Abstract
The aim of our study was to assess the performance of contrast-enhanced digital mammography (CEDM) in the preoperative loco-regional staging of invasive lobular carcinoma (ILC) patients, about the valuation of the extension of disease and in measurement of lesions. Then, we selected retrospectively, among the 1500 patients underwent to CEDM at the Breast Diagnostics Department of the Careggi University Hospital of Florence and the National Cancer Institute of Milan from September 2016 to November 2018, 31 women (mean age 57.1 aa; range 41–78 aa) with a definitive histological diagnosis of ILC. CEDM has proved to be a promising imaging technique, being characterized by a sensitivity of 100% in the detection of the index lesion, and of 84.2% in identifying any adjunctive lesions: It was the presence of a non-mass enhancement (NME) to lower the sensitivity of the technique (25% vs. 100% for mass-like enhancements or a mass closely associated with a NME). Specificity in the characterization of additional lesions was 66.7%, and the diagnosis of the extension of disease was correct in 77.4% of cases: NME also led to a decrease in diagnostic accuracy in the evaluation of disease extension up to 40% versus 85% for masses and 80% for masses associated with NME (M/NME). Moreover, in 12/31 (38.7%), CEDM allowed to correctly identify lesions not shown by mammography + ultrasonography + tomosynthesis: In the half of these (6/12), there was a multicentricity, thus allowing an adequate surgical planning change. CEDM was also very accurate in analyzing the maximum diameter of the masses, while it was much less reliable in the case of the M/NME and pure NME. In conclusion, CEDM is a new promising imaging technique in the loco-regional preoperative staging and in the evaluation of disease extension for ILC, especially in case of mass enhancement lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Invasive lobular carcinoma (ILC) is the second most frequent invasive breast cancer (5–15%) after ductal histotype (IDC) (70–90%), compared to which is more difficult to diagnose by mammography and ultrasonography and has a greater tendency to multifocality, multicentricity or bilaterality [1,2,3,4]. Then, magnetic resonance imaging (MRI) is recommended from international guidelines in the preoperative work-up for all ILC patients, thanks to its high sensitivity (95–98%), also in detecting of adjunctive lesions in the ipsilateral or contralateral breast, not previously identified with mammography or US, not even with the most recent advances in these diagnostic techniques [5,6,7,8,9,10,11,12,13,14]. Recently, contrast-enhanced digital mammography (CEDM) has shown a similar sensitivity and an even greater specificity compared to MRI, in the detection of breast lesions, both for index lesions and for possible additional lesions, with lower costs, greater rapidity, greater patient compliance, especially in the claustrophobic, greater availability, and with the possibility to verify if microcalcifications have contrast enhancement, thanks to the perfect correspondence between full-field digital mammography (FFDM) and CEDM images [15,16,17,18,19,20,21]. The aim of our study was to assess the performance of CEDM in the preoperative loco-regional staging of ILC patients, about the valuation of the extension of disease and in measurement of lesions. We also calculated the distribution of frequencies of various histological parameters (i.e., positivity to the receptor for estrogens, positivity to the receptor for the progesterone, ki67, Her-2 positivity) in our sample. Then, we verified if it changed significantly with the different types of contrast enhancement of lesions in CEDM (Table 1).
Materials and methods
Study design
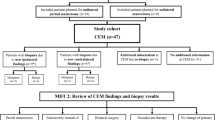
Retrospectively, among the 1500 patients underwent CEDM at the Breast Diagnostics Department of the Careggi University Hospital of Florence and at the National Cancer Institute of Milan from September 2016 to November 2018, we selected 31 women (mean age 57.1 aa; range 41–78 aa) with a definitive histological diagnosis of ILC, with these inclusion criteria: 1) written informed consensus to undergo CEDM; 2) definitive histological diagnosis of ILC, after surgical excision 3) patients underwent ultrasonography, mammography and tomosynthesis examinations previously than CEDM study. We excluded: 1) patients without a definitive histological result (n = 8); 2) patients undergoing CEDM before 2–3 weeks from the biopsy (n = 9), as shown in Figure 1.
CEDM technique
CEDM was performed using a Selenia Dimensions mammography system (Hologic, Marlborough, MA) capable of performing full-field 2D digital mammography, 3D tomosynthesis and CEDM (high and low energy). An intravenous injection of 1.5 ml/kg body weight of an iodine-based contrast agent (Ultravist 370, Bayer HealthCare LLC, Whippany, NJ) was administered with an automated bolus injection with a flow of 3 ml/s, followed by 20 ml of saline solution. The scan started about 2 min after the contrast medium injection, and all 4 standard mammography projections (cranio-caudal and mediolateral oblique images of each breast) were obtained sequentially within 5 min. For each CEDM image, 2 acquisitions were performed at 26–31 kVp with rhodium and silver filters (Rh and Ag) for low-energy acquisition, and at 45–49 kVp with a copper filter for high acquisition power. A recombination algorithm was used to subtract the non-enhanced breast tissue, and then to provide a subtracted image in which only the areas of post-contrastographic enhancement were highlighted: This will allow to evaluate the neoangiogenesis of the tumor, as in MRI. All 4 mammography projections were used for our analysis. Acquisitions in both standard projections (CC and MLO), carried out also 8 min after the administration of the contrast medium, also make it possible to carry out a qualitative assessment of the enhancement’s kinetics. [22, 23]
Imaging interpretation and histological parameters
Two different radiologists, with more than 30 years of experience in breast imaging in the two different hospitals, performed ultrasonography and analyzed mammograms and tomosynthesis of the 31 patients of our study (of which they knew the medical history), according to BI-RADS criteria established by the American College of Radiology (ACR). Then, they analyzed CEDM images of these patients using the same lexicon used to characterize the lesions in MRI according to BI-RADS [24,25,26,27]. “Radiologist A” analyzed images of 24 patients, while 7 cases were analyzed by “Radiologist B”. As in MRI, CEDM classifies all 31 index lesions detected in the subtracted images into three main groups: focus, mass and non-mass enhancement (NME); we also included a further category, called M/NME, when the index lesion is composed by a mass closely associated with a NME component. According to the BI-RADS, they analyzed morphological and kinetics findings of the enhancement of lesions and valuated the number of lesions and then the extension of the disease. The two radiologists measured the maximum diameter of index lesions at CEDM: In case of M/NME, they measure the maximum diameter of the sum of the two components. At the moment of the valuation, the two radiologists know bioptic-histological result, if available (Table 2).
CEDM, additional lesions, extension of disease and histological parameters
We correlated masses, NME and M/NME, identified by the two radiologists with the histological data relating to the extension of the disease, the type of surgery performed, the results of sentinel-node analysis, the histological type of tumor, the grading, a peritumoral/perivascular invasion and histological parameters.
Cedm and dimension of index lesion
We also verified the agreement between the measurement of lesions in CEDM with the sizes at the definitive histology.
Standard of references
Histology was considered the gold standard for disease extension and for the size of lesions: we considered as an admissible error in the measurement an overestimation/underestimate up to 20% compared to the gold standard [28,29,30]. All benign assignments have been confirmed with ultrasonography or stereotactic-guided biopsy. Histological analysis was performed by two pathologists with more than 20 years of experience in breast pathology (Table 3).
Statistical analysis
We calculated CEDM sensitivity and specificity in detecting of adjunctive lesions and the accuracy in assessing the local extent of disease first in the total of the sample and then for the various subgroups, divided for type of contrast enhancement (masses, NME and M / NME). Then, we have analyzed if and how CEDM sensitivity, specificity and accuracy in assessing of the local extent of disease were influenced by the different types of contrast enhancement. Regarding the dimensional analysis of index lesions, mean, median, standard deviation and the ranges of their measurements on the entire sample and in the subgroups were calculated. The Bland–Altman plot was used to explore the agreement between CEDM index lesion measurements and histology (gold standard), and the Intraclass Correlation Coefficient (ICC) was calculated [31, 32]. Freeman–Halton extension of Fisher’s exact probability test was used to verify any significant differences between the masses, NME, M/NME, in the distribution of lesion histological parameters. All statistical significances were calculated with p < 0.05. All data were analyzed by Microsoft Excel (version 2016).
Results
Imaging interpretation and histological parameters
In 100% of the cases (31/31), index lesions were detectable at the CEDM, and in particular in 11/31 (35.5%), it was shown a single lesion, in 9/31 (29.0%) a multifocality, in 10/31 (32.3%) a multicentricity and in 1/31 (3.2%) a bilaterality. The index lesion occurred in 20/31 (64.5%) of the cases like a mass, in 6/31 (19.3%) like NME, in 5/31 (16.1%) like a M/NME, in 0/31 (0%) like focus, and the distribution of their enhancement features is described in Tab.1.
CEDM, additional lesions, extension of disease and histological parameters
In 12/31 (38.7%), CEDM allowed to correctly identify lesions not shown by mammography + ultrasonography + tomosynthesis: In the half of these (6/12), there was a multicentricity, thus allowing an adequate surgical planning change [33,34,35,36,37,38]. In 4/31 (12.9%), CEDM led to an overstaging (3 masses and 1 M/NME), in 3/31 (9.7%) to a downstaging (all NME), in 24/31 (77.4%), the extension diagnosis was correct (95% CI 58.90–90.41). The sensitivity in identifying additional lesions was of 84.2% (95% CI 60.42–96.62); the specificity of 66.7% (95% CI 34.89–90.08). [2, 40,41,42]. CEDM accuracy in identifying the correct extension of disease was: 85% (95% CI 62.11–96.79) for masses (Fig. 2), with a sensitivity of 100.00% (95% CI 71.51–100.00) and a specificity of 66.67% (95% CI 29.93–92.51%); 40% (95% CI 5.27–85.34) for NME, with a sensitivity of 25.00% (95% CI 0.63–80.59) and a specificity of the 100.00% (95% CI 2.50–100.00); 80% (95% CI 28.36–99.49) for M/NME, with a sensitivity of 100.00% (95% CI 39.76–100.00) and a specificity of 0.00% (95% CI 0.00–97.50). Other histological features are shown in Tab.3: They were correlated with the three main categories (masses, NME, M/NME), and no significant variations were found between the various groups [39]. 31/31 (100.0%) lesions had a receptor positivity to estrogens, 24/31 (77.4%) also to progesterone. NME is associated, although without statistical significance (p: 0.20), with a higher risk of a progesterone receptor negativity (3/6, 50.0%), and with statistical significance (p: 0.03) to a moderate (2 +) or high (3 +) HER2 positivity: This significance is further greater (p: 0.021) if we consider the sum of NME and M/NME rather than masses only. FISH analysis in moderate (2 +) HER2 positivity cases showed no gene amplification for all, and then the real and relevant positivity to Her2 was detected in only 1/31 (mass-like lesion). The correlation of the various subgroups with the rate of replication (ki67 < 20%: 67.7%; ki67 ≥ 20%: 32.3%) and with the classification of lesions in the various intrinsic molecular subtypes (according to St. Gallen’s conference in 2013) were evaluated, without statistically significant differences [43].
CEDM and dimension of index lesion
The mean of the maximum diameters, correct measurements, overestimations and underestimations for various enhancement groups is shown in Tab.2. A Bland–Altman plot was performed (Fig. 3) to analyze the differences between the dimension of tumors at CEDM and at histology. Even if the sample size is very small, we applied this also into the various subgroups [44]. Then, we have calculated the Intraclass Correlation Coefficient (ICC) for the entire sample and its result (0.858; 95% IC 0.706–0.932) suggests a good performance of the CEDM in the valuation of the maximum diameter of the lesion. Although the sample size is very small, and therefore requires a multicenter study with a significantly larger sample, we have calculated preliminary data to study the performance of the CEDM in the various contrast enhancement groups: In case of masses (ICC: 0.851; 95% IC 0.623–0.941) and NME (ICC: 0.819; 95% IC − 0.296 to 0.975), CEDM showed a good performance in the dimensional evaluation, while it was worse in case of M/NME (ICC: 0.507; 95% IC − 3.735 to 0.949) [31, 32].
Discussion
In our study, ILC has a significant tendency to multifocality (35.5%), multicentricity (25.8%) or bilaterality (3.2%), rather than unifocality (35.5%), in accordance with the pre-existing literature which shows a multifocality or a multicentricity in 40–60% of cases, greater than the other histotypes and in particular than IDC [4, 10, 12, 35, 39]. Then, a correct loco-regional staging with an evaluation of the extent of the disease is fundamental, even more than in other histological variants, to allow the most appropriate treatment and avoid any complications [45,46,47,48]. For this purpose in our study, CEDM has proved to be a promising imaging technique, thanks to its sensitivity of 100% (vs. 96% reported in the literature for MRI) in the detection of the index lesion, and of 84.2% in identifying any additional lesions (vs. 90%). On the other hand, specificity in the characterization of additional lesions was 66.7% for CEDM (vs. 85% reported in the literature for MRI), and the accuracy for the disease extension evaluation was 77.4% for CEDM (vs. 88%): These data can be caused by the small number of the examined sample (31) and by the lack experience of radiologists with CEDM, which is more recent than MRI [11, 35, 39]. Furthermore, in our study, unlike what was done in previous ones, we analyzed the differences in the various categories of enhancements such as M, NME and M/NME: The presence of a NME led to a lowering of CEDM sensitivity in detecting any additional lesions up to 25%, versus 100% demonstrated in presence of a mass-like enhancement or a M/NME. Specificity was very variable, maximum for NME (100%), intermediate (66.7%) for masses and minimum (0%) for M/NME. All these data need a larger sample to be correctly evaluated. NME led to a decrease in diagnostic accuracy in the evaluation of disease extension up to 40%, unlike what happens for masses (85%) and for M/NME (80%): For the latter categories, data are absolutely similar to the performance of the MRI reported in the literature [35]. NME is associated with a higher risk of downstaging, while masses and M/NME with a higher risk of overstaging, but all not significantly. Our study is the second in the literature about the role of CEDM in the loco-regional staging of ILC. In accordance with the recent study by Patel BK. et al, CEDM proves to be accurate in assessing the maximum diameter of the index lesion, being in agreement with its dimensions at the definitive histology [41]. Even if the sample size is very small, and therefore requires a multicenter study with a significantly larger sample, the performance seems to be better in case of masses or NME, and worse in case of masses closely associated with a non-mass enhancement. As well as in Patel’s study and in other studies, the literature about ILC is described that almost all of lesions present expression of the estrogen receptor, in the ours the 100% of lesions shows a positivity to ER. NME is associated, although not significantly, with a higher risk of a progesterone receptor negativity, while is correlated significantly with an increased expression of Her2 (2 + or 3 +), compared to the presence of a mass enhancement: The necessary additional study with FISH technique on moderate positivity to Her2, however, showed that all were not amplified, and then the real positivity was present only in 1/31 (mass-like lesion). In accordance with the literature, most of the lesions in our study are classified, according to the St. Gallen criteria, as Luminal A (54.8%) while 41.9% are Luminal B/Her2 negative and 3.3% Luminal B / Her2 positive: there aren’t basal-like lesions (1.8% in the literature), and Her2-enriched lesions (0.4% in the literature) [49, 50]. The differences between the various enhancement subgroups of our study, in this case, were not statistically significant. Our study has some important limitations: First, the design is retrospective, a prospective study is needed to confirm or deny our results. Because this is a bi-centric study, the evaluation of the images was performed by different radiologists, as were different the surgeons who managed the patients, planning and performing surgical interventions and the pathologists. Every CEDM examination was analyzed by a single radiologist, and it was impossible to study an interoperating variability. Being a relatively recent diagnostic technique, the lack of experience of radiologists may have been a limitation for the study, especially in the early stages of it, even if as in case of introduction of each new diagnostic technique, it is to be considered a learning curve of the operators; we believe that the experience of over 30 years in breast imaging of our two radiologists of the study has reduced, although only partially, the influence of this limitation. The assessment of the intensity of the enhancement of lesions moreover was qualitative, in the absence, to date, of a validated quantitative system for its measurement in CEDM, and thus also the evaluation of its kinetics. Furthermore, the sample size is small, making definitive results more difficult; therefore, a larger prospective study is needed to confirm our conclusions.
Conclusions
CEDM has proved to be a new promising imaging technique in case of loco-regional preoperative staging for ILC, especially in case of mass enhancement lesions. Anyway, we need a larger prospective and multicentric study to confirm or deny our results.
References
Li CI, Anderson BO, Daling JR, Moe RE (2003) Trends in incidence rates of invasive lobular and ductal breast carcinoma. JAMA 289:1421–1424
Arpino G, Bardou VJ, Clark GM, Elledge RM (2004) Infiltrating lobular carcinoma of the breast: tumor characteristics and clinical outcome. Breast Cancer Res 6:R149–R156
Macchini M, Ponziani M, Iamurri AP et al (2018) Role of DCE-MR in predicting breast cancer subtypes. Radiol Med 123(10):753–764
Berg WA, Gutierrez L, NessAiver MS et al (2004) Diagnostic accuracy of mammography, clinical examination, US, and MR imaging in preoperative assessment of breast cancer. Radiology 233:830–849
Brem RF, Ioffe M, Rapelyea JA et al (2009) Invasive lobular carcinoma: detection with mammography, sonography, MRI, and breast- specific gamma. AJR Am J Roentgenol 192:379–383
Butler RS, Venta LA, Wiley EL, Ellis RL, Dempsey PJ, Rubin E (1999) Sonographic evaluation of infiltrating lobular carcinoma. AJR Am J Roentgenol 172:325–330
Montemezzi S, Cavedon C, Camera L et al (2017) 1H-MR spectroscopy of suspicious breast mass lesions at 3T: a clinical experience. Radiol Med 122(3):161–170
Weinstein SP, Orel SG, Heller R et al (2001) MR Imaging of the breast in patients with invasive lobular carcinoma. AJR Am J Roentgenol 176:399–406
Zanotel M, Bednarova I, Londero V et al (2018) Automated breast ultrasound: basic principles and emerging clinical applications. Radiol Med 123(1):1–12
Mann RM, Hoogeveen YL, Blickman JG, Boetes C (2008) MRI compared to conventional diagnostic work-up in the detection and evaluation of invasive lobular carcinoma of the breast: a review of existing literature. Breast Cancer Res Treat 107:1–14
Selvi V, Nori J, Meattini I, Francolini G, Morelli N, De Benedetto D, Bicchierai G, Di Naro F, Gill MK, Orzalesi L, Sanchez L, Susini T, Bianchi S, Livi L, Miele V (2018) Role of magnetic resonance imaging in the preoperative staging and work-up of patients affected by invasive lobular carcinoma or invasive ductolobular carcinoma. Biomed Res Int. https://doi.org/10.1155/2018/1569060
ACR Guidelines and Standards Committee (2008) ACR practice guideline for the performance of contrast-enhanced magnetic resonance imaging (MRI) of the breast
Kalovidouri A, Firmenich N, Delattre BMA et al (2017) Fat suppression techniques for breast MRI: Dixon versus spectral fat saturation for 3D T1-weighted at 3 T. Radiol Med 122(10):731–742
Mann RM, Kuhl CK, Kinkel K, Boetes C (2008) Breast MRI: guidelines from the European Society of Breast Imaging. Eur Radiol 18:1307–1318
Lee-Felker Stephanie A et al (2017) Newly diagnosed breast cancer: comparison of contrast-enhanced spectral mammography and breast mr imaging in the evaluation of extent of disease. Radiology 285(2):389–400
Jochelson MS, Dershaw DD, Sung JS et al (2013) Bilateral contrast-enhanced dual-energy digital mammography: feasibility and comparison with conventional digital mammography and MR imaging in women with known breast carcinoma. Radiology 266:743–751
Hobbs MM, Taylor DB, Buzynski S, Peake RE (2015) Contrast-enhanced spectral mammography (CESM) and contrast enhanced MRI (CEMRI): patient preferences and tolerance. J Med Imaging Radiat Oncol 59:300–305
Bernardi D, Belli P, Benelli E et al (2017) Digital breast tomosynthesis (DBT): recommendations from the Italian College of BreastRadiologists (ICBR) by the Italian Society of Medical Radiology (SIRM) and the Italian Group for Mammography Screening (GISMa). Radiol Med 122(10):723–730
Patel BK, Gray RJ, Pockaj BA (2017) Potential cost savings of contrast-enhanced digital mammography. AJR Am J Roentgenol 5:1–7. https://doi.org/10.2214/AJR.16.17239
Luczynska E, Heinze-Paluchowska S, Hendrick E et al (2015) Comparison between breast MRI and contrast-enhanced spectral mammography. Med Sci Monit 21:1358–1367
Francescone MA, Jochelson MS, Dershaw DD, Sung JS, Hughes MC, Zheng J, Moskowitz C, Morris EA (2014) Low energy mammogram obtained in contrast-enhanced digital mammography (CEDM) is comparable to routine full-field digital mammography (FFDM). Eur J Radiol 83(8):1350–1355
Bicchierai G, Nori J, De Benedetto D, Boeri C, Vanzi E, Bianchi S, Kaur Gill M, Cirone D, Miele V (2018) Role of contrast-enhanced spectral mammography in the post biopsy management of B3 lesions: preliminary results. Tumori J 17:300891618816212
Trimboli RM, Codari M, Khouri Chalouhi K et al (2018) Correlation between voxel-wise enhancement parameters on DCE-MRI and pathologicalprognostic factors in invasive breast cancers. Radiol Med 123(2):91–97
Bicchierai G, Di Naro F, Amato F (2018) CEDM lexicon and imaging interpretation tips. In: Nori J, Kaur M (eds) Contrast-enhanced digital mammography (CEDM), chapter. 9; pp 93–118. Springer, Berlin. ISBN 978-3-319- 94552-1. eBook ISBN 978-3-319-94553-8. https://doi.org/10.1007/978-3-319-94553-8_9
D’Orsi CJACR (2013) BI-RADS atlas: breast imaging reporting and data system. American College of Radiology, Reston
Morris EA, Comstock CE, Lee CH et al (2013) ACR BI-RADS® magnetic resonance imaging. In: ACR BI-RADS® Atlas, Breast imaging reporting and data system. American College of Radiology, Reston
Bartolotta TV, Orlando A, Cantisani V et al (2018) Focal breast lesion characterization according to the BI-RADS US lexicon: role of a computer-aided decision-making support. Radiol Med 123(7):498–506
Hilleren DJ, Andersson IT, Lindholm K, Linnell FS (1991) Invasive lobular carcinoma: mammographic findings in a 10-year experience. Radiology 178:149–154
Krecke KN, Gisvold JJ (1993) Invasive lobular carcinoma of the breast: mammographic findings and extent of disease at diagnosis in 184 patients. AJR Am J Roentgenol 161:957–960
Le Gal M, Ollivier L, Asselain B, Meunier M, Laurent M, Vielh P (1992) Mammographic features of 455 invasive lobular carcinomas. Radiology 185:705–708
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Koo Terry K, Li Mae Y (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Lee-Felker SA et al (2017) Newly diagnosed breast cancer: comparison of contrast-enhanced spectral mammography and breast MR imaging in the evaluation of extent of disease. Radiology 285(1):389–400
Boetes C et al (1995) Breast tumors: comparative accuracy of MR imaging relative to mammography and US for demonstrating extent. Radiology 197(3):743–747
Schelfout K et al (2004) Preoperative breast MRI in patients with invasive lobular breast cancer. Eur Radiol 14(7):1209–1216
Carin Anne-julie, Molière Sébastien, Gabriele Victor, Lodi Massimo, Thiébaut Nicolas, Neuberger Karl, Mathelin Carole (2017) Relevance of breast MRI in determining the size and focality of invasive breast cancer treated by mastectomy: a prospective study. World J Surg Oncol 15:128. https://doi.org/10.1186/s12957-017-1197-1
Marino MA, Pennisi O, Donia A et al (2017) Organizational and welfare mode of breast centers network: a survey of Sicilian radiologists. Radiol Med 122(9):639–650
Gruber IV et al (2013) Measurement of tumour size with mammography, sonography and magnetic resonance imaging as compared to histological tumour size in primary breast cancer. BMC Cancer 13(1):328
Kneeshaw PJ, Turnbull LW, Smith A, Drew PJ (2003) Dynamic contrast enhanced magnetic resonance imaging aids the surgical management of invasive lobular breast cancer. Eur J Surg Oncol 29(1):32–37
Rodenko GN, Harms SE, Pruneda JM, Farrell RS Jr, Evans WP, Copit DS, Krakos PA, Flamig DP (1996) MR imaging in the management before surgery of lobular carcinoma of the breast: correlation with pathology. AJR Am J Roentgenol 167(6):1415–1419
Patel BK, Davis J, Ferraro C, Kosiorek H, Hasselbach K, Ocal T, Pockaj B (2018) Value added of preoperative contrast enhanced digital mammography in patients with invasive lobular carcinoma of the breast. Clin Breast Cancer. https://doi.org/10.1016/j.clbc.2018.07.012
Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, Senn H-J (2013) Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol 24(9):2206–2223
Jiang Yi-Zhou, Xia Chen, Peng Wen-Ting, Ke-Da Yu, Zhuang Zhi-Gang, Shao Zhi-Ming (2014) Preoperative measurement of breast cancer overestimates tumor size compared to pathological measurement. PLoS ONE 9(1):e86676. https://doi.org/10.1371/journal.pone.0086676
Fallenberg EM, Dromain C, Diekmann F et al (2014) Contrast-enhanced spectral mammography versus MRI: initial results in the detection of breast cancer and assessment of tumour size. Eur Radiol 24:256–264
Zheng Y, Zhong M, Ni C et al (2017) Radiotherapy and nipple-areolar complex necrosis after nipple-sparing mastectomy: asystematic review and meta-analysis. Radiol Med 122(3):171–178
Kanyilmaz G, Aktan M, Koc M et al (2017) Unplanned irradiation of internal mammary lymph nodes in breast cancer. Radiol Med 122(6):405–411
Thomas M, Kelly ED, Abraham J et al (2019) Invasive lobular breast cancer: a review of pathogenesis, diagnosis, management, and future directions of early stage disease. Semin Oncol 46(2):121–132
Fiorentino A, Mazzola R, Naccarato S et al (2017) Synchronous bilateral breast cancer irradiation: clinical and dosimetrical issues using volumetricmodulated arc therapy and simultaneous integrated boost. Radiol Med 122(6):464–471
Iorfida Monica, Maiorano Eugenio, Orvieto Enrico, Maisonneuve Patrick, Bottiglieri Luca, Rotmensz Nicole, Montagna Emilia, Dellapasqua Silvia, Veronesi Paolo, Galimberti Viviana, Luini Alberto, Goldhirsch Aaron, Colleoni Marco, Viale Giuseppe (2012) Invasive lobular breast cancer: subtypes and outcome. Breast Cancer Res Treat 133:713–723. https://doi.org/10.1007/s10549-012-2002-z
Fallahpour S, Navaneelan T, De P, Borgo A (2017) Breast cancer survival by molecular subtype: a population-based analysis of cancer registry data. CMAJ Open 5:E734–E739
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee: “Regione Toscana, Comitato Etico Area Vasta Centro, reference number: SPE_16.251” and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical standards
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amato, F., Bicchierai, G., Cirone, D. et al. Preoperative loco-regional staging of invasive lobular carcinoma with contrast-enhanced digital mammography (CEDM). Radiol med 124, 1229–1237 (2019). https://doi.org/10.1007/s11547-019-01116-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-019-01116-7