Abstract
Most research concerning clients of commercial sex workers (CSWs) relies upon CSW reports of client characteristics and behavior. We describe correlates of ever purchasing sex among 3,829 men from three cities: São Paulo, Brazil; Cuernavaca, Mexico; and Tampa, USA. A computer-assisted self-interview collected data on demographics and sexual behavior. There were significant site differences—26.5 % paid for sex in São Paulo, 10.4 % in Cuernavaca, and 4.9 % in Tampa. In all cities, men who had sex with men and women (versus sex with women only) were more likely to have ever paid for sex. In São Paulo and Cuernavaca, CSW clients were older, had higher educational attainment, and were less likely to be married. In Tampa, older age was associated with being a CSW client but not education and marital status. In São Paulo and Cuernavaca, CSW clients had more partners than men who had never paid for sex. In São Paulo, CSW clients initiated vaginal sex at an earlier age, while in Cuernavaca they were more likely to self-report a sexually transmitted infection. CSW clients varied with respect to demographics across the three cities while the association between paying for sex and risky sexual behavior seems to be somewhat conserved. These findings suggest that interventions among CSW clients should focus on condom use with commercial and non-commercial partners as these men may be at increased risk for transmitting and acquiring sexually transmitted infections to and from their sex partners. Better understanding of client characteristics is needed for targeting interventions and creating culturally appropriate content.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most research concerned with the public health impact of commercial sex work has been conducted among female commercial sex workers (CSWs).1 This research has documented considerable morbidity and mortality among female CSWs related to their occupation. Much less is known about the clients of CSWs.2
The proportion of men who pay for sex varies within and between countries. Lifetime prevalence among European men varies by country—8.8 % in Britain,3 12.9 % in Norway,4 13.1 % in Denmark,5 and 25.4 % in Spain.6 Past year prevalence was 1.3 % in Britain,3 1.7 % in Denmark,5 and 5.3 % n Spain.6 In China, 8.1 % of men7 reported paying for sex in their lifetime, and approximately 6.3 % reported paying for sex in the past year.8 A recent analysis from the third wave of the US National Longitudinal Study of Adolescent Health (Add Health) reported that 5.1 % of males reported paying for sex.9 Past year prevalence was estimated to be 1.3 % in the General Social Survey conducted in Colorado Springs, Colorado.10 With the exception of China and the US, some form of sex work was legal in these countries.11
Very little research has focused on male clients of CSWs, and what little there is often relies on CSWs’ reports of client characteristics and behavior.1,12 With few exceptions, much of the published research can be found in the criminology literature and, as a result, does not tend to focus on the sexual risk behaviors of CSW clients. The health outcomes of CSWs and their male clients are influenced by the sexual behavior that occurs during commercial and non-commercial sex encounters among both partners, yet research—and interventions—are focused predominantly among CSWs. Here, we explore the prevalence and correlates of paying for sex among men in three cities: São Paulo (Brazil), Cuernavaca (Mexico), and Tampa (USA). Commercial sex work (i.e., prostitution) is illegal in Florida while in Brazil and Mexico it is legal under certain conditions.11
Methods
Study Population
We conducted a post hoc analysis of the baseline visit of the HPV in Men (HIM) Study. The HIM Study is a prospective cohort study of the natural history of human papillomavirus (HPV) infection among men.13,14 Between 2005 and 2009, men were recruited from São Paulo, Cuernavaca, and Tampa. Eligibility criteria included being aged 18–70 years old; a resident of one of the three cities; no prior diagnosis of penile cancer, anal cancer, genital warts, HIV, or AIDS; no sexually transmitted infection (STI) symptoms or treatment for an STI; no participation in an HPV vaccine study; no history of imprisonment, homelessness, or drug treatment during the past 6 months; and a willingness to complete follow-up visits every 6 months for 4 years with no plans to relocate in 4 years.
Men were recruited from different population sources to increase variability with respect to age, sexual behaviors, and HPV risk. In São Paulo, men were recruited from a facility for urogenital care, through general media advertising, and from among the spouses and partners of women participating in a large cohort study HPV infection and cervical neoplasia. In Cuernavaca, the underlying population was that of employees and beneficiaries of the Instituto Mexicano de Seguro Social, factory workers, and men in the Mexican army who were permanently assigned to this geographic area. In Tampa, the underlying population from the University of South Florida and the greater Tampa metropolitan area was recruited through mail and media using brochures, flyers, and posters as well as advertisements in local and university papers. All men at each study site reported being disease-free at the time of enrollment. The study was reviewed and approved by the institutional review boards at each institution.
The baseline sample included 4,074 men. Ten men were excluded because they were missing paying for sex data, and 235 men were excluded because they had never had sex. The final sample size for this analysis was 3,829.
Data Collection
Data were collected on sociodemographics and sexual history using Computer-Assisted Self-Interviewing (CASI). With respect to sociodemographics, men were asked about their age, race (i.e., white, black, or African American, Asian, American Indian (Tampa only), Indio Americano (Cuernavaca only) or Índio (São Paulo only)) and ethnicity (i.e., Hispanic or non-Hispanic), marital status (i.e., single/divorced/widowed, or married/cohabiting), educational attainment (i.e., less than 12, 12, 13–15, 16, or 17 or more years completed), and same-sex sexual behavior (i.e., men who have sex with women (MSW), men who have sex with men (MSM), and men who have sex with men and women (MSMW) based on sexual partners in the last 6 months). Men were asked about the age of vaginal sex initiation, lifetime number of sex partners, and lifetime history of STIs.
For lifetime history of purchasing sex, men were asked if they had ever: (1) exchanged sex for money or drugs and (2) paid a man or (3) paid a woman to have vaginal, anal, or oral sex. For recent (past 3 months) history of purchasing sex, men were asked if they paid a man or a woman to have sex, how many times they paid, the type of sex paid for (i.e., vaginal , anal, oral, or other sex), and condom use frequency with the paid partner.
Analysis
We first describe sociodemographic and behavioral correlates of a lifetime history of purchasing sex (never versus ever—referred to as CSW clients). Age was categorized into quartiles (i.e., 18–23, 24–31, 32–40, and 41–70 years). Age of vaginal sex initiation was categorized as ≤14, 15–16, 17–18, and ≥19 years. Lifetime number of vaginal sex partners was categorized as 0–2, 3–7, 8–19, and 20 or more partners. Because of significant differences with respect to sociodemographics and sex work policies across cities, we stratified analyses by site. Differences between CSW clients and those who never paid for sex were compared using χ 2 statistics or Fisher’s exact test when a cell had less than six respondents.
Multivariable logistic models for sociodemographic correlates of lifetime sex purchasing were constructed for each city, controlling for each variable in the model. Multivariable logistic models for sexual behavior correlates of lifetime sex purchasing were also constructed for each city. Because the sexual behavior variables were all associated with each other (i.e., number of partners was associated with both age of vaginal sex initiation and lifetime STI diagnosis in all three cities and age of vaginal sex initiation was associated with lifetime STI diagnosis in Tampa), we examined the relationship between paying for sex and each sexual behavior separately in models that adjusted for significant sociodemographic variables only (and not other sexual behavior variables). As a result, we could determine the relationship between each sexual behavior with paying for sex.
Finally, we report recent sexual behaviors among men who had recently paid for sex. We did not make comparisons between men who had not recently paid for sex because prevalence was very low. These data are meant to be descriptive only.
Results
São Paulo had the highest proportion of men who had ever been CSW clients (26.5 %), followed by Cuernavaca (10.4 %) and Tampa (4.9 %, p < 0.001). In São Paulo 23.0 % had ever paid women for sex as compared to 10.1 % in Cuernavaca and 4.6 % in Tampa (p < 0.001).
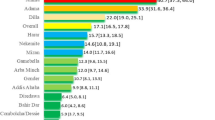
Table 1 presents sociodemographic and sexual correlates of paying for sex, stratified by study site. In São Paulo, a higher proportion of CSW clients were aged 24–40 years; single, divorced, or widowed; had higher educational attainment; and were MSMW. In terms of sexual behaviors, there were no significant differences with respect to age of vaginal sex initiation and lifetime history of STIs. São Paulo CSW clients had more vaginal sex partners than men who had never paid for sex.
Educational attainment and same-sex sexual behavior were associated with paying for sex among men in Cuernavaca in bivariable analyses. In terms of sexual behaviors, there were no significant differences with respect to age of vaginal sex initiation. In contrast to São Paulo CSW clients, CSW clients in Cuernavaca were more likely to report a lifetime history of STIs and not knowing if they had ever had an STI as compared with men who had never paid for sex. As in São Paulo, CSW clients in Cuernavaca had more vaginal sex partners than men who had never paid for sex.
In Tampa, paying for sex was associated with age, marital status, education, and same-sex sexual behavior in bivariable analyses. Unlike the São Paulo and Cuernavaca samples, CSW clients were more likely to initiate sex at earlier (i.e., before age 14 years) and later (i.e., after age 18 years) ages as compared with those who had never paid for sex. Similar to CSW clients in the other cities, CSW clients in Tampa had more vaginal sex partners as compared with those who had never paid for sex. Finally, CSW clients in Tampa were more likely to report having a history of STIs than those who had never paid for sex.
Multivariable Models for Correlates of Ever Paying for Sex
We constructed multivariable logistic regression models for the associations between lifetime history of paying for sex and sociodemographic variables (Table 2). Older age was a significant correlate of paying for sex, although the associations were different across cities. In São Paulo, CSW clients were more likely to be aged 24–31 and 32–40 as compared with 18–23 years. In Cuernavaca, CSW clients were more likely to be aged 41–71 as compared with 18–23 years. In Tampa, CSW clients were more likely to be aged 24–31, 32–40, and 41–70 as compared with age 18–23 years.
In São Paulo and Cuernavaca, male sex clients were less likely to be married or cohabitating as compared with being single; marital status was not associated with paying for sex in Tampa. Higher educational attainment was associated with being a CSW client only in the São Paulo and Cuernavaca samples. Across all three sites, MSMW had a 72–162 % increased odds of being CSW clients as compared with MSW.
We next constructed multivariable logistic regression models for the associations between lifetime history of paying for sex and sexual behaviors (Table 3). In the São Paulo, men who initiated vaginal sex at age 19 years or older were significant less likely to have been a CSW client as compared with those who initiated at age 14 years or younger after adjusting for age, marital status, education, and same-sex sexual behavior. Although in bivariable analyses paying for sex was associated with age of vaginal initiation in the Tampa sample, this association disappeared once we controlled sociodemographic variables.
Paying for sex was associated with having more lifetime vaginal sex partners even after controlling for the demographic variables in the São Paulo and Cuernavaca samples. This appears to be a dose–response relationship, such that the odds of being a CSW client increase as the number of partners increase. Although we observed a significant relationship in the bivariable analysis between lifetime STIs and being a CSW client in both Cuernavaca and Tampa, once we controlled for demographic variables, the association was only significant for Cuernavaca.
Recent Paying for Sex
Finally, we report sexual behaviors among the 130 men who had been CSW clients in the last 3 months. In São Paulo, 94 (26.6 %) of those with a lifetime history of paying for sex had been CSW clients in the past 3 months; 84.0 % paid a woman; and 18.1 % paid a man (Table 4). The mean number of paid sexual episodes was 2.5 (SD = 3.7) with a range of 1 to 30. Among those who paid women for sex, 93.7 % paid for vaginal sex, 72.2 % paid for oral, and 25.3 % paid for anal. Most (93.7 %) always used a condom when they paid a woman for sex.
Among men in Cuernavaca with a lifetime history of paying for sex, 23 (17.8 %) had been CSW clients in the past 3 months of whom 87.0 % paid a woman and one paid a man (Table 4). The mean number of paid sexual episodes was 1.8 (SD = 2.0) with a range of one to ten. Among those who paid women for sex, 80.0 % paid for vaginal sex and 35.0 % paid for oral sex; no one paid for anal sex. Sixty percent always used a condom when they paid a woman for sex
In Tampa, 13 (21.3 %) of those with a lifetime history of paying for sex had been CSW clients in the past 3 months; 92.3 % had paid a woman; and 15.4 % had paid a man (Table 4). The mean number of paid sexual episodes was 2.2 (SD = 1.7) with a range of one to six. Among those who paid women for sex, 91.7 % paid for vaginal sex and seven 58.3 % paid for oral sex; no one paid for anal sex. Ten (83.3 %) always used a condom when they paid a woman for sex.
Discussion
We observed significant differences between cities in the proportion of men that reported paying for sex in this interurban study. Overall, 14.2 % of men in the HIM study reported paying a man or a woman for sex in their lifetime. The lifetime prevalence of paying for sex was highest in São Paulo (26.5 %), followed by Cuernavaca (10.4 %) and Tampa (4.9 %). Site differences are likely related to, at least in part, differences in sex work policies and recruitment approaches in each city. Across all three cities, pimping (i.e., procuring customers for a CSW) and brothels (i.e., houses of prostitution) were illegal,11,15 but prostitution and solicitation were illegal in Florida15 and legal in Brazil and Mexico.11
Current published estimates of the prevalence of paying for sex among men in Mexico and Brazil were not available for comparison. The 1996 Brazil Demographic and Health Survey reported that 2.7 % of men had commercial sex in the past year.16 The estimate from Tampa was similar to estimates from the Add Health Study9 but higher than estimates based on arrest data, which are likely underestimate prevalence because not all male sex clients are arrested.10
Age was significantly associated with paying for sex in all three cities, although the relationships were different within sites. Generally, men aged 18–23 years were the least likely to pay for sex. In Cuernavaca, men aged 41–70 years were most likely to pay for sex, while in São Paulo and Tampa, 24–31- and 32–40-year-olds were more likely to have been CSW clients as compared with 18–23-year-olds, respectively. It is unclear why there is an association between paying for sex and age. One explanation may be that older age is associated with changes in marital status related to separation, divorce, or death of a spouse that limits access to a sex partner. While we had data on current marital status, we did not have data on the recency of that status or whether an individual had remarried. Older age could also be associated with increased disposable income, which could provide more resources for paying for sex. Unfortunately, income was only available for the São Paulo sample so we were not able to explore this further. It is also possible that the relationship between age and paying for sex are actually cohort or period effects rather than age effects. We cannot disentangle age and cohort effects in this cross-sectional data set. With respect to possible period effects, federal sex work laws and regulations appear to have been relatively stable across the participants’ adolescence and adulthood in all three cities, where the earliest birth year was 1936. Prostitution has not been criminalized in Brazil since at least 194017 and was a regulated trade in Mexico going back to the late nineteenth century.18–20 In Florida, prostitution was illegal at least as early as 1943.21,22
Married and cohabitating men in São Paulo and Cuernavaca were significantly less likely to have a lifetime history of paying for sex in multivariable analyses. However, marital status was not related to paying for sex in Tampa. Previous studies in Britain3 and the USA12,23–25 have shown that married men are less likely to pay for sex, while studies in Australia,26,27 China,8 Norway,4 and Spain6 have reported no significant associations between marital status and paying for sex. Some have suggested that imbalanced sex ratios in a community are associated with higher likelihood of paying for sex.7,25
In São Paulo and Cuernavaca, higher levels of education were generally associated with increased odds of paying for sex. Previous studies have shown no association between education and paying for sex,7 while others have shown an inverse relationship.26 This could be due to differences in the measurement and analysis of education. South and Trent7 analyzed an ordinal education variable (i.e., never attended school, elementary school, junior high school, senior high school, junior college, and university/graduate school) as a continuous variable, thereby assuming a linear relationship. Pitts et al.26 used a dichotomous variable (i.e., high school certificate versus none). Because we needed to make comparisons across three cities with different education systems, we used years of education attained rather than specific benchmarks. We also did not assume that there was a linear association between levels of education and paying for sex. One explanation for the relationship between education and paying for sex is that more education is associated with higher income (and therefore more available resources) and/or more liberal attitudes toward sex.28
In all three cities, men who purchased sex were more likely to be MSMW and less likely to be MSM compared with MSW. Overall, 0.2 % of MSW paid men for sex, 12.2 % paid women, and 0.4 % paid both men and women (data not shown). Among MSM, 14.0 % paid men for sex, and 0.6 % paid both men and women; none paid women only. Among MSMW, 8.6 % paid men for sex, 15.4 % paid women, and 7.1 % paid both men and women. The literature is mixed with respect to the relationship between same-sex sexual behavior and purchasing sex, and comparisons across studies are difficult to make due to differences in sex worker policies, setting, time, and study design. Monto and McRee24 found that men who paid for sex were less likely to identify as a homosexual in a study of American men. Among men in Britain’s 1990 National Survey of Sexual Attitudes and Lifestyles (Natsal),29 a lifetime history of a having a male partner was associated with significantly increased odds of paying for sex. There was no association between having a male partner and paying for heterosexual sex in Natsal 2000,3 an Australian study conducted at a commercial sex exhibition in 2001, and the Add Health Study.9 However, in the Natsal 1990 and 2000 as well as US Add Health analyses, researchers did not distinguish between MSM and MSMW.
The reason that MSMW have higher odds of lifetime history of paying for sex is unclear. Some have suggested that internalized homophobia may be associated with high-risk sexual behavior,30,31 but a meta-analysis suggests that the effect size is small.32 Smolenski and colleagues33 have suggested that the relations between internalized homophobia and sexual risk are not direct but are indirect through compulsive sexual behavior and sexual partnering frequency. These studies have not specifically examined the relationships between internalized homophobia and paying for sex but rather specific sexual activities such as unprotected oral or anal intercourse. The use of a behaviorally defined measure of same-sex sexual behavior rather than self-described sexual identity is a limitation of this study,34 as it may obscure important nuances in the relation between identity and behavior. On the other hand, creating a valid and culturally relevant sexual identity variable for each of these cities that is consistent and cross-nationally comparable may be difficult. In addition, neither internalized homophobia nor sexual compulsivity was measured. The relation between same-sex sexual behavior, sexual identity, internalized homophobia, and paying for sex needs to be further explored.
Several sexual behaviors were associated with paying for sex. Older age of vaginal sex initiation was associated with decreased odds of paying for sex in São Paulo. Few have looked at the relation between sexual debut and paying for sex. In population-based studies in Norway4 and Spain,6 similar associations were observed while an Australian study of people attending a sexual exhibition did not find an association.26
In all three cities, CSW clients had more lifetime vaginal sex partners in bivariable analyses, and the associations remained significant in multivariable models for São Paulo and Cuernavaca. This association has been shown in other settings.4,24,26 The association here appears to be a dose–response relationship, such that the odds of paying for sex increase as the number of lifetime vaginal sex partners increases. One explanation may be that men who pay for sex are more likely to be sexually compulsive. One study among CSW clients in Mexico35 found that sexual compulsion was associated with more frequent unprotected vaginal sex with female CSWs. In another study of STI clinic attendees, sexual compulsivity was associated with a higher number of sexual partners.36 Others have suggested that high-risk sexual behavior37 and number of sexual partners are related to sociosexuality.38 Sociosexuality, first described by Kinsey and colleagues,39,40 includes variables such as “…the preferred and actual frequency of sexual intercourse, number of sexual partners, frequency of extradyadic sex, and frequency of uncommitted sex”.38 Individuals can have liberal or conservative sociosexuality, thus one might postulate that number of sex partners and paying for sex would be associated with a more liberal sociosexual orientation. The underlying reasons for these associations that are conserved across cultures needs further exploration.
In Cuernavaca, paying for sex was associated with a self-reported lifetime history of STIs. This is consistent with findings from Chinese and British studies, which found that CSW clients had increased odds for having an STI diagnosis.3,7,8 This is congruent with the self-reported inconsistent condom use among recent CSW clients in our samples.
As with any study, the results should be considered with the limitations in mind. The HIM Study was not designed to explore commercial sex patronage as a primary outcome. As such, we have a limited number of variables that describe paid sexual encounters. On the other hand, public health research is scant with respect to commercial sex patronage in general and in these three countries in particular. Data are self-reported, but previous research suggests CASI is associated with more reports of sexual risk behavior in general41,42 and purchasing sex in particular43,44 as compared with face-to-face interviews, but we cannot rule out under-reporting. Men were only asked if they had paid for oral, anal, and vaginal sex. Other sexual interactions such as masturbation, attending sex venues (e.g., strip clubs), and paying for lap dances were not included which limited our definition of commercial sex services. We do not know the characteristics of the CSWs with whom these men partnered. Thus, the extent to which the CSWs might pose a risk to their clients for HIV and other STIs is unknown, as is whether they were children or victims of sex trafficking. The crude and adjusted odds ratios for the relationship between paying for sex and age in the Tampa sample were large, and the confidence intervals were wide due to small cell sizes. Finally, the samples were not representative of the general male populations in the respective cities from which they were recruited. Caution should be taken in generalizing the results of this study to all men.
Despite the study limitations, we can conclude that men who had ever been clients of CSWs were more likely to have had STIs, sex with men and women, and a greater lifetime number of sex partners as compared with men who had never paid for sex. CSW clients varied with respect to demographics across the São Paulo, Cuernavaca, and Tampa samples while the association between paying for sex and risky sexual behavior seems to be somewhat conserved. These findings suggest that interventions among CSW clients should focus on condom use with commercial and non-commercial partners as these men may be at increased risk for transmitting and acquiring STIs, including HIV, to their sex partners. However, in order to effectively design interventions aimed at reducing harm to both CSWs and their clients, a better understanding of client characteristics is needed for targeting interventions and creating culturally appropriate content.
References
Sanders T. Paying for Pleasure: Men Who Buy Sex. Portland, OR: Willan; 2008.
Monto MA. Prostitutes' customers: motives and misconceptions. In: Weitzer R, ed. Sex for sale: prostitution, pornography, and the sex industry. 2nd ed. New York, NY: Routledge; 2010: 233–254.
Ward H, Mercer CH, Wellings K, et al. Who pays for sex? An analysis of the increasing prevalence of female commercial sex contacts among men in Britain. Sex Transm Infect. 2005; 81: 467–471.
Schei B, Stigum H. A study of men who pay for sex, based on the Norwegian national sex surveys. Scand J Public Health. 2010; 38: 135–140.
Melbye M, Biggar RJ. Interactions between persons at risk for AIDS and the general population in Denmark. Am J Epidemiol. 1992; 135: 593–602.
Belza MJ, de la Fuente L, Suarez M, et al. Men who pay for sex in Spain and condom use: prevalence and correlates in a representative sample of the general population. Sex Transm Infect. 2008; 84: 207–211.
South SJ, Trent K. Imbalanced sex ratios, men's sexual behavior, and risk of sexually transmitted infection in China. J Health Soc Behav. 2010; 51: 376–390.
Huang ZJ, Wang W, Martin MC, Nehl EJ, Smith BD, Wong FY. "Bridge population": sex workers or their clients?—STI prevalence and risk behaviors of clients of female sex workers in China. AIDS Care. 2011; 23(Suppl 1): 45–53.
Shutt JE, Barnes JC, Beaver KM, Higgins GE, Tewksbury R. Does biology underlie the oldest profession? Prostitution and sex disparities in john behavior. Biodemography Soc Biol. 2011; 57: 155–170.
Brewer DD, Roberts JM Jr, Muth SQ, Potterat JJ. Prevalence of male clients of street prostitute women in the United States. Hum Organ. 2008; 67: 346–356.
U.S.Department of State. 2008 Country reports on human rights practices. http://www.state.gov/g/drl/rls/hrrpt/2008/index.htm [serial online] 2009; Accessed April 22, 2011.
Della Giusta M, Di Tommaso ML, Shima I, Strom S. What money buys: clients of street sex workers in the US. Appl Econ. 2009; 41: 2261–2277.
Giuliano AR, Lee JH, Fulp W, et al. Incidence and clearance of genital human papillomavirus infection in men (HIM): a cohort study. Lancet. 2011; 377: 932–940.
Giuliano AR, Lazcano E, Villa LL, et al. Circumcision and sexual behavior: factors independently associated with human papillomavirus detection among men in the HIM study. Int J Cancer. 2009; 124: 1251–1257.
State of Florida. Prostitution. http://www.flsenate.gov/Laws/Statutes/2011/Chapter796 Title XLVI, Chapter 796. 2011. 9-28-2011.
MEASURE DHS. HIV/AIDS Survey indicators database. http://www.measuredhs.com/hivdata/ [serial online] 2011; Accessed October 19, 2011.
Rodrigues MT. O sistema de justiça criminal ea prostituição no Brasil contemporâneo: administração de conflictos, discriminação e exclusão. Soc estando. 2004; 19: 151–172.
Conde-Glez CJ, Calderón E, Juárez-Figueroa L, Hernández-Avila M. Historical account of venereal diseases in Mexico. Genitourin Med. 1993; 69: 462–466.
Bliss K. The science of redemption: syphilis, sexual promiscuity, and reformism in revolutionary Mexico City. Hisp Am Hist Rev. 1999; 79: 1–40.
Bliss KE. Compromised Positions: Prostitution, Public Health and Gender Politics in Revolutionary Mexico City. University Park, PA: Pennsylvania State University Press; 2001.
Statutory Revision Department. Florida statutes 1949. Tallahassee, Florida: State of Florida; 1949.
State of Florida. Prohibiting prostitution, etc.; evidence; penalties. §796.07. 1949.
Galvan FH, Ortiz DJ, Martinez V, Bing EG. The use of female commercial sex workers' services by Latino day laborers. Hisp J Behav Sci. 2009; 31: 553–575.
Monto MA, McRee JN. A comparison of the male customers of female street prostitutes with national samples of men. Int J Offender Ther. 2011; 49: 505–529.
Parrado EA, Flippen C. Community attachment, neighborhood context, and sex worker use among Hispanic migrants in Durham, North Carolina, USA. Soc Sci Med. 2010; 70: 1059–1069.
Pitts MK, Smith AM, Grierson J, O'Brien M, Misson S. Who pays for sex and why? An analysis of social and motivational factors associated with male clients of sex workers. Arch Sex Behav. 2004; 33: 353–358.
Xantidis L, McCabe MP. Personality characteristics of male clients of female commercial sex workers in Australia. Arch Sex Behav. 2000; 29: 165–176.
Treas J. How cohorts, education, and ideology shaped a new sexual revolution on American attitudes toward nonmarital sex, 1972–1998. Sociol Perspect. 2002; 45: 267–283.
Wellings K, Field J, Johnson AM, Wadsworth J. Sexual behaviour in Britain. London: Penguin; 1994.
Dew BJ, Chaney MP. The relationship among sexual compulsivity, internalized homophobia, and HIV at-risk sexual behavior in gay and bisexual male users of internet chat rooms. Sexual Addiction & Compulsivity. 2005; 12: 259–273.
Rosario M, Hunter J, Maguen S, Gwadz M, Smith R. The coming-out process and its adaptational and health-related associations among gay, lesbian, and bisexual youths: stipulation and exploration of a model. Am J Community Psychol. 2001; 29: 133–160.
Newcomb ME, Mustanski B. Moderators of the relationship between internalized homophobia and risky sexual behavior in men who have sex with men: a meta-analysis. Arch Sex Behav. 2011; 40: 189–199.
Smolenski DJ, Stigler MH, Ross MW, Rosser BR. Direct and indirect associations between internalized homonegativity and high-risk sex. Arch Sex Behav. 2011; 40: 785–792.
Young RM, Meyer IH. The trouble with "MSM" and "WSW": erasure of the sexual-minority person in public health discourse. Am J Public Health. 2005; 95: 1144–1149.
Semple SJ, Strathdee SA, Gallardo CM, Robertson A, Goldenberg S, Patterson TL. Psychosexual and social-cognitive correlates of sexual risk behavior among male clients of female sex workers in Tijuana, Mexico. AIDS Care. 2010; 22: 1473–1480.
Kalichman SC, Cain D. The relationship between indicators of sexual compulsivity and high risk sexual practices among men and women receiving services from a sexually transmitted infection clinic. J Sex Res. 2004; 41: 235–241.
Seal DW, Agostinelli G. Individual differences associated with high-risk sexual behaviour: implications for intervention programmes. AIDS Care. 1994; 6: 393–397.
Ostovich JM, Sabini J. How are sociosexuality, sex drive, and lifetime number of sexual partners related? Pers Soc Psychol Bull. 2004; 30: 1255–1266.
Kinsey A, Pomeroy W, Martin C. Sexual Behavior in the Human Male. Philadelphia, PA: Saunders; 1948.
Kinsey A, Pomeroy W, Martin C, Gebhart P. Sexual Behavior in the Human Female. Philadelphia, PA: Saunders; 1953.
Hewett PC, Mensch BS, Ribeiro MC, et al. Using sexually transmitted infection biomarkers to validate reporting of sexual behavior within a randomized, experimental evaluation of interviewing methods. Am J Epidemiol. 2008; 168: 202–211.
Simoes AA, Bastos FI, Moreira RI, Lynch KG, Metzger DS. A randomized trial of audio computer and in-person interview to assess HIV risk among drug and alcohol users in Rio De Janeiro, Brazil. J Subst Abuse Treat. 2006; 30: 237–243.
Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ. Audio computer assisted self interview and face to face interview modes in assessing response bias among STD clinic patients. Sex Transm Infect. 2005; 81: 421–425.
Kurth AE, Martin DP, Golden MR, et al. A comparison between audio computer-assisted self-interviews and clinician interviews for obtaining the sexual history. Sex Transm Dis. 2004; 31: 719–726.
Acknowledgments
The authors would like thank the men who provided personal information for the study. This study was supported by the National Cancer Institute (1R03CA134204 and RO1CA098803 (ARG)).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publication and report contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCI/NIH.
Rights and permissions
About this article
Cite this article
Ompad, D.C., Bell, D.L., Amesty, S. et al. Men Who Purchase Sex, Who Are They? An Interurban Comparison. J Urban Health 90, 1166–1180 (2013). https://doi.org/10.1007/s11524-013-9809-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-013-9809-8