Abstract
Purpose
Intensity-modulated radiotherapy has been suggested as the technique of choice for locally advanced head and neck cancer patients. In the last decade, most radiotherapy departments have focused their efforts in programs to implement this technique. We report our experience for parotid gland and constrictor muscle sparing with intensity-modulated radiotherapy in head and neck cancer using a step-and-shoot technique.
Methods
Thirty-four consecutive patients with squamous cell carcinoma of the nasopharynx, oropharynx and larynx treated between June 2008 and June 2011 were retrospectively evaluated. A simultaneous integrated boost was adopted to treat different volumes in 30 fractions over 6 weeks. Priority as organs at risk was given to the parotid glands as well as the constrictor muscle of the pharynx in 53 % (n = 18). Dysphagia and xerostomia were evaluated according to RTOG/EORTC scale at 6, 12 and 24 months. Outcomes were analysed using Kaplan–Meier curves.
Results
The median follow-up was 43 months. The 5-year overall survival was 70 %, and local control was 94 %. Grade 2 dysphagia and xerostomia at 6, 12 and 24 months were as follows: 26 % (n = 9), 23 % (n = 8), 23 % (n = 8) and 21 % (n = 7), 12 % (n = 4), 12 % (n = 4), respectively. No grade 3 or 4 toxicity was found. Ordinal logistic regression analysis demonstrated that hyposalivation was the main predictive factor for late dysphagia.
Conclusion
Excellent loco-regional results were achieved with acceptable acute and late toxicities. The low rate of late dysphagia was related to parotid gland sparing; we did not observe a correlation between late dysphagia and dose to pharyngeal constrictors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgery and radiotherapy, with or without chemotherapy, represent the standard treatment approach for most patients with head and neck cancers (HNC). Several studies have shown that conventional 3D conformational radiation therapy (3D-CRT) can significantly affect quality of life of head and neck cancer patients, causing acute and delayed side effects, such as xerostomia and dysphagia [1].
It has been also shown that, due to the possibility of producing concave dose distributions with better avoidance of dose-limiting structures, intensity-modulated radiotherapy (IMRT) reduces acute and late toxicity rates without compromising clinical outcome [2–10]. In particular, doses to the pharyngeal constrictors and larynx have been associated with dysphagia [11, 12], while doses to the parotid glands are correlated with xerostomia [4, 13–16]. Anatomical changes of parotid glands and target volumes are independent of the immobilisation devices utilised. Nevertheless, due to these structure variations, there is a significant risk to deliver higher or lower doses compared with the planned dose. The ability to “paint” the dose with IMRT introduces the need for more precise contouring of organs at risk (OAR) and planning target volume, due to a greater risk of missing the target compared with traditional radiation therapy techniques [17–22]. To minimise the risk of xerostomia, the parotid glands have been evaluated in terms of volumes and doses changed and several trials have stated that IMRT re-planning is mandatory in selected cases. Nevertheless, few data demonstrating a survival benefit of IMRT compared with conventional radiotherapy for HNC have been reported [23, 24]. In this paper, we report our experience and results of parotid gland and constrictor muscle sparing using step-and-shoot IMRT in patients with early and loco-regionally advanced HNC.
Materials and methods
We reviewed the records of 34 patients with primary HNC, treated between June 2008 and June 2011. Of these, 12 patients (35 %) received IMRT as definitive treatment and 22 (65 %) as post-operative treatment with or without sequential and/or concurrent chemotherapy (platinum based). Patient characteristics are shown in Table 1.
Initial evaluation included clinical and laboratory examination, computed tomography (CT) and/or magnetic resonance imaging (MRI) scans of the head and neck region and endoscopy with histological confirmation. Each patient underwent a CT scan without contrast media and with 2.5 mm slice thickness using an individual head-neck mask for patient positioning.
In the radical setting, gross tumour volume (GTV), high-risk subclinical disease (clinical target volume 1, CTV1) and low-risk subclinical disease (clinical target volume 2, CTV2) were defined on CT scan after simulation procedure. PTV1 and PTV2 were generated with an isotropic expansion of 5 mm from CTV1 and CTV2, respectively. These volumes were irradiated to a total dose of 66–70, 60–63 and 54–57 Gy, respectively, with daily fractions of 2.2, 2/2.1 and 1.8/1.9.
In the post-operative setting, two volumes of interest were identified: CTV1 including the tumour bed (primary and involved nodes) and CTV2 including elective lymphatic areas. PTV1 and PTV2 were generated with an isotropic expansion of 5 mm from CTV1 and CTV2, respectively. These volumes were irradiated to a total dose of 62–66 and 50–54 Gy, respectively, with daily fractions of 2.02/2.2 and 1.66/1.8 Gy.
OAR evaluation included the parotid glands in all patients and the constrictor muscles of the pharynx (PCs) in 18 patients (53 %). PC was outlined as a single structure for which the cranial limit was the caudal tips of the pterygoid plates and the caudal limit was the inferior border of the cricoid cartilage.
Acute and late dysphagia and xerostomia were assessed according to the RTOG/EORTC scale at 6, 12 and 24 months.
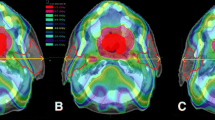
IMRT was performed with a 6 MV photon beam and step-and-shoot technique delivered with a Linac integrated MLC collimator (Primus Siemens Healthcare USA). The treatment was delivered with a 7–9 fixed field arrangement. Typical field orientations were 0°, 45°, 105°, 155°, 205°, 255°, 315° (seven field arrangement). A margin of 5–10 mm was added to the areas of interest to define the planning target volume (PTV). Treatment planning was performed on a Plato inverse treatment planning system (TPS). OAR contoured routinely, and relative dose constraints were as follows: spinal cord and brain stem with a maximum dose (D1%) of 45 and 54 Gy, respectively; larynx and parotid glands with a mean dose <50 and <26 Gy, respectively. In 18 patients, the pharyngeal constrictors were contoured, with a mean dose constraint ≤55 Gy. Pre-treatment verification was performed comparing measured versus TPS-calculated dose maps, with beam imaging system (Bis-2G) from Scanditronix Wellhofer. The measured distribution was compared with the calculated one by evaluating gamma criteria of 3 %/3 mm using a threshold of 10 %.
To assess side effects, patients were examined weekly during radiotherapy, and after treatment completion, they were seen every 3 months for the first year and every 4–6 months thereafter. Data charts, radiation therapy schedules and dose–volume histograms (DVH) of 34 patients with squamous cell carcinoma of the nasopharynx, oropharynx and larynx were evaluated.
Statistical method
Ordinal logistic regression and contingency tables with Fisher’s exact test were applied in order to analyse the correlation between acute/late dysphagia and xerostomia. The 5-year loco-regional control and overall survival probabilities were estimated using the Kaplan–Meier method. Time to recurrence and overall survival were calculated from the date of diagnosis.
Results
Planning end points were achieved for each study case: in all IMRT plans, the dose constraints reported above were respected according to the dose prescription to the PTVs. The mean dose of definitive and post-operative IMRT was 64.3 Gy (range, 62–66 Gy). A mean contralateral parotid gland dose lower than 26 Gy was achieved in 24 patients (70 %) and a dose ≥26 Gy in the remaining ten patients. The average dose to the pharyngeal constrictors was between 51.8 Gy (10 cc) and 52.86 Gy (13 cc).
The median follow-up period of the study was 43 months, with a range of 23–64 months. Acute side effects were mild, with no grade 3–4 effects registered (Table 2). Late toxicity was assessed at 6, 12 and 24 months with an actuarial incidence of G2 xerostomia and dysphagia after 2 years of 12 and 23 %, respectively.
At 24 months, late xerostomia ≥G1 was associated with a mean dose to the contralateral parotid glands ≥26 Gy (p < 0.001) (Table 3). Ordinal logistic regression analysis showed that G2 xerostomia increased the risk of late dysphagia ≥G1 at 12 months by 9.5 times (odds ratio 9.319). This effect was virtually unchanged at 24 months. The 5-year overall survival was 70 % (Fig. 1), and the local control rate was 94 %. Five patients developed distant metastasis, and two had local failure, with a median time to recurrence of 17 months. One of the patients with local recurrence was salvaged with surgery and re-irradiation, the other with exclusive irradiation with Cyberknife. Both patients are alive without evidence of disease at the last follow-up visit.
Discussion
Conventional radiation treatment reports show a high incidence of dysphagia [25, 26]. During radiation treatment, acute dysphagia begins and progressively increases: late dysphagia and aspiration are frequently reported months to years later. While acute dysphagia usually recovers rapidly after the end of treatment, late swallowing problems tend to be irreversible. IMRT can achieve an excellent dose distribution, preserving both parotid and swallowing structures with a potential improvement of quality of life. In our IMRT series, we did not observe any grade 3–4 late dysphagia, as in similar studies [4, 17, 27–29] (Table 4). Despite its limitations, our study confirms the importance of hyposalivation in determining dysphagia. Decreased saliva output causes alterations in speech and taste and difficulties with mastication and swallowing, with strong correlation with dysphagia-related quality of life [30]. Limiting mean parotid gland doses to 26–30 Gy can prevent hyposalivation [31, 32]. Several randomised studies showed that parotid sparing with IMRT reduced xerostomia and improved quality of life [4, 33, 34]. In our series, a mean parotid contralateral dose >26 Gy showed a threefold increase in the risk of xerostomia ≥G1 at 24 months.
The pharyngeal constrictors are also involved in late dysphagia. Including only the lateral retropharyngeal nodes in the target and excluding the medial ones, rarely a site of metastasis, it is possible to spare a large part of the muscle [35]. A study showed that for each additional 10 Gy after 55 Gy to the constrictor muscles, the probability of dysphagia increases by 19 % [36]. In particular, the dose to the superior constrictor was reported as the most relevant for late dysphagia [37]. In our patient series treated with IMRT, we did not observe a correlation between late dysphagia and dose to the pharyngeal constrictors. This result could be due to inter-observer variability in the delineation of OAR, as suggested by the wide range of average doses recorded for the pharyngeal constrictors. However, a limit of the present analysis is the fact that the pharyngeal constrictors were defined at planning in only 53 % of patients.
Even though a comparative analysis with another conventional technique was not available at the moment of the present evaluation, the toxicity profile of our IMRT study seems to be acceptable. Nevertheless, due to the retrospective nature of the analysis, another pitfall of our study could be the absence of a baseline systematic evaluation of symptoms. Starting from this background, we are collecting data of pre-treatment symptoms prospectively and we will report a comparative analysis, comparing also toxicity with a historical population subjected to conventional 3D-CRT.
The potential advantage of IMRT in physical dose distribution, with its tight conformality due to steep gradients, could translate into a higher risk of geographical missing. In fact, due to variations in these structures, there is a significant risk of delivering higher or lower doses compared with the planned dose. Volumes and anatomical modification of the parotid glands and target were reported as independent of the type of immobilisation system adopted. Some IMRT series reported a higher incidence of marginal failure and intra-parotideal recurrence [4, 38, 39], and one randomised study showed more in-field failures in the IMRT group compared with conventional radiation [36]. In our series, the two local recurrences occurred in field with no correlation with the attempt to spare the parotid glands or pharyngeal constrictors.
Although IMRT has been reported as the best choice to reduce toxicity, especially in terms of xerostomia, the findings of local control and outcome are still inconclusive. Keeping in mind that our study includes different cancer sites and has a short follow-up, our results are in line with other series in terms of overall survival and local control [1, 40].
Different primary tumour sites were found to be associated with different rates of both pre- and post-therapy swallowing abnormalities. The main criticism of the present report is represented by the heterogeneity of the population of study in terms of site of the primary tumour affecting dose–response relationships.
Conclusions
Acceptable rates of late dysphagia and xerostomia were achieved with optimal disease control. The severity of dysphagia is probably decreased also by reducing xerostomia through parotid gland sparing. IMRT has become the standard of care in our department for delivery of RT in head and neck cancer, reducing acute and late toxicity. Further prospective studies are needed to determine the appropriate dose constraints for other anatomical structures involved in swallowing.
References
Anand AK, Chaudhoory AR, Shukla A et al (2008) Favourable impact of intensity-modulated radiation therapy on chronic dysphagia in patients with head and neck cancer. Br J Radiol 81:865–871
Lee NY, de Arruda FF, Puri DR et al (2006) A comparison of intensity-modulated radiation therapy and concomitant boost radiotherapy in the setting of concurrent chemotherapy for locally advanced oropharyngeal carcinoma. Int J Radiat Oncol Biol Phys 66:966–974
Ricchetti F, Wu B, McNutt T et al (2011) Volumetric change of selected organs at risk during IMRT for oropharyngeal cancer. Int J Radiat Oncol Biol Phys 80:161–168
Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, Miles EA, Miah AB, Newbold K, Tanay M, Adab F, Jefferies SJ, Scrase C, Yap BK, A’Hern RP, Sydenham MA, Emson M, Hall E, PARSPORT trial management group. (2011) Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol 12:127–136
Chao KS, Deasy JO, Markman J et al (2001) A prospective study of salivary function sparing in patients with head and neck cancers receiving intensity-modulated or three-dimensional radiation therapy: initial results. Int J Radiat Oncol Biol Phys 49:907–916
Vergeer MR, Doornaert PA, Rietveld DH et al (2009) Intensity-modulated radiotherapy reduces radiation-induced morbidity and improves health-related quality of life: results of a non randomized prospective study using a standardized follow up program. Int J Radiat Oncol Biol Phys 74:1–8
Sanguineti G, Rao N, Gunn B et al (2013) Predictors of PEG dependence after IMRT ± chemotherapy for oropharyngeal cancer. Radiother Oncol 107:300–304
Kam MK, Leung SF, Zee B et al (2007) Prospective randomized study of intensity-modulated radiotherapy on salivary gland function in early-stage nasopharyngeal carcinoma patients. J Clin Oncol 25:4873–4879
Velderman L, Madani I, Hulstaert F et al (2008) Evidence behind use of intensity modulated radiotherapy. a systematic review of comparative clinical studies. Lancet Oncol 9:367–375
Marta GN, Silva V, de Andrade CH et al (2014) Intensity-modulated radiation therapy for head and neck cancer: systematic review and meta-analysis. Radiother Oncol 110:9–15
Lee N, Puri DR, Blanco AI, Chao KS (2007) Intensity-modulated radiation therapy in head and neck cancers: an update. Head Neck 29:387–400
Levendag PC, Teguh DN, Voet P et al (2007) Dysphagia disorders in patients with cancer of the oropharynx are significantly affected by the radiotherapy dose to the superior and middle constrictor muscles: a dose-effect relationship. Radiother Oncol 85:64–73
Dirix P, Nuyts S (2010) Evidence-based organ-sparing radiotherapy in head and neck cancer. Lancet Oncology 11:85–91
Tobias JS, Monson K, Gupta N, Macdougall H, Glaholm J, Hutchison I, Kadalayil L, Hackshaw A; UK Head and Neck Cancer Trialists’ Group (2010) Chemoradiotherapy for locally advanced head and neck cancer: 10-year follow-up of the UK Head and Neck (UKHAN1) trial. Lancet Oncol 11(1):66–74
Dirix P, Abbeel S, Vanstraelen B et al (2009) Dysphagia after chemoradiotherapy for head and neck squamous cell carcinoma: dose-effect relationship to the swallowings structures. Int J Radiat Oncol Biol Phys 75:385–392
Pacholke HD, Amdur RJ, Morris CG et al (2005) Late xerostomia after intensity modulated radiation versus conventional radiotherapy. Am J Clin Oncol 28:351–358
Eisbruch A, Harris J, Garden AS et al (2010) Multi-institutional trial of accelerated hypofractionated intensity-modulated radiation therapy for early-stage oropharyngeal cancer (RTOG 00-22). Int J Radiat Oncol Biol Phys 76:1333–1338
Cheung MC, Koniaris LG, Perez EA et al (2009) Impact of hospital volume on surgical outcome for head and neck cancer. Ann Surg Oncol 16:1001–1009
Eisbruch A, Marsh LH, Dawson LA et al (2004) Recurrences near base of skull after IMRT for head and neck cancer: implications for target delineation in high neck and parotid gland sparing. Int J Radiat Oncol Biol Phys 59:28–42
Cannon DM, Lee NY (2008) Recurrence in region of spared parotid gland after definitive IMRT for head and neck cancer. Int J Radiat Oncol Biol Phys 70:660–665
Grégoire V, De Neve W, Eisbruch A et al (2007) Intensity-modulated radiation therapy for head and neck carcinoma. Oncologist 12:555–564
Grégoire V, Levendag P, Ang KK et al (2003) CT-based delineation of lymph node levels and related CTVs in the node-negative neck: DAHANCA, EORTC, GORTEC, NCIC, RTOG consensus guidelines. Radiother Oncol 69:227–236
Al-Mamgani A, Van Rooij P, Tans L et al (2013) Toxicity and outcome of intensity-modulated radiotherapy versus 3-dimensional conformal radiotherapy for oropharyngeal cancer: a matched-pair analysis. Technol Cancer Res Treat 12:123–130
Fiorentino A, Caivano R, Metallo V et al (2012) Parotid gland volumetric changes during intensity-modulated radiotherapy in head and neck cancer. Br J Radiol 85:1415–1419
Smith RV, Kotz T, Beitler JJ, Wadler S (2000) Long term swallowing problems after organ preservation therapy with concomitant radiation therapy and intravenous hydroxyurea. Arch Otolaryngol Head Surg 126:384–389
Machtay M, V DI, Hershock D, Jones H, Williamson S, Greenberg MJ, Weinstein GS, Aviles VM, Chalian AA, Weber RS, Penn Cancer Center Clinical Trials Group (2002) Organ preservation therapy using induction plus concurrent chemoradiation for advanced respectable oropharyngeal carcinoma: a University of Pennsylvania phase II trial. J Clin Onc 20:3964–3971
Nguyen NP, Moltz CC, Frank C et al (2004) Dysphagia following chemoradiation for locally advanced head and neck cancer. Ann Oncol 15:383–388
Huang K, Xia P, Chuang C et al (2008) Intensity-modulated chemoradiation for treatment of stage III and IV oropharyngeal carcinoma: the University of California San Francisco experience. Cancer 113:497–507
Chen A, Lee N, Yang C et al (2010) Comparison of intensity-modulated radiotherapy using helical tomotherapy and segmental multileaf collimator-based techniques for nasopharyngeal carcinoma: dosimetric analysis incorporating quality assurance guidelines from RTOG 0225. Technol Cancer Res Treat 9:291–298
Jensen AD, Krauss J, Weichert W et al (2011) Disease control and functional outcome in three modern combined organ preserving regimens for locally advanced squamous cell carcinoma of head and neck. Radiat Oncol 6:122
De Arruda FF, Puri DR, Zhung J et al (2006) Intensity-modulated radiation therapy for the treatment of oropharyngeal carcinoma: the Memorial Sloan-Kettering Cancer Center experience. Int J Radiat Oncol Biol Phys 64:363–373
Teguh DN, Levendag PC, Noever I et al (2008) Treatment techniques and site considerations regarding dysphagia related quality of life in cancer of the oropharynx and nasopharynx. Int J Radiat Oncol Biol Phys 72:1119–1127
Fiorentino A, Cozzolino M, Caivano R et al (2013) Cone-beam computed tomography dose monitoring during intensity-modulated radiotherapy in head and neck cancer: parotid glands. Clin Transl Oncol 15:412–415
Fiorentino A, Cozzolino M, Caivano R et al (2014) Head and neck intensity-modulated radiotherapy parotid glands: time of re-planning. Radiol Med 119:201–207
Feng FY, Kim HM, Lyden TH et al (2007) Intensity-modulated radiotherapy of head and neck cancer aiming to reduce dysphagia: early dose-effect relationships for the swallowing structures. Int J Radiat Oncol Biol Phys 68:1289–1298
Levendag PC, Teguh DN, Voet P et al (2007) Dysphagia disorders in patients with cancer of the oropharynx are significantly affected by the radiotherapy dose to the superior and middle constrictor muscles: a dose-effect relationship. Radiother Oncol 85:64–73
Langendijk JA, Doornaert P, Verdonck-de Leeuw IM et al (2008) Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncology 26:3770–3776
Lee N, Xia P, Quivey JM et al (2002) Intensity modulated radiotherapy in the treatment of nasopharyngeal carcinoma: an update of the UCSF experience. Int J Radiat Oncol Biol Phys 53:12–22
Dawson LA, Anzai Y, Marsh L et al (2000) Patterns of local-regional recurrence following parotid-sparing conformal and segmental intensity-modulated radiotherapy for head and neck cancer. Int J Radiat Oncol Biol Phys 46:1117–1126
Wolden SL, Chen WC, Pfister DG et al (2006) Intensity modulated radiation therapy (IMRT) for nasopharynx cancer: update of the Memorial Sloan Kettering experience. Int J Radiat Oncol Biol Phys 64:57–62
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mazzola, R., Ferrera, G., Alongi, F. et al. Organ sparing and clinical outcome with step-and-shoot IMRT for head and neck cancer: a mono-institutional experience. Radiol med 120, 753–758 (2015). https://doi.org/10.1007/s11547-015-0512-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-015-0512-6