Abstract
Interest in transthoracic ultrasound (US) procedures increased after the availability of portable US equipment suitable for use at the patient’s bedside. It is possible to detect space-occupying lesions of the pleura, pleural effusion, focal or diffuse pleural thickening and subpleural lesions of the lung, even in emergency settings. Transthoracic US is useful as a guidance system for thoracentesis and peripheral lesion biopsy, where it minimises the occurrence of pneumothorax and haemorrhage. Transthoracic US imaging is strongly influenced by physical interaction of the ultrasonic beam at the tissue/air interface, which gives rise to reverberations classified as simple (A-line), “comet tail” and “ring down”(B-line) artifacts. Although these artifacts can be suggestive of a disease condition, they are essentially imaging errors present even in normal subjects and in empty-pleura post-pneumonectomy patients. In order to clarify some confusion and to report on the state of the art, we present a review of the literature on transthoracic US in diseases of the pleura and peripheral lung regions and our own clinical experience over 3 decades. The review focuses on quality assurance procedures and their value in diagnostic imaging and patient monitoring and warns against possible inappropriate indications and misleading information. Thoracic US is much more than “fishing for the moon in the well”.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ultrasound (US) imaging depends on the different physical interactions between ultrasonic waves and the target tissues: in transthoracic ultrasound the images are strongly influenced by the features of the chest wall and by air in the lungs. Their interference gives rise to various artifacts, and more than 95 % of the US beam is reflected by the tissue/air interface, so it is not available for further imaging [1–3]. The reverberations generated by this interaction have been classified as simple (horizontal A-line), “comet-tail” and “ring-down” (vertical B-line) artifacts, although some misunderstanding of these terms is apparent from the literature [4, 5]. Nevertheless, these artifacts all arise owing to the great difference in acoustic impedance in the pleural spaces and are visible to a certain extent when the lung is filled with air. Similar artifacts are also visible in the pneumonectomy space, which contains residual air, liquid films and/or oedema and scar tissue: this fact appears to disprove attempts to “read” such artifacts as specific disease markers [6] The US examination should always be used in conjunction with standard x-ray or CT scans of the chest and is not in itself able to provide a definitive diagnosis [7].
Methods and techniques
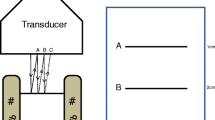
One of the main hindrances to the reproducibility of transthoracic US is the machine settings because available equipment does not provide predetermined settings for this application. This is a significant part of US knowledge skills and expertise and requires adequate comprehensive training and qualified professional certification. Before performing pleuropulmonary US, therefore, it is necessary to pre-set the machine and save the settings for subsequent examinations. Both the multifrequency 3–8 MHz convex probe and the high-frequency linear probe (8–12.5 MHz) should be pre-set. The frequency will need to be adjusted to suit the application, which means a change from 3 to 8 MHz for the convex probe, as will the probe depth, which should range from 70 to 140. Tissue harmonics are preferable, in an effort to reduce the natural artifacts, and the time gain compensation (TGC) should not exceed 55 % [8]. It is also important not to forget that the speed of US in the abdominal organs is on average 1,520 m/s, with minimal variation between organs, while in the lungs the speed falls to less than a third (450 m/s). The acoustic impedance of lung tissue is 0.0008 Rayl × 10−6, which is very different from the acoustic impedance of the abdominal organs like the liver (1.65 Rayl × 10−6) and kidney (1.62 Rayl × 10−6). This large difference in acoustic impedance at the interface between the surface tissues and air in the lung (the so-called pleural line) generates all the artifacts visible under US (simple reverberations, ring downs and comet tails). The US beam should be electronically focused on this pleural line, and similar settings should be pre-set for the high-frequency linear probe (8–12.5 MHz) [9]. No specific patient preparation is required before plain transthoracic US procedures. The examination is performed initially with the patient in a sitting position (Fig. 1), not least because this is the best posture for a patient in dyspnoea. Subsequently, whenever possible, the examination can be concluded with the patient in a supine position, so that the diaphragm can be carefully assessed. In emergency settings, however, the US examination can be performed in any position that is comfortable/safe for the patient. The thorax can be scanned from many angles. From the back, we can opt for longitudinal and transversal intercostal and paravertebral scans. From the front, in addition to the longitudinal and transversal intercostal scans, supra- and parasternal, subxyphoid and supraclavicular are all useful views. Laterally, we use the anterior, median and posterior axillary views. To improve visualisation of the structures under examination, an appropriate acoustic window needs to be used. To the right, this is supplied by the liver, while the spleen provides the window on the left. Thoracic examination must be completed with laterocervical scans, and scans of the armpit in cases where lymphadenopathy is suspected [10]. Any pathological findings must be confirmed by two perpendicular projections.
Visible anatomy, artifacts and pitfalls
The thoracic cage reduces the visible pleural surface to 70 %. This means that US is useful for viewing pleural and subpleural disease in that portion of the pleura, which corresponds to a very small part of the entire pulmonary tissue [11]. Looking from the outside of the rib cage inwards, the anatomical structures that can be examined using US are as follows: (1) the skin; (2) the subcutaneous layers; (3) the intercostal muscles and endothoracic fascia; and 4) the extrapleural fat, the parietal pleura and the visceral pleura [12].
The key anatomical findings of pleuropulmonary US in normal subjects are mainly generated by certain physical effects of US, namely imaging artifacts. For this reason the normal lung is not visible on US. The diaphragm, however, is highly visible on the right using subcostal scans at the level of the posterior face of the liver parenchyma. It is seen as a hyperechoic line made up of three separate layers, namely the liver capsule/diaphragm muscle interface (hyperechoic layer), the diaphragm muscle (hypoechoic layer) and the mirror effect artifact (hyperechoic layer).
At the pleural space, the air in the lungs reflects almost all of the US beam (more than 95 %), as there is a great difference in acoustic impedance between the soft tissues and pulmonary air at this point. This interface generates not only the so-called pleural line (Fig. 2), a visible hyperechoic (white) line that comes and goes with respiratory excursions (the gliding or sliding sign), but also reverberation artifacts (Fig. 3). These comprise simple reverberations, also known as horizontal, or A-line artifacts, and comet-tail, ring-down and vertical (B-line) artifacts [13].
Under normal conditions, with a 3.5–5 MHz convex probe, the pleural line is visible as a white band of average thickness 2 mm (range 1.4–2.6 mm). When an 8–12.5 MHz linear probe is used, the visible thickness of the pleural line is 1 mm (range 0 0.8–1.6 mm). The thickness of this line does not correspond anatomically to the parietal or visceral pleura or the pleural space, whose thickness does not exceed 300–400 μm. Indeed, a similar line is also visible, albeit fixed (without sliding or gliding sign), in the residual cavity of pneumonectomy patients. This is due to a considerable difference in impedance between the soft tissues and the postpneumonectomy cavity, which contains air and fluid [14].
In addition to these artifacts, others are generated by posterior acoustic shadowing at the dense bones of the thoracic cage (ribs, sternum and scapula) [15] and by the so-called mirror effect. Mirror effect artifacts are typically seen on right subcostal scans and arise, for example, from hepatic lesions being mirrored on the opposite side of the hyperechoic diaphragm line at the base of the lung [16].
In the normal lung, simple reverberations (horizontal or A-line artifacts) are seen as multiple hyperechoic signals of decreasing intensity parallel to the pleural line and spaced apart by a fixed period that is determined by the time between the emission and reception of the US signal.
Another type of reverberation, the ring downs (vertical or B-line artifacts), described by Avruch and Cooperberg [17], are very distinctive (and relatively easy to distinguish from comet tail artifacts). Ring downs can be seen as continuous hyperechoic stripes–parallel bands orientated along the direction of the US beam that move continuously with the excursion of the pleural line. These can be seen posterior to areas where fluid and gases are collected, for example in the bowel loops [17–19], and they have occasionally been misinterpreted as comet tails [20]. Comet-tail artifacts, initially described by Wendell and Athey [3], and subsequently by Ziskin et al. [4], are broad reverberation echoes that travel distally along the direction of propagation of the US beam. They take on a triangular shape with a distal tip and resemble the tail of a comet—hence the name. These comet tails originate at highly echoic interfaces, for example, cholesterol crystals on the anterior wall of the gallbladder, metal clips in the parenchyma and gas bubbles inside the bile duct [21–23]. In pleuropulmonary US, comet tails are also due to the presence of two contiguous tissues with a marked difference in acoustic impedance (soft tissue/pulmonary air interface), and they are found in both the normally aerated lung and in other cases where such interfaces occur, i.e., distal to pleural lesions (plaques or pleuritis exudate) or subpleural lesions of any type [23].
The number and intensity of the visible vertical artifacts (B lines) depend on the type and frequency of the probe used, as well as the degree of total gain compensation (TGC). The erroneous use of a medium-to-low frequency or excessive total gain and the lack of tissue harmonic imaging can generate a large number of such artifacts especially in pleuropulmonary US. The number of horizontal artifacts (A-line) and/or vertical artifacts (ring-downs or B-lines) is determined by the relationship between the curve of the probe used with respect to the curve of the pulmonary surface examined. The large curvatures of conventional convex probes create more horizontal reverberations with respect to the smaller curves of micro-convex or sector probes. This is another factor that influences reproducibility—the use of different probe types (convex, sectoral or linear), frequencies (2.5, 3.5, 5, 8, 10 or 12 MHz) and gain compensation. Whether tissue harmonics are or are not used can produce discrepancies, or at the very least a lack of homogeneity, between images from the same US scan [23, 24]. In-depth knowledge of US physics and artifacts enables an operator appropriately pre-set the US machine, limiting the poor reproducibility due to the use of unsuitable settings (frequency, TGC, tissue harmonic and electronic beam focusing) and/or different probes (convex, sectoral or linear). This is fundamental because several pathological conditions of the lung can cause these artifacts to increase in number and intensity. These pictures are usually strikingly different from those of the healthy lung, which features a normal ratio between air in the alveoli, quantity of liquid film (fluids, exudate), vascular circulation and pulmonary parenchyma. Hence, it is essential that we have good and accurate knowledge of the nature of these artifacts and how they appear on-screen, so that we can avoid false, and potentially detrimental interpretations [24]. Different quality of imaging is actually related to the gain level, as shown in Fig. 4a,b; In Fig. 4a, in fact, too high a gain (diagnostic pitfall) shows a homogeneously hyperechoic pleural effusion; In Fig. 4b, after the image gain has been set correctly, the fluid is seen as anechoic (correct diagnosis).
Pleural and extrapleural disease
Thoracic US is the method of choice for the assessment of pleural effusion, as the diagnosis is simple and accurate using this technique. Even small quantities of liquid can be detected, making this technique superior to standard thoracic x-ray in this respect. The effusion will show up as anechoic (black) area with distinct margins accompanied by movement deeper into the field of the pleural line. Under this, the aerated, consolidated or atelectasic lung will be visible. It is possible to quantify the degree of effusion on US by determining the longitudinal and greatest transversal dimensions of the nonechoic area. Several authors have provided formulae to calculate the volume of the effusion, or the degree of compressive atelectasis and its organisation. US also helps to establish the content of the effusion and, therefore, its nature can be diagnosed. Four characteristic effusion patterns have been described: (1) anechoic; (2) complex nonloculated; (3) complex loculated; and (4) homogeneously hyperechoic [25] (Fig. 5a–d).
Intrapulmonary effusions, often concomitant with inflammatory processes and/or various types of consolidations, are highly visible on US if they are adjacent to the pulmonary wall. Free-flowing effusion changes position with patient decubitus, distinguishing it from loculated or laminar effusion and from nonmodifiable pleural empyema [26]. Transthoracic US is particularly useful in pleural effusions, as the thoracentesis needle can be guided for risk-free diagnosis and/or treatment. It allows very small collections of fluid to be detected, even <10 ml in the costophrenic angle.
Pathological processes encroaching on the pleural space (mesothelioma or metastases) are easy to identify using US, especially if associated with pleural effusion. These are visible as hyperechoic lesions or, in certain cases, as mixed echogenic structures associated with a varying extent with pleural thickening, small discontinuities in the diaphragm and, on some occasions, invasion of the thoracic wall. In these cases, US guidance can assist in the biopsy of the lesion [27].
Local thickening of the pleural line is visible on US as an increased thickness of the pleural line (greater than >3 mm), and it is often associated with pleurisy (Fig. 6). US also enables the identification of pleural adhesions, which are visible as circumscribed hyperechoic lesions, which may on occasion be calcified [28].
In the diagnosis of pneumothorax, the negative predictive value of US reaches almost 100 %, as the presence of the sliding sign of the pleural line recognisable at B-mode US in real time and well documented by time-motion (M-mode) US excludes the possibility of this condition [29, 30]. The positive predictive value of US in the diagnosis of pneumothorax, however, is reported to vary between 55 and 90 %, because the absence of the sliding sign associated with a reduction in vertical artifacts is not a definitive clue, being also found in severe pulmonary fibrosis, fibrothorax, panlobular emphysema, in some intubated patients and those fitted with a thoracotomy drainage tube, in cancer invading the chest wall, in pleurisy sequelae and in other conditions. Furthermore, it should be taken into account that the sliding sign is scarcely visible in scans of the pulmonary apex of healthy lungs, especially in obese subjects, due to the particular anatomy of the region, namely the presence of three ligaments (transverse-pleural, costal-pleural and vertebral-pleural), which limit the visibility of the sliding sign [31, 32].
Certain extrapleural parietal lesions can also be visible in US; these include cysts, abscesses, haematomas, benign tumours, costal metastases, bacterial and tubercular osteomyelitis and tumours of the soft tissues of the thoracic cage (myelomas). Although the US images are not suitable for making a definitive diagnosis, it is possible to identify any enlargement, interruption or dislocation of the pleural line, as well as respiratory immobility. In cases of costal osteomyelitis, US can show irregularities of the ribs, as well as adjacent anechoic fluid collections. Nevertheless, in none of these cases is US alone able to provide a definitive diagnosis. This is particularly relevant in intensive care units, where chest x-ray performed at the bedside is the most widely used and valuable imaging method in the follow-up of critically ill patients [33]. Moreover, like conventional x-ray, US needs to be backed up by CT or MR imaging, in addition to, where possible, targeted US-guided targeted needle biopsy of the lesion, since greater evidence is needed both for ethical and legal considerations.
On US, fibrothorax is evidenced by a marked thickening of the pleural line, which is hypo-echoic, associated with a much reduced gliding or sliding sign [34].
Lung disease
Pathological processes of the lung can be examined by means of US when the beam is able to reach the pleura, i.e., there is no air obstructing the beam’s passage towards the lesion. For this reason lung US is only able to image peripheral pathology adjacent to the pleura, diaphragm or thoracic wall. A layer of air-containing tissue, even as thin as 0.3 cm, is sufficient to block the signal and prevent visualisation of a space-occupying lesion, even if it is very large. In all normal peripheral lung diseases, US is only able to image the lesion in cases in which the surrounding consolidated, atelectatic or effusive parenchyma provides an adequate acoustic window [34]. Pneumoconiosis, a disease caused by the accumulation of inert particles, does not present a specific or typical pattern on pleuropulmonary US. However, on occasion, when the subpleural or peripheral pulmonary regions are involved, it is possible to identify subpleural nodules, particularly in the dorsal regions at the apices in silicosis, or plaques at the periphery of the inferior lobes in asbestosis. More frequently, in various types of pneumoconiosis, it is possible to see an irregular thickening of the pleural line, especially in advanced stages of the disease [34]. Pulmonary atelectases, which are categorised as either central (caused by some kind of obstruction to the bronchial branches), or peripheral (due to compression of the lung parenchyma by effusion, pneumothorax, trauma, severe fibrosis or tumours) can easily be diagnosed using thoracic US. In cases of atelectasis, the parenchyma will be visible on US as a fairly homogeneous structure, with an echogenicity equal to or lower than that of the liver. On occasion, fluid-containing tubular structures with echogenic walls are visible inside—these are the pulmonary blood vessels and/or mucus-filled bronchi (US fluid bronchogram). Sometimes, hyperechoic spots caused by small residues of trapped air (air bronchogram) are also visible in these cases [35]. Inflammatory infiltrates, like pneumonitis, or bronchopneumonic consolidation are visible on US when they involve the peripheral zones [36]. The sonographic picture of bronchopneumonia densities is characterised by the presence of a hypoechoic/echo-free area, which may be mixed hypo/hyper-echogenic, with ill-defined borders. Hyperechoic stripes or spots—the air-filled bronchi (US air bronchogram)—and/or hypoechoic/echo-free tubular structures—trapped blood vessels or oedematous bronchi (US fluid bronchogram)–can be seen as well. It is sometimes associated with concurrent basal pleural effusion [37]. There is no specific pattern that distinguishes inflammatory density from other conditions (e.g., neoplasms). That being said, US is useful after the diagnosis, in the follow-up of pulmonary densities undergoing treatment, as it enables their healing/regression to be monitored [38]. Also in children, as in adults, after a preliminary and mandatory chest x-ray diagnosis, necessary to avoid misleading understatements or clinical decisions, thoracic US should monitor subpleural pneumonitis consolidation and the response to therapy. In this context it is a suitable and repeatable alternative to other laboratory measurements and to further radiation exposure of children.
Echo-free lesions, which are usually well circumscribed, could also be generated by malformation, bronchogenic or pleural cysts, or cysts caused by parasites, or, very rarely, sterile pulmonary infarcts. Visible echoes inside echo-free cysts may indicate complex lesions like abscesses, haematomas, necrotic neoplasms, or multilocular hydatid cysts. Pulmonary abscesses, which appear as circumscribed, fluid filled and corpuscular lesions, are only visible on US when they are peripherally located and in contact with the pleuroparietal surface. These are often associated with pleural adhesion [39]. Solid lesions, which typically present slightly irregular margins and varying degrees of hypoechogenicity and uniformity, without a particular structure are, generally speaking, typical of neoplastic masses, although these may also present as either hyperechoic, or hypoechoic/echo-free (in liquefactive necrosis). In lung carcinoma, it is possible to see areas of air and/or fluid bronchogram, like those found in inflammatory consolidation [40]. Any subpleural lesion identified on US must necessarily be confirmed by radiological techniques like computed tomography (CT), positron emission tomography (PET)-CT or magnetic resonance imaging (MRI), as there is no definitive diagnostic US pattern. In fact, even the use of colour Doppler inside the lesion, as well as being impeded by the presence of movement artifacts (flash artifacts) is unable to accurately distinguish between neoplastic and non-neoplastic disease [41]. On thoracic US, 70 % of the pleural surface is accessible or reachable via an acoustic window. Contrast-enhanced US (CEUS) provides further information in this regard. In a comparison of 204 lung cancer versus 193 pneumonitis lung consolidations, all the lung cancers presented intralesional enhancement consistent with tumour neovascularisation. In some cases, there were unenhanced areas consistent with zones of necrosis and these areas were avoided during fine-needle aspiration biopsy (FNAB) [42]. Lung cancers have a different behaviour when challenged by CEUS and the CEUS pattern is different from that of inflammatory conditions, such as pneumonitis. Differences are significant both as averages and using the most current conventional cut-off for the appearance of nodule enhancement, which is <10 s for the so-called early enhancement. Actually, among all the lung cancers, only small-cell carcinoma has a more distinctive pattern, with very early image enhancement and quite early enhancement disappearance, in comparison both with the other cancer histotypes and pneumonitis, so that this information cannot have a practical use. This criterion cannot be recommended within the work-up of patients who are to be diagnosed by biopsy and histology with the greatest possible level of confidence. Histological diagnosis is a prerequisite for any further diagnostic and therapeutic approach. Nonetheless, we find it easier to reach a small lung nodule after having accurately defined its position and US features by CEUS. Pitfalls in the diagnosis of lung nodules are related also to the “quality” of the specimen, which is the consequence of several factors. One of them is identification of the exact location and the direct guidance of the needle under the eyes of the physician. The most reliable biopsy-adapted probes have a central hole through which the biopsy set is introduced and that is followed all the time in its path with an image exactly perpendicular to the target and to the transducer, linear array or convex. Skipping necrotic areas is a useful information which is provided by CEUS, which enables the choice of the most suitable point(s). Thoracic US elastography is a novel approach useful to estimate the stiffness/elasticity of tissues, allowing a reliable preliminary differentiation with noncancer consolidation. It is followed by a focused and guided FNAB procedure for diagnosing and staging lung cancer. Thoracic US with elastography and FNAB after chest x-ray and CT scan were performed in 91 patients (67 men, 24 women; age, 62.84 ± 7.51 years) with lung consolidation. All of the lung cancer patients (n = 67) had significantly (p < 0.0001) lower elasticity of nodules (4.19 ± 0.55) versus pneumonitis (2.35 ± 0.48); the size of the densities was greater in pneumonitis (4.03 ± 0.82 cm versus 3.06 ± 0.88; p < 0.0001), and this is a further argument against the use of nodule size as a clue for the diagnosis [43]. Both US approaches, even though not yet widely validated could contribute to a more efficient work-up, at least in some patients. Both provide diagnostically useful information on peripheral lung lesions and increase the diagnostic yield of transthoracic FNAB by reducing the risk of inadequate tissue sampling.
Thoracic US is not suitable for formulating hypotheses based on conjecturally specific clues that are, however, confusing when functional-pathological diagnostic patterns do not exist. Theories put forward on the basis of signs allegedly visible in pulmonary interstitial disease (acute pulmonary oedema) seem to be difficult to demonstrate and their results are not reproducible. These theories postulated that in the presence of more than six or seven “vertical” artifacts described as “comet tail” (but in actual fact ring-downs or B-lines) per intercostal space, this pattern could enable distinction between acute pulmonary oedema from other diffuse lung disease (for example, acute phase obstructive bronchopneumopathy). Although frequently reported in the literature, this theory has never received unanimous consensus or solid support. In fact, the idea that a subjective visual count of the number of wandering artifacts can be pathognomonic of any one type of lung disease is, to say the least, scientifically weak and open to doubt [44, 45]. First, one must ask how a method like US, which only visualises a small part of the pulmonary parenchyma could ever enable assessment of diffuse lung diseases. Furthermore, artifacts are in essence imaging errors, dependent on a variety of factors and could not alone be a pathognomonic pattern of a single disease state. In fact, an increase in the number of ring-downs and B-lines per intercostal space is generated every time the US beam is intercepted by an excessive quantity of air and liquid film or exudate or by the presence of fibrosis in the pleural space. This condition is a feature of many diffuse lung and interstitial diseases of various nature, like pulmonary fibrosis, acute exacerbation of chronic obstructive pulmonary disease (COPD), acute bronchial asthma, uniformly distributed pleural effusion and lymphangitis and cannot, therefore, be considered pathognomonic of a particular disease state (acute pulmonary oedema). Moreover, this clinical condition has been studied and reported in the literature [44–46], and no statistical significance has been attributed to such artifacts in the “wet” lung of patients affected by acute pulmonary oedema, with respect to those affected by other pleuropulmonary diseases (acute exacerbations of COPD, carcinomatous lymphangitis, acute bronchial asthma, pleural effusions and/or chronic cardiac decompensation). The added value to a best-practice physical examination is, at least, disputable [45]. The comparison of the actual number of such artifacts versus normal subjects and/or pneumonectomy patients has demonstrated that while there is a statistically significant difference between patients with diffuse pulmonary diseases and normal subjects, there is no statistically significant difference in the number of ring-downs (B-lines) between patients with acute pulmonary oedema and those affected by other pleuropulmonary diseases [46] (Fig. 7a–c). The need for procedure standardisation is obvious: overall B-line measurements or score, as defined and used by some authors, is only a synthetic personal measure of wandering artifacts [47]. Although paved with good intentions such studies fail to reach their goal, i.e., lung water measurement, a frail methodological basis and weak data can lead to deceptive conclusions, like “fishing for the moon in the well”.
US-guided interventions
The earlier experiences with US-guided transthoracic puncture of the pleura or pericardium are reported in haemopericardium when emergency intervention was needed for preventing cardiac tamponade and when the subxyphoid approach is less suitable [48]. US can be used to guide the thoracentesis needle to the most significant and copious area of the effusion to avoid the risk of pneumothorax during lung drainage (Fig. 8). As written above, linear-array or convex probes with a central hole are most suitable for FNAB: both allow a biopsy needle or a therapy probe to be inserted through the centre of the transducer. The needle, therefore, enters in the centre of the image, perpendicular to the lesion, facilitating difficult procedures like intercostal biopsies. This provides visualisation of the needle beginning at the skin line and allows difficult biopsies to be performed with instant feedback on the precise location of the needle tip. Furthermore, US enables determination of the type of effusion (simple, loculated or laminar) and better characterisation of the opaque areas visible on chest x-ray (for example, to distinguish between effusion and the opaque base of pulmonary consolidation). The international literature reports a percentage of pneumothorax in unassisted thoracenteses as between 7 and 16 %, which falls to 0.5 % when US guidance is used. In our 10-year experience, comprising 2,850 consecutive US-assisted drainage procedures (diagnostic and therapeutic), it was possible to obtain a diagnosis of neoplastic effusion in 228 patients (8 %) through cytological testing and the identification of neoplastic cells in the drainage fluid. In this sample, the rate of major complications such as pneumothorax was 0.11 % (three patients, two of whom suffered minimal pneumothorax and another, a subtotal pneumothorax—both resolving spontaneously) [49].
Ultrasound is also very useful in the emergency department, where it can be used to confirm the clinical suspicion of massive pleural effusion in cases of acute respiratory disease and guide its drainage to reduce the risk of pneumothorax to almost zero. This operation can be quickly performed with a low-flow, low-pressure aspirator and a small-calibre needle (20G). This setup enables drainage of massive effusions to be performed in a relatively short time in the critical patient [50].
Pleural lesions in which US-guided transparietal needle biopsy can be useful are nodular pleural thickening, which appear as micronodular hypoechoic structures, often associated with thickening of the pleural line. Pleural mesothelioma which appears as a mixed hyperechoic lesion is very often associated with ipsilateral serosanguinous effusion [51].
It is rare to find benign lesions like fibroma or lipoma. All pulmonary lesions visible on US can be aspirated using 20–21G cutting/aspirating needles. Bronchopneumonic densities or pneumonitis, especially in immunodepressed patients, whose origin is undetermined by the usual battery of tests (sputum material, other effusions, blood culture, serum and urine tests), may need to be identified through US-guided FNAB (22G) [52, 53].
In cases of pleural empyema, US-guided drainage is a fundamental procedure, and in lung cancer US-guided needle biopsy allows a diagnostic accuracy of 85–96 %, depending on the tumour. In our experience, the diagnostic accuracy of US-guided transparietal needle lung biopsy is 96 % in a sample of 800 peripheral lung tumour patients (Fig. 9). The complication rate for this procedure was 0.2 % (one case of spontaneously healed partial pneumothorax and one case of total pneumothorax treated by drainage tube) [49].
Conclusions
Despite some confusion, enthusiasm and overstatements in the current medical literature and the advent of more advanced imaging systems, transthoracic US is a valuable diagnostic/treatment tool in pleuropulmonary imaging and interventional medicine. As in any imaging-related procedure, adequate knowledge and skills should be acquired through certified training and the use of accurate up-to-date equipment and settings. It must be stressed that transthoracic US is a complementary diagnostic technique, mostly useful in screening and monitoring. Most pleural and subpleural lesions identified on transthoracic US need to be confirmed by radiological procedures like CT, PET-CT or MRI. Currently, there is no distinctive and exclusive diagnostic US pattern for any anatomical or functional lung disease.
References
Dunn F, Fry WJ (1961) Ultrasonic absorption and reflection by lung tissue. Phys Med Biol 5:401–410
Dunn F (1974) Attenuation and speed of ultrasound in lung. J Acoust Soc Am 56:1638–1639
Ziskin MC (1993) Fundamental physics of ultrasound and its propagation in tissue. Radiographics 13:705–709
Ziskin MC, Thickman DI, Goldenberg NJ et al (1982) The comet tail artifact. J Ultrasound Med 1:1–7
Lee RK (2005) Grayscale ultrasound artifacts. In: Dogra V, Rubens DJ (eds) Ultrasound secrets. Elseiver, Philadelphia, pp 8–13
Bamber JC (1986) Attenuation, and absorption. In: Hill CR (ed) Physical principles of medical ultrasonic. Ellis Horwood Ltd., Chichester, pp 135–138
Beckh S, Bolcskei PL, Lessnau KD (2002) Real time chest ultrasonography: a comprehensive review for the pneumologist. Chest 122:1759–1773
Mathis G (1997) Thorax sonography—part I: chest wall and pleura. Ultrasound Med Biol 23:1131–1139
Dietrich CF, Hirche TO, Schreiber D, Wagner TO (2003) Sonographie von pleura and lunge. Ultraschall Med 24:303–311
Herthj FJ, Becker HD (2003) Transthoracic ultrasound. Respiration 70:87–94
Reissig A, Görg C, Mathis G (2009) Transthoracic sonography in the diagnosis of pulmonary diseases: a systematic approach. Ultraschall Med 30:438–454
Sagar KB, Rhyne TL, Myers GS, Lees RS (1978) Characterization of normal and abnormal pulmonary surface by reflected ultrasound. Chest 74:29–33
Reuter KL, Bogdan A (2009) Physics of diagnostic ultrasound creating the image. In: Bolliger CT, Herth FJF, Mayo PH, Miyazawa T, Beamis JF (eds) Clinical chest ultrasound: from the ICU to the bronchoscopy suite. Prog Respir Res. Basel, Karger, vol 37, pp 2–10
Sperandeo M, Varriale A, Sperandeo G et al (2011) Characterization of the normal pulmonary surface and pneumonectomy space by reflected ultrasound. J Ultrasound 14:22–27
Scanlan K (1991) Sonographic artifacts and their origin. Am J Roentgenol 156:1267–1272
Gustavson S, Olin JW (2006) Image in vascular medicine mirror image artifact. Vasc Med 11:175–176
Avruch L, Cooperberg PL (1985) The ring-down artifact. J Ultrasound Med 4:21–28
Targhetta R, Chavagneux R, Bourgeois JM et al (1992) Sonographic approach to diagnosing pulmonary consolidation. J Ultrasound Med 11:667–672
Wilson S, Burns PN, Wilkinson LM et al (1999) Gas at abdominal US: appearance, relevance, and analysis of artifacts. Radiology 210:113–123
Pedersen PC, Ozcan HS (1986) Ultrasound properties of lung tissue and their measurements. Ultrasound Med Biol 12:483–499
Kremkau FW (2006) Diagnostic ultrasound. Principles and instruments, 7th edn. Saunders/Elsevier, Missouri, pp 263–265
Lim JH, Lee KS, Kim TS, Chung MP (1999) Ring-down artifacts posterior to the right hemidiaphragm on abdominal sonography: sign of pulmonary parenchymal abnormalities. J Ultrasound Med 18:403–410
Shapiro RS, Winsberg F (1990) Comet-tail artifact from cholesterol crystals: observations in the postlithotripsy gallbladder and an in vitro model. Radiology 177:153–156
Sperandeo M, Carnevale V, Varriale A (2010) Response to pleuropulmonary US examination artifacts: “errors in images”. Ultrasound Med Biol 36:357
Yang PC, Luh KT, Chang DB et al (1992) Value of sonography in determining the nature of pleura effusion: analysis of 320 cases. Am J Roentgenol 159:29–33
Eibemberger KI, Wolfgang ID, Anman ME et al (1994) Quantification of pleural effusion: sonography versus radiography. Radiology 191:681–684
Cardinale L, Ardissone F, Asteggiano F et al (2013) Diffuse neoplasms of the pleural serosa. Radiol Med 118:366–378
Yu CJ, Yang PC, Chang DB et al (1992) Diagnostic and therapeutic use of chest sonography; value in critically ill patients. Am J Roentgenol 159:695–701
Kirkpatric AW, Ng AK, Dulchavsky SA et al (2001) Sonographic diagnosis of a pneumothorax inapparent on plain radiography: confirmation by computed tomography. J Trauma 50:750–752
Targhetta R, Bourgeois JM, Chavagneux R, Balmes P (1992) Diagnosis of pneumothorax by ultrasound immediately after ultrasonically guided aspiration biopsy. Chest 101:855–856
Muller NL (1993) Imaging of the pleura. Radiology 186:297–309
Doust B, Baum JK, Doust VL (1975) Ultrasonic evaluation of pleural opacities. Radiology 114:135–140
Palazzetti V, Gasparri E, Gambini C et al (2013) Chest radiography in intensive care: an irreplaceable survey? Radiol Med 118:744–751
Mathis G (1997) Thorax sonography—part II: peripheral pulmonary consolidation. Ultrasound Med Biol 23:1141–1153
Yang PC, Luh KT, Wu HD (1990) Lung tumors associated with obstructive pneumonitis: US studies. Radiology 174:717–720
Sperandeo M, Varriale A, Sperandeo G et al (2009) Transthoracic ultrasound in the evaluation of pulmonary fibrosis: our experience. Ultrasound Med Biol 35:723–729
Bolliger CT, Herth FJF, Mayo PH et al (2009) Clinical chest ultrasound: from the ICU to the bronchoscopy suite. Karger, Basel
Sperandeo M, Carnevale V, Muscarella S et al (2011) Clinical application of transthoracic ultrasonography in inpatients with pneumonia. Eur J Clin Invest 41:1–7
Sconfienza LM, Mauri G, Grossi F et al (2013) Pleural and peripheral lung lesions: comparison of US- and CT-guided biopsy. Radiology 266:930–935
Fraioli F, Serra Liberali S et al (2011) Clinical application of dual-source CT in the evaluation of patients with lung cancer: correlation with perfusion scintigraphy and pulmonary function tests. Radiol Med 116:842–857
Wang HC, Yu CJ, Chang DB et al (1995) Transthoracic needle biopsy of thoracic tumours by a colour Doppler ultrasound puncture guiding device. Thorax 50:1258–1263
Sperandeo M, Sperandeo G, Varriale A et al (2006) Contrast-enhanced ultrasound (CEUS) for the study of peripheral lung lesions: a preliminary study. Ultrasound Med Biol 32(10):1467–1472
Trovato GM, Sperandeo M, Catalano D (2013) Computed tomography screening for lung cancer. Ann Intern Med 159:155
Sperandeo M, Varriale A, Sperandeo G et al (2012) Assessment of ultrasound acoustic artifacts in patients with acute dyspnea: a multicenter study. Acta Radiol 53:885–892
Trovato GM, Rollo VC, Martines GF et al (2013) Thoracic ultrasound in the differential diagnosis of severe dyspnea: a reappraisal. Int J Cardiol 167:1081–1083
Trovato GM, Sperandeo M (2013) Sounds, ultrasounds, and artifacts: which clinical role for lung imaging? Am J Respir Crit Care Med 187:780–781
Trovato GM, Catalano D, Martines GF, Sperandeo M (2013) Is it time to measure lung water by ultrasound? Intensive Care Med 39:1662
Di Marco V, Ginardi V, Mazzone O, Trovato GM (1980) Acute pericarditis treatment during maintenance hemodialysis. G Ital Cardiol 10:79–83
Sperandeo M, Filabozzi P, Varriale A et al (2008) Role of thoracic ultrasound in the assessment of pleural and pulmonary diseases. J Ultrasound 11:39–46
Cervi PM, Trevisani L, Zucchi F (1990) Echo-guided biopsy in peripheral pulmonary lesions. Our experience. Radiol Med 80:445–450
Liao WY, Chen MZ, Chang YL et al (2000) US guided transthoracic cutting biopsy for peripheral thoracic lesions less than 3 cm in diameter. Radiology 217:685–691
Sheth S, Hamper UM, Stanley DB et al (1999) US guidance for thoracic biopsy: a valuable alternative to CT. Radiology 210:721–726
Yang PC (2000) Ultrasound-guided transthoracic biopsy of the chest. Radiol Clin North Am 38:323–343
Conflict of interest
Marco Sperandeo, Antonio Rotondo, Giuseppe Guglielmi, Daniela Catalano, Beatrice Feragalli, and Guglielmo M. Trovato declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Key points of transthoracic ultrasound (TUS)
Context
-
Wider dissemination of competence in noninvasive diagnostic procedures for outpatient clinic, elective, emergency and intensive medicine
-
Benefits of imaging assistance for safer invasive procedures.
Contribution
-
US is primarily and almost exclusively an imaging technology: the quality requisites are the greatest possible correspondence and, hopefully, a good overlap with the real anatomy, reproducibility of methods and reliable predictivity.
-
In echocardiography, vascular US (both involving Doppler techniques), elastography and CEUS imaging is linked with physical measurements which, by association and relationship, rely on actual morphology and function.
-
TUS is a significant part of US knowledge skills and expertise and requires adequate comprehensive training and professional qualified certification.
-
The invasive US-guided procedures are diagnostic FNAB, useful also for lung and mediastinal nodes, therapeutic procedures, such as US-assisted puncture of liquid cavities (pleural, pericardial, cystic, others) or intervention therapy, such as ablations, scarcely used for lungs.
-
Reliable and affordable noninvasive procedures, such as TUS, must be appropriately used concurrently.
Caution
-
Noninvasive TUS has a good safety level.
-
TUS does not allow for time-wasting procedures or uncomfortable patient positioning: both can be even harmful and distress the patients.
-
Invasive US-guided procedures are safer when provided by expert and appropriately trained specialists with adequate equipment within well-articulated facilities.
Implications
-
Studies claiming advantages from any TUS procedure are meaningless and should not be considered within any evidence-based medicine report if the methodology is unreliable and there is no robust analysis of predictivity.
-
The cost-benefit ratio depends mostly on the actual expertise of the operators.
-
Clinical expertise in the specific field of medicine and knowledge and skills acquired by adequate preliminary and ongoing training are the conditions for achieving satisfactory information and beneficial outcomes.
Rights and permissions
About this article
Cite this article
Sperandeo, M., Rotondo, A., Guglielmi, G. et al. Transthoracic ultrasound in the assessment of pleural and pulmonary diseases: use and limitations. Radiol med 119, 729–740 (2014). https://doi.org/10.1007/s11547-014-0385-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-014-0385-0