Abstract
Measurement of alcohol use and associated harms at the city level is often incomplete or non-existent even though such data are often critical to informing local prevention strategies. This paper models how to generate local estimates of the morbidity, mortality, and cost of current alcohol use instead of abstaining. Administrative data sources, including medical examiner records, hospital records, and police records, among others, were used to obtain local estimates of alcohol-attributable outcomes. In 2018, we used alcohol-attributable fractions and scaled national estimates to quantify the burden of current alcohol use in Baltimore, MD, in 2013. Fifty-two percent of Baltimore adults reported past 30-day drinking. There were 276 alcohol-attributable deaths in 2013, and 106 (38.4%) of these were persons other than the drinker. In 2013, current alcohol use cost $582.3 million in Baltimore City. This burden was distributed across drinkers (40.1%), persons other than the drinker (21.3%), and the government (38.6%). It is possible to quantify this burden at the local level, and these data could be used to inform evidence-based alcohol policy strategies at the local level.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In 2017, alcohol was responsible for just over 80,000 deaths in the United States of America (USA) [1]. The repeal of national prohibition left many powers in the hands of states and localities for controlling alcohol-related harm. Although local alcohol policies have provided a model for recent work on tobacco and food availability [2], cities have rarely used those powers in recent years for public health purposes. A common barrier to local action is the lack of locally specific data on the public health and safety burden of alcohol use. Recent analyses from the Global Burden of Disease Study and the Global Survey on Alcohol and Health make the total burden of alcohol plain at the global level. In 2016, alcohol was responsible for 2.8–3 million deaths, or roughly 1 in 20 deaths [3, 4]. Among young adults (i.e., persons aged 18–49 years), alcohol was the leading risk factor for premature death [4]. Alcohol was also responsible for 2.2% of disability-adjusted life years (DALYs) for women and 6.8% for men [4]. There are also several studies that have enumerated the costs of alcohol use in the USA at the national and state levels [5, 6]. Most recently, alcohol was estimated to cost US$249 billion in 2010 [5].
Missing from this landscape are local cost data. When they exist, local-level studies of alcohol-related harms are often limited to single or limited outcomes and lack consistent definitions of key measures. For example, there are estimates of alcohol-related health-care visits [7, 8], alcohol intoxication deaths [9], and alcohol use among suicide and homicide victims [9] in Baltimore. These studies contain an important piece of the puzzle, but they have never been and are not designed to be combined to provide a comprehensive estimate of the burden of alcohol use on the city.
This lack of comprehensive local studies may undermine the public health problem-solving process. The first step in epidemiologic inquiry is defining and measuring the scope of a problem. As existing studies of local burden of disease show [10, 11], the methods required to identify and quantify alcohol-related harms are complex, and this may deter local jurisdictions from attempting to measure the burden of alcohol in their area. This suggests that a template for standardized methods that make use of the most recent epidemiological data may support local jurisdictions’ efforts to identify the local prevalence, morbidity, mortality, and cost of alcohol consumption. In addition, converting the burden of alcohol-related harms to a common metric like cost may allow local jurisdictions to compare the burden of alcohol-related consequences to other health harms.
We are aware of only one comprehensive local area estimate of the burden of alcohol use, even though such data can inform evidence-based prevention strategies at the local level. The Canadian Substance Use Costs and Harms project provides a detailed cost of alcohol estimates at the territory level [12]. In the USA, one study assessed the cost of alcohol-related harms for 20 cities and 10 counties in Oregon [10], but this study did not include any chronic conditions except for alcohol dependence. This study is the first to thoroughly assess the local-level prevalence, morbidity, mortality, and cost of alcohol use in a major US city (Baltimore), using a comprehensive list of alcohol-related harms.
Methods
Data Sources
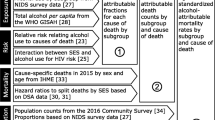
We identified secondary data sources using the conceptual framework depicted in Fig. 1. This framework displays data sources for chronic and acute harms separately. Hospital data contain information on most outcomes; however, these data will be biased to include only harms for which people sought care in a hospital setting. For this reason, additional data sources that may contain more complete records are listed separately and organized by type of alcohol-attributable harm. For data sources that do not publicly release local information, we contacted the local data sources directly, and these are listed in the column on the right. Lastly, data sources used in the present analysis appear with a solid border and data sources not used in this analysis appear with a dashed border. The data sources we used are briefly described in the following section. Additional detail is available in Appendix 3.
Alcohol Exposure
The Behavioral Risk Factor Surveillance System (BRFSS) was used to determine the prevalence of current alcohol consumption (i.e., consuming at least one alcoholic beverage during the past 30 days), binge drinking, and heavy drinking in Baltimore in 2013. The sampling methods for BRFSS have been described in detail elsewhere [13].
Non-fatal Medical Conditions
The Health Services Cost Review Commission (HSCRC) data were the primary data source for non-fatal alcohol-attributable medical conditions and costs for fatal and non-fatal alcohol-attributable hospital and emergency department (ED) visits. HSCRC provides hospital data in accordance with the Healthcare Cost and Utilization Project, and all acute care hospitals in MD must submit data to HSCRC [14]. Hospital records were used for persons aged 15 years or older, except for prematurity, low birth weight, motor vehicle crashes, and child maltreatment, which included patients of all ages.
Emergency Medical Service Transports
We used the Expeditionary Medical Support System (eMEDS) to count the number of alcohol-attributable emergency medical service (EMS) transports. The Baltimore Fire Department maintains these data. Medics enter primary impressions (e.g., chest pain, abdominal pain) and causes of injury (e.g., motor vehicle crash, assault), and therefore, we were only able to identify acute alcohol-attributable injuries from this data source.
Alcohol Treatment Admissions
The Behavioral Health Administration (BHA) provided data on alcohol treatment center admissions. BHA is an agency within the MD Department of Health that provides clinical and preventive behavioral health services and maintains records of alcohol treatment admissions in Baltimore.
Cost of Alcohol Treatment Admissions
Behavioral Health System Baltimore (BHSB) provided data on the cost of alcohol treatment admissions. BHSB is a non-profit organization that oversees the provision of health services in Baltimore.
Deaths
Chief medical examiner records were used as the primary source for alcohol-attributable mortality. The Vital Services Administration (VSA)’s Office of the Chief Medical Examiner (OCME)’s records comprise a near-census of all deaths in Maryland.
Crime
We used police data to count the number of alcohol-attributable crimes. The Baltimore Police Department (BPD) uploads victim-based incident crime data monthly to Open Baltimore, which is an online portal that publishes de-identified county-level public data with no legal restrictions on use [15].
Incarcerations
We used corrections data to determine the number of incarcerations that resulted from alcohol-attributable crime. The Center for Public Safety and Correctional Services (CPSCS) provided these data by crime code. The CPSCS data combine information from individual criminal history records with correctional management and demographic data.
Traffic Crashes
The Maryland Center for Traffic Safety and Analysis (MCTSA) provided data to determine the number of non-fatal alcohol-attributable motor vehicle crashes. The Maryland State Police collect these data at the scene of the traffic crash.
Analysis
Alcohol-Attributable Fractions
An alcohol-attributable fraction (AAF) is the proportion of an outcome attributable to alcohol [6]. In other words, it represents the fraction of cases that would not occur if all current drinkers abstained. We used the AAFs calculated by Bouchery et al. [6] for the USA, which were informed by the Guidelines for Cost of Illness Studies in the Public Health Service. There are two types of AAFs for non-fatal outcomes: (1) AAFs for non-fatal chronic medical conditions were taken from the fatal equivalent condition in CDC’s Alcohol-Related Disease Impact (ARDI) application, and (2) AAFs for non-fatal injuries were derived from a literature review conducted by Bouchery et al. [6], as using the fatal equivalent would overestimate the proportion of alcohol-attributable injuries. AAFs for fatal outcomes were derived from the CDC’s ARDI application [16].
Prevalence
Using the 2013 BRFSS data for Baltimore City, we calculated weighted proportions for estimates of the prevalence of three alcohol consumption patterns, including current alcohol use, binge drinking (i.e., consuming five or more drinks for men or consuming four or more drinks for women, on an occasion), and heavy drinking (i.e., consuming 15 or more drinks per week for men or consuming eight or more drinks per week for women). The applied weights accounted for unequal sampling probabilities and non-response biases. We did not perform subgroup analyses because the strata contained fewer than 550 respondents [35].
Morbidity
We used AAFs to calculate the number of non-fatal alcohol-attributable primary diagnoses in Baltimore hospitals and EDs, car crashes, treatment admissions, incarcerations, and EMS transports. For hospital and ED data, alcohol-attributable visits were identified using only the primary diagnosis, which was coded using the International Classification of Diseases (ICD) codes. This is the international standard used by over 100 countries to identify health-related conditions [17]. Violent crime included homicide, aggravated assault, common assault, rape, other sexual offenses, and robbery. Property crime included motor vehicle theft, larceny, and burglary. We assumed all cases were borne by the drinker except homicide, child maltreatment, fetal alcohol syndrome, and low birth weight, for which we assumed the costs were paid by someone other than the drinker. We also assumed that 38% of motor vehicle traffic crash victims were someone other than the drinker [18].
We used the North Dakota Fetal Alcohol Syndrome Center’s online prevalence calculator tool to determine the number of prevalent cases of fetal alcohol syndrome (FAS) [36]. We conservatively assumed that there were 0.5 case of FAS per 1000 live births, based on estimates of FAS prevalence ranging from 0.5 to 2 per 1000 live births [19].
Mortality
Alcohol-attributable deaths were calculated by multiplying the number of deaths in the OCME data by the fatal AAF. We attributed deaths to drinkers or others using the criteria outlined in the “Morbidity” section.
Cost
We used three approaches to calculate costs as described below.
Actual Costs
We used actual cost information for hospital and ED costs. We flagged visits where the primary diagnosis was alcohol-attributable and then summed the costs for each of these visits, because costs and charges are essentially equivalent under MD’s all-payer model. We then multiplied the total summed costs by the AAF to determine the portion of each visit’s cost stemming from alcohol use. If a patient had multiple alcohol-attributable visits for the same primary diagnosis, we summed the cost for all visits. We calculated costs for fatal and non-fatal visits separately using the appropriate AAFs, because the AAFs for fatal injuries are higher than the AAFs for non-fatal injuries.
Average Costs
We identified and used an average cost for alcohol treatment admissions, EMS transports, crime victim costs, and lost productivity costs for hospitalizations and incarceration (see Bouchery et al. [6], pp. 22–45, for a detailed description of the original methods used to estimate these productivity losses). The average costs for alcohol treatment services were estimated by BHSB using claims data for payments submitted to providers from the fiscal year 2017. The cost was estimated using claims with an alcohol-related diagnosis. The average medical cost was $3773 and was converted to 2013 dollars using a consumer price index for medical services ($3373).
We identified a flat rate for each EMS transport. The cost per transport ranges from $700 to 750, so we used $725 [20]. Of note, Baltimore also charges 10¢ per mile, but we only included the flat fee because the distance of transport was unavailable.
Following methods used and described in Bouchery et al. [6], we used average costs (median annual household income because income is highly skewed in Baltimore [15] or the 2013 minimum wage) to calculate productivity losses for days lost from work due to hospitalizations, absenteeism from non-dependent binge drinking, and incarcerations. To calculate these productivity losses, we first calculated the number of days lost. For alcohol-attributable hospitalizations, we used the actual number of days spent in the hospital, and CPSCS provided estimates for length of stay in a corrections center by crime code for incarcerations. The CPSCS estimates included only the number of days a perpetrator spent in jail immediately after conviction. Secondly, we identified average market equivalents for each type of productivity loss. We used the US Census Bureau’s American Community Survey 2013 5-year estimate [25] for the median annual household income in Baltimore ($41,385) to estimate lost productivity for hospitalizations for alcohol-attributable crimes (Tables A-16 and A-21). We used the 2013 minimum wage ($7.25) to estimate the value of one 8-h work day lost for crime perpetrators who were incarcerated ($58.00) (Table A-17).
We also used average costs to determine the cost of housing inmates in correctional facilities for alcohol-attributable crimes. The Department of Legislative Services estimated the cost to incarcerate one person for 1 year as $37,200 [21].
The National Highway Traffic Safety Administration (NHTSA) provided average unit costs for travel delay, property damage, and legal costs for motor vehicle crashes in US 2010 dollars by the Maximum Abbreviated Injury Scale (MAIS) score [22]. The crash data contained an injury severity rating using the crash-specific KABCO scoring system. We used conversion probabilities to convert the KABCO scores to the MAIS scores [22]. We then multiplied the unit costs by the number of injuries from alcohol-attributable crashes to determine the total costs within each injury severity level.
Scaled Costs
When we were unable to obtain data specific to Baltimore or identify an average cost, we scaled costs from the 2006 national cost study [6]. We used the 2006 study over the 2010 study because it had a greater level of detail. We used scaled costs to estimate charges for federal hospitals, ambulatory care visits/physician offices, nursing home admissions, retail pharmacy, other health professional costs, crime victim costs, research and prevention, training, and health insurance administration. To do this, we calculated indices to scale the costs by population, incidence, and/or price, following the methods outlined in the 2010 national cost of drinking study [5].
We used scaled costs for direct costs associated with FAS; productivity losses from FAS, non-dependent absenteeism, and productivity losses from premature mortality; and professional and household productivity losses from men with alcohol dependence. We obtained estimates for the annual cost of medical treatment, special education, and lost productivity for one person with FAS from Bouchery et al. [6] (Tables A-9, A-11, and A-19). We adjusted these estimates from 2006 dollars to 2013 dollars using the appropriate consumer price index from the US Department of Labor[23]. For losses from premature mortality, we used estimates for the 2000 net present value of the stream of future earnings by age and sex/gender from the University of California at San Francisco adjusted to 2013 dollars, which follows the methods outlined in Bouchery et al. [6] (Tables A-15). The other household and professional productivity losses scaled estimates of losses or incidence rates (e.g., non-dependent binge drinking) that were reported in Bouchery et al. [6] (Tables A-19, A-20, A-21, and A-22). Similar to hospitalizations and incarcerations, we used median annual household income to value time lost from absenteeism associated with non-dependent binge drinking.
Cost Data by Source
We categorized drinkers’ families as persons other than the drinker, whereas Bouchery et al. [6] combined costs to the drinker and their families; however, our other methods for disaggregating costs were consistent with those of Bouchery et al. [6]. We used the distribution of personal health expenditures in the National Health Expenditure Accounts to determine the proportion of health-care costs attributable to drinkers, persons other than the drinker, insurance companies, or the government/society at large [24]. When assigning productivity losses to the government, we used the share of net national income that was comprised of government receipts. Additional details are available in the notes below each table in Appendix 3.
Results
Prevalence
In 2013, 52.5% (95% CI 50.4–55.7%) of Baltimore adults drank alcohol, 16.9% binge drank (95% CI 15.7–19.9%), and 6.1% drank heavily (95% CI 4.8–7.4%).
Morbidity
Current drinking was responsible for 1453 primary diagnoses of mental illness or substance abuse, 324 primary diagnoses of digestive system diseases, 300 primary diagnoses of self-harm or interpersonal violence, and 232 unintentional injuries (Fig. 2). Of the non-fatal primary diagnoses from hospitals and EDs, the patient in 203 (7.3%) was someone other than the drinker and 2579 (92.7%) were the drinkers.
Ten most common conditions associated with alcohol-attributable morbidity, mortality, and cost in Baltimore City hospitals, in 2013. aMedical costs only include costs of non-federal hospital and ED visits; they do not include federal hospitals, doctor’s offices, retail pharmacy, nursing homes, or alcohol treatment centers
Current drinking was responsible for 8,909 non-fatal crimes in 2013 (Table A-18). Of these, 3,241 (36.4%) were violent crimes and 5,668 (63.6%) were property crimes. All crime victims were someone other than the drinker. In 2013, there were 894 perpetrators in jail for alcohol-attributable crimes for a total of 43,679 person days in jail. Violent (414, 46%) and property crimes (364, 41%) comprised most of the crimes for which persons served jail time.
Mortality
In 2013, 276 Baltimore City residents died from alcohol-attributable causes, which comprised 4.3% of all deaths that year. Of these deaths, 170 (61.6%) of the decedents were the drinker, and 106 (38.4%) were someone other than the drinker. Self-harm and interpersonal violence (109 deaths, 39.5%), cirrhosis and liver disease (61 deaths, 22.1%), and unintentional injury (52 deaths, 18.8%) were the leading causes of alcohol-attributable deaths (Fig. 2).
Cost
Current drinking cost $582.3 million in Baltimore in 2013, the majority of which was from indirect costs of productivity losses arising from premature mortality (Table 1). Of this, $233.6 million (40.1%) was paid by the drinker, $124.2 million (21.3%) was paid by someone other than the drinker, and $224.5 million (38.6%) was paid by the government/society at large (Fig. 3). Of the $124.2 million borne by persons other than the drinker, $70.0 million (56.4%) was paid by victims, $31.8 million (25.6%) was paid by private or other insurance companies, and $22.4 million (18.0%) was paid by other persons (Table A-23).
Discussion
There were 276 alcohol-attributable deaths in Baltimore in 2013, and 106 (38.4%) of these were persons other than the drinker. For the sake of comparison, in Baltimore in 2013 there were 235 homicides, a public health issue that has received far more attention. Alcohol cost over $582 million in Baltimore in 2013, and the majority of this was from productivity losses. The total cost is equal to $1,187 per Baltimore adult, $2,260 per drinker, and $2.04 per drink. Less than half of these costs from alcohol use were borne by the drinkers, and almost $2 in $5 was paid by the government/society at large.
Recent national alcohol cost studies can be used to validate these estimates. The 2010 cost study estimated that alcohol consumption cost $2.05 in the USA and $2.22 in Maryland [25]. Our estimate ($2.04 per drink) appears reasonable and suggests that the Baltimore figures may be conservative. Our estimate for alcohol-attributable motor vehicle crashes ($12.9 million) is substantially lower than Baltimore’s population-attributable share ($27.0 million) in Bouchery et al.’s [6] recent national cost study. This could be because fewer households in Baltimore have available vehicles (69.7%) than the national average (91.9%) [25]. These comparisons suggest the validity of our estimates; however, there are also limitations related to scaling national estimates to the local level based on changes in incidence and cost inflation alone, particularly if the demographics of the locality and USA as a whole differ. For example, the costs we derived by scaling the 2010 figures may underestimate health-care costs for crime victims and criminal justice costs, because Baltimore’s crime rate (1401 violent crimes per 100,000 persons) is substantially higher than the USA crime rate (367.9 violent crimes per 100,000 persons) [26]. For these reasons, wherever possible in this paper, we used local administrative data, and other researchers may want to prioritize the same over scaled national or state estimates when doing cost studies, if those data are available.
These estimates are also conservative when considering the broader picture of the types of costs from drinking in society. The administrative data sources used in this study do not contain harms that are less likely to be reported (e.g., minor fights) or are unreported for other reasons. For example, about 62% of robberies and aggravated assaults are reported to police, but only 32% of sexual assaults are reported [27]. In addition, this analysis used a human capital approach, and alternative methods (e.g., willingness to pay) may generate larger estimates of the productivity losses. Based on these considerations, these estimates should not be interpreted as exhaustive. However, the current findings offer substantial gains over previously available estimates [7,7,9, 28].
One of the largest methodological limitations in this study is the reliance on AAFs. AAFs have several shortcomings for estimating morbidity and mortality [4]. In particular, AAFs often determine the outcomes that would be prevented if alcohol consumption was eliminated [29], which may be unrealistic [4]. Other studies may use different baselines (e.g., abstinence, low-level consumption) and different alcohol exposures [30], which problematizes harmonizing methods across condition-specific AAFs. In addition, we used the same AAFs for non-fatal and fatal conditions, which may overestimate the number of non-fatal alcohol-attributable outcomes. Most of the AAFs used in this analysis were calculated using an indirect method. The indirect calculation combines information about the level of alcohol consumption with sex- and condition-specific relative risks [30]. The AAFs calculated using the extant literature are therefore limited by any weaknesses of the underlying studies that provide the relative risks such as lack of appropriate control variables and possible under-reporting in self-reported alcohol consumption [30]. Finally, this study only included AAFs for current drinking, but former drinkers also have elevated risk of some diseases and it is possible to quantify this risk with an AAF [31, 37]. Omitting these additional costs makes the costs presented here more conservative.
There are also limitations of administrative data. The sample of people included in each data source is unclear and might overlap. We accounted for this potential overlap by establishing a hierarchy for data sources so that each category was mapped to a distinct administrative dataset. This limitation is also a strength, because this overlap allowed us to assess the reliability of these estimates. For example, both OCME death and MCTSA crash data identified five fatal alcohol-attributable car crash victims, and the HSCRC hospital cost of alcohol-attributable motor vehicle crash medical care ($1,038,293) was very similar to the estimate calculated using the NHTSA figures ($1,278,528) [22]. In addition, MD’s global billing structure folds some indirect charges into patient bills, so some of the charges reported here would not be averted if the alcohol-attributable conditions had not developed.
This analysis makes use of previous research [16, 30] to add a more local application to the literature that aims to identify and quantify the burden of alcohol at the global level [3, 4]. It provides a template for how to adapt established methods to determine the burden of alcohol at the local level. Given alcohol’s significant role in morbidity and mortality in US cities, such estimates may be critical to stimulating and informing public debate regarding how best to reduce this high level of harm. Local cost studies like this one could inform and increase the utilization of evidence-based policy strategies at the local level, such as the use of local planning zoning codes [32], dram shop liability [33], and city-level taxes [34].
References
Global Burden of Disease Study. Global burden of disease (GBD) results. Seattle, WA: Institution for Health Metrics and Evaluation; 2017. p. 2017.
Ashe M, Jernigan D, Kline R, Galaz R. Land use planning and the control of alcohol, tobacco, firearms, and fast food restaurants. Am J Public Health. 2003;93(9):1404–8.
World Health Organization. Global status report on alcohol and health 2018. Geneva, Switzerland: World Health Organization; 2018.
GBD (2016) Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. Sep 22 2018;392(10152):1015-1035.
Sacks JJ, Gonzales KR, Bouchery EE, Tomedi LE, Brewer RD. 2010 national and state costs of excessive alcohol consumption. Am J Prev Med. 2015;49(5):e73–9.
Bouchery E, Simon C, Harwood H. Economic costs of excessive alcohol consumption in the United States, 2006. Atlanta, GA: Centers for Disease Control and Prevention; 2013.
Spencer M, Petteway RJ, Bacetti L, Barbot O. (2011) Healthy Baltimore 2015: a city where all residents realize their full health potential. Baltimore, MD: Baltimore City Health Department;.
Maryland Department of Health and Mental Hygiene. Drug and Alcohol-Related Emergency Department visits in Maryland 2008-2014. Baltimore, MD: Maryland Department of Health and Mental Hygiene; 2015.
Maryland Department of Health and Mental Hygiene (2012) Maryland violent death reporting system 2010 surveillance report. Baltimore, MD.
League of Oregon Cities, Association of Oregon Counties 2011. The financial impact of alcohol-related costs on cities and counties. Salem, OR.
Paileeklee S, Kanato M, Kaenmanee S, McGhee SM. Alcohol drinking behaviour and economic cost incurred by users in Khon Kaen. J Med Assoc Thail. Mar 2010;93(Suppl 3):S38–44.
Canadian Substance Use Costs and Harms Scientific Working Group. Canadian substance use costs and harms (2007–2014). Ottawa, Ontario: Prepared by the Canadian Institute for Substance Use Research and the Canadian Centre on Substance Use and Addiction; 2018.
Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System overview: BRFSS 2013. Atlanta, GA; 2014.
Chapter 10.37.06 Submission for hospital discharge data set to the commission. In: Hygiene DoHM, ed. Title 10. Part 5. Subtitle 37. Chapter 10.37.06; 2016.
City of Baltimore. Open Baltimore; 2016.
Centers for Disease Control and Prevention. Alcohol-Related Disease Impact (ARDI) tool. Available at: https://nccd.cdc.gov/DPH_ARDI/Default/Default.aspx. Accessed 21 December 2016.
World Health Organization. International Classification of Diseases (ICD) Information Sheet. Available at: http://www.who.int/classifications/icd/factsheet/en/. Accessed 9 October 2018.
National Highway Traffic Safety Administration. Traffic safety facts: alcohol impaired driving. Washington, DC: US Department of Transportation National Highway Traffic Safety Administration; 2017.
May PA, Gossage JP. Estimating the prevalence of fetal alcohol syndrome: a summary. Alcohol Res Health. 2001;25(3):159–67.
Baltimore City Government. Ambulance Billing Information. Available at: http://www.baltimorecountymd.gov/Agencies/fire/ems/ambulancebilling.html. Accessed 12 December 2018.
Justice Policy Institute. The right investment? Corrections spending in Baltimore City. Baltimore City, MD 2015.
Blincoe L, Zaloshnja E, Lawrence B (2015). The economic and societal impact of motor vehicle crashes, 2010 (revised). Washington DC: U.S. Department of Transportation, National Highway Traffic Safety Administration.
US Department of Labor. Consumer Price Index. Available at: https://www.bls.gov/cpi/. Accessed May 4, 2018.
Centers for Medicare and Medicaid. Historical National Health Expenditure Data. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsHistorical.html Accessed May 3, 2018.
United States Census Bureau. American Fact Finder. Washington, DC; 2018.
Federal Bureau of Investigation (2014) Uniform crime report: crime in the United States, 2013. Washington DC: US Department of Justice - Federal Bureau of Investigation;.
Truman J, Morgan R. (2016)Criminal victimization, 2015. Bureau of Justice Statistics, Office of Justice Programs, US Department of Justice; 2016. NCJ 250180.
Maryland Department of Health and Mental Hygiene 2017. Drug- and alcohol-related intoxication deaths in Maryland, 2016. Baltimore, MD.
Rehm J, Taylor B, Mohapatra S, Irving H, Baliunas D, Patra J, et al. Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug Alcohol Rev. Jul 2010;29(4):437–45.
Shultz JM, Rice DP, Parker DL, Goodman RA, Stroh G Jr, Chalmers N. Quantifying the disease impact of alcohol with ARDI software. Public Health Rep. 1991;106(4):443–50.
Gmel G, Shield KD, Frick H, Kehoe T, Gmel G, Rehm J. Estimating uncertainty of alcohol-attributable fractions for infectious and chronic diseases. BMC Med Res Methodol. 2011;11(1):48.
Campbell CA, Hahn RA, Elder R, Brewer R, Chattopadhyay S, Fielding J, et al. The effectiveness of limiting alcohol outlet density as a means of reducing excessive alcohol consumption and alcohol-related harms. Am J Prev Med. 2009;37(6):556–69.
Rammohan V, Hahn RA, Elder R, Brewer R, Fielding J, Naimi TS, et al. Effects of dram shop liability and enhanced overservice law enforcement initiatives on excessive alcohol consumption and related harms: two Community Guide systematic reviews. Am J Prev Med. 2011;41(3):334–43.
Elder RW, Lawrence B, Ferguson A, et al. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am J Prev Med. 2010;38(2):217–29.
Centers for Disease Control and Prevention. 2013 SMART BRFSS MMSA Methodology, vol. 2013. Atlanta, GA.
North Dakota Fetal Alcohol Syndrome Center. FASD Prevalence and Cost Calculator. Grand Forks, ND; ND.
Rehm J, Samokhvalov AV, Shield KD. Global burden of alcoholic liver diseases. J Hepatol. 2013;59(1):160–8.
Acknowledgments
We would like to thank Dr. Darcy Phelan-Emerick of the Baltimore City Health Department and Naomi Greene and Dr. Raimee Eck from Johns Hopkins Bloomberg School of Public Health for their help with this project. We would also like to thank the numerous people who helped us obtain data for this project: Dr. Linda Simoni-Wastila and Abree Johnson from the Maryland Statewide Epidemiological Outcomes Workgroup, who helped us identify data sources and connect to data custodians; Ceres Martin from the Behavioral Health Administration for providing the counts of alcohol treatment cases; Dr. Amanda Latimore and Tara Thallmayer from Behavioral Health System Baltimore for generating the cost estimates for alcohol dependence services; Oscar Ibarra from the Health Services Cost Review Commission for the help with the data request process and providing access to the hospital data; Tim Kerns and Doug Mowbray from the National Study Center for Trauma and EMS and the Maryland Department of Transportation’s Highway Safety Office, respectively, for extracting the non-fatal car crash data; and Jay Miller from the Department of Public Safety and Correctional Services who provided the corrections data.
Funding
This report was supported by Cooperative Agreement Number 5U48DP005045 from the Centers for Disease Control and Prevention. This manuscript was also supported by Award Numbers T32AA007240 (Graduate Research Training in Alcohol Problems: Alcohol-related Disparities) and P50AA005595 (Epidemiology of Alcohol Problems: Alcohol-Related Disparities from the National Institute on Alcohol Abuse and Alcoholism).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
Its contents are solely the responsibility of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, the Department of Health and Human Services, the National Institute on Alcohol Abuse and Alcoholism, or the National Institutes of Health.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 238 kb)
Rights and permissions
About this article
Cite this article
Trangenstein, P.J., Jernigan, D.H. The Health Impact of Alcohol on American Cities: Modeling the Local Burden of Current Alcohol Use in One Jurisdiction. J Urban Health 97, 260–270 (2020). https://doi.org/10.1007/s11524-019-00403-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-019-00403-y