Abstract
In the USA, undocumented Latino immigrants may have poorer health because of barriers to health care, stressors, and detrimental effects of immigration enforcement. Previous immigrant health research, however, suggests that recently arrived Latino immigrants have better health than US-born Latinos and their health deteriorates over time. Given the current environments that undocumented immigrants face, legal status is a structural factor that likely influences the patterns of immigrant health. Therefore, the aim of this study was to examine the extent to which physical and mental health differed by legal status and duration in the USA for the Latino population in Los Angeles County, California. We conducted analysis of Latino respondents (n = 1396) to the Los Angeles Family and Neighborhood Survey (L.A.FANS) Wave II. We examined self-reported health, depression measured by the Composite International Diagnostic Interview—Short Form, and blood pressure collected by trained interviewers. Respondents reported their legal status, time in the USA, and other sociodemographic characteristics. Regression models were used to test associations between each outcome and 1) legal status and 2) legal status by duration (≤ 15 and > 15 years) in the USA. Without taking duration into account, we found no significant differences in outcomes between undocumented, documented, or US-born Latinos. Taking duration into account, shorter duration undocumented immigrants had worse self-reported health than the US born. Undocumented immigrants, regardless of duration, had higher blood pressure than documented immigrants who had been in the USA for less time and the same level of blood pressure as the US born. In contrast, shorter duration documented immigrants had lower blood pressure compared to longer duration documented immigrants and US-born counterparts, and marginally lower blood pressure than shorter duration undocumented immigrants. The findings suggest that the “health advantage” generally presumed to exist among immigrants may not affect undocumented immigrants.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Currently, undocumented immigrants in the USA face more restrictive legal, social, and health care environments. First, there has been an increase in anti-immigrant rhetoric, creating environments in which undocumented immigrants are denounced and demonized by politicians and the public [1]. Second, this rhetoric has motivated federal and state policies that exclude undocumented immigrants from access to health and social services, while increasing the number of apprehensions and deportations [2,3,4], increasing concern about discrimination and racial profiling [5, 6]. Finally, militarization of the US border has altered patterns of return migration. Massey et al. (2014) argue that Mexican migrants, in particular, are now less likely to return to Mexico than in the past, as reentry is more dangerous. Thus, many undocumented immigrants have resided in the USA for long periods, unable to regularize their status within increasingly restrictive environments.
These environments may have a more negative effect on undocumented immigrants’ health compared to documented immigrants and US-born individuals [6, 7]. Yet, research on immigrant health indicates that recently arrived Latino immigrants tend to have better health than US-born Latinos and that their health deteriorates as they spend more time in the USA [8]. This trend, called the Hispanic Paradox, has been observed in outcomes such as mortality, infant health, and health behaviors [9, 10]. It is largely attributed to both health selection, in which migrants tend to be the healthiest individuals who have the resources and drive to make it to the USA [11] and behavioral changes, through which, over time immigrants lose traditional behaviors and adopt detrimental ones [9, 10]. However, most previous studies have not been able to distinguish immigrants by legal status and duration in the USA. Growing evidence indicates that structural factors in the receiving location—such as discrimination or health care policy—influence the integration process and its consequences for immigrant health [7, 12,13,14]. Given the current environment that undocumented immigrants face, legal status is a structural factor that likely influences their trajectories in the USA and may be associated with differences in health [7].
Only a limited body of research has examined the relationship between legal status and health and much less about its long-term effects. Data on legal status is seldom collected in population-based surveys out of concern about respondents’ comfort and safety [15, 16]. Thus, knowledge about differentials in health by legal status and duration in the USA generally comes from studies of non-representative samples [17, 18]. In this paper, we use a population-based sample of Latinos representative of Los Angeles County in which health outcomes were measured by trained technicians and information was collected on individuals’ legal status and time spent in the USA. Our analysis examines three indicators of health—self-reported health, depression, and high blood pressure—which have been associated in previous research with access to care and stress [19,21,22,22]. Below, we describe the study’s motivation and background, data and methods, and results.
Background
There are an estimated 11–12 million undocumented immigrants in the USA [23, 24]. The majority of the nation’s undocumented, and documented, immigrants were born in Latin America, primarily in Mexico [24]. In the USA, undocumented Latino immigrants are subject to multiple structural disadvantages. As Latinos, they face racialized discrimination rooted in US history [25, 26]. As immigrants, they may be stigmatized for their “foreign-ness,” limited English, or differences in customs [27]. As undocumented immigrants, they are subject to apprehension and deportation as well as to mistreatment by employers, landlords, and others [28, 29].
In the current era of increased enforcement, legal status affects most aspects of immigrants’ lives as well as the social mobility of their children [30, 31]. Menjívar et al. (2016) suggest that legal status is an important element of social stratification in the USA, similar to class, race, and gender. However, while US law prohibits discrimination based on race and gender, it encourages or requires discrimination based on legal status (e.g., prohibition on hiring undocumented immigrants). The significance of being undocumented is shaped by social and political forces—such as the public policies that determine eligibility for health care or the social attitudes that reinforce discrimination [4, 32].
There is extensive evidence indicating that health is associated with class, race, and gender and that more disadvantaged groups often experience worse health [33, 34]. Given the disadvantaged position of undocumented immigrants, they may experience poor mental and physical health because of limited access to health care, stressors, and detrimental effects of immigration enforcement [12]. These structural factors may have a cumulative effect on those who spend longer periods of time in an undocumented status [35].
Limited Access to Health Care
Undocumented immigrants, as well as their children, are less likely to be insured than their documented and US-born counterparts [36,38,39,40,40].They are ineligible for most public insurance programs—such as Medicaid or Medicare—due to policies such as the Personal Responsibility and Work Opportunity Reconciliation Act of 1996 and the Affordable Care Act of 2010 (ACA) [41,43,43]. Exceptions exist in a handful of states that use state funds to extend Medicaid for children and pregnant women [44]. They are also ineligible for some safety net programs, such as the Supplemental Nutrition Assistance Program [41].
Partly because of lack of insurance, undocumented immigrants also experience barriers to accessing health care. This population experiences delays in care (e.g., late or inadequate prenatal care) and less preventive care [37, 40, 45,47,47] and receives care for chronic and life-threatening conditions at more advanced stages [48,50,51,52,52]. Studies have shown that barriers to care are exacerbated by distrust of government institutions, concern about immigration enforcement, and lack of mobility [53,55,56,56].
Stressors Associated with Undocumented Status
The experience of being undocumented and living in restrictive environments can be a source of chronic stress [17, 57]. Stressors range from work conditions in low-paying occupations and family separation to concern about discrimination, xenophobia, and deportation. Research shows that the types of stress that undocumented immigrants are likely to face are associated with poor mental health outcomes [18, 19, 59–61]. For example, studies found that perceived discrimination was associated with depression and poorer self-reported health among Mexican-origin adults and that concern about deportation was associated with higher levels of emotional distress [17, 18]. After the passage of Proposition 187—an initiative that barred undocumented immigrants from public services—in California in 1994, there was a reduction in the use of preventive mental health services among young Latinos that was followed by an increase in use of crisis services [61].
Health Consequences of Immigration Enforcement
Growing evidence also suggests that immigration enforcement policies may exacerbate both barriers to access to health care and stressors faced by all immigrants, but particularly those who are undocumented [6, 56, 62]. A study of Latinos living in Arizona after the passage of SB 1070—a law that required police inquire about individuals’ legal status—found that Spanish-speaking individuals had worse self-reported health than other Latinos [5]. Studies have found that individuals who reported fear of deportation were aggravated by collaboration between law enforcement and Immigration and Customs Enforcement [53, 54, 56]. Immigrants in communities with heightened enforcement also felt that enforcement condoned racial profiling and resulted in restriction of movement around the community [53,55,55].
This Study
We examine variations by legal status and duration in the USA for the Latino population in Los Angeles County, California, in three measures of health status: self-reported health, depression, and blood pressure. These outcomes provide an overall assessment of patterns in the mental and physical health status of Latino immigrants. There is evidence that chronic stress and consequences of immigration enforcement are detrimental to mental health among undocumented immigrants [17, 18]. While there is a limited research on physical health by legal status, evidence suggests that its prevalence and outcomes also vary between undocumented and documented immigrants, even if immigrants have generally better outcomes than their US-born counterparts. For example, one study of US-born and immigrant Latinos in Utah found that immigrants had lower rates of obesity than the US born, but among women, the undocumented had a higher average BMI than the documented [64]. Another study found that undocumented Brazilian immigrants in Boston were at higher risk of cardiovascular disease than their documented counterparts [63]. Overall, the barriers to care that the undocumented face exacerbated by stress and enforcement may decrease utilization of disease prevention or treatment for both physical and mental health conditions.
We first compare outcomes between Latinos who are undocumented, documented, and US born to assess patterns by legal status. Research on the Hispanic Paradox would suggest that, regardless of legal status, Latino immigrants have better outcomes than their US-born counterparts [65]. Recent research on legal status, however, suggests that undocumented Latino immigrants may fare worse than the documented [35], and other studies suggest that health selection is small or non-existent and that some immigrants experience serious health deterioration shortly after migration [66].
Second, we include duration in the USA to examine if patterns by legal status vary based on the time spent in the USA. We compare undocumented immigrant Latinos with 15 or fewer and over 15 years in the USA, documented immigrant Latinos with 15 or fewer and over 15 years in the USA, and US-born Latinos. We chose 15 years based on the sample distribution of duration (mean = 23 years for the total foreign-born sample and 13 years for the undocumented) and because changes in health develop over many years. Given the stress associated with undocumented status, this group may experience worse outcomes at all durations compared to the documented. However, both the undocumented and documented at shorter durations may have better outcomes than US-born Latinos. US-born Latinos also face exposure to inequitable and discriminatory social structures within the USA [12, 14] and have less healthy behaviors than recently arrived immigrants [10]. At longer durations, documented immigrants may have the same health outcomes as US-born Latinos; in contrast, due to prolonged exposure to inequitable social conditions, undocumented immigrants may have significantly worse outcomes than either US born or documented individuals. Our study contributes to the literature on immigrant health by being one of the first to examine differences I physical and mental health by legal status and duration in the USA, using high quality, population-based, representative data.
Methods
Data Collection and Participants
We used Los Angeles Family and Neighborhood Survey (L.A.FANS) Wave II data, collected April 2007–January 2008. L.A.FANS is a stratified probability sample of census tracts and residents in Los Angeles County. Sample weights correct for sample design and differential response [67]. Respondents age 18 and older were interviewed in person. We included respondents who identified as Latino/Hispanic (n = 1396), including those identifying as Latino plus another race/ethnicity (n = 43). This study analyzed secondary data with no personal identifiers and received a certificate of exemption from the University of California, Los Angeles Institutional Review Board.
Measures
The legal status variable used in the analysis is based on a sequence of questions: Those responding “Yes” to the following were classified as US born: Were you born in the USA? (36.7% of sample). Those responding “No” to the born in the US question and then “Yes” to one of the following were classified as documented: Are you a citizen of the USA? (20.3%); Do you currently have a permanent residence card or a green card? (19.2%); and Have you been granted asylum, refugee status, or temporary protected immigrant status, TPS? or Do you have a valid tourist visa, a student visa, a work visa or permit, or another document which permits you to stay in the USA for a limited time (2.4%)? Those who did not say “yes” to any of the other questions were classified as undocumented (21.3%). Duration in the USA was calculated as the difference between the year of arrival and the interview date
We created a variable which combined legal status and duration, categorizing individuals as US born, documented with ≤ 15-year duration, documented with > 15-year duration, undocumented with ≤ 15-year duration, and undocumented with > 15-year duration. We used a categorical variable to allow for comparison with US-born individuals for whom duration is not applicable.
For the dependent variables, we used measures of self-reported health (SRH), depression, and continuous and dichotomous measures of blood pressure. The standard SRH question asked respondents to describe their health as Excellent, Very Good, Good, Fair, or Poor. We combined the Fair and Poor categories because they are relatively small. Larger values of the variable indicate poorer health. Depression was assessed using the Composite International Diagnostic Interview—Short Form (CIDI-SF) questionnaire that covers major depressive episodes, assessing if respondents who report feeling sad, blue, or depressed for 2 weeks or more in the past 12 months or if they lost interest in most things like hobbies or work. We employed the standard CIDI-SF dichotomous measure which indicates whether a respondent is likely or not likely to be depressed based on reported symptomology. The continuous measure of blood pressure was based on the average of three systolic blood pressure (SBP) readings collected by trained interviewers using high-quality automated machines and standardized protocols [67]. SBP, a risk indicator for heart disease, measures pressure in the arteries when the heart beats [68, 69]. Diastolic blood pressure (DBP) may also indicate heart disease risk [70]. Separate analyses (not shown) using DBP produced similar results as SBP. We also created a dichotomous measure based on the clinical cut-off off for hypertension (SBP ≤ 140 mmHg and DBP ≤ 90 mmHg).
Control variables included continuous measures for respondents’ age and completed years of education and dichotomous measures for sex, employment, cohabitation with spouse/partner, insurance status, having a usual place to receive health care, and language of interview.
Analysis
Analysis was conducted in Stata using the SVY commands to account for sampling design [71]. We conducted descriptive analysis to assess the distributions of the covariates by legal status and duration. We estimated ordinal logistic regression models for self-reported health, logistic regression models for depression and hypertension, and OLS regression models for blood pressure, each controlling for statistically significant covariates. For consistency, US-born Latinos were the reference group.
Results
Table 1 presents the characteristics of the sample by legal status and duration. Thirty-seven percent were US born, 42% were documented immigrants, and 21% were undocumented immigrants. There were differences by legal status in duration, age, employment, years of education, and cohabitation. Longer duration documented immigrants had significantly higher blood pressure and the highest proportion of hypertension than the other groups. The shorter duration undocumented immigrants had the lowest proportion of individuals reporting excellent health, while the longer duration undocumented had the highest proportion. Both undocumented and documented immigrants at shorter durations had the highest proportion of being depressed, while the longer duration undocumented had the lowest.
Self-Reported Health
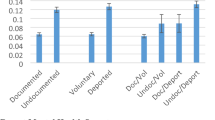
Table 2 presents the models testing differences in self-reported health (SRH) between undocumented immigrants, documented immigrants, and US-born Latinos (Model 1) and documented immigrants and undocumented immigrants with ≤ 15- or > 15-year duration and US-born Latinos (Model 2).
Although we expected poorer health status among undocumented immigrants, the results in Model 1A show no significant differences in the odds of reporting worse SRH among undocumented, documented and US-born Latinos. Age and having a usual source of health care were associated with worse SRH, while years of education and completing the interview in Spanish were associated with better SRH.
In Model 2A, we introduce duration in the USA. Undocumented immigrants who had lived in the USA for 15 or fewer years had a higher odds (OR 1.2, p < 0.01) of worse SRH compared to the US born. A test (not shown) comparing the two undocumented groups indicated that the shorter duration undocumented immigrants had greater odds (OR 4.2, p < 0.1) of worse SRH than their longer duration counterparts.
Depression
Supplemental Table A presents the models testing differences in depression by legal status and duration. We observed no differences by legal status nor by legal status by duration. In addition, the odds of being depressed did not vary across any of the covariates.
Blood Pressure and Hypertension
Table 3 presents models for blood pressure (panel A) and hypertension (panel B) by legal status (Model 1) and legal status by duration (Model 2). Similar to the result for self-reported health, the results in Model 1A show no significant differences in blood pressure by legal status among Latinos. Being on blood pressure medicine, being male, age, BMI, and current employment were associated with higher blood pressure. Having health insurance and cohabitation were associated with lower levels. These associations held across the subsequent models.
In Model 2A, the level of blood pressure by duration varied between the undocumented and documented immigrants. First, among undocumented immigrants, neither the shorter nor longer duration groups had significantly different blood pressure compared to the US born. In contrast, shorter duration documented immigrants had on average 8.1 points lower blood pressure (p < 0.01) compared to the US born. Second, there was no difference in blood pressure between shorter and longer duration undocumented immigrants, while shorter duration documented immigrants had on average 8.9 points lower blood pressure compared to their longer duration counterparts (p < 0.01). Finally, tests (not shown) comparing the undocumented and documented groups indicated a marginally significant difference between the shorter duration undocumented and documented groups, in which documented immigrants had an average of 6.2 points lower blood pressure (p = 0.07). The shorter duration documented immigrants also had on average 7.8 points lower blood pressure compared to longer duration undocumented (p < 0.01).
A comparable pattern was found in the hypertension models (panel B). In Model 1B, there was no significant difference in odds of hypertension solely by legal status. In Model 2B, there were no significant differences in odds of hypertension between undocumented immigrants at either level of duration compared to the US born. In contrast, in Model 2B, the shorter duration documented immigrants had 90% lower odds of hypertension compared to the US born, as well as compared to longer duration documented immigrants.
Discussion
This study examined variations in physical and mental health among undocumented, documented, and US-born Latinos. Undocumented Latino immigrants experience greater barriers to health care and more stress related to anti-immigrant environments and enforcement in daily life than either documented immigrant or US-born Latinos. Therefore, we anticipated observing worse health among undocumented, compared to documented, immigrants. At the same time, the Hispanic Paradox suggests that, when they arrive in the USA, Latino immigrants have better health and health behaviors compared to US-born Latinos and that their health deteriorates over time. We anticipated that both undocumented and documented immigrants might have better outcomes than their US-born counterparts, and that longer duration of residence in the USA would increase stress on undocumented immigrants and worsen their health. To examine these possible patterns, this study examined the associations between measures of SRH, depression, and blood pressure and both legal status and legal status by duration in the USA.
Without taking duration into account, we found that there were no significant differences in SRH, depression, or blood pressure between Latinos who were undocumented, documented, or US born. When duration was taken into account, we found variations in SRH and blood pressure by legal status. First, undocumented immigrants who had lived in the USA for 15 or fewer years were much more likely to report worse SRH than their US born and longer duration undocumented counterparts. Second, undocumented immigrants, regardless of duration, had higher blood pressure than documented immigrants who had been in the USA for less time. Further, their outcomes did not vary from the US born. In contrast, documented immigrants who had lived in the USA 15 or fewer years had lower blood pressure and lower odds of hypertension than the US born and undocumented with longer duration. While marginally significant, findings suggest that the shorter duration documented immigrants also had lower blood pressure compared to the shorter duration undocumented.
These different patterns by legal status and duration suggest that the health of undocumented immigrants may not fit the presumed pattern of the Hispanic Paradox. In the sample of this study, undocumented immigrants did not display the “health advantage” presumed to exist among immigrant populations [8]. It was the most recently arrived undocumented immigrants who were more likely to report worse health than the US born. Regardless of the amount of time they had lived in the USA, undocumented immigrants did not have different blood pressure or odds of hypertension than their US-born counterparts. In contrast, shorter duration documented immigrants did have lower blood pressure and odds of hypertension.
These findings are consistent with recent studies that have found that the Hispanic Paradox does not explain patterns of health for all immigrant populations [9]. Instead of experiencing a “health advantage,” undocumented immigrants likely experience a different pattern of changes in health status prior to or after arriving to the USA. First, undocumented immigrants may experience a more rapid decline in well-being than the documented [66]. For example, undocumented immigrants may experience more stressful migration; unauthorized border crossing is both physically risky and financially costly, including incurring of large debts [72, 73]. Second, undocumented immigrants may arrive in the USA with poorer health than their documented counterparts. The structural factors in home countries that influence whether immigrants are able to migrate with authorization likely shape health selection [35]. Unfortunately, the data were not available to examine health status at the time of or shortly following migration.
The lack of variation in outcomes based on legal status may stem from several factors. First, our study may have been handicapped by the age distribution of the sample, most of whom were relatively young and potentially less likely to show signs of poor health. Second, it may stem from the complexity of legal status stratification. Documented immigrants also face barriers and stressors: they also have limited eligibility for some health care and social services and, similarly, may face xenophobic environments, discrimination, and risk of deportation [2, 41]. Some studies have found significant differences in health between citizens and noncitizens, suggesting that lack of citizenship may also be a salient line of difference [74, 75]. Second, the stressors associated with undocumented status may have spillover effects as documented immigrants often reside in mixed status families. Several studies show that children of undocumented parents fare worse than their peers with documented parents [76, 77]. Finally, documented immigrants may have experienced a period in a temporary or undocumented status, resulting in past experiences of stress and barriers to care.
These findings point to recommendations for future research on legal status and health. First, our findings suggest that, in the aggregate, comparisons between US-born and foreign-born populations may mask differences that exist based on legal status. Given the relatively small body of literature on legal status and health, more research is needed that examines variations in different outcomes by legal status. This research should incorporate amount of time in the US. Second, longitudinal data could be used to further examine the patterns observed in this study to assess the individual health trajectories of undocumented and documented immigrants over time. Finally, research is needed that disentangles how mechanisms such as barriers to care or stress may affect the documented, as well as the undocumented. Longitudinal data could be used to assess associations between changes in legal status and changes in health status. Data on immigrant families could be used to assess the impact on stress and access to care of residing in a mixed status family.
This study has some limitations. First, we used a small cross-sectional data set. We compared individuals at different durations in the USA, not changes in individual health by duration. As a result, the duration groups are affected by selective return migration [78]. However, decline in the frequency of return migration for undocumented immigrants during this time period may mitigate the selection problem [23]. Also, the duration groups arrived at different points in historical time [79] and conditions in both sending and receiving country can change over time. In addition, the sample sizes for each group may have resulted in a lack of power to detect differences. Second, immigrants’ pathways among legal statuses are complex and were outside the scope of this study. Future research should examine the health impact of becoming documented. Finally, the study sample comes from Los Angeles, a social, economic, and political context for immigrants that may not be generalizable to other areas of the county, such as new destination areas in the South and South East [80].
Amid growing calls to promote the well-being of Latinos by addressing social inequality [81], it is critical to understand the impact of legal status on well-being. Overall, this study points to the importance of examining legal status as a form of inequality among Latinos. These issues are important given the nation’s large population of undocumented immigrants and the recent increase in anti-immigrant policy that has exacerbated the social and economic inequalities faced by many immigrants.
References
Chavez LR. The Latino threat: constructing immigrants, citizens, and the nation. Stanford, Calif.: Stanford University Press; 2008.
Golash-Boza T, Hondagneu-Sotelo P. Latino immigrant men and the deportation crisis: a gendered racial removal program. Latino Stud. 2013;11(3):271–92.
Valdez CR, Lewis Valentine J, Padilla B. “Why we stay”: immigrants’ motivations for remaining in communities impacted by anti-immigration policy. Cult Divers Ethn Minor Psychol. 2013;19(3):279–87.
Motomura H. Immigration outside the law. New York: Oxford University Press; 2014.
Anderson KF, Finch JK. Racially charged legislation and Latino health disparities: the case of Arizona’s S.B. 1070. Sociol Spectr. 2014;34(6):526–48.
Martinez O, Wu E, Sandfort T, Dodge B, Carballo-Dieguez A, Pinto R, et al. Evaluating the impact of immigration policies on health status among undocumented immigrants: a systematic review. J Immigr Minor Health. 2015;17(3):947-70.
Castaneda H, Holmes SM, Madrigal DS, Young ME, Beyeler N, Quesada J. Immigration as a Social Determinant of Health. Annu Rev Public Health. 2015;36:375-92.
Rodriguez H, Saenz R, Menjivar C (Eds.). Latinas/os in the United States. Changing the face of América. New York, USA: Springer; 2008.
Creighton MJ, Goldman N, Pebley AR, Chung CY. Durational and generational differences in Mexican immigrant obesity: is acculturation the explanation? Soc Sci Med. 2012;75(2):300–10.
Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–97.
Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543–8.
Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75(12):2099–106.
Zambrana RE, Carter-Pokras O. Role of acculturation research in advancing science and practice in reducing health care disparities among Latinos. Am J Public Health. 2010;100(1):18–23.
Acevedo-Garcia D, Sanchez-Vaznaugh EV, Viruell-Fuentes EA, Almeida J. Integrating social epidemiology into immigrant health research: a cross-national framework. Soc Sci Med. 2012;75(12):2060–8.
Carter-Pokras O, Zambrana RE. Collection of legal status information: caution! Am J Public Health. 2006;96(3):399; author reply 399-400.
Prentice JC, Pebley AR, Sastry N. PRENTICE ET AL. RESPOND. Am J Public Health. 2006;96(3):399–400.
Arbona C, Olvera N, Rodriguez N, Hagan J, Linares A, Wiesner M. Acculturative stress among documented and undocumented Latino immigrants in the United States. Hisp J Behav Sci. 2010;32(3):362–84.
Cavazos-Rehg PA, Zayas LH, Spitznagel EL. Legal status, emotional well-being and subjective health status of Latino immigrants. J Natl Med Assoc. 2007;99(10):1126–31.
Tamashiro KLK, Hegeman MA, Sakai RR. Chronic social stress in a changing dietary environment. Physiol Behav. 2006;89(4):536–42.
Spruill T. Chronic psychosocial stress and hypertension. Curr Hypertens Rep. 2010;12(1):10–6.
Moore CJ, Cunningham SA. Social position, psychological stress, and obesity: a systematic review. J Acad Nutr Diet. 2012;112(4):518–26.
Fowler-Brown AG, Bennett GG, Goodman MS, Wee CC, Corbie-Smith GM, James SA. Psychosocial stress and 13-year BMI change among blacks: the Pitt County Study. Obesity. 2009;17(11):2106–9.
Passel JS, Cohn DV, Rohal M. Unauthorized immigrant totals rise in 7 states, fall in 14: decline in those from mexico fuels most state decreases. Washington, D.C.: Pew Research Center; 2014.
Passel JS, Cohn DV. A portrait of unauthorized immigrants in the United States. Washington, D.C.: Pew Hispanic Center; 2009.
Ortiz V, Telles E. Racial Identity and Racial Treatment of Mexican Americans. Race Soc Probl. 2012;4(1):10.1007/s12552-012-9064-8.
Lopez IFH. Race and erasure: the salience of race to Latinos/as. In: Delgado R, Stefancic J, editors. Critical race theory: the cutting edge. Philadelphia, USA: Temple University Press; 2000. p. 369–78.
Massey DS, Sánchez M. Brokered boundaries: creating immigrant identity in anti-immigrant times. New York: Russell Sage Foundation; 2010.
Gleeson S, Gonzales RG. When do papers matter? An institutional analysis of undocumented life in the United States. Int Migr. 2012;50(4):1–19.
Gleeson S. Labor rights for all? The role of undocumented immigrant status for worker claims making. Lawn Soc Inq. 2010;35(3):561–602.
Menjívar C, Abrego LJ. Immigrant families. Cambridge, UK: Polity; 2016.
Bean FD, Brown SK, Bachmeier JD. Parents without papers : the progress and pitfalls of Mexican-American integration. New York: Russell Sage Foundation; 2015.
Gee GC, Ford CL. Structural racism and health inequities: old issues, New Directions. Du Bois review: social science research on race. 2011;8(1):115–132.
Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;51(Suppl):S28–40.
Marmot M, Allen JJ. Social determinants of health equity. Am J Public Health 2014;104(Suppl 4):S517–9.
Torres JM, Young MED. A life-course perspective on legal status stratification and health. SSM - Population Health. 2016;2:141–8.
Flores G, Abreu M, Tomany-Korman SC. Why are Latinos the most uninsured racial/ethnic group of US children? A community-based study of risk factors for and consequences of being an uninsured Latino child. Pediatrics. 2006;118(3):e730–40.
Guendelman S, Angulo V, Wier M, Oman D. Overcoming the odds: access to care for immigrant children in working poor families in California. J Matern Child Health. 2005;9(4):351–62.
Stevens GD, West-Wright CN, Tsai KY. Health insurance and access to care for families with young children in California, 2001-2005: differences by immigration status. J Immigr Minor Health. 2010;12(3):273–81.
Vargas Bustamante A, Chen J, Fang H, Rizzo JA, Ortega AN. Identifying health insurance predictors and the main reported reasons for being uninsured among US immigrants by legal authorization status. Int J Health Plann Manage. 2014;29(1):e83-e96.
Vargas Bustamante A, Fang H, Garza J, Carter-Pokras O, Wallace SP, Rizzo JA, et al. Variations in healthcare access and utilization among Mexican immigrants: the role of documentation status. J Immigr Minor Health. 2012;14(1):146–55.
Broder T, Moussavian A, Blazer J. Overview of Immigrant Eligibility for Federal Programs. Los Angeles, USA: National Immigrant Law Center; 2015.
Hagan J, Rodriguez N, Capps R, Kabiri N. The effects of recent welfare and immigration reforms on immigrants’ access to health care1. Int Migr Rev. 2003;37(2):444–63.
Kaushal N, Kaestner R. Welfare reform and health insurance of immigrants. Health Serv Res. 2005;40(3):697–722.
Rodriguez M, Young ME, Wallace SP. Creating conditions to support healthy people: state policies that affect the health of undocumented immigrants and their families. Los Angeles, USA: UCLA Center for Health Policy Research; 2014.
Rodriguez MA, Bustamante AV, Ang A. Perceived quality of care, receipt of preventive care, and usual source of health care among undocumented and other Latinos. J Gen Intern Med. 2009;24(Suppl 3):508–13.
Ortega AN, Fang H, Perez VH, Rizzo JA, Carter-Pokras O, Wallace SP, et al. Health care access, use of services, and experiences among undocumented Mexicans and other Latinos. Arch Intern Med. 2007;167(21):2354–60.
Korinek K, Smith KR. Prenatal care among immigrant and racial-ethnic minority women in a new immigrant destination: exploring the impact of immigrant legal status. Soc Sci Med. 2011;72(10):1695–703.
Poon KK, Dang BN, Davila JA, Hartman C, Giordano TP. Treatment outcomes in undocumented Hispanic immigrants with HIV infection. PLoS One. 2013;8(3):e60022.
Pivnick A, Jacobson A, Blank AE, Villegas M. Accessing primary care: HIV+ Caribbean immigrants in the Bronx. J Immigr Minor Health. 2010;12(4):496–505.
Chin JJ, Kang E, Kim JH, Martinez J, Eckholdt H. Serving Asians and Pacific Islanders with HIV/AIDS: challenges and lessons learned. J Health Care Poor Underserved. 2006;17(4):910–27.
Castro-Echeverry E, Kao LS, Robinson EK, Silberfein EJ, Ko TC, Wray CJ. Relationship between documentation status and survival for medically underserved Hispanic breast cancer patients. J Surg Res. 2013;180(2):284–9.
Campesino M, Ruiz E, Glover JU, Koithan M. Counternarratives of Mexican-origin women with breast cancer. ANS Adv Nurs Sci. 2009;32(2):E57–67.
Berk ML, Schur CL. The effect of fear on access to care among undocumented Latino immigrants. J Immigr Minor Health. 2001;3(3):151–6.
Hacker K, Chu J, Leung C, Marra R, Pirie A, Brahimi M, et al. The impact of immigration and customs enforcement on immigrant health: perceptions of immigrants in Everett, Massachusetts, USA. Soc Sci Med. 2011;73(4):586–94.
Maldonado CZ, Rodriguez RM, Torres JR, Flores YS, Lovato LM. Fear of discovery among Latino immigrants presenting to the emergency department. Acad Emerg Med. 2013;20(2):155–61.
Rhodes SD, Mann L, Siman FM, Song E, Alonzo J, Downs M, et al. The impact of local immigration enforcement policies on the health of immigrant hispanics/latinos in the United States. Am J Public Health. 2015;105(2):329–37.
Menjivar C, Kanstroom D. Introduction—immigrant “illegality”: constructions and critiques. In: Cecilia Menjivar DK, editor. Constructing immigrant “illegality”: critiques, experiences, and responses. New York: Cambridge University Press; 2014.
Potochnick SR, Perreira KM. Depression and anxiety among first-generation immigrant Latino youth: key correlates and implications for future research. J Nerv Ment Dis. 2010;198(7):470–7.
Ojeda L, Pina-Watson B. Day laborers’ life satisfaction: the role of familismo, spirituality, work, health, and discrimination. Cultur Divers Ethnic Minor Psychol. 2013;19(3):270–8.
Negi NJ. Battling discrimination and social isolation: psychological distress among Latino day laborers. Am J Community Psychol. 2013;51(1–2):164–74.
Fenton JJ, Catalano R, Hargreaves WA. Effect of proposition 187 on mental health service use in California: a case study. Health Aff (Millwood). 1996;15(1):182–90.
Amuedo-Dorantes C, Puttitanun T, Martinez-Donate AP. How do tougher immigration measures affect unauthorized immigrants? Demography. 2013;50(3):1067–91.
Holmes LM, Marcelli EA. Neighborhoods and systemic inflammation: high CRP among legal and unauthorized Brazilian migrants. Health Place. 2012;18(3):683–93.
Wen M, Maloney TN. Neighborhood socioeconomic status and BMI differences by immigrant and legal status: evidence from Utah. Econ Hum Biol. 2014;12:120–31.
Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543–8.
Goldman N, Pebley A, Creighton M, Teruel G, Rubalcava L, Chung C. The consequences of migration to the United States for short-term changes in the health of Mexican immigrants. Demography. 2014;51(4):1159–73.
Peterson C, Pebley AR, Sastry N, Yuhas K, Ghosh-Dastidar B, Haas A, et al. The Los Angeles family and neighborhood survey, wave 2 user’s guide and codebook: labor and population program. Los Angeles, CA: RAND Corporation; 2011.
Franklin SS, Larson MG, Khan SA, Wong ND, Leip EP, Kannel WB, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation. 2001;103(9):1245–9.
MacMahon S, Peto R, Collins R, Godwin J, MacMahon S, Cutler J, et al. Blood pressure, stroke, and coronary heart disease: Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335(8692):765–74.
Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: Part I diagnosis, prognosis, and measurements of diastolic function. Circulation. 2002;105(11):1387–93.
StataCorp. Stata: Release 13. In: Statistical Software. College Station, TX: StataCorp LP.; 2013.
Abrego LJ. Sacrificing families: navigating laws, labor, and love across borders. Stanford, CA: Stanford University Press; 2014.
Holmes SM. “Is it worth risking your life?”: ethnography, risk and death on the U.S.–Mexico border. Soc Sci Med. 2013;99:153–61.
Gee GC, Ryan A, Laflamme DJ, Holt J. Self-reported discrimination and mental health status among African descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 initiative: the added dimension of immigration. Am J Public Health. 2006;96(10):1821–8.
Gubernskaya Z, Bean FD, Van Hook J. (Un)Healthy immigrant citizens: naturalization and activity limitations in older age. J Health Soc Behav. 2013;54(4):427–43.
Pong SL, Landale NS. Academic achievement of legal immigrants’ children: the roles of parents’ pre- and postmigration characteristics in origin-group differences. Child Dev. 2012;83(5):1543–59.
Landale NS, Hardie JH, Oropesa RS, Hillemeier MM. Behavioral functioning among Mexican-origin children: does parental legal status matter? J Health Soc Behav. 2015;56(1):2–18.
Arenas E, Goldman N, Pebley AR, Teruel G. Return migration to Mexico: does health matter? Demography. 2015;52(6):1853-68.
Miranda PY, Schulz AJ, Israel BA, Gonzalez HM. Context of entry and number of depressive symptoms in an older Mexican-origin immigrant population. J Immigr Minor Health. 2011;13(4):706–12.
Zúñiga V, Hernández-León R. New destinations: Mexican immigration in the United States. New York: Russell Sage Foundation; 2005.
Council NR. Hispanics and the future of America. Washington, DC: The National Academies Press; 2006.
Acknowledgements
This work was supported by a Graduate Summer Research Mentorship from the UCLA Graduate Division and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD051764 and R24HD041022).
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Supplemental Table A
(XLSX 10 kb)
Rights and permissions
About this article
Cite this article
Young, ME.D., Pebley, A.R. Legal Status, Time in the USA, and the Well-Being of Latinos in Los Angeles. J Urban Health 94, 764–775 (2017). https://doi.org/10.1007/s11524-017-0197-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-017-0197-3