Abstract
Aim
To assess the diagnostic performance of magnetic resonance imaging (MRI) with gadoxetic acid in the identification of hepatocellular carcinoma (HCC) nodules by comparison with histological findings.
Methods
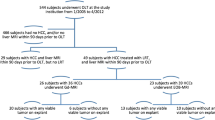
In a cohort of patients suffering from cirrhosis of various etiologies (chronic hepatitis C virus (HCV) or hepatitis B virus (HBV), alcohol abuse, cryptogenic forms), we selected 17 patients affected by HCC who were eligible for liver transplantation on the basis of a computed-tomography (CT) total-body examination. Such patients also underwent an MRI examination under basal conditions, and with four dynamic phases, as well as a hepatobiliary phase acquired after at least 20 min and recognized by the excretion of contrast agent into the bile duct, following intravenous administration of 0.05 mol/kg of gadoxetic acid (gadoxetate disodium, Primovist®; Bayer, Osaka, Japan). The MRI images were then evaluated in a double-blinded experimental setup by two radiologists experienced in imaging of the liver. The diagnosis of HCC was made in the presence of nodular lesions that showed typical or atypical enhancement patterns. The liver was subsequently explanted (on average 47.4 days after MRI evaluation), dissected into 1-cm samples, and histologically evaluated according to the classification of Edmondson–Steiner.
Results
At the histopathological examination, 46 nodules were identified, on average 2.7 nodules for each patient. Of these, 37 were hepatocellular carcinomas, 3 were characterized by histologically unrecognizable complete necrosis, and 6 showed high-grade dysplasia. MRI with hepatospecific contrast medium showed inter-observer average values of sensitivity, specificity, and diagnostic accuracy of 94.6, 90, and 93.6 %, respectively. In one case, a nodule was not identified by MRI with gadoxetic acid, even in the hepatospecific phase (false negative (FN)). This result could be implicated to the long time interval between the analysis and the explant (88 days). In another case, there was an overdiagnosis of a HCC with a typical nodular pattern (false positive (FP)), but which most likely should have been attributed to a previous echinococcus cyst. MRI analysis, in combination with the study of the hepatobiliary phase, also showed a greater sensitivity, the same specificity, and a greater diagnostic accuracy compared to MRI evaluated only in the dynamic phases (with an average percentage between the two operators, respectively, of 75.7, 90, and 78 %).
Conclusions
MRI with gadoxetic acid shows a diagnostic accuracy superior to contrast-enhanced MRI, allowing for the diagnosis of additional lesions, and it could be considered as an imaging method to carry out a more appropriate management of waiting lists for liver transplants.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Liver transplantation represents the best available treatment for hepatocellular carcinoma (HCC), as it offers the chance to eradicate also the underlying disease, i.e., cirrhosis [1]; however, in a regime of low availability of organs, a proper selection of patients judged to be candidates for this complex operation is crucial.
To date, magnetic resonance imaging (MRI) with non-tissue-specific contrast media has been reported to be an excellent imaging technique for preoperative staging and tumor size measurement [2–4]. In this framework, notably, the introduction of MRI studies with the use of a hepatospecific contrast agent has increased the diagnostic performance of this method, especially in the identification and characterization of lesions with atypical patterns.
Lesions with less functioning hepatocytes, such as most HCCs, do not accumulate Gd-EOB-DTPA and appear as low-signal-intensity foci against the enhancing high-signal parenchyma in the hepatobiliary phase, thus improving tumor detection.
Since the amount of hepatocyte-selective contrast agent uptake by HCCs depends on the grade of differentiation of the tumor and the number of functional hepatocytes, post-contrast delayed images have been shown to correlate with the histological degree of malignancy [5, 6].
In this study, we aimed to investigate the correlation, in terms of sensitivity and specificity, between the identification of focal liver lesions with MRI using gadoxetic acid as contrast agent, and the histological findings obtained from explanted livers.
Materials and methods
We retrospectively evaluated the contrast-enhanced (CE) MRI examinations performed with a hepatospecific contrast medium in 17 patients with HCC, who were eligible for liver transplantation on the basis of a computed-tomography (CT) total-body examination, and compared these measurements with the histological findings on explanted livers.
MRI analyses were performed on average 47.4 days before surgery (range 1–89 days) in order to perform a restaging of disease.
All participants, or a legal guardian on their behalf, provided informed consent.
The majority of patients (14) (82 %) had previously undergone surgery (resection of liver segments) or interventional procedures (transjugular intrahepatic portosystemic shunt (TIPS), pseudoaneurysm embolization, chemoembolization, ablation therapy through radiofrequency or microwaves)—as summarized in Table 1—in order to maintain patients within the list for transplantation (13) (76.5 %), with the exception of a TIPS (positioned to remedy a condition of portal hypertension) and an embolization of a pseudoaneurysm (performed to prevent bleeding).
The mean time on waiting list was 149 ± 140 days for patients with bridging therapy, and 86 ± 61 for patients without bridging therapy.
All patients met the Milan and up-to-seven criteria, on the basis of number and size of tumors diagnosed by standard MRI.
MRI examinations
MRI examinations were performed on a 1.5-T MR system (Achieva, Philips Medical SystemsTM, Best, the Netherlands) using a 16-channel phased-array surface coil, with the patients resting in a supine position and having fasted for at least 4 h before.
In all cases, the acquisition was performed in basal conditions and in dynamic phases after the intravenous administration of 0.05 mol/kg of gadoxetic acid (gadoxetate disodium, Primovist®; Bayer, Osaka, Japan), followed by a bolus of 10 ml of saline injected at a flow rate of 2 ml/s.
The dynamic phases acquired were the following:
-
early arterial (15 s after administration of the contrast agent);
-
late arterial (35 s from the start and immediately after the previous phase);
-
portal (about 70 s after administration of the contrast agent);
-
at equilibrium (150 s after administration of the contrast agent).
Subsequently, other sequences were acquired in the axial plane: T2 TSE (turbo spin-echo), T2 adiabatic spectral inversion recovery (SPAIR), and diffusion-weighted imaging (DWI).
After at least 20 min, the hepatobiliary phases, recognized by the excretion of contrast agent into the bile duct (or bile ducts in the main event of a previous surgery on the biliary system), were acquired with the use of T1 and T1 SPGR fat-sat-spoiled gradient-echo (GRE) “in phase” on the axial plane.
The detailed acquisition protocol is summarized in Table 2.
Analysis of images
The MR images were evaluated under double-blind conditions by two radiologists with at least 10 years of experience in liver imaging and at least 5 years of experience in hepatobiliary-phase MR imaging. The diagnosis of HCC was made in the presence of nodular lesions that showed one of the following enhancement patterns:
-
intense enhancement in the arterial phase and washout in the portal phase or equilibrium (typical pattern);
-
intense enhancement in the arterial phase, washout in the portal phase or equilibrium, and “hypointensity” due to no uptake of the contrast agent during the hepatobiliary phase (typical pattern);
-
intense enhancement in the arterial phase and “hypointensity” due to no uptake during the hepatobiliary phase (atypical pattern);
-
mild or atypical enhancement in the arterial phase gradient, presence of washout in the portal phase or equilibrium, and no uptake during the hepatobiliary phase (atypical pattern).
During hepatobiliary phase, we defined “no-uptake” as positive only when the lesion was clearly depicted as moderately or substantially hypointense compared with the hepatic parenchyma.
Each operator reported size and location of the lesions found.
Treated lesions with partial or no response were evaluated only for the residual vital portion of the lesions as the presence of enhancement pattern described above.
Statistical analysis
Sensitivity, specificity, and diagnostic accuracy of each measurement were first evaluated separately, and then correlated with the histopathological findings, which are considered the gold standard for diagnosis.
Sensitivity was calculated as the ratio of TP (true positives; the number of nodules correctly diagnosed through imaging techniques) to total tumors identified histologically (TP/TP + FN, false negatives). Specificity was calculated as the ratio of TN (true negatives, which is the number of dysplastic nodules and those considered non-viable or necrotic after downstaging) to the total of non-neoplastic nodules (TN/TN + FP, false positives). The diagnostic accuracy was calculated using the formula: TP + TN/total nodules identified (TP + TN + FN + FP).
The imaging measurements obtained (TP and TN) were also compared separately with those detected histologically, using the nonparametric Spearman correlation coefficient; a value of p < 0.001 was considered statistically significant.
In addition, the correlation between the results obtained by the examiners was calculated using the kappa test in order to assess the repeatability of the evaluations. Subsequently, the two radiologists performed a review of the MRI examinations, in order to evaluate the diagnostic accuracy of the dynamic and hepatobiliary phases.
In particular, it was compared the number of lesions (TP and TN) identified only by dynamic MRI positive phases (typical pattern), MRI with dynamic and hepatobiliary positive phases (typical pattern), and the MRI dynamic negative phases, but positive only with the aid of hepatobiliary phase (atypical patterns, i.e., cases in which the use of the hepatospecific contrast agent is essential for the diagnosis).
Lastly, a restaging of patients was performed, in agreement with the data obtained through hepatospecific contrast-enhanced MRI, and was calculated by the number of patients as follows:
-
subjects who met the Milan criteria with standard dynamic MRI but not with the MRI using gadoxetic acid. These patients, however, met the up-to-seven criteria;
-
subjects who met the Milan or up-to-seven criteria with standard methods, but did not meet any criteria currently in use after MRI with hepatospecific contrast medium.
Histopathological analysis of explanted livers
The organ was removed, weighed, and subsequently dissected into 1-cm explants to be closely examined; the hepatic artery, portal vein, bile duct, and gallbladder were cut longitudinally.
For each tumor lesion, the following features were described: the seat, or the anatomical segment; the dimensions; the cellular grading based on nuclear characteristics according to the classification of Edmondson–Steiner; the presence of microscopic vascular invasion; and the possible presence of satellite nodules, i.e., located within 2 cm of the primary lesion.
Results
A total of 46 nodules were identified on the basis of a histopathological examination (average 2.7 nodules for each patient; range 1–6 nodules/patient). Of these nodules, 37 were HCCs, 3 were characterized by histologically unrecognizable complete necrosis, and 6 showed high-level dysplasia. Some of these HCCs showed areas of partial necrosis, and most of them were moderately or poorly differentiated (Grade II–III of the Edmondson–Steiner scale).
The histological data are summarized in Table 3.
Histologically, the nodules showed an average size of 17.2 mm (range 5–56 mm). The correlation of the dimensions measured with MRI imaging was high for both operators (r = 0.96) with statistically significant values (p < 0.0001).
On the analysis carried out by both operators, 28 showed a typical pattern (75.6 %) (Fig. 1), 8 showed an atypical pattern (21.6 %) (Fig. 2), and 1 nodule was not detected by any of the methods used (FN).
Hepatospecific CE-MRI (gadoxetic acid) and T1 spoiled gradient-echo fat-sat show HCC nodule (28 × 31 mm) with typical pattern located in the VI liver segment. There is evidence of early enhancement during the arterial phase (a), and washout with evidence of a pseudocapsule during the portal phase (b). Lesion does not show uptake of contrast agent during hepatobiliary phase (c). Histological findings: poorly differentiated hepatocellular carcinoma
Hepatospecific CE-MRI (gadoxetic acid) and T1 spoiled gradient-echo fat-sat depict two nodules: one HCC with atypical pattern and another one with typical pattern both in the VII liver segment. CE-MRI shows early enhancement on arterial phase of two nodules of 9 mm of diameter (a). During portal phase (b), a nodule (yellow arrow) is characterized by rapid washout, differently from the other lesion (red arrow). During the hepatobiliary phase (c), both lesions show no uptake of the hepatospecific contrast agent. Histological findings: well-differentiated hepatocellular carcinomas
The hepatobiliary phase allowed for the efficacious diagnosis of 8 (28.6 %) additional hepatocellular carcinomas.
MRI with hepatospecific contrast medium showed sensitivity, specificity, and diagnostic accuracy of 97.3, 90, and 95.7 % for the first operator, and 91.9, 90, and 91.5 % for the second operator. The inter-observer average values of sensitivity, specificity, and diagnostic accuracy were 94.6, 90, and 93.6 %, respectively.
In one case, a nodule was not identified by MRI with gadoxetic acid, even in the hepatospecific phase (FN). In this case, the time interval between the analysis and the explant was particularly high (88 days).
In another case, a nodule was diagnosed as a hepatocellular carcinoma with a typical nodular pattern, although likely it should have been referable to a previous inflammatory–infectious event (echinococcus cyst), as reported in the medical history of the patient.
MRI assessment, together with the hepatobiliary-phase analysis, also showed greater sensitivity, the same specificity, and greater diagnostic accuracy (94.6, 90, and 93.6 %) compared to MRI evaluated in the dynamic phases alone (75.7, 90, and 78 %).
The staging of patients before transplantation performed with standard dynamic MRI methods resulted in the inclusion of 12 patients according to the Milan criteria and all 17 patients considering the up-to-seven criteria.
With the aid of the hepatobiliary phase, 11 patients were included in the Milan criteria (1 less, 5.9 %) and 14 in the up-to-seven criteria (3 less, 17.6 %). These 3 patients were found to be outside the transplantation criteria currently in use, and the diagnosis was confirmed histologically.
The comparison between the staging performed through hepatobiliary MRI with hepatospecific contrast medium, and that deduced from the histological analysis, showed a high correlation, except for two patients who were not included in the Milan criteria with standard MRI. Of these, one result was a false positive, and the other had been excluded from the Milan criteria due to an overestimation of the size, although it fit the up-to-seven criteria.
Discussion
Given the low availability of organs and the related allocation inadequacy, a proper selection of patients eligible for liver transplantation is crucial, especially in light of the ethical controversies that emerged with the current scoring system, which seems to favor patients with HCC compared to those with other diseases [7, 8], leading to the so-called MELD-exception (Model for End-Stage Liver Disease).
MRI and CT with dynamic use of extracellular contrast agents are currently considered the preferable choice for noninvasive diagnosis and staging of hepatocellular carcinomas greater than 1 cm, and with a typical pattern (intense contrast enhancement in the blood phase and the presence of washout in the portal phase and/or late phase) [9].
A correct diagnosis has gained more importance following the recent expansion of the criteria for inclusion in the transplant list: The “Milan criteria” are often replaced by the “up-to-seven criteria” proposed by Mazzaferro et al. [10], as these ensure a patient survival rate of 71.2 % at 5 years from transplantation, which is indeed similar to that of patients who fit the conventional criteria.
The introduction of the MRI studies with hepatospecific contrast media has increased the diagnostic performance of this method, especially in the identification and characterization of lesions with atypical patterns, i.e., those which do not show one or more of the typical characters described above (lesions that do not show a significant washout in the portal and/or late stages or lesions characterized by washout with small or no obvious enhancement in the arterial phase).
The analysis of the hepatobiliary phase in which we can appreciate the excretion of the contrast agent formerly taken up by liver cells, in the bile ducts, adds valuable information about the degree of cellular anaplasia: liver cells which have lost cell differentiation will likely have a different behavior than the surrounding liver parenchyma and appear “hypointense.”
Our study showed a high sensitivity (94.6 %) of hepatospecific MRI contrast agents and a specificity of 90 %, equal to the specificity of non-hepatospecific MRI contrast agents. These encouraging results are attributable to the large diagnostic criteria selected that consider both positive nodules with a typical pattern (Fig. 1) and those with an atypical pattern, associated with hypointensity in the hepatobiliary phase (Fig. 2). This type of analysis is based on several studies that have shown a higher diagnostic value of the hepatobiliary phase when used in the diagnostic workup, in association with the dynamic phases [11, 12].
The two examiners within the double-blinded setup adopted showed a good correlation in the evaluations (k = 0.72), which was particularly high for positive observations (k = 0.83), probably due to the higher prevalence of the latter.
In this study, all examinations were reviewed by radiologists with at least 10 years of experience in liver imaging and at least 5 years of experience in hepatobiliary-phase MR imaging. However, the hepatobiliary-phase imaging appearance of HCC was not included in the New OPTN/UNOS (Organ Procurement and Transplantation Network/United Network for Organ Sharing) Policy for Liver Transplant Allocation because the consensus meeting took place shortly after Food and Drug Administration approval of the agent for clinical use in the United States [13].
We think that it could be interest to evaluate the added value of the hepatobiliary phase also for novice reader in order to quantify the real contribution to the final diagnosis in clinical practice.
The high incidence of hepatocellular carcinomas (100 %) in our sample of patients, who were already considered candidates for transplantation on the basis of a CT-total-body examination, could also have influenced the assessments made by the two operators, with a tendency toward overestimation of tumor lesions. The results, however, showed only 1 FP (Fig. 3), and the data are in agreement with different studies in the literature which demonstrated a high diagnostic accuracy of MRI with hepatospecific contrast medium, in comparison with dynamic contrast-enhanced MRI alone [14, 15].
False-positive case. Hepatospecific CE-MRI (gadoxetic acid) and T1 spoiled gradient-echo fat-sat in the arterial phase show a nodule (17 mm) in the VII liver segment with intense enhancement (a) and a washout with pseudocapsule evidence during the late phase (b). In the hepatobiliary phase (c), nodule does not show contrast medium uptake, and it was considered as a typical pattern for HCC. The patient had another HCC nodule, which is not shown. Histological findings: infectious–inflammatory sequelae
Such studies, however, encompass different types of patients, which include both those subjected to total hepatectomy in view of liver transplantation, and those who underwent a lobectomy, removal of a segment, or simply a needle biopsy for histological confirmation of suspicious lesions. Thus, it cannot be excluded that the patients considered in these studies had additional injuries, undiagnosed with standard imaging analysis, with an underestimation of lesions actually present and a consequent overestimation of diagnostic accuracy.
The peculiarity of our study lies in the population itself of the patients selected, as we considered only transplant candidates with a histological assessment of the actual number of tumor lesions present or not in the organ considered as a whole; this brought us to a more accurate and reliable evaluation of diagnostic performance. The diagnostic accuracy as evaluated through the analysis of MRI with hepatospecific contrast medium is also more than just a dynamic study, with the diagnosis of eight further hepatocellular carcinomas, corresponding to an additional 28.6 % of diagnosed lesions.
In our experience, the mean time on waiting list was 149 days, and the interval for imaging before orthotopic liver transplantation (OLT) was 47 days. As reported by Singh et al., imaging of the recipient liver should be performed as close to the time of transplantation as possible because tumors may grow rapidly, invade local structures, or metastasize, which may affect the stage of disease, management perspective, and surgical technique [16].
Several recent studies have evaluated MRI data with gadoxetic acid in patients eligible for transplantation and compared it with findings from the histological examination of the liver in toto [16–19]. Bartolozzi et al. [17] evaluated the dynamic phases of RM separately, particularly the arterial phase and the hepatobiliary one, demonstrating a high predictive value of the typical pattern and the high sensitivity of the hepatobiliary phase, close to 100 % in the group of hepatocellular carcinomas, as well as high specificity, considered evaluating both hepatocellular carcinomas and high-degree dysplastic lesions.
Nakamura et al. [18] compared different combinations of diagnostic criteria, obtained by considering only the arterial and hepatobiliary phases, reporting very low sensitivity values (ranging between 22.5 and 69 %). However, an important limitation of such approach is the missing evaluation of the portal and late phases, which instead were included in our present study, and in which lesions that showed washout associated with hypocaptation during hepatobiliary phases (atypical pattern) were considered positive.
Baird et al. [19] showed a very high specificity (100 %) but a very low sensitivity (42.5 %). These results could be explained by the time lag between the diagnostic test and the liver removal (in 1/3 of the cases of more than 4 months) and also by the high prevalence of moderately differentiated or well-differentiated hepatocellular carcinomas in the study population.
Criticism toward this methodological approach was addressed to the excessive number of false positives that the assessment of hepatobiliary phase can generate, resulting in reduced specificity. To overcome this limitation, in our study we considered positive only the cases in which the intensity of the lesions was markedly and unequivocally lower than that of the surrounding parenchyma.
Moreover, our study shows that MRI with gadoxetic acid can influence and change the diagnostic classification of patients, and thus re-establish available therapeutic strategies. Our restaging, simulated on the basis of data obtained taking into account the hepatobiliary evaluation, shows that a significant percentage of patients (17.6 %, 3 patients) did not even meet the broadened up-to-seven criteria, recently introduced.
In two of those 3 cases, the additional lesions found, which resulted in the exclusion from transplantability criteria, showed a diameter less than or equal to 1 cm as well as an atypical pattern (Fig. 3). This demonstrates the high diagnostic potential of MRI with gadoxetic acid, particularly in the early diagnosis of HCCs, even when these lesions do not express the typical alterations of the microcirculation (sinusoidal capillarization and presence of arteries “not coupled” to bile vessels), which occur when studied with the characteristic dynamic MRI pattern.
In the third case, the exclusion from the up-to-seven criteria was determined by a more accurate assessment of the main nodule size (56 vs. 48 mm). The reliability of the measurements is shown in our study by the high correlation between the actual size of the lesions identified, as reported histologically, and those measured with pre-intervention MRI (r = 0.96).
Today, due to the continuous improvement of imaging technique, the right allocation of patients for OLT is a real challenge both for clinicians both for radiologists and surgeons. When Radiologists made a false-positive diagnosis of HCC, it could be an incorrect elimination from transplantation candidacy. Indeed, a false-positive diagnosis of HCCs in potential candidates may lead to incorrect assignment of additional priority for liver transplantation according to the UNOS guidelines. Nevertheless making a false-negative diagnosis of HCC might also cause problems [20].
The increased sensitivity of Gd-EOB MRI could exclude from the best therapy available but it is also true that it is well debated that both Milan and new Milan criteria for listing are felt to be too restrictive. However approaches to expand criteria for OLT listing are limited by the shortage of donated livers and lack of robust pretransplant imaging findings to identify predictors of tumor recurrence such as microscopic vascular invasion and tumor satellites that prevail among patients exceeding Milan criteria [21].
Listing for transplantation based on UCSF criteria, which include 1 nodule ≤6.5 cm, or 2–3 nodules ≤4.5 cm to reach a total tumor diameter ≤8 cm, resulted in a comparable 5-year recurrence-free probability (90 and 94 %) in patients within and outside Milan criteria, while the risk of pretreatment tumor understaging was similar for patients within the Milan (20 %) and UCSF (University of California San Francisco) (29 %) criteria [22].
On the basis of all these considerations, it can be deduced that choices leaning toward liver transplantation that lie outside the currently accepted criteria determine not only a waste of economic resources, but also a high probability of recurrence of the disease in an organ that is ineluctably subtracted to other patients with higher life expectancy.
An important limitation of our study is the small number of patients. Further studies with a large population should be performed to verify the potential of hepatobiliary imaging, especially in patients with advanced liver cirrhosis.
Conclusions
MRI with hepatospecific contrast medium shows high sensitivity and specificity in the diagnosis of hepatocellular carcinomas in liver cirrhosis. Our results show that the diagnostic accuracy was superior to that of the dynamic MRI alone, leading to the diagnosis of 8 additional HCCs (28.6 % of the total lesions).
The clinical use of this method, especially in patients whose perspectives are liver transplantation, could play a primary role, allowing for a more appropriate management of waiting lists, with a reduced squander of economic and health resources and, above all, a minimization of the waste of organs that could instead be assigned to those patients who could potentially show greater benefits in terms of outcome. In our study, three patients, or 17.6 %, would not have been eligible for transplantation if the staging had taken into account the hepatobiliary phase with gadoxetic acid.
In conclusion, our data are encouraging and may be useful in the critical decision-making of whether a patient is eligible for liver transplantation; however, additional studies are needed to confirm and extend the results of our research, in order to consider them more stable and reliable.
References
Forner A, Llovet JM, Bruix J (2012) Hepatocellular carcinoma. Lancet 379:1245–1255. doi:10.1016/S0140-6736(11)61347-0 (PMID: 22353262)
Noguchi Y, Murakami T, Kim T, Hori M, Osuga K, Kawata S, Kumano S, Okada A, Sugiura T, Nakamura H (2003) Detection of hepatocellular carcinoma: comparison of dynamic MR imaging with dynamic double arterial phase helical CT. AJR Am J Roentgenol 180:455–460 (PMID:12540451)
Libbrecht L, Bielen D, Verslype C, Vanbeckevoort D, Pirenne J, Nevens F, Desmet V, Roskams T (2002) Focal lesions in cirrhotic explant livers: pathological evaluation and accuracy of pretransplantation imaging examinations. Liver Transpl 8:749–761 (PMID:12200773)
Hanna RF, Kased N, Kwan SW, Gamst AC, Santosa AC, Hassanein T, Sirlin CB (2008) Double-contrast MRI for accurate staging of HCC in patients with cirrhosis. AJR Am J Roentgenol 190:47–57 (PMID: 18094293)
Kim HY, Choi JY, Kim CW, Bae SH, Yoon SK, Lee YJ, Rha SE, You YK, Kim DG, Jung ES (2012) Gadolinium ethoxybenzyl diethylenetriamine pentaacetic acid-enhanced magnetic resonance imaging predicts the histological grade of hepatocellular carcinoma only in patients with Child-Pugh class A cirrhosis. Liver Transpl 18:850–857. doi:10.1002/lt.23426 (PMID: 22407909)
Choi JY, Kim MJ, Park YN, Lee JM, Yoo SK, Rha SY, Seok JY (2011) Gadoxetate disodium-enhanced hepatobiliary phase MRI of hepatocellular carcinoma: correlation with histological characteristics. AJR Am J Roentgenol 197:399–405. doi:10.2214/AJR.10.5439 (PMID: 21785086)
Samuel D, Colombo M, El-Serag H, Sobesky R, Heaton N (2011) Toward optimizing the indications for orthotopic liver transplantation in hepatocellular carcinoma. Liver Transpl 17(Suppl 2):S6–S13. doi:10.1002/lt.22423 (PMID: 21858912)
David G, French B, Abt P, Feng S, Cameron AM (2012) Increasing disparity in waitlist mortality rates with increased MELD scores for candidates with versus without hepatocellular carcinoma. Liver Transpl 18:434–443. doi:10.1002/lt.23394 (PMID: 22271656)
Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A (2012) OLT for HCC Consensus Group. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol 13:11–22. doi:10.1016/S1470-2045(11)70175-9 (PMID: 22047762)
Mazzaferro V, Llovet JM, Miceli R, Bhoori S, Schiavo M, Mariani L, Camerini T, Roayaie S, Schwartz ME, Grazi GL, Adam R, Neuhaus P, Salizzoni M, Bruix J, Forner A, De Carlis L, Cillo U, Burroughs AK, Troisi R, Rossi M, Gerunda GE, Lerut J, Belghiti J, Boin I, Gugenheim J, Rochling F, Van Hoek B, Majno P (2009) Metroticket Investigator Study Group. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol 10:35–43. doi:10.1016/S1470-2045(08)70284-5 (PMID: 19058754)
Golfieri R, Grazioli L, Orlando E, Dormi A, Lucidi V, Corcioni B, Dettori E, Romanini L, Renzulli M (2012) Which is the best MRI marker of malignancy for atypical cirrhotic nodules: hypointensity in hepatobiliary phase alone or combined with other features? Classification after Gd-EOB-DTPA administration. J Magn Reson Imaging 36:648–657. doi:10.1002/jmri.23685 (PMID: 22592930)
Onishi H, Kim T, Imai Y, Hori M, Nagano H, Nakaya Y, Tsuboyama T, Nakamoto A, Tatsumi M, Kumano S, Okada M, Takamura M, Wakasa K, Tomiyama N, Murakami T (2012) Hypervascular hepatocellular carcinomas: detection with gadoxetate disodium-enhanced MR imaging and multiphasic multidetector CT. Eur Radiol 22:845–854. doi:10.1007/s00330-011-2316-y (PMID: 22057248)
Wald C, Russo MW, Heimbach JK, Hussain HK, Pomfret EA, Bruix J (2013) New OPTN/UNOS policy for liver transplant allocation: standardization of liver imaging, diagnosis, classification, and reporting of hepatocellular carcinoma. Radiology 266:376–382. doi:10.1148/radiol.12121698
Sano K, Ichikawa T, Motosugi U, Sou H, Muhi AM, Matsuda M, Nakano M, Sakamoto M, Nakazawa T, Asakawa M, Fujii H, Kitamura T, Enomoto N, Araki T (2011) Imagingstudy of early hepatocellular carcinoma: usefulness of gadoxetic acid-enhanced MR imaging. Radiology 261:834–844. doi:10.1148/radiol.11101840 (PMID: 21998047)
Di Martino M, Marin D, Guerrisi Baski M, Galati F, Rossi M, Brozzetti S, Masciangelo R, Passariello R, Catalano C (2010) Intra-individual comparison of gadoxetate disodium-enhanced MR Imaging and 64-section multidetector CT in the detection of hepatocellular carcinoma in patients with cirrhosis. Radiology 256:806–816. doi:10.1148/radiol.10091334
Singh AK, Nachiappan AC, Verma HA, Uppot RN, Blake MA, Saini S, Boland GW (2010) Postoperative imaging in liver transplantation: what radiologists should know. Radiographics 30:339–351. doi:10.1148/rg.302095124
Bartolozzi C, Battaglia V, Bargellini I, Bozzi E, Campani D, Pollina LE, Filipponi F (2013) Contrast-enhanced magnetic resonance imaging of 102 nodules in cirrhosis: correlation with histological findings on explanted livers. Abdom Imag 38:290–296. doi:10.1007/s00261-012-9952-9 (PMID: 23053453)
Nakamura Y, Tashiro H, Nambu J, Ohdan H, Kakizawa H, Date S, Awai K (2013) Detectability of hepatocellular disodium-enhanced hepatic MRI: tumor-by-tumor analysis in explant livers. J Magn Reson Imaging 37:684–691. doi:10.1002/jmri.23855
Baird AJ, Amos GJ, Saad NF, Benson MD (2013) Retrospective audit to determine the diagnostic accuracy of Primovist-enhanced MRI in the detection of hepatocellular carcinoma in cirrhosis with explant histopathology correlation. J Med Imaging Radiat Oncol 57:314–320. doi:10.1111/1754-9485.12038 (PMID: 23721140)
Lee DH, Lee JM, Baek JH, Shin CI, Han JK, Choi BI (2015) Diagnostic performance of gadoxetic acid-enhanced liver MR imaging in the detection of HCCs and allocation of transplant recipients on the basis of the Milan criteria and UNOS guidelines: correlation with histopathologic findings. Radiology 274:149–160. doi:10.1148/radiol.14140141
Sangiovanni A, Colombo M (2016) Treatment of hepatocellular carcinoma: beyond international guidelines. Liver Int 36(Suppl 1):124–129. doi:10.1111/liv.13028
Yao FY, Xiao L, Bass NM, Kerlan R, Ascher NL, Roberts JP (2007) Liver transplantation for hepatocellular carcinoma: validation of the UCSF expanded criteria based on preoperative imaging. Am J Transpl 7:2587–2596. doi:10.1111/j.1600-6143.2007.01965.x
Acknowledgments
The authors thank Viola Giacobbe for revising the English version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they do not have anything to disclose with respect to this manuscript.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the institutional and national ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Orlacchio, A., Chegai, F., Fabiano, S. et al. Role of MRI with hepatospecific contrast agent in the identification and characterization of focal liver lesions: pathological correlation in explanted livers. Radiol med 121, 588–596 (2016). https://doi.org/10.1007/s11547-016-0636-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-016-0636-3