Abstract
The goal of this longitudinal analysis was to characterize factors associated with the experience of life stress in low-income, inner-city mothers of minority children with high-risk asthma.Participants (n = 276) reported on family demographics, child asthma control and healthcare utilization, social support, contemporary life difficulties (housing, finances, violence exposure) measured by the validated Crisis in Family Systems scale, and daily stress. Latent growth curve modeling examined predictors of life stress across 12 months as a function of home and community difficulties, asthma-specific factors, and social support. Mothers were primarily single (73%), unemployed (55%), and living in extreme poverty with most (73%) reporting an annual family income <$20,000 (73%). The children were young (mean age = 5.59, SD = 2.17), African-American (96%), and had poorly controlled asthma (94%) at study enrollment. Higher daily stress was associated with financial difficulties, safety concerns in the home and community, and housing problems. Access to social support was consistently related to reduced stress. The only asthma-specific factor associated with life stress was healthcare utilization, with more emergency services for asthma related to higher daily stress. Findings underscore the clinical significance of assessing diverse home and community stressors and social support in low-income, inner-city caregivers of children with poorly controlled asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pediatric asthma is a common health condition affecting nearly 10 million children under the age of 18 in the USA, with higher prevalence rates in racial/ethnic minority youths [1,2,3]. Low-income minority children are likewise disproportionately impacted by asthma morbidity and mortality [4, 5]. Poorly controlled asthma is associated with negative health and social consequences for the affected child [6,7,8], as well as caregiver quality of life and increased caregiver burden, productivity loss, and financial strain [9, 10]. Achieving the goal of well-controlled asthma requires ongoing monitoring, management, and environmental control activities. However, implementing these complex self-management activities in the home may be challenging for impoverished, inner-city caregivers who encounter a range of home and community-level stressors.
Concerns about neighborhood safety [11], violence exposure [12], and residence in poor housing conditions characterized by pest infestation (rodents, cockroaches) and mold [13] were previously identified as significant hardships experienced by inner-city caregivers of children with frequent Emergency Department (ED) utilization for asthma. Extreme poverty [14], single-parent households [15], and general neighborhood disadvantage [16] further contribute to chronic stress in this population, beyond the burden of caring for a child with high-risk asthma. Additionally, in cross-sectional research with 201 mothers of inner-city children (6–12 years) with asthma, Kub and colleagues [17] observed utilities insecurity and housing instability as sources of life stress. Evidence from other cross-sectional research with families of children (5–12 years) with asthma suggests caregiver functioning is particularly compromised when several home and community difficulties are present [18]. This finding is noteworthy since racial disparities in the number of stressors reported by caregivers have been reported. For example, a community-based study of caregiver functioning, life stress, and child asthma found African-American mothers to be more likely to experience accumulating negative life events [15] that, in turn, deplete family resources and undermine adaptive coping responses [19, 20].
Since impoverished caregivers who encounter a high number of home and community hardships are more likely to endorse clinically significant depressive, anxiety, and trauma symptomatology [21, 22], and have children with greater asthma morbidity [23], it is important to identify and develop responsive interventions for the sources of life stress. However, the limited studies examining life stress experienced by caregivers of children with asthma are primarily cross-sectional and fail to differentiate the relative contribution of asthma-specific, sociodemographic, and home and community-level risk experiences on stress over time. Even less is known about whether social support, previously shown to be associated with increased child asthma control [24], may moderate the negative effects of home and community stressors. Therefore, the goal of this longitudinal analysis was to extend understanding of life stress experienced by low-income mothers of children with asthma by characterizing the unique contributions of asthma factors (asthma control level, emergency services utilization), home and community difficulties, and social support in explaining life stress. Additionally, we hypothesized that the relationships between home and community risk experiences and life stress would be moderated by caregiver level of social support.
Methods
This secondary data analysis is part of a larger randomized controlled trial that tested the effectiveness of a behavioral/educational intervention in urban families of children with frequent ED utilization for poorly controlled asthma [25]. Following institutional review board approval, families of 300 inner-city children with asthma were recruited from two major urban hospitals after the child was discharged from a Pediatric ED for an acute asthma exacerbation. A Health Insurance Portability and Accountability Act (HIPAA) waiver was used to abstract contact information during daily review of electronic ED medical records and mail caregivers study information inclusive of an opt-out letter. Caregivers who did not decline participation were contacted by the study team to ascertain study interest and eligibility: (a) child age 3–10 years; (b) physician-diagnosed asthma; (c) >2 symptom days or rescue medication use/week or 2> symptom nights/month; (d) controller medication use during the prior 6 months; (e) two or more ED visits or one hospitalization during the prior 12 months of the index ED visit; and, (f) no other major comorbid respiratory condition. Caregivers completed informed consent, randomized into a home-based standard asthma education attention control group or a behavioral/education intervention group and prospectively followed for 12 months. Research assistants administered study questionnaires during face-to-face interviews with caregivers at baseline, 6 months, and 12 months post enrollment. This sub-analysis focused on biological mothers who completed the study (n = 276).
Behavioral/Education Intervention
Families randomized to the intervention group received two home visits by a trained nurse for asthma education, completion of a written asthma action plan, and assistance in arranging a follow-up appointment with the child’s primary care provider (PCP). The intervention nurse also accompanied the mother and child to a PCP appointment as an advocate for guideline-based asthma management including preventive medication.
Standard Asthma Education Attention Control Group
Control group families received three home visits by a trained nurse providing the same asthma education as experienced by the intervention families and a prompt to schedule a follow-up appointment for the child with their PCP for asthma management.
Measures
Asthma Severity
Child asthma severity was assessed at study enrollment and based on mother report of frequency of asthma day symptoms over past 14 days and night symptoms over the past 30 days, child activity limitations due to asthma, number of ED visits, use of controller and rescue medications over the past 6 months, and number of PCP visits over past 6 months. Children were categorized as having intermittent, mild persistent, moderate persistent, or severe persistent asthma based on national asthma guidelines [26].
Asthma Control
Child asthma control level was calculated using an algorithm based on the National Asthma Education and Prevention Program (NAEPP) Guidelines [26] and included frequency of day and night cough, wheeze, and shortness of breath or difficulty breathing symptoms, rescue medication use, activity limitation, and number of ED visits and hospitalizations. Asthma control was coded as follows: well controlled = 1, not well controlled = 2, or very poorly controlled = 3.
Asthma Emergency Services Utilization
To quantify child asthma-related emergency services utilization, the number of urgent care visits, ED visits, and hospitalizations reported by mothers was summed for the prior 6 months at baseline, 6-month, and 12-month data collection.
Life Stress
Mothers were asked to quantify the level of daily stress experienced over the past month using a visual analog scale (VAS). A score of “0” indicated no stress and “10” reflected the highest possible level of life stress. A score of 6–7 suggested moderate stress, and a score of 8 or above was regarded as a high level of stress. Construct validity of the VAS is supported through moderate to high correlations with standardized measures of psychological stress [27].
Home and Community Stressors
The Crisis in Family Systems (CRISYS) was administered to the mothers as a self-report index of stressful life events experienced in the home and community [22]. Subscales of the CRISYS measure a range of contemporary stressors including the following: financial difficulties (11 items; e.g., “Did you go without food because you didn’t have the money to pay for it; Did you miss rent or mortgage payment because you couldn’t pay for it”), legal problems (3 items; e.g., “Did anyone in your family get arrested”), career challenges (4 items; e.g.,“Did you get laid off”), social relationships (6 items; e.g., “Did you get a divorce or break up with a partner”), safety concerns in the home (3 items; e.g., “Did you feel emotionally or physically abused”), safety concerns in the community (8 items; e.g., “Did anything happen in your neighborhood that made you feel unsafe; Did you see violence”), and home issues (7 items; e.g., “Did rats, mice, or insects bother you in your home; Did you have trouble with your landlord”). The dichotomized items are summed (0 = no; 1 = yes) with higher scale scores reflecting more difficulties. Construct validity was previously established through significant associations between total counts of life stressors and caregiver depressive symptomology in a comparable sample of inner-city caregivers [28].
Social Support
Participating mothers completed the eight-item emotional/informational support subscale of the Medical Outcomes Study (MOS) as a self-report measure of social support [29]. Mothers described how available social support was to them across scenarios (e.g., “Someone you can count on to listen to you when you need to talk; “Someone to turn to for suggestions about how to deal with a personal problem”), with higher scores indicating greater perceived social support (score range 8–40).
Data Analysis
Data Analysis Plan
Latent growth curve modeling (LGCM) using Mplus version 6 [30] was performed to examine changes in daily life stress over the 12-month time period. Data in LGCM are described by latent change factors (i.e., means and slopes) that estimate both group-level change and individual-level change. Intercept values were estimated by fixing factor loadings at each time point to one. Slope values were then estimated by assigning fixed factor loading representing time (baseline = T1; 6 months = T2; 12 months = T3). Maximum-likelihood estimation with robust standard errors (MLR) was used to address missing data that never exceeded 10% for any variable. Based on α = .05 and β = .80, a priori power analysis indicated a minimum sample of 217 for testing the structure of the LGCM (RMSEA <.10), and a minimum sample of 152 for testing individual parameters (b >0) [31, 32]. Guidelines provided by Hu and Bentler [33] and Kline [34] were used as model fit criteria (RMSEA <.05, CFI/TLI >.90, SRMS <.08). One-tailed tests were used in the analyses with directionality based on previous research.
The outcome variable of interest was the level of caregiver daily life stress measured at each time point at (T1), (T2), and (T3). Independent control variables measured at (T1) were treatment group assignment (intervention vs. control), child’s age, mother’s education level, marital status, employment status, and baseline asthma severity. Time-varying covariates in the model measured at (T1), (T2), and (T3) included social support, asthma control level, emergency services utilization for asthma, and the seven subscales of the CRISYS. Interactions between social support and CRISYS subscales were also tested. Assumptions of parametric analyses were assessed and only minor violations in normal distributions were noted with minimal impact based on study sample size.
Results
Participants were primarily single (73.4%), unemployed (55.4%), and living in extreme poverty, with over half of the mothers reporting an annual family income of less than $10,000 USD (51.7%) (Table 1). Most caregivers had graduated from high school or received their GED (39.3%) or attended some college or trade school (28.4%). The children were young (mean age = 5.59, SD = 2.17), African-American (95.7%), male (59.4%), and nearly all were categorized with poorly controlled asthma (93.8%) at study enrollment [26]. The children averaged 7.32 asthma symptoms days (e.g., cough, wheeze, shortness of breath) (SD = 5.32) and 6.72 asthma symptom nights (SD = 5.61) over the prior 2 weeks at baseline. High emergency services for asthma was reported for the children. Mean ED and urgent care visits were 3.34 (SD 3.28) and 1.37 (SD 2.43), respectively, during the previous 6-month period. Over one quarter of the children (28.3%) had experienced at least one hospitalization.
Forty percent of mothers (40.3%) were categorized as experiencing high daily life stress at baseline (M = 6.42, SD = 2.86), and over a fifth (20.9%) endorsed the highest possible stress score of 10 on the VAS. The mothers reported diverse home and community hardships based on responses to the CRYSIS subscales. In total, participants endorsed a mean of 8.17 (SD = 5.05) stressful life events in the previous 6-month period and over a third of the mothers (35.7%) experienced 10 or more stressors. The most frequently reported home and community hardships were as follows: [1] looking for a job (56.0%); [2] utility or phone company threatening to cut off service because bills not paid (52.7%); [3] evidence of rats, mice, or insects in home (49.1%); [4] missed an appointment or changed plans because of no transportation (41.9%); [5] violence heard outside of home (38.7%); and [6] witnessing drug dealing in building or neighborhood (38.7%). Most mothers reported access to emotional/instrumental support, with 72.1% scoring at 30 or above on the MOS social support scale (range 8–40) at baseline.
Latent Growth Curve Model Results
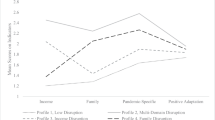
LGC model analyses were used to assess changes in life stress over time as a function of child asthma control, asthma-related emergency services utilization, home and community hardships, and social support. Fit statistics for the nested models are presented in Table 2. Results presented below are unstandardized parameter estimates. An unconditional model using only life stress over time was tested first. Results for the intercept and slope were 6.34 (p < .001, 95% CI 6.01, 6.67) and −.56 (p < .001, 95% CI −.76, −.36), respectively. The statistically significant and positive intercept indicates that the mean daily life stress score was greater than 0 over time; the statistically significant and negative slope indicates that daily life stress scores decreased across the 12-month study.
Baseline (T1) control variables and time-varying covariates (T1, T2, T3) were added to create a second LGC model. Results for the second model indicate good fit as evidenced by a RMSEA of .03, high values for CFI (.95) and TFI (.91), and a SRMR of .02. Results for the second model identified a significant positive intercept (I = 10.07, p < .001, 95% CI 6.35,13.79) and a negative but non-statistically significant slope (S = −1.95, p = .10, 95% CI −4.95, 1.05). Post hoc analysis indicated that the slope was quadratic in nature: there was a negative slope from T1 to T2 but the slope flattened out from T2 to T3. There were no statistically significant parameter estimates for any of the control variables on the slope intercept, which suggests that life stress was not associated with any of the baseline (T1) characteristics.
Parameters were also estimated for the observed direct effects of the time-varying covariates on daily life stress at each time point (T1, T2, and T3). Unstandardized parameter estimates and p values are provided in text, and unstandardized and standardized parameter estimates with confidence intervals are provided in Table 3. No statistically significant relationships were detected between child asthma control level and maternal life stress at any time point. Additionally, asthma-related emergency services utilization was only a statistically significant predictor of stress at baseline (b = .06, p = .002).
In contrast, self-reported daily stress had more robust relationships with maternal social support and the CRISYS subscales measuring home and community hardships. Specifically, social support was associated with daily life stress at baseline (T1) (b = −.06, p = .001), 6 months (T2) (b = −.08, p < .001), and 12 months (T3) (b = −.06, p = .02), with increased emotional/informational support related to decreased life stress in this sample of mothers residing in extreme urban poverty. Parameter estimates were also obtained for each of the CRISYS subscales: financial difficulties, legal problems, career challenges, social relationships, safety concerns in the home, safety concerns in the community, and home issues. Financial difficulties were found to be statistically significant predictors of daily life stress at all three time points, T1 (b = .21, p = .01), T2 (b = .21, p = .01), and T3 (b = .20, p = .02). Safety concerns in the home were not statistically significant at T1 (b = .35, p = .19) or T2 (b = −1.35, p = .12) but achieved significance at T3 (b = .94, p = .03), with increased trauma exposure associated with higher maternal life stress. Statistically significant parameters were also detected for community safety concerns at baseline (b = .29, p = .003) and 12 months (b = .23, p = .03) with more violence and crime exposure associated with increased daily stress. Significant findings were likewise observed for the home issues subscale, with a greater number of negative home challenges related to maternal life stress at T2 (b = .39, p = .02). No statistically significant relationships were identified between career challenges, legal problems, social relationships, and daily stress.
The third nested model incorporated interaction effects between social support and each CRISYS subscale at T1, T2, and T3. None of the interaction terms were statistically significant at any time point (p > .10) and fit statistics were comparable across models 2 and 3 (Table 2). Consequently, model 2, the covariates model, is the more parsimonious model and was chosen as the final model.
Discussion
In this sample of low-income, urban mothers of children with poorly controlled asthma, home and community hardships were more consistently associated with self-reported life stress compared to asthma-specific risk factors. Although asthma morbidity was high and previous qualitative research revealed psychological distress about raising a child with moderate to severe asthma [35, 36], neither asthma control nor asthma severity was predictive of life stress. Furthermore, despite frequent ED and urgent care services for asthma, life stress was only associated with emergency services utilization at a single time point. Instead, diverse risk experiences at home and in the community appear to be major contributors to the elevated rates of self-reported life stress in this sample of low-income, inner-city mothers. The range and frequency of negative life events reported by participants is a particularly noteworthy and innovative finding that helps address previous calls for increased understanding of the family’s context [37]. Financial strains, concerns about safety in the home, concerns about violence and crime in the community, and housing difficulties were each independently predictive of life stress over time. Due to the extreme poverty of these families, it was not surprising that financial concerns emerged as a consistent predictor of daily life stress. Focus group research with low-income caregivers of children with poorly controlled asthma revealed a profound psychological toll of poverty, particularly related to caregiver ability to achieve optimal asthma management and home environmental control responsibilities [13].
The scope of safety concerns in the home and community reported by study participants is alarming yet consistent with findings on life events and chronic stress in a comparable sample of low-income mothers who reported seeing violence (20%) and feeling unsafe (23%) in their communities [17]. Ameliorating community violence exposure is a challenging public health endeavor, but one that must be addressed based on the current findings of a negative impact of safety concerns on life stress, as well as prior research linking fears about community violence exposure to poor healthcare follow-up rates and low adherence to asthma management routines [38] and erosion of family functioning and stability [39]. Complete remediation of community-based violence and crime may be difficult to achieve, so implementing violence reduction programs in tandem with interventions strengthening family coping in the context of ongoing trauma exposures may be necessary. Supporting evidence for targeting caregiver coping skills comes from earlier asthma research with a sample of ethnically diverse families in which adaptive coping was associated with higher child quality of life outcomes [40]. Other research suggests positive family outcomes, such as enhanced empowerment and caregiver well-being, may be generated through family-to-family support and advocacy programs [41, 42].
Housing difficulties were likewise associated with higher daily life stress in these vulnerable mothers. In fact, home rodent infestation was one of the most commonly reported negative life events, comparable to rates observed in a sample of urban Puerto Rican families of children with asthma [43]. Addressing poor housing stock is particularly critical since, beyond its relationship with elevated caregiver life stress, environmental exposures stemming from sub-standard housing were associated with higher rates of ED visits in children with asthma aged 6–17 years [44]. Recommendations to improve the quality of housing stock include implementing healthy housing guidelines for new construction, increased enforcement of housing codes, and home visiting education and environmental intervention programs to reduce trigger exposures [45]. However, these interventions may be less feasible in low-income communities with limited resources and options for change in housing quality.
Social support also emerged as a consistent predictor of life stress, with high levels of emotional/informational support associated with reduced life stress in the mothers. Social support was previously identified as a salient factor to explore in relation to child asthma functional morbidity and second-hand smoke exposure [23], and our findings similarly emphasize its importance as a potential protective mechanism for self-reported life stress. However, contrary to expectations, social support failed to moderate the observed relationships between home and community hardships and life stress. This may be due to the shared environment in which neighbors who are providing support are likewise experiencing the same home and community difficulties.
Finally, increased understanding of the chronic nature of stress in low-income mothers of children with asthma is significant. Although life stress decreased over time, half (50.2%) of the mothers consistently reported moderate-to-high levels of stress at 12 months and nearly a third (31.6%) endorsed scores in the high range (8 or above). The chronicity of stress is most concerning since it may erode coping skills in family systems [46], leave mothers feeling overwhelmed, and perhaps ineffective, in asthma home management, and ultimately result in increased asthma morbidity. This assertion is partly supported by research with a community-based sample of caregiver-child dyads in which higher caregiver stress was associated with poorer child asthma control [47].
Collectively, study findings highlight the need for intensive, multi-faceted interventions to support mothers as they manage their child’s asthma in the context of ongoing, high-acuity home and community hardships. Screening for a range of stressors (financial difficulties, safety concerns, home issues) is an important initial step to engage mothers of children with poorly controlled asthma and help them feel supported. However, provider-caregiver interactions must extend beyond the clinical assessment process to link mothers with comprehensive community resources that may ameliorate identified stressors. Yet, pediatric asthma healthcare delivery systems, and particularly ED-based care, typically lack the necessary case management services to effectively connect caregivers to community supports and provide a bridge for the range of systems (school, behavioral health, child welfare) that the family may be involved with [48].
Limitations and Future Directions
Study findings are to be interpreted cautiously due to the inability to rule out common method variance (e.g., reliance on self-report measures) as a contributing factor for the observed significant relationships. Future research would benefit from including more than one data source and, ideally, objective community-level data on violence and crime rates as well as the quality of housing stock where participants reside. Examining whether the accumulating risks are related to particular negative health outcomes in caregivers is also a fertile area for continued research. Although correlations among stress and depressive symptomology have long been established, less is known about how elevated rates of life stress are associated with health conditions in low-income mothers of children with asthma. However, in a mixed-method study with 40 low-income caregivers of children with asthma, nearly all participants were found to have a health condition of their own [14]. The lack of longitudinal data for caregiver sociodemographics presents other limitations. Marital status, education level, family income, and employment status were only assessed at baseline. Although some of these constructs were included in the CRISYS subscales, we were unable to test whether changes in discrete sociodemographic variables over time (e.g., employment status T1 to T2) contributed to variation in stress scores. Finally, findings may not be representative of all low-income, inner-city families since the current sample was comprised of mothers who agreed to participate and were able to be tracked across 12 months. It is possible that mothers who experience the most extreme levels of home and community hardships were not captured in the study sample.
Despite these limitations, our longitudinal study is innovative in that the results focus on characterizing specific home and community hardships contributing to the elevated rates of life stress in low-income mothers of young children with high-risk asthma. Findings underscore the importance of assessing for diverse sources of stress in mothers of high-risk children with asthma. In particular, regular screening for financial difficulties to include concerns about utilities stability, exposure to violence in the home and broader social context, and poor housing conditions are salient domains to explore in clinical encounters with inner-city mothers of children with poorly controlled asthma.
References
Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, Liu X. (2012) Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS data brief, no 94. Hyattsville, MD: National Center for Health Statistics.
Bloom B, Jones LI, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey. National Center for Health Statistics. Vital Health Stat. 2013;10(258):1–73.
Thakur N, Oh SS, Nguyen EA, Martin M, Roth LA, Galanter J, et al. Socioeconomic status and childhood asthma in urban minority youths. The GALA II and SAGE II studies. Am J Respir Crit Care Med. 2013;188(10):1202–9.
Akinbami L, Moorman J, Lui X. (2011) Asthma Prevalence, Health Care Use, and Mortality United States, 2005–2009. Hyattsville, MD: U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
Celano MP, Holsey CN, Kobrynski LJ. Home-based family intervention for low-income children with asthma: a randomized controlled pilot study. J Fam Psychol. 2012;26(2):171–8.
Amaral LMD, Moratelli L, Palma PV, Leite ICG. The quality of life of Brazilian adolescents with asthma: associated clinical and sociodemographic factors. J Asthma. 2014;51:660–6.
Booster GD, Oland AA, Bender BG. Psychosocial factors in severe pediatric asthma. Immunol Allergy Clin N Am. 2016;36(3):449–60.
Wildhaber J, Carroll WD, Brand PL. Global impact of asthma on children and adolescents’ daily lives: the room to breathe survey. Pediatr Pulmonol. 2012;47(4):346–57.
Dean BB, Calimlim BM, Kindermann SL, Khandker RK, Tinkelman D. The impact of uncontrolled asthma on absenteeism and health-related quality of life. J Asthma. 2009;46(9):861–6.
Dean BB, Calimlim BC, Sacco P, Aguilar D, Maykut R, Tinkelman D. Uncontrolled asthma: assessing quality of life and productivity of children and their caregivers using a cross-sectional internet-based survey. Health Qual Life Outcomes. 2010;8:1–10.
Kopel LS, Gaffin JM, Ozonoff A, Rao DR, Sheehan WJ, Friedlander JL, Pl P, Baxi SN, Fu C, Subramanian SV, Gold DR, Phipatanakul W. Perceived neighborhood safety and asthma morbidity in the school inner-city asthma study. Pediatr Pulmonol. 2015;50(1):17–24.
Authors. The influence of community violence and protective factors on asthma morbidity and healthcare utilization in high-risk children. J Urban Health (2014); 91:677–689.
Authors. Caregiver perception of asthma management of children in the context of poverty. J Asthma 2016; 15 (June), 1–11 .
Sampson MNR, Parker EA, Cheezum MRR, Lewis TC, O’Toole MA, Patton MJ, Keirns CC. A life course perspective on stress and health among caregivers of children with asthma in Detroit. Fam Community Health. 2013;36(1):51–62. 6.
Shalowitz MU, Mijanovich T, Berry CA, Clark-Kauffman E, Quinn KA, Perez EL. Context matters: a community-based study of maternal mental health, life stressors, social support, and children’s asthma. Pediatr. 2006;117:e940–8.
Williams DR, Sternthal M, Wright RJ. Social determinants: taking the social context of asthma seriously. Pediatr. 2009;123(Suppl.3):S174–84.
Kub J, Jennings JM, Donithan M, Walker JM, Land CL, Butz A. Life events, chronic stressors, and depressive symptoms in low-income urban mothers with asthma children. Public Health Nurs. 2009;26:297–306.
Everhart RS, Fiese BH, Smyth JM. A cumulative risk model predicting caregiver quality of life in pediatric asthma. J Pediatr Psychol. 2008;33(8):809–18.
Kiser LJ, Medoff DR, Black MM. The role of family processes in childhood traumatic stress reactions for youths living in urban poverty. Traumatology. 2010;26:33–42.
Patterson JM, McCubbin HI. The impact of family life events and changes on the health of a chronically ill child. Fam Relat. 1983;32:255–64.
Kiser LJ, Donohue A, Hodgkinson S, Medoff D, Black MM. Strengthening family coping resources: the feasibility of a multifamily group intervention for families exposed to trauma. J Trauma Stress. 2010;23:802–6.
Shalowitz MU, Berry CA, Rasinski KA, Dannhausen-Brun CA. A new measure of contemporary life stress: development, validation, and reliability of the CRISYS. Health Serv Res. 1998;33(5):1381–402.
Clawson AH, Borrelli B, McQuaid EL, Dunsiger S. The role of caregiver social support, depressed mood, and perceived stress in changes in pediatric secondhand smoke exposure and asthma functional morbidity following an asthma exacerbation. Health Psychol. 2016;35(6):541–51.
Scheckner B, Arcoleo K, Feldman JM. The effect of parental social support and acculturation on childhood asthma control. J Asthma. 2015;52:606–13.
Authors. Improving preventive care in high risk children with asthma: Lessons learned. J Asthma 2014; 51:498–507.
U.S. Department of Health and Human Services. (2007) The National Asthma Education and Prevention Program. Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Washington, DC.
Lesage FX, Beriot S, Deschamps F. Clinical stress assessment using a visual analogue scale. Occup Med. 2012;62:600–5.
Berry C, Shalowtiz M, Quinn K, Wolf R. Validation of the crisis in family systems-revised, a contemporary measure of life stressors. Psychol Report. 2001;88:713–24.
Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–14.
Muthén LK, Muthén BO. Mplus User’s Guide (6th ed.) 2011. Los Angeles, CA: Muthén & Muthén.
Preacher KJ, Coffman DL. (2006) Computing power and minimum sample size for RMSEA [Computer software]. Available from http://quantpsy.org/.
Soper DS. (2013) A-priori sample size calculator for structural equation models [Software]. Available from http://www.danielsoper.com/statcalc
Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55.
Kline RB. Principles and Practices of Structural Equation Modeling 2005. New York, NY: Guilford Press.
Chen S-H, Huang J-L, Yeh K-W, Tsai Y-F. The stress of caring for children with asthma: a qualitative study of primary caregivers. J Nurs Res. 2015;23:298–307.
Laster N, Holsey CN, Shendell DG, McCarty FA, Celano M. Barriers to asthma management among urban families: caregiver and child perspectives. J Asthma. 2009;46:731–9.
Cloutier MM. Considerations in culturally directed asthma disease management programs. Dis Manag Health Out. 2008;16(2):95–105.
Wright RJ, Mitchell H, Visness CM, Cohen S, Stout J, Evans R, Gold DR. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health 2004. 2004;94(4):625–32.
Collins KS, Strieder FH, DePanfilis D, Tabor M, Clarkson-Freeman PA, Linde L, Greenberg P. Trauma Adapted Family Connections (TA-FC). Child Welfare. 2011;90(6):29–47.
Sales J, Fivush R, Teague GW. The role of parental coping in children with asthma’s psychological well-being and asthma-related quality of life. J Ped Psychol. 2008;333(2):208–19.
Hoagwood KE, Cavaleri MA, Olin SS, Burns BJ, Slaton E, Gruttadaro D, Hughes R. Family support in children’s mental health: a review and synthesis. Clin Child Family Psychol Rev. 2010;13:1–45.
Robbins V, Johnston J, Barnett H, Hobstetter W, Kutash K, Duchnowski AJ, Annis S. (2008) Parent to Parent: a Synthesis of the Emerging Literature. Tampa, FL: University of South Florida, The Louis de la Parte Florida Mental Health Institute, Department of Child & Family Studies.
Martin MA, Press VG, Nyenhuis SM, Krishman JA, Erwin K, Mosnaim G, Margellos-Anast H, Paik SM, Ignoffo W, McDermott M. Chicago Plan Consortium. Care transition interventions for children with asthma in the emergency department. J Allergy Clin Immunol. 2016;138(6):1518–25.
Hughes HK, Matsui EC, Tschudy MM, Pollack CE, Keet CA. (2016) Pediatric asthma health disparities: race, hardship, housing, and asthma in a national survey. Acad Pediatr 19.
Krieger J. Home is where the triggers are: increasing asthma control by improving the home environment. Pediatr Allergy Immunol Pulm. 2010;23(2):139–45.
Kiser LJ, Black MM. Family processes in the midst of urban poverty: what does the trauma literature tell us? Aggress Violent Behav. 2005;10:715–50.
Sharp LK, Curtis LM, Mosnaim G, Shalowitz MU, Catrambone C, Sadowski LS. The influence of caregiver’s psychosocial status on childhood asthma and obesity. Ann Allergy Asthma Immunol. 2009;103(5):386–94.
Martin MA, Thomas AM, Mosnaim G, Greve M, Swider SM, Rothschild SK. Home asthma triggers: barriers to asthma control in Chicago Puerto Rican children. J Health Care Underserved. 2013;24(2):813–27.
Acknowledgements
All phases of this study were supported by a National Institute of Nursing Research, NIH grant NR010546. This clinical trial is registered with www.clinicaltrials.gov and the registration number is NCT00860418. We thank the participating families for their time invested in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bellin, M.H., Collins, K.S., Osteen, P. et al. Characterization of Stress in Low-Income, Inner-City Mothers of Children with Poorly Controlled Asthma. J Urban Health 94, 814–823 (2017). https://doi.org/10.1007/s11524-017-0162-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-017-0162-1