease should be crossed obliquely. Superficially, either the Henry approach can be utilized or the trans-FCR approach. If the latter is used, the flexor carpi radialis tendon should be fully mobilized and retracted ulnarly to maximize release and entry through its tendon sheath floor. Using blunt dissection, the flexor pollicis longus tendon and the flexor digitorum superficialis and profundus tendons are swept ulnarly. Avoid radial retraction of the flexor pollicis longus to avoid potential denervation of the muscle. Retraction is best held with reverse or right angle retractors. Self-retaining retractors should be used with caution. The pronator quadratus is released along its radial border of the distal radius and raised ulnarly (see Fig. 5). In order to facilitate repair of the pronator quadratus upon closure, the release is performed as far radial as possible and should be raised in a sub-periosteal fashion. Alternatively, a cuff of pronator quadrates may be left attached to facilitate repair upon closure. The brachioradialis tendon inserts along the lateral aspect of the distal radius, deep to the first dorsal compartment, and can be released if necessary to eliminate its deforming influence. The tendons of the first dorsal compartment should be identified as they enter their retinaculum and retracted radially thereby exposing the brachioradialis which can then be sharply released off of the styloid. The first dorsal compartment, in contrast, is not typically a deforming force and should be maintained. If also released, the first dorsal compartment should be released with caution to avoid tendon subluxation and hardware irritation.
While exposing the fracture fragments of a distal radius, care must be taken to avoid raising and destabilizing the origin of the volar radiocarpal ligaments distal to the pronator quadratus. The distal limit of the distal radius can be estimated by placing a needle through the joint capsule. Similarly, the radiocarpal joint should not be arthrotomized volarly to avoid devascularization of the carpal bones and radiocarpal ligament destabilization [26]. If joint visualization is necessary, then this should be achieved dorsally through direct dissection and exposure or arthroscopically.
If the carpal tunnel requires release connecting the original incision with the carpal tunnel, incision should be avoided due to the high risk of injury to branches of the palmar cutaneous branch of the median nerve. Similarly, identification and protection of the branches can avoid inadvertent traction or injury. Alternatively, the carpal tunnel can be released through the same incision utilizing distal identification and release of the transverse carpal ligament [33]. The release requires retraction of the FCR tendon from its opened sheath superficially and radially revealing the superficial aspect of the transverse carpal ligament for release. Next, the superficial aspect, the FPL tendon is retracted ulnarly revealing the deep slip of the transverse carpal ligament for subsequent release [33].
A variation to the trans-FCR is the extended FCR approach, which involves release of the “radial septum” and pronation of the proximal radius out of the fracture site to expose the distal radius metaphysis and dorsal fragments [34]. The authors described the radial septum as a simple fascial wall separating the flexor and extensor tendons and include the first dorsal compartment and brachioradialis tendon [34]. Prior to pronating the proximal radius out of the wound, the brachioradialis is released off of the radial styloid, and the first to fifth dorsal compartments are released sub-periosteally off of the dorsal cortex of the radius. Upon release of the extensor tendons, the proximal radius can be pronated out of the wound exposing the distal radial component, metaphyseal comminution, and articular fragments.
The Volar-Extensile Approach
The volar-extensile approach requires placement of an incision further ulnar in a longitudinal fashion between the palmaris longus and flexor carpi ulnaris tendons. The incision is brought obliquely across the wrist into the palm for the carpal tunnel release. The fascia is released between the flexor carpi ulnaris and the palmaris longus, and the interval between the ulnar neurovascular structures deep to the flexor carpi ulnaris ulnarly and the flexor digitorum superficialis/profundus tendons radially is developed. As the dissection is taken distally, the ulnar neurovascular structures are allowed to traverse ulnarly as they travel towards Guyon’s canal and the finger flexor tendons are retracted radially thereby exposing the volar ulnar corner of the distal radius and the floor of the carpal tunnel.
Alternatively, a direct volar approach may be used, utilizing a longitudinal midline incision with an oblique incision across the wrist and incorporates a concomitant carpal tunnel release. In contrast to the volar-extensile approach that protects the median nerve by retracting it with all of the flexor tendons as a group, the direct volar approach involves direct release, exposure, and manipulation of the median nerve and places it at risk for injury and irritation [35]. Lattmann et al. compared the direct volar approach with a concomitant carpal tunnel release versus the standard Henry approach for volar plate fixation of distal radius fractures and found a significant increase in median nerve irritation both early and late following fracture fixation [36].
Radial Approach
The radial approach to the distal radius can be used for radial plate, fragment-specific pin plate, Kirschner wire, and intramedullary fixation (see Fig. 5). Although fairly subcutaneous, approaching the radius along its radial border requires diligent identification and protection of the radial sensory nerve. It becomes subcutaneous approximately 9 cm proximal to the radial styloid as it exits below the brachioradialis tendon and travels distally between it and the extensor carpi radialis longus tendon [15]. The nerve will typically arborize into at least two but on average four branches approximately 5 cm proximal to the radial styloid [15]. The radial sensory nerves have a high predilection towards irritation and the development of neuritis and therefore should be routinely identified and meticulously protected [13, 16]. Deep to the soft tissue in the subcutaneous tissue, the radial aspect of the distal radius is covered by the first and second dorsal compartments traversing the radial styloid as well as the brachioradialis inserting deep into them.
The Radial Approach
Place the incision along the radial side of the wrist in a longitudinal or oblique fashion. Identify the branches of the radial sensory nerve that will be located immediately in the subcutaneous tissue. Gently mobilize and retract these nerves. The first dorsal compartment will be crossing along the volar border of the radial styloid. The second dorsal compartment will be crossing along the dorsal border of the radial styloid. The brachioradialis inserts onto the radial styloid deep into the first dorsal compartment at its base. There will be a bare area between the first and second dorsal compartments at the distal aspect of the radial styloid. To expose the styloid, raise the first compartment in a sub-periosteal fashion volarly. Alternatively, the first compartment’s tendon sheath can be released in its entirety and both the abductor pollicis longus and extensor pollicis brevis tendons can be retracted and the styloid exposed through the compartment floor. Proximally, the brachioradialis can be released in its entirety as needed both for exposure or to eliminate its deforming force [22].
Dorsal Approach
The dorsal approach to the distal radius can be used for dorsal plate and fragment-specific fixation of fractures [6, 12]. Approaching the distal radius along its dorsal surface requires identification and navigation between the dorsal compartments of the wrist (see Fig. 5). The dorsal margin of the distal radius extends further distally then the volar surface, resulting in the volar tilt that is observed on sagittal radiographs. Multiple intervals may be utilized between the various dorsal extensor compartments to approach the distal radius dorsally [35]. Two will be emphasized for their versatility and commonality. The trans-EPL approach, also referred to the “universal dorsal approach,” provides extensile exposure to much of the dorsal aspect of the distal radius. The dorsal–ulnar approach provides direct visualization of the dorsal–ulnar corner of the distal radius as well as the distal radioulnar joint.
The Trans-EPL Approach
Identify and mark Lister’s tubercle. Place a 7–8-cm incision longitudinally in line with the third metacarpal just ulnar to Lister’s tubercle. Dissect down to the extensor retinaculum and then raise full thickness skin flaps. By raising flaps off of the retinaculum, the branches of the radial sensory and dorsal ulnar sensory nerves, and any dorsal veins, will retract away with the flaps. Identify the extensor pollicis longus tendon exiting the extensor retinaculum just distal to Lister’s tubercle. Place a full thickness incision across the extensor retinaculum through the roof of the third dorsal compartment, thereby releasing the extensor pollicis longus tendon. Retract the tendon radially. Raise the second and fourth compartments in a sub-periosteal fashion in opposite directions to thereby expose the dorsal surface of the distal radius.
At the proximal floor of the fourth dorsal compartment resides the posterior interosseous nerve. At this level, it provides sensation and proprioceptive function to the dorsal wrist capsule [37]. In order to expose the nerve, the fourth compartment should be elevated off not sub-periosteally, but rather off of the periosteum. To avoid hardware impingement, it should be retracted and transposed above the hardware. Alternatively, it may be neurectomized proximally by excising a 2-cm segment of the nerve if dorsal capsular denervation is sought [38, 39].
In the case of a distal radius fracture, a formal capsulotomy is not typically required, but if visualization of the radiocarpal joint is necessary, a capsulotomy may be performed in a longitudinal fashion in line with the skin incision. Care must be taken to avoid injury to the scapholunate ligament which typically lies 1.0–1.5 cm distal to Lister’s tubercle. Alternatively, a radially based ligament sparing dorsal capsular flap can be raised to avoid destabilization of the dorsal radiocarpal ligaments while still providing visualization of the radiocarpal and mid-carpal joints [40].
Upon closure, the compartments are allowed to return to their normal positions and the retinacular incision closed. The extensor pollicis tendon may be left outside of the repaired retinaculum to prevent constriction or late tenosynovitis.
The Dorsal–Ulnar Approach
Palpate the distal radioulnar joint and place a longitudinal incision above it. Identify and open the fifth dorsal compartment by visualizing the extensor digiti minimi exiting distally. Through its floor, the distal radioulnar joint can be entered. Multiple components of the distal radioulnar joint, including the TFCC, pronator quadratus volarly, and the radioulnar ligaments, all contribute to distal radioulnar joint stability [41]. The dorsal capsule incorporates the dorsal radiolunar ligament and TFCC. Therefore, upon closure, the dorsal capsule should be meticulously closed to prevent distal radioulnar joint instability but not over-sewn so to avoid loss of forearm rotation (Fig. 6).
Arthroscopic Approach
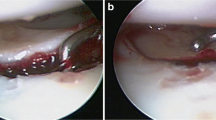
Visualization of the articular surface of the distal radius is best achieved arthroscopically. Often wrist arthroscopy can be performed alone or in conjunction with other open approaches to the distal radius. Arthroscopy affords direct visualization of the radial styloid, scaphoid fossa, lunate fossa, triangular fibrocartilage complex, and the volar radiocarpal ligaments. Appropriate set-up is integral for efficient arthroscopy of the wrist. Traction of 5 to 10 lb provides for adequate visualization and fluid flow. A small joint arthroscope with a diameter of 2.7 mm or smaller and a 30° lens is necessary. Similarly, small joint arthroscopy instruments should be available. Please note that throughout the procedure very little fluid is necessary to facilitate visualization of the joint. In the case of intra-articular fractures of the distal radius, the limb will be predisposed to the potentially devastating complications of proximal fluid extravasation. To minimize this, the forearm can be bandaged or the fluid can be introduced manually, with gravity, or with a low-pressure arthroscopy pump. Alternatively, “dry arthroscopy” has been proposed in the arthroscopic visualization of the wrist to avoid the potential complications of fluid extravasation [42]. Dry arthroscopy of the wrist utilizes the standard portals but no fluid is used. Instead, the joint space is maintained by traction, synoviotome suction, and neurosurgical patties.
Recognition of surface landmarks and understanding the anatomy of the dorsal extensor compartments of the wrist is paramount to facilitating efficient portal placement and joint visualization. Portals are designated by their relationship to the six dorsal compartments (Fig. 7). Palpation between these compartments will identify the sites of joint entry. For example, the 3-4 portal occurs between the extensor pollicis tendon of the third compartment and the extensor digitorum comminis of the fourth compartment. The 3-4 portal is the main viewing portal and is typically established first. It can be identified by palpating the soft spot just distal to Lister’s tubercle. Place the insufflation needle through the planned portal site and inject 5 to 10 cc of saline. Insufflation should occur with little resistance. Place a 3- to 5-mm longitudinal incision over the soft spot with an 11 blade pointing distally. Holding the blade in this position will avoid injury to tendons and any cutaneous nerves since they fan away as they arborize distally. Spread the soft tissue down to the capsule with a hemostat. Enter the joint with a blunt tipped trocar and canula. Avoid iatrogenic injury to the articular surfaces by not aggressively plunging. The normal volar tilt of the distal radius is 10° and this normally should be replicated in the direction of canula entry. In the case of fractures, note prior to portal entry the extent of any dorsal articular surface angulation and comminution that may predispose the joint surface to iatrogenic injury.
Beginning from radial to dorsal, the 3-4 portal will afford excellent visualization of the radial styloid, scaphoid fossa, lunate fossa, and the triangular fibrocartilage complex. In addition, the volar radiocarpal ligaments should be clearly visible as well as the base of the scaphoid and lunate and the intervening scapholunate ligament.
Additional outflow or working portals can be established including the 4-5, 6-R (radial to the extensor carpi ulnaris), and 6-U (ulnar to the extensor carpi ulnaris). The 6-U portal is close to the path of the dorsal ulnar sensory nerve and should be placed with caution. Lastly, the 1-2 portal can be established as an additional viewing portal but is limited by the risk of injury to branches of the radial sensory nerve and limited visualization afforded by the steep radial inclination of the distal radius [16].
Summary
Surgical approaches to the distal radius can be broadly divided into volar, radial, and dorsal. In addition, visualization of the articular surface can be accomplished best arthroscopically, either with fluid or dry. Each approach requires thorough understanding of the local anatomy of the distal radius to safely navigate and expose fractures of the distal radius.
References
Ismail AA, Pye SR, Cockerill WC, Lunt M, Silman AJ, Reeve J, et al. Incidence of limb fracture across Europe: results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int. 2002;13:565–71.
Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26A:908–15.
Koval KJ, Harrast JJ, Anglen JO, Weinstein NJ. Fractures of the distal part of the radius. The evolution of practice over time. where’s the evidence? J Bone Jt Surg. 2008;90:1855–61.
Trumble TE, Schmitt SR, Vedder NB. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg Am. 1994;19A:325–40.
McQueen MM, Hajducka C, Court-Brown CM. Redisplaced unstable fractures of the distal radius: a prospective randomised comparison of four methods of treatment. J Bone Jt Surg. 1996;78B:404–9.
Gesensway D, Putnam MD, Mente PL, Lewis JL. Design and biomechanics of a plate for the distal radius. J Hand Surg Am. 1995;20:1021–7.
Rikli DA, Regazzoni P. Fractures of the distal end of the radius treated by internal fixation and early function. A preliminary report of 20 cases. J Bone Jt Surg [Br]. 1996;78(4):588–92.
Jupiter JB, Fernandez DL, Toh C-L, Fellman T, Ring D. Operative treatment of volar intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1996;78:1817–28.
Fitoussi F, Ip WY, Chow SP. Treatment of displaced intra-articular fractures of the distal end of the radius with plates. J Bone Jt Surg [Am]. 1997;79(9):1303–12.
Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002;27:205–15.
Wigart CR, Wolfe SW. Limited incision open techniques for distal radius fracture management. Orthop Clin North Am. 2001;32:317–27.
Schnall SB, Kim BJ, Abramo A, Kopylov P. Fixation of distal radius fractures using a fragment-specific system. Clin Orthop Relat Res. 2006;445:51–7.
Ilyas AM, Thoder JJ. Intramedullary fixation of displaced distal radius fractures: a preliminary report. J Hand Surg [Am]. 2008;33(10):1706–15.
Melone CP. Open treatment for displaced articular fractures of the distal radius. Clin Orthop. 1988;202:103–11.
Abrams RA, Brown RA, Botte MJ. The superficial branch of the radial nerve: an anatomic study with surgical implications. J Hand Surg [Am]. 1992;17(6):1037–41.
Robson AJ, See MS, Ellis H. Applied anatomy of the superficial branch of the radial nerve. Clin Anat. 2008;21(1):38–45.
Grossman JA, Yen L, Rapaport D. The dorsal cutaneous branch of the ulnar nerve. An anatomic clarification with six case reports. Chir Main. 1998;17(2):154–8.
Mok D, Nikolis A, Harris PG. The cutaneous innervation of the dorsal hand: detailed anatomy with clinical implications. J Hand Surg Am. 2006;31(4):565–74.
Mackinnon SE, Dellon AL. The overlap pattern of the lateral antebrachial cutaneous nerve and the superficial branch of the radial nerve. J Hand Surg Am. 1985;10A:522–6.
Cheung JW, Shyu JF, Teng CC, Chen TH, Su CH, Shyr YM, et al. The anatomical variations of the palmar cutaneous branch of the median nerve in Chinese adults. J Chin Med Assoc. 2004;67(1):27–31.
Watchmaker GP, Weber D, Mackinnon SE. Avoidance of transection of the palmar cutaneous branch of the median nerve in carpal tunnel release. J Hand Surg [Am]. 1996;21(4):644–50.
Koh S, Andersen CR, Buford Jr WL, Patterson RM, Viegas SF. Anatomy of the distal brachioradialis and its potential relationship to distal radius fracture. J Hand Surg [Am]. 2006;31(1):2–8.
Buzzell JE, Weikert DR, Watson JT, Lee DH. Precontoured fixed-angle volar distal radius plates: a comparison of anatomic fit. J Hand Surg [Am]. 2008;33(7):1144–52.
Harness NG, Jupiter JB, Orbay JL, et al. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am. 2004;86A:1900–8.
Andermahr J, Lozano-Calderon S, Trafton T, Crisco JJ, Ring D. The volar extension of the lunate facet of the distal radius: a quantitative anatomic study. J Hand Surg [Am]. 2006;31(6):892–5.
Berger RA, Landsmeer JM. The palmar radiocarpal ligaments: a study adult and fetal human wrist joints. J Hand Surg Am. 1990;15A:847–54.
Siegel DB, Gelberman RH. Radial styloidectomy: an anatomical study with special reference to radiocarpal intracapsular ligamentous morphology. J Hand Surg [Am]. 1991;16(1):40–4.
Ilyas AM, Jupiter JB. Chap 7: distal radius fractures. In: Budoff J, editor. Hand surgery update 4. Rosemont: American Society for Surgery of the Hand; 2008.
Mudgal C, Hastings H. Scapho-lunate diastasis in fractures of the distal radius. Pathomechanics and treatment options. J Hand Surg [Br]. 1993;18B:725–9.
Nana AD, Joshi A, Lichtman DM. Plating of the distal radius. J Am Acad Orthop Surg. 2005;13(3):159–71.
Henry AK. Extensile exposures. Edinburgh: Churchill Livingston; 1973. p. 19.
Kozin SH. Perilunate injuries: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(2):114–20.
Pensy RA, Brunton LM, Parks BG, Higgins JP, Chhabra AB. Single-incision extensile volar approach to the distal radius and concurrent carpal tunnel release: cadaveric study. J Hand Surg Am. 2010;35(2):217–22.
Orbay JL, Badia A, Indriago IR, Infante A, Khouri RK, Gonzalez E, et al. The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Up Extrem Surg. 2001;5(4):204–11.
Fernandez DL. Distal radius/wrist. In: Ruedi TP, editor. AO principles of fracture management. New York: Thieme; 2000. p. 357–77.
Lattmann T, Dietrich M, Meier C, Kilgus M, Platz A. Comparison of 2 surgical approaches for volar locking plate osteosynthesis of the distal radius. J Hand Surg Am. 2008;33(7):1135–43.
Patterson RW, Van Niel M, Shimko P, Pace C, Seitz Jr WH. Proprioception of the wrist following posterior interosseous sensory neurectomy. J Hand Surg Am. 2010;35(1):52–6.
Wilhelm A. Articular denervation and its anatomical foundation. A new therapeutic principle in hand surgery. On the treatment of the later stages of lunatomalacia and navicular pseudarthrosis [in German]. Hefte Unfallheilkd. 1966;86:1–109.
Buck-Gramcko D. Denervation of the wrist joint. J Hand Surg. 1977;2A:54–61.
Berger RA, Bishop AT, Bettinger PC. New dorsal capsulotomy for the surgical exposure of the wrist. Ann Plast Surg. 1995;35(1):54–9.
Palmer AK, Werner FW. Biomechanics of the distal radioulnar joint. Clin Orthop. 1984;187:26–35.
del Piñal F, García-Bernal FJ, Pisani D, Regalado J, Ayala H, Studer A. Dry arthroscopy of the wrist: surgical technique. J Hand Surg Am. 2007;32(1):119–23.
Disclosure
No benefits in any form have been received or will be received by the author related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ilyas, A.M. Surgical approaches to the distal radius. HAND 6, 8–17 (2011). https://doi.org/10.1007/s11552-010-9281-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-010-9281-9