Abstract
The rapid increase in fentanyl overdose deaths, particularly those also attributed to stimulants, has led to concerns about unintentional fentanyl exposure. Utilizing vital and medical record data, we identified overdose decedents from 2018 to 2021 in San Francisco who received care in the safety net system in the 3 years preceding death. Among 506 decedents, medical record evidence of pre-mortem opioid use was present for 48% of stimulant-only, 56% of stimulant-fentanyl, 65% of fentanyl-only, and 82% of non-fentanyl opioid decedents (p<0.001). Among stimulant-fentanyl decedents, an increase in 10 years of age (adjusted odds ratio (aOR) 0.74 [95% CI:0.59–0.94]) and race other than White or Black (aOR 0.36 [95% CI:0.15–0.87]) had lower odds of evidence of pre-mortem opioid use. While not conclusive, these findings raise the possibility that a significant proportion of fentanyl overdose decedents in San Francisco may have not intended to consume an opioid on the occasion of their death.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The fourth wave of the overdose crisis includes deaths driven by fentanyl and a surge in cases involving cocaine and methamphetamine [1]. The combination of fentanyl and stimulants accounts for the largest plurality of deaths [2], raising several possibilities. Co-use of stimulants and opioids is a longstanding phenomenon, with, for example, 45% of cocaine or heroin overdose deaths in New York City in the 1990s due to both drugs [3]. More recently, many people who use fentanyl also use stimulants in order to stay awake, complete daily activities, and remain safe [4]. Thus, intentional fentanyl use may explain the increase in stimulant-fentanyl mortality.
Fentanyl marketing characteristics are different from other opioids. In the eastern USA and Canada, fentanyl is often mixed with powder heroin, creating a complex blend of street opioids [4]. In the western USA, heroin is sold as black tar and rarely mixed with fentanyl [4]. Therefore, most people intending to use heroin in the western USA are believed to be aware when they use fentanyl because the appearance is distinct. However, among persons intending to use stimulants, there have been cases of unintentional fentanyl ingestion [5]. Some investigators have suggested that fentanyl is added to stimulants [6]; a drug checking study in British Columbia found that 5.9% of drug samples presumed to be methamphetamine contained fentanyl [7], a small proportion but potentially enough to cause substantial mortality. Moreover, the appearance of fentanyl, similar to that of methamphetamine or cocaine, could lead consumers to mistake one product for another.
Based on anecdotal community reports, we assumed that most stimulant-fentanyl decedents in San Francisco had intended to use an opioid. To explore this assumption, we sought evidence of pre-mortem opioid use from medical records. Prior research found 85% of opioid overdose decedents to have medical record evidence of problematic use [8], suggesting that such evidence of pre-mortem opioid use may be a reasonable, albeit imperfect, proxy for intentional opioid use at the time of death. We expected to find the proportion of fentanyl overdose decedents and other opioid decedents with evidence of pre-mortem opioid use to be similar, regardless of the involvement of stimulants.
Materials and Methods
Procedures
We utilized data collected by the San Francisco Department of Public Health to evaluate drug overdose death. We included certified deaths from January 1, 2018 to November 4, 2021, attributed by the medical examiner to acute toxicity from cocaine, methamphetamine, fentanyl, or other opioids, excluding those involving fentanyl with other opioids, as well as suicides and homicides. Only cases that had received primary outpatient or acute inpatient medical care in the safety net healthcare system in the 3 years preceding death were included in the analysis, because medical record data were not available for other decedents. We reviewed 3 years of clinical records to increase sensitivity, given that some persons may seek care intermittently, without sacrificing too much specificity with regard to recent opioid use. Staff collecting medical record data were not aware of cause of death.
Measurements
Vital record data included demographics as determined by the medical examiner (i.e., age, sex, race, and ethnicity), and causes of death. We categorized causes of death as acute toxicity due to cocaine, methamphetamine, fentanyl, or another opioid. After initial review, we simplified the categories into stimulants without opioids (stimulant-only), stimulants with fentanyl but not other opioids (stimulant-fentanyl), fentanyl without stimulants or other opioids (fentanyl-only), and other opioids without fentanyl (non-fentanyl opioids). We also identified involvement of benzodiazepines or alcohol in death.
Medical record data for decedents included race when missing from vital records, as well as the following from the 3 years preceding death: (1) opioid-related diagnosis; (2) mention of opioid use in a provider note; (3) opioid prescription; and (4) opioid-positive urine drug screen. These data were collected by manual review and using the Epic search function with the phrase: “fentanyl OR opioid OR opiate OR heroin OR dilaudid OR hydrocodone OR oxycodone OR tramadol OR methadone OR morphine OR vicodin OR oxycontin OR percocet OR norco OR hydromorphone OR oxymorphone OR buprenorphine OR codeine OR mscontin OR lortab OR kadian OR roxicodone OR opana OR suboxone.”
Our primary outcome was a binary composite outcome of any evidence of opioid use, including opioid-related diagnosis, provider note mention of opioids, opioid prescription, or opioid-positive urine drug screen.
Statistical Analysis
We described the demographics of all decedents by causal drugs, then restricted the sample to those with primary outpatient or acute inpatient medical care in the 3 years preceding death. We compared the outcome (evidence of pre-mortem opioid use) by whether decedents were included in the sample based on primary care or only inpatient data. We also compared deaths due to combinations of cocaine or methamphetamine to determine if the outcome was sufficiently similar to merge those two substances into a single “stimulant” category. Since age was skewed across measures, we presented medians with interquartile ranges (IQRs) and compared age across categories using Kruskal-Wallis tests. We presented proportions for categorical variables and compared them across categories using Pearson chi-square tests and Fisher’s exact tests for expected cell counts less than 5. We also presented the proportion of decedents by demographic characteristics and causal drug category for whom evidence of pre-mortem opioid use was found.
We conducted a multivariable logistic regression analysis to determine demographic predictors of evidence of pre-mortem opioid use among stimulant-fentanyl deaths, as well as all fentanyl deaths. We rescaled age to an increase of 10 years in the regression analysis. Analysis was conducted using Stata 14.2. P-values <0.05 were considered statistically significant. This analysis was determined exempt by the University of California San Francisco Institutional Review Board (IRB#21-35068).
Results
All Decedents
Of 1294 cases, 506 (39%) had received care in the safety net system in the 3 years preceding death. Decedents who had received care in the safety net system were significantly different from others: they were older, a larger proportion were female or Black/African American, and smaller proportions were Hispanic/Latinx or White or died from fentanyl-only (see Appendix Table 2 for additional details).
Decedents with Safety Net Care
Decedents who had received safety net primary care (n=182, 36%) were older (54 vs 52 years old, p=0.04) and died from different drugs compared to those who had only received inpatient care (p<0.001). Slightly less than half of stimulant-fentanyl and fentanyl-only decedents, and approximately one-quarter of stimulant-only and non-fentanyl opioids decedents, had primary care data in the 3 years preceding death. There was no difference between these groups in evidence of pre-mortem opioid use (p=0.66). Evidence of pre-mortem opioid use was also similar when comparing subcategories of deaths due to cocaine and methamphetamine, thus those drugs were combined as “stimulants” (see Appendix Table 3).
Among all decedents with safety net care, median age was 53 (43–60) years, although fentanyl-only decedents were significantly younger (fentanyl median age 40 [34–59] years, all others median age 53 [44–60] years, p=0.013). Other demographic characteristics were similar among drug categories (see Table 1). The proportion of deaths involving benzodiazepines was significantly lower among stimulant-only and stimulant-fentanyl deaths, compared to fentanyl-only and non-fentanyl opioid deaths; there was no difference with regard to involvement of alcohol.
Among non-fentanyl opioid decedents, 82% had evidence of pre-mortem opioid use, compared to 65% among fentanyl-only decedents, 56% among stimulant-fentanyl decedents, and 48% among stimulant-only decedents (p<.001) (see Table 1 and Appendix Tables 3 and 4). Among all fentanyl decedents, 57% had evidence of pre-mortem opioid use. The mention of opioid use in a note was the most sensitive marker for pre-mortem evidence of opioid use. The mention of opioid use in a note and the presence of an opioid-related diagnosis both differed by drug category, in the same direction as the composite outcome. There were no significant differences by drug category for opioid prescriptions or opioid-positive urine drug screens.
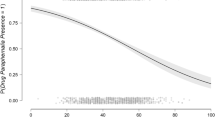
Evidence of pre-mortem opioid use was significantly different by age across drug categories (p<0.001; see Appendix Table 6). Moreover, while evidence of pre-mortem opioid use was more common among older non-fentanyl opioid decedents, it was more common among younger stimulant-fentanyl decedents.
On multivariate analysis among stimulant-fentanyl decedents (see Appendix Table 7), older decedents had lower odds of evidence of pre-mortem opioid use (aOR for an increase of 10 years of age 0.74 [0.59–0.94], p=0.013). In addition, stimulant-fentanyl decedents of race other than White or Black had lower odds of evidence of pre-mortem opioid use (aOR 0.36 [0.15–0.87], p=0.023), compared to White decedents. Among stimulant-fentanyl decedents with evidence of premortem opioid use, the Other race category consisted of Asian (46%), Native American (7%), and Other/Multiracial (46%) decedents, with similar proportions among those without evidence of opioid use. Benzodiazepines were not included in the model because all decedents whose death involved benzodiazepines also had evidence of pre-mortem opioid use. Results of the multivariate analysis were unchanged when applied to all fentanyl deaths (see Appendix Table 8)
Discussion
Among patients in a safety net healthcare system in San Francisco, 82% of non-fentanyl opioid overdose decedents had evidence of pre-mortem opioid use in the 3 years preceding death, compared to only 57% of fentanyl overdose decedents. This difference was most pronounced among stimulant-fentanyl decedents. These findings conflict with our a priori assumption and suggest that fentanyl overdose deaths among people without a known history of opioid use may be more common than previously believed.
Evidence of pre-mortem opioid use was common among all decedents. About half of stimulant-only decedents had evidence of pre-mortem opioid use, with little variation by demographics, suggesting a significant rate of opioid use even among decedents whose deaths were not attributed to opioids. About four-fifths of non-fentanyl opioid decedents had evidence of pre-mortem opioid use, again with little variation by demographics or involvement of stimulants in death. In contrast, evidence of pre-mortem opioid use varied by age and race for all fentanyl decedents. In fact, among stimulant-fentanyl decedents, older age was independently associated with no evidence of pre-mortem opioid use. This finding is unlikely to be explained by the sampling framework of decedents who had received safety net care, as older decedents should have more well-documented medical histories. Instead, these results suggest that older persons who use drugs may be at particularly high risk for fentanyl overdose death due to unintentional or recent onset use.
If additional investigations confirm that a substantial proportion of fentanyl decedents were not intending to use an opioid at the time of their death, overdose prevention messaging and outreach efforts would need to be significantly altered to focus more directly on people who use non-opioid drugs. Aggressive promotion of naloxone for people who use non-opioid drugs should be considered. Public health authorities might also consider, for example, emphasizing drug checking interventions, including fentanyl test strips that overcome problematic false positive results, as well as mass spectroscopy and related programs to track the prevalence of different substances in the drug supply.
Limitations
There are several limitations to this hypothesis-generating study. First, we relied upon data from clinical care, which may be incomplete. In addition, only a small number of deaths were due to fentanyl only, limiting the ability to interpret that category of results. Furthermore, clinical data of pre-mortem opioid use does not confirm intentional use of fentanyl on the day of death. Fentanyl use may have been initiated recently and thus not detected clinically. Moreover, fentanyl is often smoked in San Francisco, which may not be as clinically apparent due to fewer injection-related complications [9]. Nonetheless, the close concordance of our findings with previous findings that 85% of overdose decedents had evidence of problematic use [8] suggests some generalizability to these results. Finally, the results of a similar analysis may have different implications in a region, such as the eastern USA, where fentanyl and other opioids are indistinguishable and commonly mixed.
Conclusions
In this exploratory study, we found significantly less evidence of pre-mortem opioid use in the medical records of people who died from acute fentanyl toxicity, compared to other opioid toxicity, in San Francisco. These findings heighten the urgency to definitively establish the proportion of persons who died from fentanyl overdose who were not intending to use an opioid at all.
References
Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and geographic patterns in drug and synthetic opioid overdose deaths - United States, 2013-2019. MMWR Morb Mortal Wkly Rep 2021;70(6):202–7.
Centers for Disease Control and Prevention. National Center for Health Statistics Mortality Data on CDC Wonder. Available at: https://wonder.cdc.gov/mcd.html. Published 2021. Accessed 2 Oct 2021.
Coffin PO, Galea S, Ahern J, Leon AC, Vlahov D, Tardiff K. Opiates, cocaine and alcohol combinations in accidental drug overdose deaths in New York City, 1990-98. Addiction 2003;98(6):739–47.
Ciccarone D. The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Curr Opin Psychiatry. 2021;34(4):344–50.
Centers for Disease Control and Prevention. Rising Numbers of Deaths Involving Fentanyl and Fentanyl Analogs, Including Carfentanil, and Increased Usage and Mixing with Non-opioids. Available at: https://emergency.cdc.gov/han/HAN00413.asp. Published 2018. Accessed 4 Dec 2021.
Nolan ML, Shamasunder S, Colon-Berezin C, Kunins HV, Paone D. Increased presence of fentanyl in cocaine-involved fatal overdoses: implications for prevention. J Urban Health 2019;96(1):49–54.
Tupper KW, McCrae K, Garber I, Lysyshyn M, Wood E. Initial results of a drug checking pilot program to detect fentanyl adulteration in a Canadian setting. Drug Alcohol Depend 2018;190:242–5.
Bauer LK, Brody JK, Leon C, Baggett TP. Characteristics of homeless adults who died of drug overdose: a retrospective record review. J Health Care Poor Underserved 2016;27(2):846–59.
Kral AH, Lambdin BH, Browne EN, et al. Transition from injecting opioids to smoking fentanyl in San Francisco, California. Drug Alcohol Depend 2021;227:109003.
Acknowledgements
This project was supported by NIDA grant K24DA042720 and CDC grant R01CE003364.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Coffin, P.O., McMahan, V.M. & Murphy, C. Evidence of Pre-mortem Opioid Use among Fentanyl Overdose Decedents in a Safety Net Healthcare System. J Urban Health 99, 865–872 (2022). https://doi.org/10.1007/s11524-022-00663-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-022-00663-1