Abstract
Background
Periacetabular osteotomy (PAO) is the treatment of choice for younger patients with developmental hip dysplasia. The procedure aims to normalize the joint configuration, reduce the peak-pressure, and delay the development of osteoarthritis. The procedure is technically demanding and no previous study has validated the use of computer navigation with a minimally invasive transsartorial approach.
Methods
Computer-assisted PAO was performed on ten patients. Patients underwent pre- and postoperative computed tomography (CT) scanning with a standardized protocol. Preoperative preparation consisted of outlining the lunate surface and segmenting the pelvis and femur from CT data. The Biomechanical Guidance System was used intra-operatively to automatically calculate diagnostic angles and peak-pressure measurements. Manual diagnostic angle measurements were performed based on pre- and postoperative CT. Differences in angle measurements were investigated with summary statistics, intraclass correlation coefficient, and Bland–Altman plots. The percentage postoperative change in peak-pressure was calculated.
Results
Intra-operative reported angle measurements show a good agreement with manual angle measurements with intraclass correlation coefficient between 0.94 and 0.98. Computer navigation reported angle measurements were significantly higher for the posterior sector angle (\(1.65^{\circ }\), \(p=0.001\)) and the acetabular anteversion angle (\(1.24^{\circ }\), \(p=0.004\)). No significant difference was found for the center-edge (\(p=0.056\)), acetabular index (\(p=0.212\)), and anterior sector angle (\(p=0.452\)). Peak-pressure after PAO decreased by a mean of 13% and was significantly different (\(p=0.008\)).
Conclusions
We found that computer navigation can reliably be used with a minimally invasive transsartorial approach PAO. Angle measurements generally agree with manual measurements and peak-pressure was shown to decrease postoperatively. With further development, the system will become a valuable tool in the operating room for both experienced and less experienced surgeons performing PAO. Further studies with a larger cohort and follow-up will allow us to investigate the association with peak-pressure and postoperative outcome and pave the way to clinical introduction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In patients with developmental hip dysplasia, the coverage of the femur by the acetabulum is insufficient, leading to pain, disability, and early development of osteoarthritis [1,2,3,4,5]. For patients, without any development of osteoarthritis, a joint preserving periacetabular osteotomy (PAO) has become the treatment of choice [6, 7]. During the procedure, the acetabulum is cut free (leaving the posterior pelvic column intact) and repositioned, normalizing the joint configuration to reduce the peak-pressure and increase the lateral coverage [7, 8]. This is thought to delay the onset of osteoarthritis and improve the survival of the natural joint [9, 10]. However, PAO is a technically demanding procedure, and intra-operative evaluation of the applied correction can be difficult due to the lack of three-dimensional feedback during surgery when using standard single tube fluoroscopy.
With the development of computer-assisted surgery systems such as the Biomechanical Guidance System (BGS), the surgeon can visualize and gain important intra-operative three-dimensional feedback during the procedure [11,12,13]. The BGS provides intra-operative tracking of the acetabular fragment and displays diagnostic angles and peak-pressure measurements in real time. In particular, the acetabular version is difficult for the surgeon to determine using fluoroscopy due to imaging limitations in two dimensions.
Previous work on computer-assisted PAO [14,15,16,17,18] has been based on the procedure introduced by Ganz et al. [8] or a modified rotational osteotomy [19], requiring a more invasive procedure. In this work, performing PAO with a minimally invasive transsartorial approach aims to reduce the soft tissue trauma which has been shown to shorten the duration of surgery, reduce blood loss, transfusion requirements, and length of postoperative rehabilitation [7]. However, it is unclear if this minimally invasive approach is compatible with navigation surgery because the incision from the anterior superior iliac spine descending along the sartorius muscle is only 7 cm long [7]. This offers reduced visibility and limits the accessibility when using the optically tracked pointer of the navigation system [13]. Therefore, it is important to ensure that the method is compatible and to validate the accuracy of computer reported angle measurements against manual CT angle measurements. The goal of PAO is to reduce the peak contact pressure for daily activities; however, it is unknown how the peak-pressure changes postoperatively.
The primary aim of this study was to determine if intra-operative computer navigation reported angle measurements agree with manual angle measurements. The secondary aim was to determine if peak-pressure decreased postoperatively.
Methods
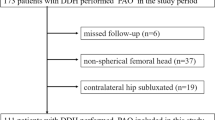
The study was a prospective case series study conducted at Aarhus University Hospital, Denmark. Patients were recruited and operated on between September 2013 and January 2014. Informed consent was obtained from all individual participants included in the study. Ethical approval was obtained from the Central Denmark Region Committee on Biomedical Research Ethics (Journal Number: M-20100274), and the study was registered at Clinical Trials.gov (NCT02015247). In the inclusion period, all patients (\(n=65\)) with hip dysplasia scheduled for PAO were identified and considered for inclusion. Inclusion criteria were: radiological diagnosed dysplasia (center-edge angle \(< 25^{\circ }\)), osteoarthritis degree \(\le 1\) according to the criteria of Tönnis and Heinecke [20], and hip pain. Exclusion criteria were: Legg–Calvé–Perthes disease, neuromuscular diseases, previous major hip surgery, persons with cognitive problems, and age < 18. Due to the need for cleaning and sterilizing the navigation instruments between surgeries, only one patient could be included per day of operation. When multiple candidates were available, the final decision was left to the discretion of the senior author (KS) and the most technically challenging patient was selected. In particular, patients with a retroverted acetabulum were included to evaluate the reliability of the system with a range of cases typically seen in clinical practice.
Patients underwent preoperative computed tomography imaging on a Brilliance 64 (Philips Healthcare, Best, The Netherlands) one week prior to scheduled surgery. Patients were scanned in a supine position from above the L5S1 joint until below the lesser trochanter. All scans were acquired with a voxel size of \(0.45 \times 0.45 \times 0.7\) mm. Postoperative scanning was performed one day postoperatively using the same protocol. The bony pelvis and femurs were automatically segmented by a graph cut segmentation technique [21, 22]. The method uses the second-order Hessian statistics to identify strong edges of the cortical bone and optimally separate the bone from the surrounding soft tissue. The resulting segmentation is then separated into individual bones by connected component analysis, and surface models of the pelvis and femur were created using the marching cubes algorithm [23]. All segmentations were visually inspected and verified to be within voxel accuracy (< 0.45 mm).
The lunate surface was manually segmented using the lunate-trace method described by Armiger et al. [24]. The procedure consists of identifying the center of the femoral head and subsequently selecting points along the medial and lateral edge of the lunate surface on oblique slices through the CT volume at \(7.5^{\circ }\) increments along the medio-lateral axis of the pelvis. A preoperative surgical plan was created based on the biomechanically predicted optimal alignment [11, 13, 25]. However, the surgical plan was not used during surgery and was not revealed to the surgeon in accordance with IRB approval. The preoperative workflow is shown in Fig. 1.
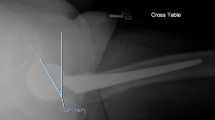
The surgical setup follows that described in Murphy et al. [13]. In summary, prior to the start of the surgery, a Polaris optical tracking system (Northern Digital Inc., Waterloo, Canada) was set up on the contralateral side. During surgery, the surgical assistant performed a pivot calibration of the optically tracked pointer. The surgeon performed the opening and initial approach as described in [7]. In addition, on the contralateral side, two small incisions were made on the iliac crest, and the base of the removable reference geometry (BrainLab, Feldkirchen, Germany) was fixated with two screws. The reference geometry establishes a fixed reference allowing the tracking of the fragment. Before the iliac osteotomy, the pelvis surface model was registered to the patient anatomy. An initial registration was established by touching the anterior superior iliac spine on the operative and contralateral side and the anterior inferior iliac spine on the operative side with the pointer. After collecting surface points on the ilium, pubis, and the iliac crest, a point to surface registration was performed [26]. Before the final osteotomy, four small indentations, referred to as fiducials, were created in an approximately square pattern on the intra-operatively planned fragment using a 1 mm bone burr. The initial position of the fragment was recorded by touching the fiducials with the pointing device. The final osteotomy was completed, and the surgeon re-oriented the fragment under fluoroscopic guidance. As noted above, the BGS-optimized surgical plan was not used during reorientation. When satisfied with the final positioning, the fragment was fixated by the use of two cannulated screws and the final position was recorded by touching the fiducials again in the same order. Validation of the BGS system was performed and was previously reported by Murphy et al. [13, 27]. The procedure for this study was practiced on six cadavers prior to patient inclusion by the operating surgeon and surgical team to reduce the learning curve and establish an efficient workflow. The intra-operative workflow is shown in Fig. 2.
The following diagnostic angles were measured based on CT data and recorded: center-edge angle of Wiberg [28], acetabular index angle of Tönnis [5], posterior sector, anterior sector, and the acetabular anteversion angle [29]. The center-edge angle quantifies the lateral coverage of the acetabulum, and the acetabular index is a measurement of the steepness of the acetabular roof. The posterior and anterior sector angles together with the acetabular anteversion angle quantify the anterior and posterior coverage of the femur. The measured angles are illustrated in Fig. 3. Manual measurements were performed using a custom developed application based on the medical imaging interaction toolkit (MITK) [30]. The program provides the user with an axial, coronal, and sagittal view of the CT data. After selecting the centers of the femoral heads and the most anterior point on the L5S1 joint, the volume is re-oriented such that the axis aligns the centers of the femoral heads. Subsequently, the anterior, posterior, lateral and medial point of the lunate is selected for each hip. Angle measurements are then calculated between the points. Repeated measurements by three observers in an inter- and intra-observer study showed a good intra- and inter-operative reliability with intraclass correlation coefficient (ICC) > 0.94 for all angle measurements. Measurements were repeated to determine the intra-observer reliability in the current study. An experienced operator (SDR) performed all measurements. BGS-reported angle and pressure measurements were calculated based on the segmented lunate surface. In summary, the angle measurements were calculated by finding the intersection points between the lunate trace and the coronal or axial plane [24]. Subsequently, the angles were calculated according to standard definitions. Intra-operative angles were determined before the final osteotomy and after final fixation of the fragment during surgery. Pressure measurements were based on discrete-element analysis, which finds the peak-pressure by simulating the joint force in gait and modeling the pressure distribution on the surface [11].
A schematic overview of the intra-operative workflow. First, the registration between the model and patient is performed by matching the anterior superior iliac spine on the operative and contralateral side and the anterior inferior iliac spine on the operative side with manually selected points on the model (blue and green numbers). After collecting surface points (green points) on the ilium, pubis, and the iliac crest, a point to surface registration was performed to refine the registration. Subsequently four fiducial points (red numbers) are digitized on the planned fragment. Measurements of the position of the fragment and the corresponding angle measurements can then be determined by digitizing the fiducial points
The agreement between computer reported angle measurements and manual measurements was examined by summary statistics and the ICC and Bland–Altman plots to examine bias and limits of agreement [31]. The change in peak-pressure was analyzed as percentage change with respect to baseline. Data were tested for normality by using Shapiro–Wilk test [32] in addition to Skewness and Kurtosis tests. Normally distributed data with equal variances were tested with a paired t-test. Significance level was set at \(p< 0.05\). The study was planned as an initial pilot to gain experience with the procedure and hence the sample size was set to ten patients. All analysis was performed using Stata 13 (StataCorp, College Station, USA).
Results
The study population consisted of the first ten patients to fulfill the inclusion criteria and who accepted to participate in the study. The study population consisted of three males and seven females with a mean age of 32 (median 31.5, range 20 to 47) years.
We found a good agreement between manual and BGS reported angle measurements with ICC varying between 0.94 and 0.98. Results are shown in Table 1. Bland–Altman plots for each angle are shown in Fig. 4. No statistically significant difference was found for the center-edge (\(p=0.056\)), acetabular index (\(p=0.212\)), and anterior sector (\(p=0.452\)) angles, meaning that there was no significant difference between the intra-operative BGS reported angle measurements and the manual measurements. A statistically significant difference was found for the posterior sector (\(p=0.001\)) and acetabular anteversion (\(p=0.004\)) angles. For one patient, the anterior inferior edge of the lunate surface was superior to the center of the femoral head. As a result, no anterior reference point for the calculation of the anterior sector and the acetabular anteversion angle could be found. Hence, the corresponding angle measurements could not be performed, and the patient was excluded for analysis for the corresponding angles. Results for repeated manual measurements are shown in Table 2. A good agreement between repeated manual angle measurements was found with ICC ranging from 0.95 to 0.99. A statistically significant difference was found for the anterior sector angle (\(p=0.007\)).
The mean decrease in peak-pressure for simulated gait after surgery was 13% (95% CI 4–22%, \(p=0.008\)). In one patient, the peak-pressure increased by 5% postoperatively.
Discussion
In PAO, accurate intra-operative evaluation of the reorientation of the acetabular fragment is crucial to obtaining satisfactory results and long-term survival of the biological hip joint [7, 9]. Traditional use of single plane fluoroscopy allows the evaluation of the center-edge angle and acetabular index. However, evaluating the posterior and anterior coverage and the acetabular version using a false profile view with fluoroscopy is difficult. Using a computer navigation system such as the BGS, all angle measurements can be reported as intra-operative feedback to the surgeon, and the peak-pressures without subjecting the patient to extra intra-operative radiation. In this study, we validated the intra-operative measured angle measurements against manual CT-based angle measurements and evaluated the change in peak-pressure.
This study had a number of limitations. First, the study population was limited to ten patients as an initial pilot study to gain experience with the procedure. However, previous to this study the surgeon and surgical team performed a cadaver study with six cadavers to reduce the learning curve using BGS and streamline the surgical workflow. Validation of the BGS system was previously performed on 19 cadavers [13] and 12 clinical surgeries [27]. Second, reorientation was performed under fluoroscopic guidance without use of the information from the navigation system or the BGS calculated preoperative plan. We therefore did not evaluate the ability of the surgeon to achieve the BGS proposed preoperative plan. However, comparing the BGS calculated plan with postoperative results, we found that the optimized reorientation based on peak-pressure differed from the reorientation performed by the surgeon. It is however unclear if the system optimized reorientation leads to long-term satisfactory outcome or if the used algorithm should be adapted to match the planning of an experienced surgeon. In particular, overcorrection may lead to the risk of femoroacetabular impingement and should be taken into account during automatic preoperative planning [33]. This should be validated in a larger randomized controlled study. Third, the pressure calculations are based on the lunate surface based on the bony structure of the acetabulum. A more accurate pressure distribution could be calculated by using the cartilage and the labrum [34]. Techniques for the accurate segmentation of the cartilage and labrum require CT arthrography or magnetic resonance imaging [35]. However, it is believed that the pressure distribution based on CT segmentations of the lunate surface is an accurate approximation of the joint pressures [11, 13, 25].
We found a good agreement between computer navigation reported angle measurements and manual angle measurements with similar results to repeated manual measurements. In a previous study, they found a mean difference between \(-\,0.46^{\circ }\) and \(0.42^{\circ }\) and a standard deviation between \(2.73^{\circ }\) and \(3.30^{\circ }\) in a study with three observers [24]. We found a similar range in mean difference and slightly smaller standard deviations in the current study. This might be attributed to higher quality CT volumes and a smaller in-plane voxel size (0.4 vs. 1.0 mm), allowing for more accurate landmark identification. As noted by Armiger et al. [24], a difference of 1.0 mm in landmark identification can result in a \(2^{\circ }\) difference in angle measurement. We found a statistically significant difference for the acetabular anteversion and posterior sector angles between the intra-operative and manual measurements. From Fig. 4, it is apparent that the BGS exhibits a slight bias with respect to manual measurements. However, the 95% limits of agreement are within the expected variation from previous inter- and intra-observer studies and we conclude that the variation is within the clinically acceptable range [36].
We found that the peak-pressure decreased by a mean of 13% postoperatively in the current study. For one patient, the peak-pressure increased by 5% postoperatively. In Armiger et al. [11], they found a similar case showing an increase of 5% in peak-pressure. They associated the increase with lateral overcorrection and a negative acetabular index angle. This also corresponds to the measurements reported by the BGS system center-edge: \(33.3^{\circ }\) and acetabular index: \(-\,2.6 ^{\circ }\). However, manual angle measurements were center-edge: \(30.1^{\circ }\) and acetabular index: \(-\,0.1^{\circ }\). These values are within optimal acetabular angle limits with a center-edge angle between \(30 ^{\circ }\) and \(40^{\circ }\) and acetabular index of less than \(10^{\circ }\) [37]. In a previous study on the validation of the BGS planning system on 29 dysplastic subjects, a mean decrease of 49.2% peak-pressure was found after optimal reorientation [25]. The optimal plan was calculated by the BGS based on biomechanical simulation of the peak-pressure. This decrease was much larger than we found in the current study. However, the average change in center-edge angle was also larger (\(-\,19.0^{\circ }\,\pm \, 7.7^{\circ }\)) compared to this study (\(-\,10^{\circ }\,\pm \, 6^{\circ }\)). The smaller correction needed for the patients in the current study may therefore lead to a smaller decrease in peak-pressure.
No significant changes to the procedure were needed for the minimally invasive transsartorial approach. The same regions could be accessed for registration and digitalization of the fiducial points. In previous work, it was shown that the average intra-operative patient registration error was 0.7 ± 0.4 mm [13]. In the current study, the average intra-operative patient registration error was 0.6 ± 0.2 mm. In previous studies using the BGS, additional fiducial points were created on the intact area as confidence points. The confidence points were previously introduced to allow recovery if the reference body needed to be removed during surgery or was accidentally moved [27]. However, the reference body used in the current study is removable due to a fixed base and therefore no additional confidence points were needed.
Conclusions
In this work, we investigated and validated the use of computer navigation with a minimally invasive transsartorial approach for PAO on patients with hip dysplasia. The system offers reliable angle measurements intra-operatively and provides the surgeon with three-dimensional visualization of the applied reorientation and the peak-pressure. The additional information with respect to that obtained by fluoroscopy may especially be of value for less experienced surgeons. However, the system may become an important tool for both less experienced and experienced surgeons to ensure optimal reorientation is achieved for all patients. Further studies with a larger cohort and follow-up will allow us to investigate the association with peak-pressure and postoperative outcome and pave the way to clinical introduction.
References
Cooperman DR, Wallensten R, Stulberg SD (1983) Acetabular dysplasia in the adult. Clin Orthop Relat Res No 175:79–85
Reijman M, Hazes JMW, Pols HAP, Koes BW, Bierma-Zeinstra S (2005) Acetabular dysplasia predicts incident osteoarthritis of the hip: the Rotterdam study. Arthritis Rheum 52:787–793
Sharp IK (1961) Acetabular Dysplasia. J Bone Joint Surg Br 43–B:268–272
Siebenrock KA, Schöll E, Lottenbach M (1999) Bernese periacetabular osteotomy. Clin Orthop Relat Res 363:9–20
Tönnis D (1987) Congenital dysplasia and dislocation of the hip in children and adults. Springer, Berlin
Leunig M (2011) Evolution of technique and indications for the Bernese periacetabular osteotomy. Bull NYU Hosp Jt Dis 69(Suppl 1):S42–6
Troelsen A, Elmengaard B, Søballe K (2008) A new minimally invasive transsartorial approach for periacetabular osteotomy. J Bone Joint Surg Am 90:493–498
Ganz R, Klaue K, Vinh TS, Mast JW (1988) A new periacetabular osteotomy for the treatment of hip dysplasias technique and preliminary results. Clin Orthop Relat Res 232:26–36
Hipp JA, Sugano N, Millis MB, Murphy SB (1999) Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res 364:134–143
Troelsen A, Elmengaard B, Søballe K (2009) Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am 91:2169–2179
Armiger RS, Armand M, Tallroth K, Lepisto J, Mears SC (2009) Three-dimensional mechanical evaluation of joint contact pressure in 12 periacetabular osteotomy patients with 10-year follow-up. Acta Orthop 80:155–161
Lepisto J, Armand M, Armiger RS (2008) Periacetabular osteotomy in adult hip dysplasia—developing a computer aided real-time biomechanical guiding system (BGS). Suom Ortoped Traumatol 31:186–190
Murphy RJ, Armiger RS, Lepisto J, Mears SC, Taylor RH, Armand M (2014) Development of a biomechanical guidance system for periacetabular osteotomy. Int J Comput Assist Radiol Surg 10(4):497–508
Akiyama H, Goto K, So K, Nakamura T (2010) Computed tomography-based navigation for curved periacetabular osteotomy. J Orthop Sci 15:829–833
Hsieh P-H, Chang Y-H, Shih C-H (2006) Image-guided periacetabular osteotomy: computer-assisted navigation compared with the conventional technique: a randomized study of 36 patients followed for 2 years. Acta Orthop 77:591–597
Langlotz F, Bächler R, Berlemann U, Nolte LP, Ganz R (1998) Computer assistance for pelvic osteotomies. Clin Orthop Relat Res 354:92–102
Langlotz F, Stucki M, Bächler R, Scheer C, Ganz R, Berlemann U, Nolte LP (1997) The first twelve cases of computer assisted periacetabular osteotomy. Comput Aided Surg 2:317–326
Mayman DJ, Rudan J, Yach J, Ellis R (2002) The Kingston periacetabular osteotomy utilizing computer enhancement: a new technique. Comput Aided Surg 7:179–186
Hsieh PH, Shih CH, Lee PC, Yang WE, Lee ZL (2003) A modified periacetabular osteotomy with use of the transtrochanteric exposure. J Bone Joint Surg Am 85:244–250
Tönnis D, Heinecke A (1999) Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 81:1747–1770
Krčah M, Székely G, Blanc R (2011) Fully automatic and fast segmentation of the femur bone from 3D-CT images with no shape prior. In: ISBI. pp 2087–2090
De Raedt S, Mechlenburg I, Stilling M, Søballe K, Rømer L, de Bruijne M (2013) Automated measurement of diagnostic angles for hip dysplasia. In: Novak CL, Aylward S (eds) Medical imaging 2013: computer-aided diagnosis. SPIE, p 867009
Schroeder W, Martin K, Lorensen B (2006) The visualization toolkit, 4th edn. Kitware, Clifton Park, NY
Armiger RS, Armand M, Lepisto J, Minhas D, Tallroth K, Mears SC, Waites MD, Taylor RH (2007) Evaluation of a computerized measurement technique for joint alignment before and during periacetabular osteotomy. Comput Aided Surg 12:215–224
Niknafs N, Murphy RJ, Armiger RS, Lepisto J, Armand M (2013) Biomechanical factors in planning of periacetabular osteotomy. Front Bioeng Biotechnol 1:20
Besl PJ, McKay HD (1992) A method for registration of 3-D shapes. IEEE Trans Pattern Anal Machine Intell 14:239–256
Murphy RJ, Armiger RS, Lepisto J, Armand M (2016) Clinical evaluation of a biomechanical guidance system for periacetabular osteotomy. J Orthop Surg Res 11:36
Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complications of osteoarthritis. Acta Chir Scand 83:53–68
Anda S, Terjesen T, Kvistad KA, Svenningsen S (1991) Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr 15:115–120
Nolden M, Zelzer S, Seitel A, Wald D, Müller M, Franz AM, Maleike D, Fangerau M, Baumhauer M, Maier-Hein L, Maier-Hein KH, Meinzer H-P, Wolf I (2013) The medical imaging interaction toolkit: challenges and advances: 10 years of open-source development. Int J Comput Assist Radiol Surg 8:607–620
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Shapiro SS, Wilk MB (1965) An analysis of variance test for normality (complete samples). Biometrika 52:591–611
Myers SR, Eijer H, Ganz R (1999) Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res 363:93–99
Anderson AE, Ellis BJ, Maas SA, Peters CL, Weiss JA (2008) Validation of finite element predictions of cartilage contact pressure in the human hip joint. J Biomech Eng 130:051008
Tabrizi PR, Zoroofi RA, Yokota F, Tamura S, Nishii T, Sato Y (2015) Acetabular cartilage segmentation in CT arthrography based on a bone-normalized probabilistic atlas. Int J Comput Assist Radiol Surg 10:433–446
Troelsen A, Rømer L, Kring S, Elmengaard B, Søballe K (2010) Assessment of hip dysplasia and osteoarthritis: variability of different methods. Acta Radiol 51:187–193
Hartig-Andreasen C, Troelsen A, Thillemann TM, Søballe K (2012) What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin Orthop Relat Res 470:2978–2987
Acknowledgements
This study was funded by the Danish Rheumatism Association (Gigtforeningen). We would like to acknowledge Netherlands Organisation for Scientific Research (NWO). The BGS was previously developed under grant number R01EB006839 from National Institutes of Health National Institute of Biomedical Imaging and Bioengineering.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Ryan Murphy is currently with Auris Health, Inc., Redwood City, CA.
Rights and permissions
About this article
Cite this article
De Raedt, S., Mechlenburg, I., Stilling, M. et al. Reliability of computer-assisted periacetabular osteotomy using a minimally invasive approach. Int J CARS 13, 2021–2028 (2018). https://doi.org/10.1007/s11548-018-1802-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-018-1802-y