Abstract
Background
Fluid samples obtained from an affected joint still play a central role in the diagnosis of periprosthetic joint infection (PJI). It is the only preoperative test able to discover the causative microbiological agent. In the hip, fluid aspiration can be performed through fluoroscopy, ultrasound, or, less commonly, computed tomography. However, there is still a lack of consensus on which method is preferable in terms of efficacy and costbenefit.
Purposes
We, therefore, asked whether (1) the benefits in terms of sensitivity and specificity and (2) the costs were comparable between fluoroscopy- and ultrasound-guided joint aspirations in a suspicious of hip PJI.
Methods
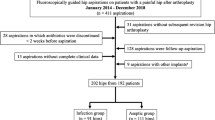
Between 2013 and 2016, 52 hip aspirations were performed on 49 patients with clinical, radiological, or serological suspicion of PJI, waiting for a revision surgery. The patients were divided in two groups: fluoroscopy- (n = 26) vs ultrasound-guided hip aspiration group (n = 26). These groups were also divided in control and infected patients. The criteria of MusculoSkeletal Infection Society (MSIS) were used, as gold standard, to define PJI.
Results
(1) Ultrasound-guided aspiration revealed valid sensitivity (89% vs 60%) and specificity (94% vs 81%) in comparison with fluoroscopic-guided aspiration. (2) The cost analysis was also in favor of ultrasound-guided aspiration (125.30€) than fluoroscopic-guided aspiration (343.58€).
Conclusions
We concluded that ultrasound-guided hip aspiration could represent a valid, safe, and less expensive diagnostic alternative to fluoroscopic-guided aspiration in hip PJI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Periprosthetic joint infection (PJI) is a devastating complication of hip arthroplasty, mostly requiring revision surgery. The diagnosis is often a challenge for orthopaedic surgeons. The MusculoSkeletal Infection Society (MSIS) recently developed a definition for PJI based on different criteria [1].
In this setting, the role of hip aspiration is of paramount importance for the management of PJI. Furthermore, it is the only preoperative test that can bring to the identification of the causative pathogen defining its antibiotic sensitivity. Hip aspiration can be performed under fluoroscopy (F) [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23], ultrasound (US) [24,25,26], or, less commonly, computed-tomography (CT) guidance [27]. Fluoroscopy-guided hip aspiration is the most common and described procedure worldwide; nevertheless, ultrasound aspiration is gaining popularity, especially for patient safety, because of the absence of X-rays and iodinated contrast agents. However, there is still a lack of consensus on which method is preferable in terms of diagnostic efficacy and risk–benefit for patients.
The main purpose of this retrospective study was to compare the diagnostic characteristics (sensitivity and specificity) between fluoroscopy and ultrasound-guided hip aspirations in a suspicious of PJI. Because of this primary objective, we compared the results of these preoperative hip aspirations with the results of cultures from multiple intraoperative tissue samples obtained during revision surgery, together with all the other MSIS criteria, to evaluate the accuracy of these two radiological techniques. The costs and pros/cons of these two procedures were also analyzed and discussed.
Methods
A retrospective cohort study comparing two different aspiration techniques for PJI diagnosis was performed in collaboration between Hip and Radiology Departments at our institution.
Patients who underwent hip aspiration between January 2013 and August 2016 before total hip arthroplasty revision (rTHA) were studied. The inclusion criteria were defined as:
-
clinical, radiological, or serological suspicion of PJI;
-
antibiotics suspension at least 3 weeks before hip aspiration and revision surgery;
-
revision surgery after hip aspiration;
-
informed consent for hip aspiration and revision surgery.
All procedures followed were in accordance with the 1975 Declaration of Helsinki, as revised in 2000 and 2008. The study was approved by the local ethics committee. Details that might disclose the identity of the subjects under the study were omitted, in accordance with HIPAA.
Fluoroscopy was mostly performed until 2015; then, due to different management and policy of health resources at our institutions, ultrasound has been especially used.
The patients were so divided in two groups on the basis of the used radiological technique: (1) fluoroscopy- vs (2) ultrasound-guided hip aspiration. Each patient of the fluoroscopy or ultrasound group was defined infected (PJI) or control (non-infected) using the MSIS criteria selected as the gold standard for PJI diagnosis. Based on these criteria, a patient was defined as affected by PJI when at least one of the major criteria or four of the minor criteria were satisfied [1].
Major criteria:
-
1.
A sinus tract communicating with the prosthesis before revision; or
-
2.
A pathogen isolated by culture from at least two separate tissues or fluid samples obtained from the affected prosthetic joint at the time of revision surgery.
Minor criteria:
-
a.
Elevated serum erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) concentration before revision,
-
b.
Elevated synovial leukocyte count,
-
c.
Elevated synovial neutrophil percentage (PMN%),
-
d.
Presence of purulence in the affected joint,
-
e.
Isolation of a microorganism in one culture of periprosthetic tissue or fluid, or
-
f.
Greater than five neutrophils per high-power field in five high-power fields observed from histologic analysis of periprosthetic tissue at 400× magnification.
A patient who fulfilled the criteria was considered infected (PJI group). A patient who did not fulfil the previous criteria was considered as non-infected (control group). Therefore, matching the aspiration technique and the presence or absence of infection, each procedural group was subdivided in two subgroups: fluoroscopy-PJI group, fluoroscopy-control group, ultrasound-PJI group, and ultrasound-control group.
The preoperative aspiration of each patient was then compared to the definitive intraoperative multiple cultures (one of the two major criteria) and all the other MSIS criteria to determine the rate of true positive, false positive, true negative, and false negative of both radiological groups (Table 1). The patient was so considered true positive when multiple intraoperative cultures or other MSIS criteria were satisfied and the preoperative aspiration was positive. A false positive was considered when multiple intraoperative cultures or the other MSIS criteria were finally negative, but the preoperative aspiration was positive. A true negative patient had multiple intraoperative cultures negative and the other MSIS criteria unsatisfied for an infection and the preoperative aspiration was negative. The patient was described as false negative if bacterial growth was not reported after preoperative aspiration, but then, the multiple intraoperative cultures or the other MSIS criteria reported the presence of infection.
Fluoroscopic aspiration
The patient was admitted for a day-hospital procedure for local regulatory laws. The procedure was carried out by two experienced orthopaedic surgeons with at least 15 years expertise in hip surgery. In the operating room, the patient was place supine on a fluoroscopic table. The sterile operative field was limited to few centimeters around the hypothetical entry point above the greater trochanter. Once the operative field was ready, under a C-arm fluoroscopy view, a 17-gauge spinal needle was inserted through the standard antero-lateral (AL) arthroscopic portal into the hip joint.
Fluoroscopy was used intermittently during the procedure to guarantee the correct insertion and advancement of the needle (Fig. 1). A loss of resistance was appreciated when the spinal needle penetrated the joint capsule. Excessive resistance suggested that the needle was about to penetrate through the labrum rather than the capsule. Once the fluoroscopic position of the needle was considered satisfactory, the inserter was removed from the needle and then the vacuum phenomenon caused by the negative intracapsular pressure was appreciated, indicating the intra-articular position.
Because of its bacteriostatic effect, injection of contrast media (arthrogram) was not performed to confirm the intra-articular position of the needle [28]. Routinely, the aspirated fluid was inoculated into two culture blood bottles and two swabs (containing aerobic or anaerobic liquid enrichment medium) in sterile conditions.
Ultrasound aspiration
The ultrasound investigation was performed by radiologists with at least 5 years of musculoskeletal experience, using a 5-MHz convex ultrasound probe with puncture guide. Under sterile conditions, a 17-gauge needle was advanced into hip joint at the level of the head–neck prosthesis junction, and then, fluid was aspirated with continuous control on the screen (Fig. 2).
On the left, ultrasound image shows periprosthetic fluid collection (white asterisk). The collection extends from superficial (S) to deep (D) soft tissues showing multiloculated aspect with thick synovial walls (yellow arrow) and septa (white arrow). On the right, ultrasound-guided procedure of hip aspiration. The needle (arrows) is advanced with an in-plane approach up to reach a small fluid collection (white asterisk) surrounding the hyper-echoic surface of hip prosthesis (arrowhead). F femur, A acetabulum
Local anesthesia was not performed prior to aspiration, because of its possible bactericidal effect [29]. All samples (two blood bottles and two culture swabs) were sent to laboratory for culture.
Revision surgery
During revision surgery, three-to-five samples were obtained from the hip joint and nearby tissues and then transferred to microbiology and cultured for a minimum of 15 days. Standard microbiological techniques were performed to identify the possible pathogen and determine antibiogram, screening for aerobic, anaerobic, acid-fast bacillus, and fungal microorganisms.
Costs
Any surgical procedure comprises direct costs, measurable, such as operating room and surgical performance, and indirect costs, not so easily quantifiable, such as social costs, loss of work, or salary [30]. This retrospective study considers only direct costs of fluoroscopy- and ultrasound-guided hip aspirations. The costs of hip aspiration were calculated by summing the costs of operating room, performance, and microbiological culture.
The cost of the operating room was calculated per hour of procedure (€1000/h) (Region of Lombardy, Italy), considering the start of the procedure as the moment of making the first insertion of the needle and the end as when the procedure was completed. The ultrasound performance in the radiology department comprised the investigation of the joint (€36.55/patient) and hip aspiration (€28.50/patient).
The microbiological culture costs, which were the same for both procedures, account for two stabs (€13.35 × 2/patient), two blood bottles (€13.35 × 2/patient), culture procedure (€6.85/patient), and only in case of microbiological growth, microorganism identification (€13.90/patient), and antibiogram (€7.55/patient).
The costs of the fluoroscopic procedure, requiring hospital admission, were on charge of the Italian National Health Service (Servizio Sanitario Nazionale—SSN). The costs of the ambulatorial ultrasound procedure were on charge of both the SSN and the patient, with the payment of a co-pay fee (ticket), except for those who were entitled to exemptions.
Statistical analysis
Continuous variables were expressed as mean and standard deviation (SD). Demographical and clinical data were analyzed using t test independent for continuous variables. The level of statistical significance was fixed to 5% (p < 0.05) to reject the null hypothesis. The sensitivity and specificity along with the exact confidence intervals (CIs) were calculated. Fisher’s exact test was used to compare sensitivities and specificities of the two diagnostic procedures [31]. Calculations were performed using analysis computer software (Excel, Microsoft) and interactive statistical pages (http://www.statpages.org for exact tests and 95% CI). The ROC plot was used to graphically compare the two tests under investigation according to the considerations of Biggerstaff [32]. Specifically, each test is represented according to its sensitivity and 1-specificity and connected to the point (0,0) and (1,1) through two lines. The slope of the two lines represents the likelihood ratio positive and negative of the test.
Results
Fifty-two hip aspirations were performed on forty-nine patients (23 men and 26 women). Twenty-six were performed under fluoroscopy guidance and 26 under ultrasound guidance. The average age in the F group was 66.7 ± 15.4 years, while that in the ultrasound group was 66.3 ± 9.2 years. The average time from hip aspiration to revision surgery was 126.5 ± 235.3 days in the fluoroscopy group and 118.5 ± 69.1 in the ultrasound group. There were no statistically significant differences when comparing the mean age of patients (p = 0.93) and the mean wait time for revision surgery (p = 0.20) of the two groups.
In the fluoroscopy group, ten patients (38.5%) were considered infected (fluoroscopy-PJI group) (Table 2). After the revision surgery, of these 10 infected hips, 6 patients (60%) had positive preoperative hip aspiration (true positive) and 4 patients (40%) had negative preoperative hip aspiration (false negative). In the fluoroscopy-PJI group, seven hips presented MSIS major criteria (sinus tract or positive multiple intraoperative culture) and three hips multiple minor criteria. In the fluoroscopy-control group, three positive hip aspirations (18.8%) were considered false positive, because the MSIS was not satisfied even after revision surgery.
The sensitivity of hip aspiration in the fluoroscopy group was 60% (95% CI 26–88%). The specificity was 81% (95% CI 54–96%). Hip aspiration under fluoroscopy guidance required an average time of 17 ± 6.7 min.
In the ultrasound group, nine patients (34.6%) were diagnosed septic after MSIS criteria (ultrasound-PJI group) (Table 3). Preoperative hip aspirations were positive in 8 of these 9 infected patients (89%) (true positive). One preoperative hip aspiration (11%) was negative (false negative) in this septic-ultrasound group. All these nine infected hips had multiple intraoperative positive samples during revision surgery (MSIS major criteria). In the ultrasound-control group, only one false-positive preoperative aspiration (5.9%) was reported.
Pathogen identified pre and intraoperatively at revision surgery is shown in Tables 4 and 5.
In the ultrasound group, the sensitivity of preoperative hip aspiration was 89% (95% CI 51–100%), while the specificity was 94% (95% CI 71–100%). The diagnostic performances of the two tests are reported in Fig. 3. There was no evidence of statistically significant difference comparing sensitivities or specificities of the two techniques (sensitivities: p = 0.73; specificities: p = 0.80).
The costs of the fluoroscopy-guided procedure was calculated as follows: 17 min of the average operating theater time at an hourly cost of €1000 (€283.33) + cost of microbiological cultures (€60.25) = €343.58. The costs of the ultrasound-guided procedure was calculated as follows: radiological performance (€65.05) + cost of microbiological culture (€60.25) = €125.30. In the PJI groups, all these costs increased of €21.45 for microbiological identification and sensitivity.
Discussion
Defining preoperatively, the microbiological pathogen responsible for PJI is crucial. The accuracy of different aspiration techniques to achieve this step has been reported in the literature. Fluoroscopy-guided aspiration with or without injection of iodinated contrast (hip arthrography) is the most commonly technique published in the literature (Table 6) [2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23]. It appears to be an effective and reproducible procedure, but there are risks derived from doses of radiations and the potential adverse reactions against iodinated contrast.
In this retrospective study, ultrasound-guided aspiration showed good and superior outcomes in comparison with fluoroscopy-guided procedure evaluating sensitivity (89% vs 60%) and specificity (94% vs 81.3%), even if the difference was not statistically significant.
In our study, a low sensitivity was found for fluoroscopy. In fact, four false-negative results (40%) were found. This rate of false-negative outcomes could be explained by the incapability of fluoroscopy to drive the needle toward a fluid collection, collecting potentially less fluid to cultivate than US. Scarce fluid for culture and consequentially low concentrations of the microorganisms has been described as potential causes of false-negative results [33]. The main limitation of this study is the small sample size that does not permit the detection of a statistical difference in terms of sensibility and specificity, even if the main purpose of the study was to show US as valid as fluoroscopy in detecting PJI. Larger randomized controlled clinical trials are needed to confirm and validate these clinical results and to draw the future role of the radiologist and ultrasound in the preoperative management of PJI.
A first question dealing with effectiveness of a diagnostic procedure in PJI is how this procedure may resemble fluoroscopy-guided aspiration results. Ultrasound-guided hip aspiration is an emerging technique showing the advantage of avoiding X-rays and contrast exposure. US has been reported an excellent modality to visualize the soft tissues surrounding the hip (greater trochanteric bursa, iliopsoas tendon/bursa, gluteal tendons, and iliotibial band), cystic or solid soft-tissue masses [34], and extra-articular fluid collections communicating with the joint: these structures, undetectable with fluoroscopy, can be possible locations of pathologies after hip arthroplasty and may be passible of aspiration [35, 36]. Colour and power Doppler imaging has been described as potential tools in differentiating synovitis from hip effusion [37]. US provide theoretical advantages also considering needle insertion, which can be more precise and safer, monitoring continuously on the screen the tip of the needle, to avoid accurately heterotopic ossifications or septic extra-articular collections, with the potential risk of introducing infective microorganisms into a sterile joint [38].
There are few studies about the accuracy of ultrasound-guided aspiration for hip PJI diagnosis [24,25,26]. Results seem comparable to the fluoroscopy procedure (Table 7). However, Eisler et al. [25] do not suggest the use of preoperative US: the fluid cultures showed high specificity but were of limited clinical value because of poor sensitivity. Battaglia et al. [26] compared the clinical outcomes of ultrasound vs fluoroscopy hip aspiration, reporting similar results to our study, but different statistical comparison was performed.
The cost analysis of our study showed an average difference of €218.28. Fluoroscopy-guided hip aspiration costs more than double compared to the ultrasound-guided one.
This is the first study, to our knowledge, that included a full statistical analysis, focusing on the accuracy, pros/cons, and costs of the two procedures, with updated criteria (MSIS) as gold standard to evaluate the validity of each hip aspiration technique for PJI detection. Usually, in the literature, the intraoperative culture results obtained during revision surgery were considered as the gold standard for the attestation of PJI: this methodology does not appear completely reliable to differentiate PJI from aseptic failure in our case series and in literature, due to possibility to underestimate the presence of PJI. We had 4 patients in 19 infected (21%) that presented intraoperative negative cultures: with the use of other major (sinus tract) or minor criteria, we were able to differentiate the septic failure of the prosthesis and better investigate the accuracy of the radiological techniques in managing PJI.
Conclusions
Preoperative hip aspiration is a useful diagnostic tool for detection of PJI. There is still debate in the literature on which technique of aspiration is preferable, based on accuracy, costs, and pros/cons. In our study, ultrasound-guided aspirations showed good outcomes compared to fluoroscopy, but at lower costs.
References
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469(11):2992–2994
O’Neill DA, Harris WH (1984) Failed total hip replacement: assessment by plain radiographs, arthrograms and aspiration of the hip joint. J Bone Jt Surg 66A:540
Barrack RL, Harris WH (1993) The value of aspiration of the hip joint before revision total hip arthroplasty. J Bone Jt Surg 75-A:66
Fehring TK, Cohen B (1996) Aspiration as a guide to sepsis in revision total hip arthroplasty. J Arthroplasty 11:543
Gould ES, Potter HG, Bober SE (1990) Role of routine percutaneous hip aspirations before prosthesis revision. Skeletal Radiol 19:427
Lachiewicz PF, Rogers GD, Thomason HC (1996) Aspiration of the hip joint before revision total hip arthroplasty. Clinical and laboratory factors influencing attainment of a positive culture. J Bone Joint Surg 78-A:749
Spangehl MJ, Masri BA, O’Connell JX et al (1999) Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of 200 and two revision total hip arthroplasties. J Bone Joint Surg 81-A:672
Mulcahy DM, Fenelon GC, McInerney DP (1996) Aspiration arthrography of the hip joint its uses and limitations in revision hip surgery. J Arthroplasty 11(1):64–68
Ali F, Wilkinson JM, Cooper JR, Kerry RM, Hamer AJ, Norman P, Stockley I (2006) Accuracy of joint aspiration for the preoperative diagnosis of infection in total hip arthroplasty. J Arthroplasty 21(2):221–226
Levitsky KA, Hozack WJ, Baldersson RA et al (1991) Evaluation of the painful prosthetic joint: relative value of bone scan, sedimentation rate and joint aspiration. J Arthroplasty 6:237
Pons M, Angles F, Sanchez C et al (1999) Infected total hiparthroplasty—the value of intra-operative histology. Int Orthop 23:34
Williams JL, Norman P, Stockley I (2004) The value of hip aspiration versus tissue biopsy in diagnosing infection before exchange hip arthroplasty surgery. J Arthroplasty 19:582–586
Tigges S, Stiles RG, Meli RJ, Robertson JR (1993) Hip aspiration: a costeffective and accurate method of evaluating the potentially infected hip prosthesis. Radiology 189:485–488
Taylor T, Beggs I (1995) Fine needle aspiration in infected hip replacements. Clin Radiol 50:149–152
Kraemer WJ, Saplys R, Waddell JP, Morton J (1993) Bone scan, gallium scan, and hip aspiration in the diagnosis of infected total hip arthroplasty. J Arthroplasty 8:611–615
Jonhson JA, Christie MJ, Sandler MP, Parks PF, Homra L, Kaye JJ (1988) Detection of occult infection following total joint arthroplasty using sequential Technetium-99m HDP bone scintigraphy and Indium-111 WBC imaging. J Nucl Med 29:1347–1353
Glithero PR, Grigoris P, Harding LK, Hesslewood SR, McMinn DJW (1993) White cell scans and infected joint replacements. J Bone Jt Surg Br 75:371–374
Roberts P, Walters AJ, McMinn DJW (1992) Diagnosis infection in hip replacements. J Bone Jt Surg Br 74:265–269
Lieberman JR, Huo MH, Schneider R, Salvati EA, Rodi S (1993) Evaluation of painful hip arthroplasties. J Bone Jt Surg Br 75:475–478
Itasaka T, Kawai A, Sato T, Mitani S, Inoue H (2001) Diagnosis of infection after total hip arthroplasty. J Orthop Sci 6:320–326
Cheung A, Lachiewicz PF, Renner JB (1997) The role of aspiration and contrast enhanced arthrography in evaluating the uncemented hip arthroplasty. Am J Roentgenol 168:1305–1309
Somme D, Ziza JM, Desplaces N, Chicheportiche V, Chazerain P, Leonard P, Lhotellier L, Jacquenod P, Mamoudy P (2003) Contribution of routine joint aspiration to the diagnosis of infection before hip revision surgery. Jt Bone Spine 70(6):489–495
Cross MC, Kransdorf MJ, Chivers FS, Lorans R, Roberts CC, Schwartz AJ, Beauchamp CP (2014) Utility of percutaneous joint aspiration and synovial biopsy in identifying culture-positive infected hip arthroplasty. Skeletal Radiol 43(2):165–168
van Holsbeeck MT, Eyler WR, Sherman LS, Lombardi TJ, Mezger E, Verner JJ, Schurman JR, Jonsson K (1994) Detection of infection in loosened hip prostheses: efficacy of sonography. AJR Am J Roentgenol 163(2):381–384
Eisler T, Svensson O, Engström CF, Reinholt FP, Lundberg C, Wejkner B, Schmalholz A, Elmstedt E (2001) Ultrasound for diagnosis of infection in revision total hip arthroplasty. J Arthroplasty 16(8):1010–1017
Battaglia M, Vannini F, Guaraldi F, Rossi G, Biondi F, Sudanese A (2011) Validity of preoperative ultrasound-guided aspiration in the revision of hip prosthesis. Ultrasound Med Biol 37(12):1977–1983
Tomas X, Bori G, Garcia S, Garcia-Diez AI, Pomes J, Soriano A, Ríos J, Almela M, Mensa J, Gallart X, Martinez JC, Riba J (2011) Accuracy of CT-guided joint aspiration in patients with suspected infection status post-total hip arthroplasty. Skeletal Radiol 40(1):57–64
Blake MP, Kalasz SJ (1995) The effect of X-ray contrast media on bacterial growth. Australas Radiol 39:10
Phillips WC, Kattapuram SV (1983) Efficacy of preoperative hip aspiration performed in the radiology department. Clin Orthop 179:141
Angevine PD, Berven S (2014) Health economic studies: an introduction to cost–benefit, cost-effectiveness, and cost-utility analyses. Spine (Phila Pa 1976) 39((22 Suppl 1)):S9–15
Zhou X, Obuchowski NA, McClish DK. Statistical methods in diagnostic medicine, 2nd edn. Wiley, New York
Biggerstaff BJ (2000) Comparing diagnostic tests: a simple graphic using likelihood ratios. Stat Med 19(5):649–663
Müller M, Morawietz L, Hasart O, Strube P, Perka C, Tohtz S (2008) Diagnosis of periprosthetic infection following total hip arthroplasty—evaluation of the diagnostic values of pre- and intraoperative parameters and the associated strategy to preoperatively select patients with a high probability of joint infection. J Orthopaedic Surg Res 3:3
Randelli F, Banci L, Favilla S, Maglione D, Aliprandi A (2013) Radiographically undetectable periprosthetic osteolysis with ASR implants: the implication of blood metal ions. J Arthroplasty 28(8):1259–1264
Messina C, Banfi G, Aliprandi A, Mauri G, Secchi F, Sardanelli F, Sconfienza LM (2016) Ultrasound guidance to perform intra-articular injection of gadolinium-based contrast material for magnetic resonance arthrography as an alternative to fluoroscopy: the time is now. Eur Radiol 26(5):1221–1225
Sdao S, Orlandi D, Aliprandi A, Lacelli F, Sconfienza LM, Randelli F, Sardanelli F, Serafini G (2014) The role of ultrasonography in the assessment of peri-prosthetic hip complications. J Ultrasound 18(3):245–250
Weybright PN, Jacobson JA, Murry KH, Lin J, Fessell DP, Jamadar DA et al (2003) Limited effectiveness of sonography in revealing hip joint effusion: preliminary results in 21 adult patients with native and postoperative hips. AJR Am J Roentgenol 181:215–218
Long SS, Surrey D, Nazarian LN (2012) Common sonographic findings in the painful hip after hip arthroplasty. J Ultrasound Med 31:301–312
Acknowledgements
None.
Funding
The current study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors of this manuscript declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Investigation performed at Milan, Italy.
Rights and permissions
About this article
Cite this article
Randelli, F., Brioschi, M., Randelli, P. et al. Fluoroscopy- vs ultrasound-guided aspiration techniques in the management of periprosthetic joint infection: which is the best?. Radiol med 123, 28–35 (2018). https://doi.org/10.1007/s11547-017-0811-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-017-0811-1