Abstract
Young adult transgender men who have sex with men (TMSM) engage in sexual behaviors that place them at risk of sexually transmitted infections (STIs) including HIV. To date, no HIV and STI prevention interventions have been developed specifically for young adult TMSM. To address this gap, the current study aimed to (1) adapt a small group-based behavioral HIV prevention intervention designed for young transgender women (“LifeSkills”) to address the unique HIV and STI prevention needs of young TMSM ages 18–29 years and (2) conduct a pilot evaluation of the intervention (“LifeSkills for Men”; LS4M). LS4M was carried out in an iterative approach with community input along the way, which allowed for refinement of the intervention manual and enhanced participant acceptability. A LS4M Task Force was convened to guide intervention development/adaptation and study implementation. Initially, focus groups were conducted to examine the sexual health needs, concerns, and stressors facing young TMSM (n = 12; mean age = 23.8 years; 16.7 % people of color). Next, LS4M was pilot tested (n = 17; mean age = 24.3 years; 23.5 % people of color) to assess acceptability with the study population and feasibility of all study procedures. Overall attendance, participation rates, and positive feedback from participants demonstrate that LS4M is highly acceptable and feasible to carry out with young TMSM. Trends in outcome measures across 4 months of follow-up suggest that participation in the intervention may improve mental health, reduce internalized stigma, and reduce HIV- and STI-related risk behaviors. Further testing of the intervention enrolling young TMSM with recent sexual risk behavior at baseline and with a control group is warranted. Lessons learned for future work with young TMSM are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
US youth age 29 years and younger represent a population at risk of sexually transmitted infections (STIs), including HIV.1–3 Youth ages 13–24 years accounted for an estimated 26 % of all new HIV infections in the USA in 2010, and some of the highest STI rates in the USA are in youth ages 20–24 years. Little research has been conducted on HIV and STIs in transgender youth who have a current gender identity or expression that differs from their assigned sex at birth, and existing research is most often focused in young transgender women.4–7 Young transgender men—assigned a female sex at birth who are identified as male, men, female-to-male (FTM), transgender men, gender nonconforming, and non-binary or have another diverse gender identity or expression on the trans masculine continuum—remain largely invisible.
Transgender men are often assumed to be heterosexual—meaning they have sex with cisgender (non-transgender) females only—and are therefore often perceived to be at low risk for HIV and STIs.8 This erroneous assumption may in part account for the dearth of research in transgender men, including among youth. In actuality, research highlights the heterogeneity of sexual identities and behaviors among transgender men.9–12 For example, according to data from the U.S. National Transgender Discrimination Survey among 2578 transgender men, the vast majority (82 %) were non-heterosexual identifying their sexual orientation as 19 % gay, 12 % bisexual, and 51 % queer.13 Burgeoning research shows that transgender men who have sex with cisgender males (TMSMs) engage in sexual risk behaviors that place them at risk of HIV and STIs.9,10,13,14 TMSM remain a unique and understudied population warranting further study to better characterize and understand how the intersection of gender identity and sexual orientation influence HIV and STI risk behaviors, particularly for young TMSM who must navigate socially stigmatized gender and sexual identities alongside routine developmental tasks which affects their sexual health.
Sexual minority stress theory hypothesizes that health disparities for gay or bisexual MSM are due to the differential distribution of social stress processes (e.g., discrimination, victimization, mistreatment, internalized homophobia) experienced as the result of a disadvantaged social status in society.15–17 Although sexual minority stress data are lacking specific to young TMSM, sexual minority stress has been shown to correlate with HIV transmission risk behaviors among cisgender young MSM.18,19 Qualitative data suggest that TMSM contend with additional layers of stigma, including rejection from cisgender MSM and fear of or anticipated rejection from cisgender males (e.g., internalized transphobia) for being transgender and/or not being socially affirmed or recognized as men.9 This fear may manifest behaviorally in TMSM-specific HIV-related risks linked to social and psychological gender affirmation.9
Gender affirmation is the desire or need to be affirmed by others in one’s self-identified gender and is a key determinant of wellbeing for young transgender adults.20 Gender affirmation is a dynamic process that can include social (e.g., name, pronoun, gender expression), medical (e.g., cross-sex hormones, surgery), legal (e.g., name and gender marker change), and psychological (e.g., internalized transphobia) dimensions.21,22 Gender affirmation was first theorized and linked to HIV risk behavior in transgender women of color.23 Since then, recent studies have shown that TMSM may engage in sexual risk behaviors to affirm their gender, with a qualitative study of TMSM describing how the desire for gender affirmation or validation through sexual interactions with their cisgender male partners often supersedes their desire to protect themselves from HIV and STIs.9 This risk may be particularly evident in young TMSM who are emerging adults, as they navigate routine developmental tasks such as accomplishing identity consolidation which may include sexual experimentation to explore aspects of their gender and sexual identities, establishing healthy peer and intimate relationships, and managing family stressors and pressures and achieving personal autonomy.24 HIV and STI prevention and intervention efforts are warranted that consider developmental factors alongside gender and sexuality development in sexual risk behaviors for young TMSM.
To our knowledge, no HIV and STI prevention interventions have yet been developed for young TMSM. However, behavioral interventions have shown promise for empowering young transgender women to protect their sexual health.25 “LifeSkills” is a theoretically driven small group-based behavioral HIV prevention intervention designed to address the unique lived realities driving HIV risk in young transgender women, originally developed by and for young transgender women in Chicago, and is now being tested in the context of an R01 efficacy trial.25 The current study aimed to adapt a small group-based behavioral HIV prevention intervention designed for young transgender women (LifeSkills) to address the unique HIV and STI prevention needs of young TMSM ages 18–29 years and conduct a pilot evaluation of the intervention (“LifeSkills for Men”; LS4M). LS4M was carried out using an innovative intervention refinement process, which allowed for refinement of the intervention manual and enhanced participant acceptability.
Method
Guiding Conceptual Frameworks for Intervention with Young TMSM
The original LifeSkills intervention with young transgender women was based in Brofenbrenner’s social-ecological model,26 a developmentally focused framework which heuristically situates individual behavior in multi-level contexts (e.g., social, cultural, structural).25 The adapted LifeSkills for Men (LS4M) intervention uses a modified social ecological model of HIV risk27 to conceptualize the multiple contexts and dimensions of sexual risk behaviors for young TMSM.
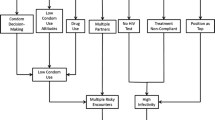
LS4M integrates three additional conceptual frameworks relevant for young TMSM: (1) the sexual minority stress theory has been linked to health disparities among sexual minorities,15–17 including the acquisition of HIV among cisgender MSM.18 Given that TMSM experience unique stressors related to their gender identity and sexuality (homophobia, transphobia, and internalized transphobia and homophobia), intervention components were developed to address these experiences among TMSM. (2) Gender affirmation was applied to understand existing and hypothesized HIV and STI risk behaviors in young adult TMSM. The desire or need to be affirmed by others in one’s self-identified gender is a key determinant of well-being for young adult TMSM. (3) The information, motivation, and behavioral skills (IMB) model, a health behavior change model previously used in development of prevention interventions for youth in diverse settings,28–31 was integrated to address sexual risk behaviors.32 IMB was applied to HIV and STI prevention by providing young TMSM information and knowledge about safer sex behaviors, addressing young TMSM’s motivations to perform safer sex behaviors, and empowering young TMSM to gain the behavioral skills necessary to perform safer sex behaviors across different hook-up scenarios, partnership types, and sexual situations.
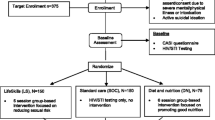
Approach to Intervention Adaptation and Development
A staged intervention approach33 was used to adapt and evaluate a behavioral HIV and STI prevention intervention with young adult TMSM ages 18 to 29 years in 2013–2014. The approach included the following: (1) a task force comprised of community members; (2) focus groups with young TMSM to formatively examine the sexual health needs, concerns, and stressors facing young TMSM; (3) iterative design and writing of the LS4M intervention curriculum with study team and TMSM community members; and (4) pilot test of the intervention to examine initial acceptability and feasibility. Throughout all steps of intervention development, community-based participatory research (CBPR) principles34 were used to ensure research conducted was “with” not “on” young TMSM. CBPR principles were chosen to maximize the potential impact and sustainability of the intervention by engaging with and helping to strengthen existing “on the ground” young TMSM community networks and infrastructure. Young TMSM’s unique experiences directly informed and shaped the context, content, and delivery of the intervention ensuring the developmental-appropriateness of LS4M.
Task Force
A task force comprised of community members (n = 6) was convened to guide the study course and implementation, including development of survey items and gender-affirming sexual risk assessment measures, intervention design and content, recruitment and retention efforts, dissemination of findings, etc. LS4M Task Force members were purposively selected by the implementing study team in Boston (SR, DP) through their interpersonal connections to the target population. LS4M Task Force members were engaged as members of the target population (e.g., TMSM individuals age 18 to 29 years) or as “older brothers” of the target population who were highly experienced working within and as part of local Boston area trans masculine communities. Three LS4M Task Force meetings were convened over the study period. Dinner and a $50 gift card were provided as compensation for Task Force participation at each meeting. Online consultation with the LS4M Task Force occurred regularly throughout the study.
Focus Groups
Three focus groups were conducted with young TMSM (totaling n = 12 participants; mean age = 23.8 years; 16.7 % people of color; POC) in the Boston, Massachusetts area to formatively examine the sexual health needs, concerns, and stressors facing young TMSM and guide intervention development. Participants were recruited via flyers at Fenway Health, online postings such as Facebook, from LS4M Task Force members’ networks, and venue-based recruitment such as community events. Participants were screened by trained study staff on the telephone and were considered eligible for the focus groups and pilot (see “Open-Phase Pilot” below) if they met the following five criteria: (1) were age 18 to 29 years; (2) assigned a female sex at birth; (3) self-identified as a transgender man, FTM, man, male, or another diverse gender identity on the trans masculine spectrum; (3) reported any sexual contact (digital penetrative, oral, frontal, and/or anal sex—protected or unprotected) with a cisgender (non-transgender) man in the last 12 months prior to screening; (4) were able to speak and read English; and (5) lived in the Boston metropolitan area.
In addition to completing a qualitative focus group (1 h), participants also completed a self-administered quantitative survey via iPad (1 h), which included a sexual risk measure that was adapted by the LS4M Task Force and study team specifically for the young TMSM study population.35 Dinner and a $25 gift card were provided as compensation for participation. Each focus group discussion was facilitated by two members of the target population using a semi-structured qualitative focus group guide. Focus groups were audio recorded, transcribed verbatim, and analyzed inductively by two independent coders using methods of constant comparative analysis.36
Iterative Design and Development of the LS4M Intervention Curriculum
LS4M Task Force input and focus group data were used to design the LS4M intervention, including a manualized curriculum written by members of the study team (SR, DP) in collaboration with a local community member experienced in facilitating local group programs with the target population. Members of the target study population collaborated with the team to refine the manualized curriculum in order to ensure the intervention consisted of developmentally appropriate scenarios and themes reflecting the unique experiences of young TMSM. Development and design of the LS4M intervention was iterative. The study team drafted intervention content; LS4M Task Force members reviewed, offered feedback and suggestions; and the study team revised activities and content accordingly. The adapted LS4M intervention is comprised of four consecutive weekly small-group sessions, approximately 2 h in length each (1 month, 8 h of content). LS4M intervention sessions and content are outlined in Table 1.
Open-Phase Pilot
Recruitment methods and study eligibility for the open-phase pilot were the same as for focus groups (see criteria above). For the open-phase pilot, individual in-person study visits were conducted at baseline and at 4 months post-intervention. The baseline study visit consisted of informed consent process, quantitative survey via ACASI, and a life history calendar interview of sexual and gender development.37–41 The open-phase pilot of LS4M enrolled 18 young TMSM across 3 cohorts (cohort 1 n = 7; cohort 2 n = 4; cohort 3 n = 7).
Intervention Acceptability and Satisfaction
At baseline, in addition to the survey and life history interview, participants completed a brief semi-structured qualitative interview to solicit feedback about the quantitative survey. At 4 months post-intervention, a qualitative exit interview and evaluation survey were used to assess intervention acceptability and satisfaction.
Measures
Sociodemographics
Age was assessed in years. Race and ethnicity were assessed separately and coded as White (non-Hispanic) vs. people of color (POC = Black, Latino, multiracial, other race/ethnicity) due to small sample size. For education, participant responses were coded as some college or less vs. college graduate or more. For employment, participant responses were coded as employed full-time, employed part-time, and unemployed. Participant responses regarding their educational attainment were coded as college degree or higher vs. less than a college degree. Gender identity was coded as male, transgender man/FTM, genderqueer/non-binary, and agender. Sexual orientation identity was assessed by asking how they describe their sexual orientation today. Participant responses included gay/same-gender attraction, bisexual, queer, pansexual, asexual, and other. Sources of current income were also assessed and included the following options (yes/no): “under the table” employment, income from friends, family or partner, student stipend, SSI or disability, street income, selling or dealing drugs, and sex work.
Psychosocial Health Indicators
Five psychosocial health indicators were investigated.
-
1.
The validated 10-item Transgender Adaptation and Integration Measure (TG-AIM)42 was adapted for young transgender men and assessed how often (never, rarely, occasionally, frequently) participants had experienced a variety of mental health and social outcomes such as, “I see/have seen a mental health professional about my gender in the past 4 months” or “In the past 4 months, my gender has interfered with my quality of life.” The items were summed, with a higher mean TG-AIM score indicating greater gender identity adaptation and integration.
-
2.
Three measures of stigmatization based on sexual orientation and gender identity were developed to assess the extent to which participants perceived, experienced, and internalized transphobia and homophobia. The measure included three domains: internalized homophobia, other people’s attitudes and beliefs, and experienced transgender male stigma. On a scale from 1 to 7, the four-item internalized homophobia domain asked participants to indicate on how strongly they agreed or disagreed with statements like, “Sometimes I dislike myself for being gay/ bisexual/ queer/ attracted to men.” Using a four-item Likert scale, the other people’s attitudes and beliefs domain asked participants how strongly they agree with statements like, “Most cisgender men do not see transgender men as “real” men.” Finally, the three-item cisgender male stigma domain used a four-item Likert scale to assess how often (never to many times) participants had experienced stigma as a trans person in the context of a sexual encounter with a cisgender male. The domain included item such as, “I have been mis-pronouned during or after sex” or “I have been disrespected by having my body referred to by words/ terms that I felt uncomfortable with.” Items in each domain were summed, with higher scores indicated greater stigmatization.
-
3.
The 18-item Brief Symptom Inventory assessed psychological distress and psychiatric disorders.43 On a scale from 0 (not at all) to 4 (extremely), participants were asked to indicate how much they felt distressed by symptoms in the past 7 days including “Faintness of dizziness,” “Feeling lonely,” or “Feelings of worthlessness.” The items were then summed with higher scores indicating greater distress in the past week.
-
4.
The collective self-esteem scale44 assessed thoughts and feelings associated with being a member of the transgender community. A shortened version of the scale was used and adapted to denote participant membership in transgender community. Four subscales (membership self-esteem, private collective self-esteem, public collective self-esteem, and importance to identity) consisting of two questions asked participants to indicate how strongly they agreed or disagreed (1 = “strongly disagree” to 7 = “strongly agree”) with items like, “Overall, the trans or gender non-conforming community is considered good by others” or “the trans or gender non-conforming community I belong to is unimportant to my sense of what kind of a person I am.” Higher scores on each subscale are indicative of greater collective self-esteem in that domain.
-
5.
Substance use was assessed by asking participants to indicate how frequently (from 0 = did not use to 5 = daily) they had used drugs (marijuana, cocaine, crack, heroin, ecstasy, GHB, LSD, crystal methamphetamine, amphetamine, poppers, other drugs) in the past 4 months. Binge drinking was also assessed by asking participants, “In the past 4 months, how many times did you drink 5 or more alcohol drinks over a few hours?” (responses 0 = none to 5 = 4 or more times). Participants reporting any binge drinking or drug use in the past 4 months were coded as 1 (referent no use = 0). Binary substance use variables were summed to create a continuous measure of substance use in the past 4 months. The use of any drug in the past 4 months was coded as yes/no, while the use of two or more drugs (polydrug use) was coded as yes (referent = no).
Sexual Health Knowledge and Efficacy Indicators
Four sexual health knowledge and efficacy indicators were assessed. (1) The 10-item behavioral skills sub-scale from the information, motivation, and behavioral skills (IMB) measure45,46 assessed changes in behavioral skills for HIV prevention. Participants were asked how hard or easy (from 1 = “Very hard” to 5 = “Very easy”) it was for them to implement a variety of skills, including discussing sex and condom use with sexual partners, and acquiring and using condoms. Items were summed with higher scores indicating greater efficacy in behavioral skills. (2) Condom self-efficacy (CSE) was assessed using the 5-item self-efficacy for negotiating condom use assessment.47,48 The items were adapted to account for the different forms of condoms or other barriers TMSM use. Using a 5-point Likert scale from 1 = “Can’t do at all” to 5 = “Certain can do,” the assessment included items like, “I can ask a new partner to use condoms or other barriers” or “I can refuse sex when I don’t have a condom or other barrier available.” (3) HIV knowledge was assessed using a shortened version of the 18-item HIV knowledge questionnaire.49 Participants were asked to indicate true, false, or don’t know to 10 statements related to knowledge of sexual transmission such as, “A person can get HIV from oral sex.” A single summary score was created with higher scores indicating greater HIV-related knowledge. (4) Knowledge of pre-exposure prophylaxis (PrEP) was assessed by asking participants, “Have you heard of HIV negative people taking HIV medication (also known as PrEP) before sex because they thought it would lower their chances of getting HIV?” (yes/no).50
Primary Outcomes: Sexual Risk Behavior
The AIDS-Risk Behavior Assessment (ARBA),51 a computerized self-interview designed specifically for use with adolescents, was used to assess participants’ sexual behaviors. The interview was adapted to reflect the diversity of identity and experience that exists within the TMSM population.52 Using items from the ARBA, five indicators measured sexual risk: (1) number of sexual partners in past 4 months (continuous); (2) unprotected (condomless) anal and/or vaginal sex with a partner who was assigned a male sex at birth—past 4 months (yes/no); (3) unprotected (condomless) vaginal sex—past 4 months (yes/no); (4) unprotected (condomless) anal sex—past 4 months (yes/no); and (5) unprotected (condomless) anal and/or vaginal sex—past 4 months (yes/no).
Secondary Outcomes, HIV and STI Status
Participants were tested for HIV and C. trachomatis and N. gonorrhoeae urethral infections at pre- and post-intervention. HIV status was assessed using the OraQuick® ADVANCE™ rapid HIV test (finger-stick). C. trachomatis and N. gonorrhoeae urethral infections were tested using DNA amplification assays (BD Probetec ET SDA, BD Diagnostics, Sparks, MD) on participant urine specimens. Lifetime STI status was also assessed by asking participants if they have ever been told by a doctor or nurse that they had a sexually transmitted infection, other than HIV, such as Chlamydia, genital warts (HPV), trichomoniasis (trich), syphilis, gonorrhea (clap), genital herpes, or another STI (yes/no).
Data Analysis
Pre- and 4-month post-intervention data were analyzed descriptively (frequencies, means, standard deviations) in SAS v9.3. Paired t tests were used to compare within-person change on scale scores pre- and 4 months post-intervention. For nominal variables, Fisher’s exact tests were used to evaluate proportional differences due to small cell sizes. Given the small size of this open-phase pilot intervention, emphasis is placed on the direction of anticipated behavior change and trends in statistical significance, rather than on achieving statistical significance at the alpha 0.05-level per se. Qualitative data were both merged and connected with quantitative data to contextualize findings. Immediately following each qualitative focus group event and individual qualitative exit interview, study staff took field notes in the form of brief rapid thematic summaries. Transcripts from focus groups and exit interviews were then transcribed verbatim. Themes from staff field notes were used to compile an initial code set, which was then refined by the study team to integrate additional coding content and re-review to ensure codes were as representative as possible.
Results
Feasibility
Of the 18 participants who enrolled at baseline, 22.2 % completed two sessions, 11.1 % three sessions, and 66.7 % all four sessions. Retention was 94.4 % (17/18) across the 4-month follow-up. One participant was lost to follow-up due to physical health issues, which made him unable to complete his in-person 4-month follow-up visit. Thus, baseline and follow-up data are presented from the 17 participant completers (mean age = 24.3; 23.5 % POC).
Table 2 presents demographic and other related characteristics. Participants had a mean age of 24.3 (SD = 2.8). The majority (75.5 %) were White (non-Hispanic). Although the majority of the sample had a college degree or higher (58.8 %), nearly one fifth (17.7 %) were unemployed. Transgender men/FTM was the gender identity endorsed by the majority of participants (70.1 %), followed by man (17.7 %). The most commonly endorsed sexual identities were bisexual and pansexual (both 35.3 %), followed by queer (33.3 %).
Table 3 shows pre- and 4-month post-intervention data on psychosocial and sexual risk indicators. Changes in psychosocial and sexual risk outcomes trended in the hypothesized direction for all psychosocial and sexual health indicators. A significant increase was observed in the mean TG-AIM score post-baseline (p = 0.02), suggesting greater integration into the transgender community and improved gender identity adjustment among TMSM post-intervention. A marginally significant increase in condom self-efficacy scores were also observed post-intervention (p = 0.05). A modest decrease in perceived cisgender male stigma, a subscale of the transphobia measure, was observed post intervention, as was a modest increase in the public collective self-esteem subscale, although neither changes reached statistical significance (p = 0.10).
The baseline and follow-up prevalence of HIV was 0.0 % and the urethral GC/CT was 0.0 %; however, 29.4 % (n = 5) of participants reported a lifetime STI history (chlamydia, HPV, and genital herpes), and 17.6 % had engaged in recent sex work in the last 4 months.
Acceptability
Satisfaction with the intervention was high: 64.7 % reported being “very satisfied” and 29.4 % “satisfied,” 5.9 % said “neutral.” When asked about the overall quality of the intervention, 64.7 % rated it “excellent,” 29.4 % “good,” and 5.9 % as “neutral.” Of open-phase pilot completers, 94.1 % said they would recommend the intervention to a friend. Several participants (n = 6; 33.3 %) reported wanting the program to be longer with more sessions but shorter duration of each session (i.e., eight weekly sessions for 1 h each; 2 months and 8 h of content).
In brief qualitative exit interviews at 4-month follow-up, participants overwhelmingly described their experiences with LS4M as “positive” and “fun.” For example, one young TMSM said: “I liked it. It was fun. I was able to make connections between behaviors and how I felt about myself, which was helpful. I liked the activities - particularly the scenarios and discussing how we felt.” (age 28, gender transgender man/FTM/trans man, sexuality queer). Participants described LS4M as a much needed sexual health resource to meet their sexual health needs: “There is nothing else out there for TMSM” (age 28, gender transgender man/FTM/trans man, sexuality queer). Having a sexual health resource specifically for young TMSM was affirming for many participants: “Very positive experience - I had no problem with it. Liked the new things I learned; I really do need to take sexual health seriously. Like that it was happening here [at the intervention site]. It was empowering to know that space and money were put aside for TMSM. LS4M fills an important gap in existing services and programs for us” (age 25, gender transgender man/FTM/trans man, sexuality pansexual).
Participants often highlighted the small group format as an essential component of LS4M, connecting their individual experience of “safety” with being in a young TMSM group space: “It was good. Really informative (which was unexpected). It made me feel better about myself. It felt very safe” (age 21, gender genderqueer/Gender non-conforming/non-binary, sexuality asexual). Others liked the way the intervention integrated group and personal experiences: “A lot of good information. Activities were open enough to allow the group members to get what they needed. Good balance between facts and personal experience” (age 24, gender transgender man/FTM/trans man, sexuality pansexual).
Discussion
Overall, attendance and participation rates demonstrate the LS4M intervention, developed “by” and “for” young TMSM, is highly acceptable to, and feasible to carry out with, young TMSM. Trends in outcome measures suggest that participation in the intervention may improve mental health and reduce internalized stigma; whether the intervention reduces HIV- and STI-related risks warrants future research and evaluation.
The process of adapting and evaluating LS4M offers several “lessons learned” to guide future HIV and STI research, intervention, and practice with young TMSM (Table 4). First, it is imperative to engage TMSM during initial study development and ensure meaningful ongoing participation of local communities throughout the project. This includes engaging one or more TMSM community members to collaborate closely with the study team (there should already be one or more TMSM on the study team) preferably people with experience facilitating local community programs with the target population. It is also critical that TMSM are compensated for their time, even a modest stipend communicates to community members that their time and energy is as valuable as that of any other individual.
Second, recognize that diverse heterogeneity of gender identities and expressions exist among TMSM. This can be difficult for interventions insofar as it is challenging to meet all the needs of the diverse community, especially when doing small-group-based intervention work. However, the diversity can be, and was in LS4M, used as a platform to build community by acknowledging differences/similarities. The diversity was a core component to be celebrated by the community themselves to ensure individual participants are “seen” and affirmed in their uniqueness.
Third, ensure sexual risk behavior assessments are gender affirmative and accurately assess sexual risks. Sexual risk assessments need to ask about specific sexual risk behaviors (bioanatomically) using gender-affirmative language with diverse sexual partner genders (e.g., male, female, and transgender sexual partners) and types (e.g., poly, kink). Assessments are most acceptable to TMSM if they ask about all sexual practices in order to validate and affirm young TMSM sexuality, regardless of whether or not sexual practices confer high risk for HIV or STIs.
This exploratory study should be interpreted in light of several limitations. First, the adaptation and initial pilot testing of LS4M was conducted in Boston, Massachusetts; thus, differences in young TMSM communities and terminology by geographic region may necessitate consideration in future research. Second, given that the pilot of LS4M did not include recent sexual risk behavior as an inclusion criterion for eligibility, further testing of the intervention with sexual risk inclusion criteria and with a control group is needed.
The goal of this study was to adapt LifeSkills, a behavioral HIV/STI prevention intervention originally designed for young transgender women,25 to address the sexual health needs of young TMSM. Our work with young TMSM and staged approach to intervention adaptation found that young TMSM have many different factors and life experiences fueling HIV and STI risk than those of young transgender women; however, our experience shows some shared core intervention aspects for young TMSM as for transgender women: (1) work “with” not “on” youth transgender communities to empower themselves; (2) address sexual risk in context—explicitly recognize that sexual health is not the number one life priority for young transgender people and that “lives in context” can and should guide intervention efforts; and (3) honor that gender affirmation is a key aspect of life for young transgender people and work with them to understand the specific ways that gender affirmation—social, medical, legal, and psychological—plays out in all contexts and areas of functioning, including sexual health.
References
CDC. HIV among youth. June 30, 2015. Available at: http://www.cdc.gov/hiv/group/age/youth/index.html. Accessed Aug 1, 2015.
Kann L, Kinchen S, Shanklin SL, et al. Youth risk behavior surveillance—United States, 2013. MMWR Surveill Summ. 2014; 63(Suppl 4): 1–168.
CDC. 2013 Sexually transmitted diseases surveillance. Available at: http://www.cdc.gov/std/stats13/toc.htm. Accessed March 12, 2015
Reisner SL, Vetters R, White JM, et al. Laboratory-confirmed HIV and sexually transmitted infection seropositivity and risk behavior among sexually active transgender patients at an adolescent and young adult urban community health center. AIDS Care. 2015; 27(8): 1031–1036.
Wilson EC, Chen YH, Arayasirikul S, et al. Differential HIV risk for racial/ethnic minority trans*female youths and socioeconomic disparities in housing, residential stability, and education. Am J Public Health. 2015; 105(Suppl 3): e41–e47.
Brennan J, Kuhns LM, Johnson AK, et al. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012; 102(9): 1751–1757.
Hotton AL, Garofalo R, Kuhns LM, Johnson AK. Substance use as a mediator of the relationship between life stress and sexual risk among young transgender women. AIDS Educ Prev. 2013; 25(1): 62–71.
Kenagy GP, Hsieh CM. The risk less known: female-to-male transgender persons' vulnerability to HIV infection. AIDS Care. 2005; 17(2): 195–207.
Sevelius J. "There's no pamphlet for the kind of sex I have": HIV-related risk factors and protective behaviors among transgender men who have sex with nontransgender men. Am Psychiatr Nurses Assoc. 2009; 20(5): 398–410.
Reisner SL, Perkovich B, Mimiaga MJ. A mixed methods study of the sexual health needs of New England transmen who have sex with nontransgender men. AIDS Patient Care STDs. 2010; 24(8): 501–513.
Adams A, Lundie M, Marshall Z, et al. Getting primed: informing HIV prevention with gay/bi/queer trans men in Ontario. Ontario, Canada: Ontario Ministry of Health and Long-Term Care; 2008.
Bauer GR, Redman N, Bradley K, Scheim AI. Sexual health of trans men who are gay, bisexual, or who have sex with men: results from Ontario, Canada. Int J Transgend. 2013; 14(2): 66–74.
Reisner SL, Pardo ST, Garamel KE, White JM, Pardee DJ, Meier SC. Trans masculine experiences of stigma in U.S. healthcare: a gender minority stress model of substance use to cope with mistreatment. LGBT Health. In Press.
Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001; 91(6): 915.
Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav. 1995; 36(1): 38–56.
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003; 129(5): 674–697.
Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the minority stress model. Prof Psychol Res Pract. 2012; 43(5): 460.
Hamilton CJ, Mahalik JR. Minority stress, masculinity, and social norms predicting gay men's health risk behaviors. J Couns Psychol. 2009; 56(1): 132.
Fields EL, Bogart LM, Smith KC, Malebranche DJ, Ellen J, Schuster MA. "I always felt I had to prove my manhood": homosexuality, masculinity, gender role strain, and HIV risk among young black men who have sex with men. Am J Public Health. 2015; 105(1): 122–131.
Stieglitz KA. Development, risk, and resilience of transgender youth. J Assoc Nurses AIDS Care. 2010; 21(3): 192–206.
Scheim AI, Bauer GR. Sex and gender diversity among transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. J Sex Res. 2015; 52(1): 1–14.
Reisner SL, White Hughto JM, Pardee D, Sevelius JM. Syndemics and gender affirmation: HIV sexual risk in female-to-male trans masculine adults reporting sexual contact with cisgender males. Int J STD & AIDS. in press.
Sevelius JM. Gender affirmation: a framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013; 68(11–12): 675–689.
Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000; 55(5): 469.
Garofalo R, Johnson AK, Kuhns LM, Cotten C, Joseph H, Margolis A. Life skills: evaluation of a theory-driven behavioral HIV prevention intervention for young transgender women. J Urban Health. 2012; 89(3): 419–431.
Bronfenbrenner U. The ecology of human development: experiments by design and nature. Cambridge, MA: Harvard University Press; 1979.
Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013; 13: 482.
Lemieux AF, Fisher JD, Pratto F. A music-based HIV prevention intervention for urban adolescents. Health Psychol. 2008; 27(3): 349–357.
Robertson AA, Stein JA, Baird-Thomas C. Gender differences in the prediction of condom use among incarcerated juvenile offenders: testing the information-motivation-behavior skills (IMB) model. J Adolesc Health. 2006; 38(1): 18–25.
Malow RM, Stein JA, McMahon RC, Devieux JG, Rosenberg R, Jean-Gilles M. Effects of a culturally adapted HIV prevention intervention in Haitian youth. J Assoc Nurses AIDS Care. 2009; 20(2): 110–121.
Singh S. Study of the effect of information, motivation and behavioural skills (IMB) intervention in changing AIDS risk behaviour in female university students. AIDS Care. 2003; 15(1): 71–76.
Fisher JD, Fisher WA, Misovich SJ, Kimble DL, Malloy TE. Changing AIDS risk behavior: effects of an intervention emphasizing AIDS risk reduction information, motivation, and behavioral skills in a college student population. Health Psychol. 1996; 15(2): 114–123.
Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: getting started and moving on from stage I. Clin Psychol Sci Pract. 2001; 8(2): 133–142.
Leung MW, Yen IH, Minkler M. Community based participatory research: a promising approach for increasing epidemiology's relevance in the 21st century. Int J Epidemiol. 2004; 33(3): 499–506.
Reisner S, Pardee D. Access to care barriers among transgender people in the US: findings from the U.S. National Transgender Discrimination Survey. The 2015 National Transgender Health Summit. Oakland, CA; 2015, April.
Zhang Y, Wildemuth BM. Qualitative analysis of content. In: Wildemuth B, ed. Applications of social research methods to questions in information and library science. Santa Barbara, CA: Greenwood Press; 2009: 308–319.
Nelson IA. From quantitative to qualitative: adapting the life history calendar method. Field Methods. 2010; 22(4): 413–428.
Yoshihama M, Gillespie B, Hammock AC, Belli RF, Tolman RM. Does the life history calendar method facilitate the recall of intimate partner violence? Comparison of two methods of data collection. Soc Work Res. 2005; 29(3): 151–163.
Pearce L, Ghimire D. Innovations in life history calendar applications. Soc Sci Res. 1999; 28: 243–264.
Freedman D, Thornton A, Camburn D, Alwin D, Young-demarco L. The life history calendar: a technique for collecting retrospective data. Sociol Methodol. 1988; 18: 37–68.
Fisher CM. Assessing developmental trajectories of sexual minority youth: discrepant findings from a life history calendar and a self-administered survey. J LGBT Youth. 2012; 9(2): 114–135.
Sjoberg MD, Walch SE, Stanny CJ. Development and initial psychometric evaluation of the transgender adaptation and integration measure (TG AIM). Int J Transgenderism. 2006; 9(2): 35–45.
Derogatis LR. Brief symptom inventory 18. Minneapolis, MN: NCS Pearson; 2000.
Crocker J, Luhtanen R. Collective self-esteem and ingroup bias. J Pers Soc Psychol. 1990; 58: 60–67.
Starace F, Massa A, Amico KR, Fisher JD. Adherence to antiretroviral therapy: an empirical test of the information-motivation-behavioral skills model. Health Psychol. 2006; 25(2): 153.
Amico K, Toro-Alfonso J, Fisher JD. An empirical test of the information, motivation and behavioral skills model of antiretroviral therapy adherence. AIDS Care. 2005; 17(6): 661–673.
Forsyth AD, Carey MP, Fuqua RW. Evaluation of the validity of the condom use self-efficacy scale (CUSES) in young men using two behavioral simulations. Health Psychol. 1997; 16(2): 175–178.
Brafford LJ, Beck KH. Development and validation of a condom self-efficacy scale for college students. J Am Coll Heal. 1991; 39(5): 219–225.
Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev: Off Publ Int Soc AIDS Educ. 2002; 14(2): 172.
Kuhns LM, Reisner SL, Mimiaga MJ, Gayles T, Shelendich M, Garofalo R. Correlates of PrEP Indication in a Multi-Site Cohort of Young HIV-Uninfected Transgender Women. AIDS Behav. Sep 3 2015.
Donenberg GR, Emerson E, Bryant FB, Wilson H, Weber-Shifrin E. Understanding AIDS-risk behavior among adolescents in psychiatric care: links to psychopathology and peer relationships. J Am Acad Child Adolesc Psychiatry. 2001; 40(6): 642–653.
Reisner SL, Pardee D. gender affirmative assessment of HIV risk behaviors in female-to-male trans masculine youth who have sex with cisgender males (TMSM). Paper presented at: 2015 National Transgender Health Summit, 2015; Oakland, CA.
Acknowledgments
For their invaluable collaboration and input to ensure transgender community engagement in this research project: Tre’Andre Valentine, Thomas Lewis, Mick Rehrig, Mackenzie Pawliger, Justice Williams, Jesse Pack. For their assistance with qualitative focus group data coding and thematic analysis: Gabriel Murchison, Elijah Cohen, Renee Randazzo. For sharing their voices and lived experiences: Our participants.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding Source
Research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under Award Number R01MH094323 (MPIs: Garofalo and Mimiaga). The present ancillary study was funded under an administrative supplement to the parent R01 grant (PI: Reisner). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Rights and permissions
About this article
Cite this article
Reisner, S.L., Hughto, J.M.W., Pardee, D.J. et al. LifeSkills for Men (LS4M): Pilot Evaluation of a Gender-Affirmative HIV and STI Prevention Intervention for Young Adult Transgender Men Who Have Sex with Men. J Urban Health 93, 189–205 (2016). https://doi.org/10.1007/s11524-015-0011-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-015-0011-z