Abstract
Aim
To assess the amount of computed tomography (CT) scans for minor head injury (MHI) performed in young patients in our emergency department (ED), not indicated by National Institute for Health and Clinical Excellence (NICE) and Canadian Computed Tomography Head Rules (CCHR), and to analyze factors contributing to unnecessary examinations. Secondary objectives were to calculate the effective dose, to establish the number of positive CT and to analyze which of the risk factors are correlated with positivity at CT; finally, to calculate sensitivity and specificity of NICE and CCHR in our population.
Materials and methods
We retrospectively evaluated 493 CT scans of patients aged 18–45 years, collecting the following parameters from ED medical records: patient demographics, risk factors indicating the need of brain imaging, trauma mechanism, specialty and seniority of the referring physician. For each CT, the effective dose and the negativity/positivity were assessed.
Results
357/493 (72%) and 347/493 (70%) examinations were not in line with the CCHR and NICE guidelines, respectively. No statistically significant difference between physician specialty (p = 0.29 for CCHR; p = 0.24 for NICE), nor between physician seniority and the amount of inappropriate examinations (p = 0.93 for CCHR, p = 0.97 for NICE) was found but CT scans requested by ED physicians were less inappropriate [p = 0.28, odds ratio (OR) 0.562, CI (95%) 0.336–0.939]. There was no statistically significant correlation between patient age and over-referral (p = 0.74 for NICE, p = 0.93 for CCHR). According to NICE, low speed motor vehicle accident (p = 0.009), motor vehicle accident with high energy impact (p < 0.01) and domestic injuries (p = 0.002) were associated with a higher rate of unwarranted CT; according to CCHR only motor vehicle accident with high energy impact showed a significant correlation with unwarranted CT scan (p < 0.001, OR 44.650, CI 33.123–1469.854). 2% of CT was positive. Multivariate analysis demonstrated that factors significantly associated with CT scan positivity included signs of suspected skull fracture (p < 0.001, OR 20.430, CI 2.727–153.052) and motor vehicle accident with high energy impact (p < 0.001, OR 220.650, CI 33.123–1469.854). In our series, CCHR showed sensitivity of 100%, specificity of 74%; NICE showed sensitivity of 100%, specificity of 72%.
Conclusion
We observed an important overuse of head CT scans in MHI; the main promoting factor for inappropriate was injury mechanism. 2% of head CT were positive, correlating with signs of suspected skull fracture and motor vehicle accident with high energy impact.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Head trauma is a frequent cause for emergency department (ED) access (1.7–2 million/year in US) [1] and is considered a public health concern, with a major economic burden on health care services [2]. More than 75% of head trauma arriving at ED are classified as minor head injury (MHI) [3], which is defined as a history of loss of consciousness, amnesia, or disorientation, with Glasgow Coma Scale (GCS) from 13 to 15 [3]. Head CT is considered the gold standard for the evaluation of head trauma, due to its high sensitivity for detecting brain hemorrhage and skull fractures [4], but the dramatic increase in its use has raised some concerns about its applicability, cost burden, ionizing radiation exposure, especially in the emergency setting [5, 6].
Since < 1% of MHI needs surgical interventions [3, 7, 8], the execution of head CT in all MHI patients would not be fully justifiable economically and would expose patients to an unjustified radiation dose. Rigorously validated clinical decision rules have been introduced to establish which patients are eligible for brain imaging and to manage patients suffering from MHI. The most used clinical decision rules are: National Institute for Health and Clinical Excellence (NICE) [9], Canadian Computed Tomography Head Rules (CCHR) [3], American College of Emergency Physician (ACEP) [10], Neurotraumatology Committee of the World Federation of Neurosurgical Societies (NCWFNS) [11], National Emergency X Radiography Utilization Study (NEXUS-II) [12], New Orleans Criteria (NOC) [7], and Scandinavian Clinical Decision Rules [13]. Their main goal is to reduce costs and exposure to ionizing radiation [14].
NICE and CCHR proved to have high value of specificity in detecting intracranial lesions needing neurosurgical intervention [3, 4, 15].
Despite these guidelines, the overuse of head CT in MHI still remains a diffuse problem both for patients-related and non-clinical human factors [16].
Therefore, our aim was to assess the amount of CT scans for MHI performed in relatively young patients in our ED that are not recommended by NICE and CCHR guidelines, and to analyze factors contributing to unnecessary examinations.
Secondary objectives were: to calculate the effective dose of head CT scans, to establish the rate of positive CT scans in our population and to analyze which of the risk factors, included in the clinical decision rules selected in our study, are correlated with CT positivity in our series.
Materials and methods
Patient population
Institutional review board approval was granted for this study with a waiver of the requirement to obtain written informed consent from each patient.
We choose to study a relatively young population of patients, as more sensitive to radiation exposure.
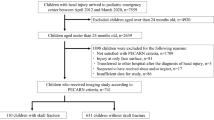
We retrospectively evaluated head CT scans of consecutive patients aged 18–45 years from January 1 to June 30th 2016, presented for MHI to the Emergency Department of an urban Hospital of Milan (Northern Italy) with a number of access to the ED of 100,000/year.
Our exclusion criteria were: patients aged < 18 years or > 45 years, trauma occurred > 24 h before the access in ED, GCS < 13, missing clinical data, refusal to undergo head CT scan, head CT scan performed at the request of the patient, unreliable history provided by the patient, and head trauma resulting from syncope or seizure. All head CT scans were executed between 30 and 180 min from the patients’ arrival at the ED (mean time: 75 ± 25).
Clinical decision rules
Because of their high values of sensitivity and specificity, we chose to use the following clinical decision rules: NICE and CCHR guidelines.
NICE [9] include the following risk factors: (1) GCS score < 13 on arrival in the ED, (2) GCS score < 15 at 2 h after head injury on assessment in the ED, (3) suspected open or depressed skull fracture, (4) any sign of basal skull fracture: hemotympanum, “panda” eyes, cerebrospinal fluid leakage from ear or nose, Battle’s sign, (5) post traumatic seizure, (6) focal neurological deficit, (7) > 1 episode of vomiting.
CCHR [3] include: (1) GCS score < 15 at 2 h after injury, (2) suspected open or depressed fracture, (3) any sign of basal skull fracture: hemotympanum, “raccoon” eyes, cerebrospinal fluid leakage from ear or nose, Battle’s sign, (4) ≥ 2 episodes of vomiting, (5) age ≥ 65 years, (6) amnesia before impact ≥ 30 min, or dangerous mechanism of trauma (e.g., pedestrian struck by motor vehicle, occupant ejected from motor vehicle, fall from height > 3 feet or 5 stairs).
We evaluated if the included CT scans met the NICE and CCHR guidelines.
Data collection: risk factors
For every patient included in this study, we collected the following parameters from ED medical records: patient demographics, GCS, headache, vomit (> 1 episode), dizziness, loss of consciousness, amnesia > 30 min, post traumatic seizure, presence of focal neurological deficit (any new posttraumatic neurological complaint: sensory or motor abnormality, abnormal speech, visual change, and hearing defects), well-evident head wound, signs of suspected skull fracture, hemotympanum, raccoon/panda eyes, presence of cerebrospinal fluid leakage from the nose/ear, previous cerebral surgery, alcohol assumption, and oral anticoagulant assumption.
Data collection: trauma mechanism
We categorized the mechanism of trauma as follows: (1) low-speed motor vehicle accident (as a passenger or driver or pedestrian), (2) motor vehicle accident (as a passenger or driver or pedestrian) with high-energy impact, (3) work accident, (4) domestic injury, (5) assault, (6) accidental fall injury, (7) sports injury, (8) self-induced injury (voluntary collision against wall/window), (9) hit by an object.
Data collection: physician characteristics
We also assessed the specialty of the referring physician to the CT scan: (1) emergency physician, (2) general surgeon, (3) orthopedic, (4) neurosurgeon, (5) neurologist, (6) ophthalmologist, and the seniority of the referring physician (only specialized physicians and not residents work in our ED), divided in three groups: (1) < 5 years, (2) 5–10 years, (3) ≥ 10 years.
CT protocol
All CT scans were performed on a second-generation dual-source scanner, Somatom Definition Flash (Siemens, Forchheim, Germany); parameters of acquisition: kV: 120, Reference mAs: 320 (Care Dose), collimation: 128 × 0.6 mm, tube rotation: 1 s; pitch value: 0.55; scan direction: caudocranial; reconstruction thickness: 5 mm; reconstruction filters: H30 for parenchyma and H60 sharp for bone.
CT analysis
For each examination, we determined the radiation exposure from the effective dose, automatically calculated by NEXO [DOSE] Multi-Modality Radiation Informatics, and the negativity/positivity of the examination (established by two neuroradiologists in consensus, who revised all the examinations), considering positivity as follows: (1) subarachnoid hemorrhages, (2) intracerebral hemorrhages, (3) skull fractures, (4) subdural hemorrhages.
Statistical analysis
Statistical analysis was performed using SPSS (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp).
Percentages of patients who underwent head CT not indicated by the NICE or CCHR were calculated.
We compared differences among patients who underwent head CT not indicated by the NICE or CCHR using Pearson χ2 test for categorical variables and Mann–Whitney U test for continuous variables.
A multivariable model for predicting inappropriate head CT request was built, by subjecting variable with a p value less than 0.200 to a backward stepwise logistic regression procedure. Adjusted odds ratios with 95% confidence intervals were estimated for each risk factor.
We then sought to determine predictive factors of positive head CT in our cohort. We performed group comparison using Pearson χ2 test for categorical variables and Mann–Whitney U test for continuous variables to identify any risk factor with statistically significant correlation with positive head CT. A multivariable model for predicting positive head CT was built, as previously described.
A two-tailed p value of < 0.05 was considered significant.
Finally, we calculated the sensitivity, specificity, positive predictive value and negative predictive value of NICE and CCHR in the prediction of positive head CT after trauma.
Results
Appropriateness according to the guidelines
A total of 493 CT scans were collected; 357 (72%) and 347 (70%) examinations were not indicated according to the CCHR and NICE, respectively.
Promoting factors: referring physicians’ characteristics
The total number of requested CT scans divided by types of physician specialty and by physicians’ seniority and number of inappropriate requested CT scans divided by types of specialty according to NICE and CCHR is shown in Table 1. No statistically significant difference between the specialty of the referring physician and over-referral was found (p = 0.29 for CCHR; p = 0.24 for NICE), nor between the seniority of the referring physician and the amount of inappropriate examinations (p = 0.93 for CCHR, p = 0.97 for NICE).
The correlation between the different types of physician specialty and the three-different referring physician age range and inappropriately requested CT scans is shown in Table 2.
At multivariate analysis, CT scans requested by emergency physicians were found to be less inappropriate than those required by other types of physician for NICE guideline [p = 0.28, odds ratio (OR) 0.562, CI (95%) 0.336–0.939]. No other significant correlation was found at multivariate analysis.
Promoting factors: patient age
The mean age of the patients in our group was 32 ± 3 years.
Analyzing the relationship between the patient age and unwarranted CT studies, we found no statistically significant correlation (p = 0.74 for NICE and p = 0.93 for CCHR).
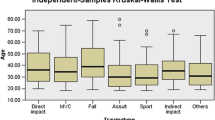
Promoting factors: trauma mechanism
The number of traumas divided for mechanism and the correlation between the trauma mechanism and inappropriate CT are shown in Tables 3 and 4, respectively.
Regarding the trauma mechanism, we observed that only three types of trauma showed a statistically significant correlation with unwarranted CT scans considering NICE guideline: low-speed motor vehicle accident (p = 0.009), motor vehicle accident with high-energy impact (p < 0.01) and domestic injuries (p = 0.002), while according to CCHR only motor vehicle accident with high-energy impact showed a statistically significant correlation with unwarranted CT scan (p < 0.005).
At multivariate analysis, the only trauma mechanism showing statistically significant association with inappropriate CT considering CCHR guideline was motor vehicle accident with high-energy impact (p < 0.001, OR 44.650 CI 33.123–1469.854). No significant correlation was found between trauma mechanisms and inappropriate CT requests according to NICE at multivariate analysis.
CT scans positivity and risk factors related to CT positivity
Only 10/493 CT scans were positive (2%), divided as follows: (1) subarachnoid hemorrhages (SAH), n = 2, (2) intracerebral hemorrhages (IH), n = 1, (3) skull fractures (SF), n = 3, (4) subdural hemorrhages (SDH), n = 1; one patient had IH + SAH, one patient had SF + SAH, one patient had IH + SAH + SDH.
2/10 of the positive CT did not meet NICE and CCHR criteria, 1 CT showed a fracture of the frontal bone and 1 CT demonstrated a fracture of the temporal bone; in both cases the patients did not show any risk factor included in the clinical guidelines. Moreover, one positive CT highlighted the presence of small parenchymal frontal hemorrhages, subarachnoid hemorrhage and subdural hemorrhage; in this case, the patient presented only with seizure, therefore, the CT scan met the NICE criteria, but not the CCHR.
1/10 patients (whose CT scan met both NICE and CCHR criteria) required neurosurgical intervention; the other patients underwent clinical follow-up and CT repetition till the resolution of the anomalies.
We analyzed the correlation between CT scan positivity and risk factors and trauma mechanisms at univariate and multivariate analysis (Table 5).
At univariate analysis, we observed a significant correlation between abnormal CT scan, and well-evident head wound (p < 0.001), signs of suspected skull fracture (p < 0.001), hemotympanum (p < 0.001), panda/raccoon eyes (p = 0.02), trauma with high energy impact (p < 0.001), and sport injuries (p = 0.01). Multivariate analysis demonstrated that factors significantly associated with CT scan positivity included signs of suspected skull fracture (p < 0.001, OR 20.430, CI 2.727–153.052) and motor vehicle accident with high-energy impact (p < 0.001, OR 220.650, CI 33.123–1469.854).
CT scan effective dose (ED)
Mean ED was 2.2 ± 0.2 mSv, calculated by NEXO [DOSE].
Sensitivity and specificity of CCHR and NICE
In our series, NICE showed sensitivity of 100%, specificity of 74%, accuracy of 74%, positive predictive value (PPV) of 7%, and negative predictive value (NPV) of 100%.
CCHR showed sensitivity of 100%, specificity of 72%, accuracy of 72%, PPV of 7%, and NPV of 100%.
Discussion
In the diagnostic workup of head trauma, head CT is the first imaging investigation to be executed because it is widely available, fast, and has a high sensitivity for the detection of intracranial injuries requiring neurosurgery [17]. However, its use creates concern about costs and radiation exposure when applied to large population. To decide whether to perform CT imaging, various clinical decision rules have been developed; among these, the NICE and CCHR have been used in our study.
According to both guidelines, we observed an important overuse of head CT, greater than the data reported in literature.
Jame et al. [18], in a study on 400 patients with MHI, reported that 36.8% patients had no indication for the execution of the CT scan, according to a list of CT indications created by a panel of experts from a revision of the literature. Klang et al. [19] considering CCHR as reference, observed 10.9% of CT scans non-appropriate in the population study in general, and 37.3% of non-indicated examinations, when analyzing patients younger than 65 years. Melnick et al. [20], in their study on 346 patients found a proportion of appropriate CT for head trauma in MHI of 64.7% according to CCHR, of 86.7% according to NICE, of 74.3% for ACEP, and 90.5% for NOC. When investigating the possible contributing factors for unwarranted CT, we did not find a significant association with physician specialty, while Jame et al. [18] found that the risk of inappropriate examinations by ENT specialists was five times higher than by emergency physician, and Klang et al. [19] showed a significant higher tendency of the neurologists to request non-indicated CT.
No type of seniority was statistically significant as a risk factor, as also reported by Klang et al. [19], even if in the latter study residents are included. In our study, only specialized physicians work in our emergency room, and the level of experience of our first aid physicians can be considered more homogeneous.
Significant correlation between patient age and unwarranted CT was not observed in our group, unlike other series [19] and this can be explained by the fact that we considered a restricted age range of young patients.
When analyzing the mechanism of head trauma, motor vehicle accidents with high-energy impact was found to be a significant risk factor for non-indicated CT for both NICE and CCHR; these findings are in line with Klang et al. [19]. Moreover, we found an association between domestic injuries and appropriate CT scans only for CCHR (p = 0.02).
Since in our case series we found many inappropriate requests for CT but few correlations with the clinical parameters, we can assume that there are other non-clinical factors that influence CT examinations requirements, such as the physician’s attitude towards the patient, fear of litigation and of missed diagnosis, patient expectations and compensation methods, as suggested by Melnick et al. [16]. Other proposed non-clinical factors related to the inappropriate/different use of head CT in ED were race/ethnicity [21] and patient economic factors [22]. Therefore, we can hypothesize that the problem of CT overuse in MHI is a complex issue, involving clinical and non-clinical factors. The differences between our data and those reported in the literature can be largely explained by the different models of Health organization in the various countries: given that in Italy the access to the exams is not bound to the presence of a patient’s insurance, the use of the CT scan in the emergency department is more widespread than in other countries and not limited by patient social or economic factors.
In our case series, we found only 10 positive CT (about 2%) and this is less than what reported by Lee [23], who observed an important increase of the use of head CT in head trauma from 2001 to 2007 with a constant rate of detected intracranial hemorrhages (that is 3%) and by Sadegh et al. [8], who observed 13% of abnormal CT in a group of 500 patients affected by minor head trauma. However, in their series the patients had at least one of the risk factors included in decision rules. In our group of abnormal CT scans, we did not observe a significant prevalence of brain contusions, as previously reported [3, 7, 8, 24, 25], while subarachnoid hemorrhage was the most frequent finding. Analyzing the correlation between trauma mechanisms, risk factors and CT positivity, at univariate analysis we observed a significant correlation between abnormal CT scan, and well-evident head wound, signs of suspected skull fracture, hemotympanum, raccoon eyes, motor vehicle accident with high energy impact, and sport injuries. At multivariate analysis, we found a correlation with only two variables: signs of suspected skull fracture and motor vehicle accident with high-energy impact.
The evidence that suspected skull fracture is correlated with CT abnormal findings has already been reported [18], as well as the presence of hemotympanum and raccoon eyes, that are both signs of basal skull fracture [3, 7, 8, 18, 26].
As in other studies, headache and amnesia did not have a significant association with positive CT scan [3, 7, 8, 24]. Previous studies demonstrated a correlation between abnormal CT and various risk factors, such as focal neurological deficit [8, 25,26,27], loss of consciousness [28], and GSC [8, 29].
In our study, the majority of risk factors did not show a significant correlation with abnormal head CT, and this can be explained by the fact that in our series only a reduced number of patients had a positive CT scan.
In our case series, only 1/493 patient needed a neurosurgical intervention, and this rate is below the data reported in the literature; Sadegh et al., in a study on MHI including patients who had at least one risk factor according to clinical decision rules reported a rate of MHI patients needing neurosurgery of 1% [8], Stiell et al. of 1.4% [3] and Geijerstam et al. of 0.9% [29]; our data are more similar to the one reported by Haydel et al., of 0.4% [7].
Calculating the radiation exposure from our CT scan, the effective dose of about 2 mSv is similar to the dose reported in literature [23, 30].
The main concern regarding the use of CT in the ED is that CT is a significant source of radiation exposure [31, 32]. The radiation sensitivity is greatest in childhood, but cancer risk persists into adulthood, especially in young adults, as in our population. Effective dose varies according to patient age, conduct of scan and CT scanner. Individual cancer risk is a multifactorial entity that is difficult to estimate; however, age, sex and delivered examination dose are important contributing factors [32,33,34]. 2 mSv is a relatively low dose of radiation exposure, anyway, the risk from repeated low-dose exposure need to be considered [24, 31, 32]. In our case series, we observed two patients with abnormal CT whose CT scan was not required according to both CCHR and NICE, and one patient with intracranial post traumatic lesions with CT scan indicated by NICE but not by CCHR; therefore, on the one hand we can consider that a close adhesion to the guidelines would have resulted in missing post-traumatic findings, on the other hand, none of the patients with a CT scan not in line with the clinical guidelines required a neurosurgical intervention.
This is a retrospective study; we carefully analyzed patient medical records for any sign and symptoms, but we have to consider the possibility that patients who underwent CT scan had signs/symptoms that could justify the execution of brain imaging but were not reported in the medical records and this fact can lead to an overestimation of the rate of non-indicated CT, even if we can suppose that severe signs or symptoms have been registered.
Moreover, this study was conducted in a single Institution with a particular organization and may not be generalizable to another ED.
Conclusions
In conclusion, we observed an overuse of CT scan in MHI in young patients according to both CCHR and NICE guidelines. The main contributing factor for over-referral was injury mechanism.
In our case series, 2% of positive CT scans were observed, and a correlation between CT positivity and signs of suspected skull fracture and motor vehicle accident with high-energy impact.
The overuse of head CT scan in MHI is the cause of unnecessary radiation exposure and health care cost. An analysis of the causes for overuse should be carried out in every ED to target specific interventions, education of the staff, compliance with the guidelines, and revision of the management protocols.
References
Morton MJ, Korley FK (2012) Head computed tomography use in the emergency department for mild traumatic brain injury: integrating evidence into practice for the resident physician. Ann Emerg Med 60(3):361–367
Smits M, Dippel DW, Nederkoorn PJ, Dekker HM, Vos PE, Kool DR, van Rijssel DA, Hofman PA, Twijnstra A, Tanghe HL, Hunink MG (2010) Minor head injury: CT-based strategies for management—a cost-effectiveness analysis. Radiology 254(2):532–540
Stiell IG, Wells GA, Vandemheen K, Clement C, Lesiuk H, Laupacis A, McKnight RD, Verbeek R, Brison R, Cass D, Eisenhauer ME, Greenberg G, Worthington J (2001) The Canadian CT Head Rule for patients with minor head injury. Lancet 357(9266):1391–1396
Papa L, Stiell IG, Clement CM, Pawlowicz A, Wolfram A, Braga C, Draviam S, Wells GA (2012) Performance of the Canadian CT Head Rule and the New Orleans Criteria for predicting any traumatic intracranial injury on computed tomography in a United States Level I trauma center. Acad Emerg Med 19(1):2–10
Haydon NB (2013) Head injury: audit of a clinical guideline to justify head CT. J Med Imaging Radiat Oncol 57(2):161–168
Griffey RT, Sodickson A (2009) Cumulative radiation exposure and cancer risk estimates in emergency department patients undergoing repeat or multiple CT. AJR Am J Roentgenol 192(4):887–892
Haydel MJ, Preston CA, Mills TJ, Luber S, Blaudeau E, DeBlieux PM (2000) Indications for computed tomography in patients with minor head injury. N Engl J Med 343(2):100–105
Sadegh R, Karimialavijeh E, Shirani F, Payandemehr P, Bahramimotlagh H, Ramezani M (2016) Head CT scan in Iranian minor head injury patients: evaluating current decision rules. Emerg Radiol 23(1):9–16
National Clinical Guideline Centre (UK) (2014) Head injury: triage, assessment, investigation and early management of head injury in children, young people and adults. National Institute for Health and Clinical Excellence: Guidance
Jagoda AS, Bazarian JJ, Bruns JJ Jr, Cantrill SV, Gean AD, Howard PK, Ghajar J, Riggio S, Wright DW, Wears RL, Bakshy A, Burgess P, Wald MM, Whitson RR (2008) American College of Emergency Physicians; Centers for Disease Control and Prevention Clinical policy: neuroimaging and decision making in adult mild traumatic brain injury in the acute setting. Ann Emerg Med 52(6):714–748
Servadei F, Teasdale G, Merry G (2001) Neurotraumatology Committee of the World Federation of Neurosurgical Societies. Defining acute mild head injury in adults: a proposal based on prognostic factors, diagnosis, and management. J Neurotrauma 18(7):657–664
Mower WR, Hoffman JR, Herbert M, Wolfson AB, Pollack CV Jr, Zucker MI, NEXUS II Investigators (2002) National Emergency X-Radiography Utilization Study. Developing a clinical decision instrument to rule out intracranial injuries in patients with minor head trauma: methodology of the NEXUS II investigation. Ann Emerg Med 40(5):505–514
Harnan SE, Pickering A, Pandor A, Goodacre SW (2011) Clinical decision rules for adults with minor head injury: a systematic review. J Trauma 71(1):245–251
Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, Khorasani R (2009) Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 251(1):175–184
Fabbri A, Servadei F, Marchesini G, Dente M, Iervese T, Spada M, Vandelli A (2005) Clinical performance of NICE recommendations versus NCWFNS proposal in patients with mild head injury. J Neurotrauma 22(12):1419–1427
Melnick ER, Shafer K, Rodulfo N, Shi J, Hess EP, Wears RL, Qureshi RA, Post LA (2015) Understanding overuse of computed tomography for minor head injury in the emergency department: a triangulated qualitative study. Acad Emerg Med 22(12):1474–1483
Schueller G, Scaglione M, Linsenmaier U, Schueller-Weidekamm C, Andreoli C, De Vargas MM, Gualdi G (2015) The key role of the radiologist in the management of polytrauma patients: indications for MDCT imaging in emergency radiology. Radiol Med 120(7):641–654
Jame SZB, Majdzadeh R, Sari AA, Rashidian A, Arab M, Rahmani H (2014) Indications and overuse of computed tomography in minor head trauma. Iran Red Crescent Med J 16(5):e13067
Klang E, Beytelman A, Greenberg D, Or J, Guranda L, Konen E, Zimlichman E (2017) Overuse of Head CT examinations for the investigation of minor head trauma: analysis of contributing factors. J Am Coll Radiol 14(2):171–176
Melnick ER, Szlezak CM, Bentley SK, Dziura JD, Kotlyar S, Post LA (2012) CT overuse for mild traumatic brain injury. Jt Comm J Qual Patient Saf 38(11):483–489
Natale JE, Joseph JG, Rogers AJ, Mahajan P, Cooper A, Wisner DH, Miskin ML, Hoyle JD Jr, Atabaki SM, Dayan PS, Holmes JF, Kuppermann N, PECARN (Pediatric Emergency Care Applied Research Network) (2012) Cranial computed tomography use among children with minor blunt head trauma: association with race/ethnicity. Arch Pediatr Adolesc Med 166(8):732–737
Fortin EM, Fisher J, Qiu S, Babcock CI (2016) Privately insured medical patients are more likely to have a head CT. Emerg Radiol 23(6):597–601
Lee J, Evans CS, Singh N, Kirschner J, Runde D, Newman D, Wiener D, Quaas J, Shah K (2013) Head computed tomography utilization and intracranial hemorrhage rates. Emerg Radiol 20(3):219–223
Borczuk P (1995) Predictors of intracranial injury in patients with mild head trauma. Ann Emerg Med 25(6):731–736
Gómez PA, Lobato RD, Ortega JM, De La Cruz J (1996) Mild head injury: differences in prognosis among patients with a Glasgow Coma Scale score of 13–15 and analysis of factors associated with abnormal CT findings. Br J Neurosurg 10(5):453–460
Bouida W, Marghli S, Souissi S, Ksibi H, Methammem M, Haguiga H, Khedher S, Boubaker H, Beltaief K, Grissa MH, Trimech MN, Kerkeni W, Chebili N, Halila I, Rejeb I, Boukef R, Rekik N, Bouhaja B, Letaief M, Nouira S (2013) Prediction value of the Canadian CT Head Rule and the New Orleans criteria for positive head CT scan and acute neurosurgical procedures in minor head trauma: a multicenter external validation study. Ann Emerg Med 61(5):521–527
Wu SR, Shakibai S, McGahan JP, Richards JR (2006) Combined head and abdominal computed tomography for blunt trauma: which patients with minor head trauma benefit most? Emerg Radiol 13(2):61–67
Khaji A, Eftekhar B, Karbakhsh M, Ardalan KM (2006) The use of head CT scanning in mild head injury. Neurosciences (Riyadh) 11(4):248–251
af Geijerstam JL, Britton M (2003) Mild head injury—mortality and complication rate: meta-analysis of findings in a systematic literature review. Neurochirurgica (Wien) 145(10):843–850 (discussion 850)
Brenner DJ, Elliston CD (2004) Estimated radiation risks potentially associated with full-body CT screening. Radiology 232(3):735–738
Salerno S, Marrale M, Geraci C, Caruso G, Re GL, Casto AL, Midiri M (2016) Cumulative doses analysis in young trauma patients: a single-centre experience. Radiol Med 121(2):144–152
Giannitto C, Campoleoni M, Maccagnoni S, Angileri AS, Grimaldi MC, Giannitto N, De Piano F, Ancona E, Biondetti PR, Esposito AA (2018) Unindicated multiphase CT scans in non-traumatic abdominal emergencies for women of reproductive age: a significant source of unnecessary exposure. Radiol Med 123(3):185–190
Vrijheid M, Cardis E, Ashmore P, Auvinen A, Bae JM, Engels H, Gilbert E, Gulis G, Habib R, Howe G, Kurtinaitis J, Malker H, Muirhead C, Richardson D, Rodriguez-Artalejo F, Rogel A, Schubauer-Berigan M, Tardy H, Telle-Lamberton M, Usel M, Veress K (2007) Mortality from diseases other than cancer following low doses of ionizing radiation: results from the 15-Country Study of nuclear industry workers. Int J Epidemiol 36(5):1126–1135
Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, Howe G, Kaldor J, Muirhead CR, Schubauer-Berigan M, Yoshimura T, Bermann F, Cowper G, Fix J, Hacker C, Heinmiller B, Marshall M, Thierry-Chef I, Utterback D, Ahn YO, Amoros E, Ashmore P, Auvinen A, Bae JM, Solano JB, Biau A, Combalot E, Deboodt P, Diez Sacristan A, Eklof M, Engels H, Engholm G, Gulis G, Habib R, Holan K, Hyvonen H, Kerekes A, Kurtinaitis J, Malker H, Martuzzi M, Mastauskas A, Monnet A, Moser M, Pearce MS, Richardson DB, Rodriguez-Artalejo F, Rogel A, Tardy H, Telle-Lamberton M, Turai I, Usel M, Veress K (2005) Risk of cancer after low doses of ionising radiation: retrospective cohort study in 15 countries. BMJ 331(7508):77
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Institutional review board approval was granted for this retrospective study with a waiver of the requirement to obtain written informed consent from each patient.
Rights and permissions
About this article
Cite this article
Cellina, M., Panzeri, M., Floridi, C. et al. Overuse of computed tomography for minor head injury in young patients: an analysis of promoting factors. Radiol med 123, 507–514 (2018). https://doi.org/10.1007/s11547-018-0871-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0871-x