Abstract
Background
Synovial hypertrophy, synovial effusions, and abnormalities in the subchondral bone play a key role in the pathogenesis of osteoarthritis (OA) and are associated with pain. Understanding and careful clinical assessment together with better imaging such as magnetic resonance imaging (MRI) of the knee may improve treatment strategies. The aim of this cross-sectional study was to investigate the associations between the structural findings on MRI (bone marrow lesions [BMLs], synovitis, cartilage defects, meniscal lesions), X-ray examination (Kellgren and Lawrence [K/L] grade), and psychological aspects with pain in patients with knee osteoarthritis (KOA).
Methods
In this study, patients with symptomatic KOA were included. Knee radiographs were acquired and scored according to the K/L score. MRI was performed with a 1.5 T whole-body scanner; the presence of the following alterations was collected: BMLs, infrapatellar fat pad (IFP) synovitis, condral defects, and meniscal tears. Knee pain was assessed with Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale. The Mental Component Summary Scale Score (MCS) of the Medical Outcomes Study Short-Form 36 Health Survey (SF-36) questionnaire was used to evaluate psychological impact.
Results
BMLs were detected in 57 (38.3%) subjects of 149 participants (aged 51–81 years, female 75.8%). Cartilage defects were found in 91.9% of patients, IFP synovitis in 37.5%, meniscal lesions in 34.9%. In multiple regression analyses, WOMAC knee pain was significantly associated with the volume of the BMLs (p = 0.0001), IFP synovitis (p = 0.0036), and SF-36 MCS (p = 0.0001), but not with K/L grades, meniscal lesion score, cartilage defect, sex, age, educational level, disease duration and BMI.
Conclusion
In symptomatic KOA patients, MRI features, such as larger BMLs, IFP synovitis, and high levels of psychological distress, are associated with greater knee pain. Confirmation of these findings in the prospective studies of KOA is needed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the most prevalent musculoskeletal complaint worldwide, affecting 7.5–40% of the population by the age of 65 years [1,2,3]. In Italy, the overall prevalence of symptomatic OA is estimated as 8.95%, and knee is the most frequent site involved, with a prevalence of 5.39% (95% CI 3.41–7.99) [4]. Individuals with knee OA (KOA) suffer progressive loss of function, displaying increasing dependency in walking, stair climbing and other lower extremity tasks [5,6,7,8], and risk of cardiovascular comorbidity [9].
Joint pain is usually the major complaint of symptomatic KOA which leads patients to seek medical attention. It is believed to be the result of a complex interaction between local tissue damage and inflammation, peripheral and central nervous system [10]. The pathology of OA involves multiple structures of the joint. The disease process includes progressive degradation of articular cartilage with concomitant changes in the bone underneath the cartilage, including development of marginal outgrowths (osteophytes), abnormal increase in density and thickness of bone (bony sclerosis), and alterations in trabecular bone structure and bone marrow lesions (BMLs). Soft tissues in and around the joint are also affected. These tissues include synovium, which may reveal modest inflammatory infiltrates; ligaments, which often become lax; menisci, which may present traumatic and degenerative lesions; and bridging muscles, which become weak [10].
Radiological assessment is widely used for the diagnosis of the structural severity of KOA, for outcome evaluation in epidemiological studies and in clinical trials of structure-modifying drugs [11]. However, in cross-sectional studies, radiological changes are not strongly related to the severity of knee joint pain or disability, while a weak correlation between changes in clinical parameters and changes in radiological signs had been demonstrated in longitudinal studies [11]. Furthermore, a major limitation of conventional radiology is the inability to detect early and subtle OA changes.
In this context, magnetic resonance imaging (MRI) is a more appropriate tool, and has the capability to visualize all the structures within the knee joint, including the soft tissues [12]. In the last years, a growing number of studies employed MRI to examine the correlations between structural findings and symptoms. In a large cohort study, synovial hypertrophy, synovial effusions, and abnormalities in the subchondral bone have been associated with knee pain [13]. Felson et al. reported that in persons with KOA, or at risk of KOA, a growth in the size of BMLs (seen on knee MRI) is related to the contemporary onset of knee pain [14]. Zhai et al. suggested that knee pain is independently associated with both full and non-full-thickness medial tibial chondral defects, BMLs, but not with radiographic KOA, expanding our understanding of knee pain in older adults [15]. Other MRI studies showed a connection between signal alterations in Hoffa’s fat pad (or infrapatellar fat pad [IFP]) and knee pain [16].
The aims of this cross-sectional study are to describe the associations between the structural findings on MRI (BMLs, IFP synovitis, cartilage defects, meniscal lesions), X-ray examination (Kellgren and Lawrence [K/L] grade) [17], and psychological aspects with pain in patients with KOA.
Methods
Study population
This is a cross-sectional study, realized over a 6-months period, including subjects referring to the Department of Rheumatology of the Polytechnic University of the Marche (Jesi, Ancona–Italy). The inclusion criteria were the following: an age ≥50 years; a diagnosis of KOA, according to the American College of Rheumatology criteria [18]: the presence of unilateral or bilateral knee pain >30 mm (knee discomfort on most days for at least one month in past 12 months) measured by the visual analog scale (VAS—0–100 mm); tibiofemoral OA on posterior–anterior weight-bearing semi-flexed knee radiographs (K/L grade ≥2); and a clinical examination confirming knee pain or discomfort referable to the knee joint [17]. Exclusion criteria were represented by: a history of a previous knee injury requiring non-weight-bearing treatment for >24 h or surgery (including arthroscopy); a history of any arthritis (such as chronic inflammatory arthritis, gout, and calcium pyrophosphate dihydrate deposition disease) diagnosed by a rheumatologist; and any contraindication to MRI (including claustrophobia).
For each patient, weight (kg) and height (m) were collected to determine the body mass index (BMI).
Knee selection
For each patient, one knee was identified. If both knees were eligible, the choice concerned the knee with a greater Western Ontario and McMaster Universities osteoarthritis index (WOMAC) pain subscale score [19]. If both knees had equivalent WOMAC pain subscale scores, the knee with a greater K/L grade was chosen. All patients were examined by the same rheumatologist.
Patient-reported outcome measures
The KOA symptoms and the impact on quality of life were assessed using the WOMAC scale and the Medical Outcomes Study SF-36 Health Survey (SF-36) [19]. The WOMAC is a disease-specific self-report multidimensional questionnaire assessing pain, stiffness, and physical functional disability, with a recall of 30 days. In this study, the Italian WOMAC was used in its VAS format, and all 24 items are rated by the subject on a 100 mm VAS ranging from 0 (indicating no pain, stiffness, or difficulty) to 100 (indicating extreme pain, stiffness, or difficulty). The range of the WOMAC scores is pain (0–500); stiffness (0–200), and function (0–1700) [19].
The SF-36 questionnaire is a generic instrument exploring general health. Scores are summarized into eight scales, each of which measures a health domain: physical functioning (PF), role function–physical aspect (RP), bodily pain (BP), general health perception (GH), vitality (VT), social functioning (SF), role function–emotional aspect (RE), and mental health (MH) [20]. For each of the SF-36 scales, necessary items are recoded so that higher values indicate better health, and then added. The summed scores are transformed to a 0–100 scale following its designated scoring algorithm, with higher scores reflecting better quality of life. The originators of the SF-36 have developed algorithms to calculate two psychometrically based summary measures: the Physical Component Summary Scale Score (PCS) and the Mental Component Summary Scale Score (MCS) [21]. For the purpose of this study, we used only SF-36 MCS scale score.
Radiological evaluation
All patients had X-rays of their more painful knee. The standing weight-bearing anterior–posterior (AP) view was used to assess the medial and the lateral tibial femoral joints and a skyline view of the knee to assess the patello-femoral joint. The X-rays were then assessed independently using a standardized scoring sheet and also be graded according to the K/L classification [17] by an experienced musculoskeletal radiologist (MC—with 15 years of experience in musculoskeletal imaging), and by an experienced rheumatologic reader (FS), blinded to the clinical and MRI results and to each other. Each final score was determined by consensus of the two readers who simultaneously assessed the radiograph, with immediate reference to the atlas. Intraobserver repeatability was assessed in a randomly selected sample of 46 radiographs (20 right and 26 left knees) with a weighted k statistics of 0.821.
MRI measurements
An MRI scan of the selected knee was performed in each patient, with a 1.5 T whole-body scanner (Philips Achieva 1.5 T), using a commercial transmit-receive extremity coil. The following image sequence was used, according to Peterfy et al. [22]: (1) axial T1-weighted spin echo (SE: 700/11 [TR msec/TE msec], 20 cm field of view [FOV], 5 mm/1 mm [slice thickness/interslice gap], 256 Å ~ 192 matrix, frequency encoding [FE] anterior–posterior, one excitation), (2) coronal T1-weighted SE (600/11, 16 cm FOV, 4 mm/0.5 mm, 256 Å ~ 192, FE superior–inferior, two excitations averaged), (3) sagittal T1-weighted SE (600/11, 16 cm FOV, 4 mm/0.5 mm, 256 Å ~ 192, FE anterior–posterior, two excitations averaged), (4) sagittal T2 weighted fast spin echo (FSE: 2500/90; echo train length (ETL) of eight; 14 cm FOV, 4 mm/0 mm, 256 Å ~ 192, FE superior–inferior, two excitation averaged) with fat suppression (frequency-selective presaturation), (5) and sagittal fat suppressed T1-weighted three-dimensional (3D) spoiled gradient echo (FS-3DSPGR: 58/6, 40° flip angle, 14 cm FOV, 256 Å ~ 128 matrix, 60 contiguous 2-mm slices covering all articular cartilage plates in the knee, FE, superior–inferior, one excitation, frequency-selective fat saturation, superior–inferior saturation bands to minimize pulsation artifacts). The MRI was scored for size of BMLs, synovitis (in IFP), cartilage morphology, and meniscal lesions [23]. Subchondral BMLs were assessed on the T2-weighted with fat suppression images and defined as discrete areas of increased signal adjacent to the subcortical bone at the lateral, medial femur and/or tibia [24]. Given that the results of previous studies have suggested that the size of BMLs is associated with pain [25], it has been focused on the volume of the lesion as our measure of BMLs. Images were reconstructed and analyzed by OsiriX MD 7, a DICOM software viewer (Osi-riX MD version 7, 64-bit format), on a Mac Mini (2.8 GHz Intel Core 2 Duo Desktop Computer, 16 GB random-access memory; Apple Computer, Cu-pertino, CA, USA) running Mac Operating System OSX 10.12.2. Prior to measuring BML size, image brightness and contrast were adjusted until normal bone signal appeared black and homogenous. The volumetric measurements of BMLs were based on segmentation method by a thresholding approach applied to the MR images (Fig. 1). The total segmented volume of BMLs was reported in cubic centimeters (cm3).
One radiologist (MC), and one rheumatologist (FS—trained in MRI interpretation), blinded to both the case/control status and clinical data, evaluated independently of each other the same MRIs. Inter-reader reliability for the volume of BML was excellent (ICC = 0.887; 95% CI 0.797–0.901). IFP synovitis may be considered as a surrogate for the identification of the activity of the inflammatory process or non-contrast-enhanced MRI. IFP synovitis was assessed in infrapatellar region on sagittal T2-weighted fat suppressed sequences and is defined by areas of hyperintensity within Hoffa’s fat pad. IFP synovitis was scored semiquantitatively and assessed for magnitude as follows: 0 = normal/no hyperintensity, 1 = mild, 2 = moderate, and 3 = severe [26] (Fig. 2). According to Zhai et al. [15], condral defects were evaluated on the T1-weighted MR images and scored at medial tibial, medial femoral, lateral tibial, lateral femoral, and patellar sites using a semiquantitative score from 0 to 4 (grade 0 = normal cartilage, grade 1 = focal blistering and intracartilaginous low-signal intensity area with an intact surface, grade 2 = irregularities on the surface or basal layer and loss of thickness <50%, grade 3 = deep ulceration with loss of thickness >50% (Fig. 3), and grade 4 = full-thickness chondral wear with exposure of subchondral bone. Meniscal lesions were graded in medial and lateral menisci separately based on a combined Whole-Organ Magnetic Resonance Imaging Score (WORMS) scoring system from grade 0 to 2 based on both the sagittal and coronal images [22]. Intraobserver repeatability for IFP synovitis, condral defects, meniscal lesions were assessed in a randomly selected sample of 52 patients (25 right and 27 left knees), with a weighted kappa statistics of 0.821, 0.792 and 0.842, respectively.
Sagittal T2-weighted fat suppressed MRI. Image shows a effusion at the suprapatellar region and mild signal alterations within Hoffa’s fat pad representing synovitis on non-enhanced MRI (grade 1); b focal thickness chondral loss at the medial tibial femoral joint without bone marrow lesion. This image also shows effusion with moderate signal alterations within Hoffa’s fat pad (grade 2); c marked signal alterations within Hoffa’s fat pad representing synovitis (grade 3). Partial thickness chondral loss with subcondral bone marrow lesion of the medial tibial plateau, popliteal cyst, prepatellar bursitis and deep infrapatellar bursitis can also be observed
Statistical analysis
Data were inserted into a Microsoft Excel database and analyzed using MedCalc® version 16.0 (MedCalc Software, Ostend, Belgium). Qualitative data were described as absolute frequencies and percentages. Quantitative data were described as mean, median and typical deviation (minimum and maximum). Chi-squared and Fisher’s test were used for qualitative data. Student’s t test and Mann–Whitney U test were used for comparing means. Intraclass correlation coefficients (ICC) were determined for volume of BMLs as a measure of inter-observer agreement. Inter-observer agreement for K/L radiographic evaluation (16), IFP synovitis, condral defects and meniscal lesions scores were calculated by weighted kappa statistics. A value of 0–0.20 was considered poor, 0.21–0.40 fair, 0.41–0.60 moderate, 0.61–0.80 good, and 0.81–1.00 excellent [27]. Associations among features were expressed as Spearman’s Rho. A multiple regression model was used to determine which variables were independently associated with knee pain (by WOMAC pain subscale). Age, gender, disease duration, educational level, BMI, and K/L grades were examined as potential confounders based on the significant associations with MRI findings. All statistical analyses were performed at p < 0.05.
Results
A total of 149 patients were recruited in this study; 113 of them were female (75.8%) with a mean age of 70.6 (8.7 SD) years, and 36 male with a mean age of 69.3 (9.9 SD) years. There were 89 right and 60 left knees. The mean duration of knee symptoms before KOA diagnosis was 11.1 years (range 1–18 years). The school education level was generally low: 48.6% had received only a primary school education, and just 10.8% had received a high school education or more. The majority of the patients (81.8%) were married and lived with the family, up to 56.5% of the patients were house-wives. BMI indicative of overweight was recorded for 59.7% of the patients examined. All subjects were affected by primary KOA with a radiological severity prevalently of grade 2 and grade 3 on K/L scale (respectively, 48.9 and 42.3%). Table 1 summarizes the demographic data as well as the characteristics of all subjects with pain scores, MRI and X-ray findings.
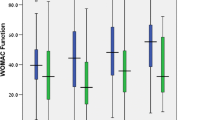
For the analyses of the present study, we employed only WOMAC pain score and SF-36 MCS scale score. However, in Table 2 the means, SDs, median values, and interquartile ranges for each dimension covered by WOMAC and SF-36 are detailed.
BMLs were found in 57 of 149 patients (38.3%). Cartilage defects were detected in 91.9% of patients, IFP synovitis in 37.5%, meniscal tears and/or extrusions in 34.9%.
Spearman’s correlation coefficient between WOMAC pain score was significantly correlated with both BMLs (ρ = 0.498; p < 0.0001) and IFP synovitis (ρ = 0.313; p < 0.0001). In addition, the WOMAC pain score was inversely correlated with psychological distress as measured by the SF-36 MCS scale score (ρ = −0.328; p = 0.0001).
In multiple regression analyses, WOMAC knee pain was significantly associated with higher volume BMLs (p = 0.0001), IFP synovitis (p = 0.0036), and SF-36 MCS (p = 0.0001), but not with K/L grading, meniscal lesion score, cartilage defect, sex, age, educational level, disease duration and BMI (Table 3).
Discussion
The pain of OA has multifaceted etiologies, involving mechanisms within and outside the joint. Nociceptive and neuropathic mechanisms as well as abnormal excitability pathways of the peripheral and central nervous system drive the OA pain [10]. Subchondral microfractures, bone stretching with elevation of periosteum due to osteophyte growth, bone remodeling and repair, BMLs, and bone angina caused by decreased blood flow and elevated intraosseous pressure are believed as bone-related causes of pain. Central factors can deeply modulate the pain perception setting the “gain” in a chronic disease such as KOA. When a peripheral input is persistent, it is processed against a background of central factors that can enhance or diminish the experience of pain [28]. As a complex phenomenon with a strong subjective component, pain is not only influenced by the nature of the underlying disease, but also by personal predisposition (biologic and psychological), as well as by environmental and psychosocial factors [10].
Radiography is relatively insensitive in detecting the earliest OA changes, and the majority of symptomatic knees with normal X-ray (i.e., K/L grade 0) have some alterations detectable on MRI [13].
In our cross-sectional cohort, in order of frequency the main findings were represented by cartilage damage (91.9%), BMLs (38.3%), IFP synovitis (37.5%), and meniscal lesions (34.9%). Interestingly, knee pain was significantly associated with larger BMLs, IFP synovitis, and SF-36 MCS, but not with K/L grades, meniscal lesions, cartilage defects, sex, age, educational level, disease duration, or BMI. MRI lesions have been evaluated recently by Sharma et al. in a cohort of 849 participants at increased risk for OA but with K/L grade 0 in both knees [29]. Cartilage defects were found by MRI in 76% of patients, BMLs in 61%, meniscal tears in 21%, and meniscal extrusions in 14%. In this work, cartilage damage, BMLs and meniscal extrusion correlated with prevalent and frequent symptoms at the baseline. BMLs seem to play an integral if not pivotal role in the symptoms that derive from KOA, and MRI is the only technique to visualize bone marrow edema [25]. Histopathological findings showed that BMLs pattern correlates with bone infarction or necrosis, bone fibrosis necrosis and abnormalities of trabecular bone [30]. In our community-based adult population with symptomatic KOA, BMLs were highly prevalent. Felson et al. first reported that BMLs were found in 77.5 and 30% of OA subjects with and without knee pain, respectively, and that large lesions were present almost exclusively in those with knee pain [25]. Other experiences about BMLs have been performed mostly in subjects with OA, with reported prevalences ranging from 66 to 91.1% in subjects with symptomatic KOA [24, 31]. Other reports of the prevalence of BMLs in adults without KOA have ranged from 14 to 52% of asymptomatic subjects [32, 33]. Differences in the prevalence of BMLs between our study and previous works are more likely to ascribe partly at the differences of the study population. Several studies in KOA have confirmed the strong correlation between bone marrow edema and pain [14, 25].
However, a final verdict on the issue cannot be derived since many papers have not documented a relationship between bone marrow edema and pain [34–36].
Different pathologic changes detectable in MRI, such as bone marrow lesions [25], subarticular bone attrition [26], synovitis, and effusion, have been related to knee pain. Additional bone-related causes of pain include periostitis associated with osteophyte formation [37], subchondral microfractures [38, 39], and bone angina due to decreased blood flow and elevated intraosseous pressure [30]. One likely source that remains understudied is that of intraosseous hypertension [31].
The volume of BMLs was calculated by a semiautomatic image processing (OsiriX). Compared to manual quantification, threshold-based segmentation of BMLs shows higher intra- and inter-observer reliability [40]. Several other studies reported the quantitative measurement of BMLs using manual segmentation. Schmid et al. described a slice-by-slice manual segmentation of the BMLs [41]. In an attempt to minimize the observer-dependent nature of the BML volume quantification process, Mayerhoefer et al. used a computer-assisted model to automatically calculate bone marrow volume at the knee applying a thresholding technique [42]. Roemer et al. [43] recently employed a volumetric measurement of BMLs using a modified version of the method originally suggested by Schmid [41].
Synovitis is a frequent detectable feature of KOA which may predict other structural changes, even in patients without radiographic evidence of OA [44]. Synovial thickening around the IFP using non-contrast MRI showed on histopathology to represent mild chronic synovitis [45]. Anterior knee pain is thought to be associated with alterations of the IFP. Since the IFP is extensively innervated, the IFP is exquisitely sensitive as are the anterior synovial tissue and capsule [46]. Hill et al. demonstrated that a semiquantitative measure of synovitis from the IFP is associated with pain severity [16]. Javaid et al. confirmed previous reports regarding the correlation between knee pain [47], structural characteristics of KOA assessed radiographically, and MRI findings [48]. The IFP can be regarded as a specialized adipose tissue in close contact with synovial layers and the articular cartilage. Immune cells infiltration of the IFP has been described in human KOA and in animal models of OA. Furthermore, the dense presence of nociceptive nerve fibers can determine anterior pain and are capable of maintaining inflammation by the release of substance P. Studies separately assessing and investigating signal alterations in IFP and joint effusion on non-contrast-enhanced MRI images gave controversial results: some indicated that effusion was associated with pain or cartilage loss, while signal alterations in IFP were not [49, 50]. Different experiences suggest the opposite [51]. Crema and colleagues, in a study using contrast-enhanced MRI images, demonstrated that pain is associated with peripatellar synovial thickness and not with signal alterations in IFP itself [52]. Recently, Ballegaard et al. described that perfusion variables observed using dynamic contrast-enhanced (DCE) MRI, reflecting the intensity of inflammation in the IFP, were associated with pain severity in KOA [53].
As already mentioned, the psycho-affective sphere is strongly impactful in KOA. Central pain sensitivity plays an important role in pain severity among patients with knee OA [10], and psychosocial factors account for some of this variance in pain and other symptoms [54, 55]. Observational studies found that negative mood was correlated with more joints involvement and disability by OA and vice versa [56]. OA was demonstrated to be responsible for declined life satisfaction, and depression and anxiety were two major mood problems correlated. The level of disability experienced in patients with KOA showed to correlate more accurately with psychological involvement than with radiographic scores [57].
There are some limitations in the present study that have to be mentioned. First of all, a potential selection bias is that our cohort was composed of subjects referring to a tertiary rheumatologic center, not reflecting the general population. Secondly, the degenerative findings on patients with KOA were not compared to an age- and sex-matched control group of asymptomatic subjects and, therefore, the crucial imaging findings responsible for the clinical symptoms could not be isolated. Third, we used non-contrast MRI to assess the severity of synovitis. However, as of today, in the majority of large epidemiologic studies, contrast has not been used for assessing synovitis, because of the potential toxicity involved with the intravenous administration of contrast agents and the associated costs. Finally, the difficulty to assess the cross-sectional relationship between MRI findings and knee pain has recently been pointed out, demonstrating the fluctuating nature of BMLs and knee pain, with the latter dependent on the former. Longer follow-up is needed to fully evaluate the importance of these OA findings on MRI for long-term clinical outcomes, such as the development of persistent pain.
Conclusions
This study presents a comprehensive comparison of radiographic- and MRI-based structural findings in a cohort of KOA patients, who constitute a sound proportion of all KOA patients. Our results suggest that knee pain is independently associated with MRI features, such as larger BMLs, IFP synovitis, and high levels of psychological distress, but not with radiographic knee OA, expanding our understanding of knee pain in older adults. The findings have the potential to be translated towards developing targeted therapies to prevent the development of KOA.
References
Guccione AA, Felson DT, Anderson JJ et al (1994) The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health 84:351–358
Felson DT, Zhang Y (1998) An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum 41:1343–1355
Oliveria SA, Felson DT, Reed JI, Cirillo PA, Walker AM (1995) Incidence of symptomatic hand, hip, and knee osteoarthritis among patients in a health maintenance organization. Arthritis Rheum 38:1134–1341
Salaffi F, De Angelis R, Grassi W (2005) MArche Pain Prevalence INvestigation Group (MAPPING) study. Prevalence of musculoskeletal conditions in an Italian population sample: results of a regional community-based study. I. The MAPPING study. Clin Exp Rheumatol 23:819–828
Salaffi F, De Angelis R, Stancati A, Grassi W (2005) MArche Pain Prevalence INvestigation Group (MAPPING) study. Health-related quality of life in multiple musculoskeletal conditions: a cross-sectional population based epidemiological study. II. The MAPPING study. Clin Exp Rheumatol 23:829–839
Salaffi F, Carotti M, Stancati A, Grassi W (2005) Health-related quality of life in older adults with symptomatic hip and knee osteoarthritis: a comparison with matched healthy controls. Aging Clin Exp Res 17:255–263
Salaffi F, Carotti M, Grassi W (2005) Health-related quality of life in patients with hip or knee osteoarthritis: comparison of generic and disease-specific instruments. Clin Rheumatol 24:29–37
Fotiadou A, Karantanas A (2009) Acute nontraumatic adult knee pain: the role of MR imaging. Radiol Med 114:437–447
Philbin EF, Ries MD, Groff G, Sheesley KA, French TS, Pearson TA (1996) Osteoarthritis as a determinant of an adverse coronary heart disease risk profile. J Cardiovasc Risk 3:529–533
Salaffi F, Ciapetti A, Carotti M (2014) The sources of pain in osteoarthritis: a pathophysiological review. Reumatismo 66:57–71
Dieppe P, Cushnaghan J, Shepstone L (1997) The Bristol OA500 Study: progression of osteoarthritis (OA) over 3 years and the relationship between clinical and radiographic changes at the knee joint. Osteoarthr Cartil 5:87–97
Solivetti FM, Guerrisi A, Salducca N et al (2016) Appropriateness of knee MRI prescriptions: clinical, economic and technical issues. Radiol Med 121:315–322
Conaghan PG, Felson D, Gold G, Lohmander S, Totterman S, Altman R (2006) MRI and non-cartilaginous structures in knee osteoarthritis. Osteoarthr Cartil 14(Suppl A):A87–A94
Felson DT, Niu J, Guermazi A et al (2007) Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum 56:2986–2992
Leigh Zhai G, Blizzard L, Srikanth V et al (2006) Correlates of Knee Pain in Older Adults: tasmanian Older Adult Cohort Study Arthritis and Rheumatism. Arthritis Care Res 55:264–271
Hill CL, Hunter DJ, Niu J et al (2007) Synovitis detected on magnetic resonance imaging and its relation to pain and cartilage loss in knee osteoarthritis. Ann Rheum Dis 66:1599–1603
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16:494–502
Altman R, Asch E, Bloch D et al (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 29:1039–1049
Salaffi F, Leardini G, Canesi B et al (2003) GOnorthrosis and Quality Of Life Assessment (GOQOLA). Reliability and validity of the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index in Italian patients with osteoarthritis of the knee. Osteoarthr Cartil 11:551–560
Ware J, Sherbourne CD (1992) The MOS 36-item short form health survey (SF-36). 1. Conceptual frame work and item selection. Med Care 30:473–481
Ware J, Kosinski M, Bayliss M, Rogers WH, Razec A (1995) Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care 4:AS264–AS279
Peterfy CG, Guermazi A, Zaim S et al (2004) Whole-organ magnetic resonance imaging score (WORMS) of the knee in osteoarthritis. Osteoarthr Cartil 12:177–190
Paparo F, Revelli M, Piccazzo R et al (2015) Extrusion of the medial meniscus in knee osteoarthritis assessed with a rotating clino-orthostatic permanent-magnet MRI scanner. Radiol Med 120:329–337
Tanamas SK, Wluka AE, Pelletier JP et al (2010) Bone marrow lesions in people with knee osteoarthritis predict progression of disease and joint replacement: a longitudinal study. Rheumatology (Oxford) 49:2413–2419
Felson DT, Chaisson CE, Hill CL et al (2001) The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med 134:541–549
Atukorala I, Kwoh CK, Guermazi A, Roemer FW, Boudreau RM, Hannon MJ, Hunter DJ (2016) Synovitis in knee osteoarthritis: a precursor of disease? Ann Rheum Dis 75:390–395
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Mease PJ, Hanna S, Frakes EP, Altman RD (2011) Pain mechanisms in osteoarthritis: understanding the role of central pain and current approaches to its treatment. J Rheumatol 38:1546–1551
Sharma L, Chmiel JS, Almagor O et al (2014) Significance of preradiographic magnetic resonance imaging lesions in persons at increased risk of knee osteoarthritis. Arthritis Rheumatol 66:1811–1819
Zanetti M, Bruder E, Romero J, Hodler J (2000) Bone marrow edema pattern in osteoarthritic knees: correlation between MR imaging and histologic findings. Radiology 215:835–840
Lo GH, McAlindon TE, Niu J et al (2009) Bone marrow lesions and joint effusion are strongly and independently associated with weight-bearing pain in knee osteoarthritis: data from the osteoarthritis initiative. Osteoarthr Cartil 17:1562–1569
Dore D, Quinn S, Ding C et al (2010) Natural history and clinical significance of MRI-detected bone marrow lesions at the knee: a prospective study in community dwelling older adults. Arthritis Res Ther 12:R223
Guermazi A, Niu J, Hayashi D et al (2012) Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study). BMJ 345:e5339
Kornaat PR, Bloem JL, Ceulemans RY et al (2006) Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology 239:811–817
Kornaat PR, Kloppenburg M, Sharma R et al (2007) Bone marrow edema-like lesions change in volume in the majority of patients. With osteoarthritis; associations with clinical features. Eur Radiol 17:3073–3078
Torres L, Dunlop DD, Peterfy C et al (2006) The relationship between specific tissue lesions and pain severity in persons with knee osteoarthritis. Osteoarthr Cartil 14:1033–1040
Cicuttini FM, Baker J, Hart DJ et al (1996) Association of pain with radiological changes in different compartments and views of the knee joint. Osteoarthr Cartil 4:143–147
Burr DB (2004) The importance of subchondral bone in the progression of osteoarthritis. J Rheumatol Suppl 70:77–80
Simkin P (2004) Bone pain and pressure in osteoarthritic joints. Novartis Found Symp 260:179–186
Mayerhoefer ME, Breitenseher M, Hofmann S et al (2004) Computer-assisted quantitative analysis of bone marrow edema of the knee: initial experience with a new method. Am J Roentgenol 182:1399–1403
Schmid MR, Hodler J, Vienne P, Binkert CA, Zanetti M (2002) Bone marrow abnormalities of foot and ankle: STIR versus T1- weighted contrast-enhanced fat-suppressed spin-echo MR imaging. Radiology 224:463–469
Mayerhoefer ME, Breitenseher MJ, Kramer J, Aigner N, Norden C, Hofmann S (2005) STIR vs. T1-weighted fat-suppressed gadolinium-enhanced MRI of bone marrow edema of the knee: computer-assisted quantitative comparison and influence of injected contrast media volume and acquisition parameters. J Magn Reson Imaging 22:788–793
Roemer FW, Khrad H, Hayashi D et al (2010) Volumetric and semiquantitative assessment of MRI-detected subchondral bone marrow lesions in knee osteoarthritis: a comparison of contrast-enhanced and nonenhanced imaging. Osteoarthr Cartil 18:1062–1066
Scanzello CR, McKeon B, Swain BH et al (2001) Synovial inflammation in patients undergoing arthtroscopic meniscectomy: molecolar characterization and relationship to symptom. Arthritis Reum 63:391–400
Fernandez-Madrid F, Karvonen RL, Teitge RA et al (1995) Synovial thickening detected by MR imaging in osteoarthritis of the knee confirmed by biopsy as synovitis. Magn Reson Imaging 13:177–183
Dye SF, Vaupel GL, Dye CC (1998) Conscious neurosensory mapping of the internal structures of the human knee without intraarticular anesthesia. Am J Sports Med 26:773–777
Javaid MK, Kiran A, Guermazi A, Health ABC Study et al (2012) Individual magnetic resonance imaging and radiographic features of knee osteoarthritis in subjects with unilateral knee pain. Arthritis Rheum 64:3246–3255
Neogi T, Felson D, Niu J et al (2009) Association between radiographic features of knee osteoarthritis and pain: results from two cohort studies. BMJ 339:b2844
Roemer FW, Guermazi A, Felson DT et al (2011) Presence of MRI-detected joint effusion and synovitis increases the risk of cartilage loss in knees without osteoarthritis at 30-month follow-up: the MOST study. Ann Rheum Dis 70:1804–1809
Ai F, Yu C, Zhang W, Morelli JN, Kacher D, Li X (2010) MR imaging of knee osteoarthritis and correlation of findings with reported patient pain. J Huazhong Univ Sci Technol Med Sci 30:248–254
Zhang Y, Nevitt M, Niu J et al (2011) Fluctuation of knee pain and changes in bone marrow lesions, effusions, and synovitis on magnetic resonance imaging. Arthritis Rheum 63:691–699
Crema MD, Felson DT, Roemer FW et al (2013) Peripatellar synovitis: comparison between non-contrast-enhanced and contrast-enhanced MRI and association with pain. The MOST study. Osteoarthr Cartil 21:413–418
Ballegaard C, Riis RG, Bliddal H et al (2014) Knee pain and inflammation in the infrapatellar fat pad estimated by conventional and dynamic contrastenhanced magnetic resonance imaging in obese patients with osteoarthritis: a cross-sectional study. Osteoarthr Cartilage 22:933–940
Rosemann T, Backenstrass M, Joest K, Rosemann A, Szecsenyi J, Laux G (2007) Predictors of depression in a sample of 1021 primary care patients with osteoarthritis. Arthritis Rheum 57:415–422
Somers T, Keefe F, Godiwala N, Hoyler G (2009) Psychosocial factors and the pain experience of osteoarthritis patients: new findings and new directions. Curr Opin Rheumatol 21:501–506
Van Baar ME, Dekker J, Lemmers JA (1998) Pain and disability in patients with osteoarthritis of hip or knee. J Rheumatol 25:125–133
Salaffi F, Cavalieri F, Nolli M, Ferraccioli GF (1991) Analysis of disability in knee osteoarthritis: relationship with age and psychological variables but not with radiographic score. J Rheumatol 8:1581–1586
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have not conflict of interests.
Ethical approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institution and national research committee and with the 1964 Helsinki declaration and its later amendments of comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Carotti, M., Salaffi, F., Di Carlo, M. et al. Relationship between magnetic resonance imaging findings, radiological grading, psychological distress and pain in patients with symptomatic knee osteoarthritis. Radiol med 122, 934–943 (2017). https://doi.org/10.1007/s11547-017-0799-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-017-0799-6