Abstract
Among inner-city populations in Canada, the use of crack cocaine by inhalation is prevalent. Crack smoking is associated with acute respiratory symptoms and complications, but less is known about chronic respiratory problems related to crack smoking. There is also a gap in the literature addressing the management of respiratory disease in primary health care among people who smoke crack. The purpose of our study was to assess the prevalence of acute and chronic respiratory symptoms among patients who smoke crack and access primary care. We conducted a pilot study among 20 patients who currently smoke crack (used within the past 30 days) and who access the “drop-in clinic” at an inner-city primary health care center. Participants completed a 20- to 30-min interviewer-administered survey and provided consent for a chart review. We collected information on respiratory-related symptoms, diagnoses, tests, medications, and specialist visits. Data were analyzed using frequency tabulations in SPSS (version 19.0). In the survey, 95 % (19/20) of the participants reported having at least one respiratory symptom in the past week. Thirteen (13/19, 68.4 %) reported these symptoms as bothersome. Chart review indicated that 12/20 (60 %) had a diagnosis of either asthma or chronic obstructive pulmonary disease (COPD), and four participants (4/20, 20 %) had a diagnosis of both asthma and COPD. Majority of the participants had been prescribed an inhaled medication (survey 16/20, 80 %; chart 12/20, 60 %). We found that 100 % (20/20) of the participants currently smoked tobacco, and 16/20 (80 %) had smoked both tobacco and marijuana prior to smoking crack. Our study suggests that respiratory symptoms and diagnoses of asthma and COPD are prevalent among a group of patients attending an inner-city clinic in Toronto and who also smoke crack. The high prevalence of smoking tobacco and marijuana among our participants is a major confounder for attributing respiratory symptoms to crack smoking alone. This novel pilot study can inform future research evaluating the primary health care management of respiratory disease among crack smokers, with the aim of improving health and health care delivery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Among inner-city populations in Canada, the use of crack cocaine by inhalation has been reported as prevalent among injection drug users,1 illicit opioid users,2 and homeless adults.3
There are several acute respiratory complications of smoking crack cocaine, including acute exacerbations of asthma, pneumothorax, pulmonary edema, interstitial pneumonitis, diffuse alveolar hemorrhage, bronchiolitis obliterans with organizing pneumonia, “crack lung” (acute pulmonary infiltrates associated with a spectrum of clinical and histological findings), and thermal airway injury.4,5
Additionally, crack smoking is associated with acute respiratory symptoms of cough with black sputum, wheeze, hemoptysis, chest pain, and shortness of breath.4,5 However, less is known about chronic respiratory problems related to crack smoking. Some evidence suggests higher rates of respiratory diagnoses among people who use crack. For example, a survey of homeless adults who smoke crack revealed a higher incidence of asthma and chronic obstructive pulmonary disease (COPD) as compared to people who did not use crack.3
People who use crack are a particularly vulnerable group. Although the Canadian health care system offers universal coverage for physician and hospital services, marginalized groups, such as crack users, experience multiple barriers to health and health care such as homelessness, survival sex work, physical and mental illness, incarceration, and physical and sexual victimization.3,6–11 In fact, homeless adults who use crack face worse access to shelter when compared to those who do not use crack.3
Currently, a wealth of literature exists exploring the health needs of injection drug users, including primary and public health services directed at injection drug use. Internationally, the World Health Organization recommends providing sterile injecting equipment to injection drug users.12 Provincially in Ontario, the Ministry of Health and Long-Term Care requires that local boards of health ensure access to sterile needles and syringes,13 and best practice recommendations for needle and syringe programs have been developed.14 This is not the case for patients who smoke crack, where a lack of both health care services and literature for addressing unique needs in this population exists.15–17
Considering that crack users are in significant need of primary care overall, this gap in the literature is surprising. One study of adult cocaine users (79 % of whom smoked crack cocaine) found that users of crack cocaine reported significantly more frequent medical visits than other cocaine users.18 Metsch et al. suggest that this finding may be complicated by gender, where men may use more emergent health care services while women who use crack cocaine may feel more inhibited overall from using health care services.19 This gap in the literature highlights the importance of the current study.
We hypothesize that acute and chronic respiratory symptoms and subsequent complications are common among people who smoke crack in an inner-city primary health care setting. Given the increased health risks, vulnerability of this particular group, and lack of knowledge regarding medical management, our study is important and can lead to future efforts toward improving the overall health of and health care delivery to people who smoke crack.
Methods
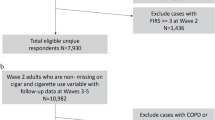
We conducted a pilot study among 20 patients who currently smoke crack (used within the last 30 days) and who access an inner-city “drop-in clinic” for primary health care. This interdisciplinary clinic provides primary health care to marginalized patients, some of whom smoke crack.
The clerical staff at the clinic initially screened all patients for the study when they attended the clinic and registered to be seen for health care. A standardized invitation page that provided a brief description of the study was used to recruit patients. Inclusion criteria were reviewed, and eligible patients were invited to participate. Inclusion criteria were as follows: age of 18 years or over, had smoked crack within the past 30 days, and able to speak and understand the English language. We excluded individuals who were unable to complete the survey, had previously participated in the survey, or were unable to give informed consent (e.g., intoxicated, experiencing a psychotic episode, or for any other reason, judged by the interviewer).
Eligible and interested participants then met with one of the interviewers (PL or NR) to receive additional information and review the consent form. Interviewers administered the survey to consenting participants over 20–30 min using a private space within the clinic. An interviewer-administered survey was used to adjust for low literacy levels among our study population. The interviewers were not involved in the direct care of the patients.
Participants were compensated CA$20 for their time completing the survey. With participants’ permission, survey information was supplemented with additional data from the clinic chart, including pertinent hospital records or investigations already contained within the chart involving respiratory illness.
We developed standardized chart extraction and survey forms, which were reviewed and piloted with the guidance of the entire group of investigators. Both sets of forms were used in a standardized fashion, agreed upon by the group, to eliminate variation between interviews/chart extractions. This study was reviewed and approved by the University of Toronto, Health Sciences Research Ethics Board.
Setting
At this clinic (the drop-in clinic), a family physician, nurse practitioner, and case coordinator provide comprehensive primary health care to people who experience challenges to accessing traditional primary health care models. Barriers facing many patients include substance use, homelessness, severe mental illness, and sex work. The clinic population can be considered representative of people who smoke crack in downtown Toronto and may extend to marginalized populations in Canada who use illicit drugs and receive primary care. We consider it likely that the patients at the clinic have social determinants of health similar to those in other inner-city clinics in large cities across Canada.
Statistical Analysis
We analyzed the results using frequency tabulations in SPSS version 19.0 to produce descriptive tables of our findings. There was no statistical testing of the amount of crack smoking and respiratory signs or symptoms due to the limited sample size of this pilot study.
Results
Twenty individuals participated in this pilot study. Demographic characteristics of the participants are summarized in Table 1.
The prevalence of respiratory symptoms among the participants is summarized in Figure 1 using information from the survey and chart review. This figure includes symptoms in the past week, during or shortly after smoking crack, and symptoms documented during clinical visits.
In the survey, 95 % (19/20) reported that they had at least one respiratory symptom in the past week. Only 15 % (3/20) reported no symptoms during or shortly after smoking crack. We found that 13/20 (65 %) reported their symptoms as bothersome. When asked about symptoms during a time of abstinence from crack, 13/19 (68.4 %) reported an improvement in their symptoms. These improved within 1 day to 3 months after stopping crack use (mean 23 days).
Table 2 summarizes the diagnoses of asthma and COPD reported in the survey and review of patient records. Four people (20 %) had a diagnosis of both asthma and COPD based on chart review data, and 12/20 (60 %) had either asthma or COPD listed in their chart.
The use of prescribed inhaled medication was reported more frequently among survey results than in the chart review (16/20, 80 % vs. 12/20, 60 %), but both findings suggest that the majority of participants had been prescribed an inhaled medication. Twenty-five percent (5/20) stated during the survey that they had used an inhaled medication before using crack for the first time. The most frequently used inhaled medications were fluticasone (chart 4/20, 20 %; survey 7/20, 35 %), salbutamol (chart 10/20, 50 %; survey 14/20, 70 %), and ipratropium (chart 10/20, 50 %; survey 3/20, 15 %). Additionally, the chart review revealed that 35 % (7/20) had been prescribed an antibiotic for pneumonia or acute exacerbation of COPD (AECOPD), and 15 % (3/20) had used prednisone for AECOPD or acute exacerbation of asthma.
Table 3 summarizes health service utilization in the past 6 months based on the survey results. In the chart review, we found that only two participants (2/20, 10 %) had an emergency room visit documented, two (2/20, 10 %) had a respirology consult, and three (15 %) had respiratory admission documented throughout their entire chart at the drop-in clinic.
Table 4 summarizes crack use patterns that participants reported in the survey. We found that 11/20 (55 %) reported having received treatment for crack use previously. The mean age at which crack was first used was 22.4 years old (range 15–37 years). Overall, participants reported using crack for a mean of 20.4 years (range 1–40 years), and crack use for an average of 15.55 days per month (range 1–30 days). Interestingly, 14/20 (70 %) of the participants reported a mean total usage of between 15–25 years, with two participants reporting 40 years of usage. We did not distinguish between freebased cocaine use versus crack use in our questionnaire, which may account for these two higher observations.
When we collected information about other inhaled substances, 100 % (20/20) reported on the survey that they were current smokers, with a mean of 28.89 pack years (range 2–100 years). Among the chart review data, we did not calculate a percentage of current smokers or mean number of pack years due to the large amount of missing data. Among the participants, 3/20 (15 %) reported on the survey that they smoked only tobacco prior to smoking crack, and 16/20 (80 %) had smoked both tobacco and marijuana prior to smoking crack. In the chart review, there was documentation of marijuana use for 10/20 (50 %) participants.
Among the participants, 6/20 (30 %) reported injection drug use in the past 6 months on the survey. Additionally, non-injection drug use in the past 6 months most frequently included alcohol (12/20, 60 %), marijuana (15/20, 75 %), and opiates (codeine 5/20, 25 %; oxycodone 4/20, 20 %; heroin 1/20, 5 %; percocet 1/20, 5 %).
Finally, we gathered information on relevant testing from the chart review. We found that 9/20 (45 %) had a chest X-ray included in their chart, and 5/9 (55.6 %) of these had had abnormal results. The abnormal findings on the chest X-ray included pleural effusion (1/20), hyperinflation (2/20), other (atelectasis and pleural thickening) (1/20), cavitations (1/20), and consolidation (2/20). There was one participant (1/20, 5 %) who had a CT scan report included in their chart—the results were abnormal (bullous emphysema). There were 3/20 (15 %) participants who had spirometry or pulmonary function tests recorded in their chart, and all had abnormal results.
Discussion
In summary, our study suggests that respiratory symptoms among crack smokers in primary health care are prevalent, and diagnoses of asthma and COPD are common in this group. For the respiratory symptoms defined in our survey, 95 % of participants reported having at least one present in the past week prior to being surveyed. Only 15 % reported not having any symptoms during or shortly after smoking crack. Black sputum (75 %) and shortness of breath (65 %) were the most frequently reported symptoms occurring during or shortly after smoking crack. Of those surveyed, 65 % felt that their symptoms were bothersome. Of the 19 participants who reported some period of abstinence from smoking, 68.4 % felt that abstinence from smoking led to improvement in their symptoms. Regardless of readiness to quit, these results suggest that a significant number of participants are aware of how crack smoking may affect their sense of respiratory health.
It is concerning that a high number of patients reported black sputum as a symptom. Whereas black sputum tends to signify serious respiratory pathology in a non-crack-smoking population, this finding was quite common among our study population, and this phenomenon has not been previously described in the literature. We feel that further study is warranted to determine how this symptom should be managed among patients who smoke crack.
The rates of asthma (45 %) and COPD (35 %) elicited through chart review and the survey far exceed the Canadian prevalence of 8.3 % (ages 12 years and older) and 4.4 % (ages 35 years and older), respectively.20 At least 60 % of participants were prescribed an inhaled medication for these conditions as evidenced in the chart review, and this may be higher given that 80 % of survey respondents recall using these medications at some point in their life.
Crack smoking is a risk factor for lack of health care access in Canada,6 and in our study, only 35 % of participants reported discussing their crack use with a primary care provider in the last 6 months, even in a setting where patients have a good rapport with their providers. The demographics in Table 1 suggest that our group face other social determinants of health related to the decreased access to health care discussed earlier.
Asthma and COPD are often managed in primary care, while acute life-threatening respiratory illness from crack smoking is managed in emergency rooms (ERs), which would explain our study’s low documented prevalence of acute illness. ER visits in the past 6 months were reported among 25 % of participants, although it was unclear if visits were for respiratory concerns. Primary health care providers might find value in frequently inquiring about visits to ERs to document awareness of acute pathology arising from crack use otherwise not presenting in primary care.
In a study looking at cigarette smokers and objective evidence of lung pathology,21 participants first underwent pulmonary function tests (PFTs) and were subsequently given counseling on how to quit. In the group of participants who had demonstrated lung impairment on PFTs, there was a higher 6-month rate of self-help material usage and counseling services compared to those who had no demonstrated lung impairment with testing. In our study, 90 % of the participants surveyed indicated that they would be interested in future monitoring of their respiratory status through special tests such as spirometry and PFTs. This suggests that investigation of lung function might help to promote health awareness among interested patients. Whereas formal PFTs may not be feasible in the drop-in clinic setting, office-based spirometry is likely more practical in caring for this population and has been recommended as an essential tool to be used by primary care providers.22,23
We believe that our study had a number of strengths. First, the “mixed methods” approach to data gathering (survey plus chart review) helped to provide a more comprehensive picture of symptoms, crack usage patterns, and relevant medical information than would have been available from one method alone.
Second, the clinic in our study is a supportive environment for our participants, where good rapport was established and where our surveys could be piloted and tested with drug users who volunteer with the clinic to ensure that they were appropriate. We felt that the harm-reduction-focused philosophy of the clinic and the local community allowed for more candid responses to be elicited from participants and that this in part may have helped validate our findings.
Third, the survey was partly designed based on the I-Track study in order to have comparable data with a larger national database. Indeed, some of our study’s demographic data were found to be comparable to the data found in I-Track.1 For example, 35 % of our participants lived in unstable housing (compared to 40 % in I-Track), and 25 % of our participants participated in some post-secondary education (compared to 22.9 % in I-Track). Because of our study’s similar demographics, we feel that similar respiratory symptoms may be found among individuals who smoke crack in other inner-city groups across the country. Lastly, the questions posed in our survey were meant to be directly relevant to primary care providers wanting to know more about how to provide appropriate care for patients who smoke crack, a priority concern which initiated this study.
Despite these strengths, our study has limitations. Our study was done at a single center with a small sample size and no comparison group. This limited us to a descriptive, hypothesis-generating analysis. Also, the high prevalence of smoking tobacco and marijuana among our participants is a major confounder for attributing respiratory symptoms to crack use alone. It is difficult to determine the true number of documented visits to emergency rooms, consultation notes from respirologists, test results from spirometry or thoracic imaging, and other data elements given that chart reviews are subject to missing data. We did not attempt to capture the relationship between HIV status and respiratory symptoms, although the HIV seroprevalence among this group is known to be about 4 % (Peggy Millson 2011, personal communication). We do not expect that the main outcomes we studied (COPD, asthma, chronic respiratory symptoms, and medications) were greatly influenced by HIV status in our group. Further, our recruitment rate was slower than expected and seemed to be related to significant variability in participants presenting to the clinic depending on whether their own trusted primary care provider was known to be not available for consultation.
Additionally, it was difficult to accurately quantify the amount of crack used by each participant. While the mode average of our participants’ usage was around 0.15 g per use, the range of reported usage was from 0.05 to 20 g per use, and we are uncertain of the reliability of these data as an estimate. This limits the understanding whether a dose–response relationship exists between respiratory symptoms and the amount of crack used. As well, the length of exposure to crack was difficult to quantify as the range of years of crack smoking reported in our study likely exceed the plausible history of crack usage in this geographic region. As mentioned earlier, our study did not distinguish between freebased cocaine and crack use, and this may have affected our estimation of the duration of use. Further studies on the dose–response relationship between symptoms and the amount and duration of use may likely require methods of verifying self-reported data as well as clarifying the forms used. It is nonetheless vital that, based on findings from this study, clinicians who work with patients who smoke crack identify the presence of respiratory symptoms, especially with multiple exposures.
The current pilot study solely focused on providing an initial description of the respiratory effects of smoking crack; however, it raises interesting findings for further investigation. More research is needed to estimate the respiratory effects of smoking crack. Additionally, an understanding of the impact of crack smoking on health care utilization would be important. Considering that our participants’ mean age was 44, it would be of value in future studies on crack-smoking populations to capture detailed and accurate information on age-related illness.
Our study suggests that acute and chronic respiratory illnesses are an issue that primary care providers will need to be aware of in managing their patients who smoke crack. A larger multicenter study will be important in establishing true prevalence of respiratory symptoms and pathology related to crack usage. Future research could aim to correlate symptoms with spirometry results. This could also lead to better understanding of chronic respiratory problems among crack smokers and their providers and may increase engagement with patients to monitor their respiratory status with their primary care provider. With more information available on the chronic respiratory effects of crack and comorbid inhaled substances, we hope that we can optimize the management of symptoms and that there may be increased opportunities to reduce the burden of illness associated with crack smoking.
In summary, our study suggests that respiratory symptoms and diagnoses of asthma and COPD are prevalent among a group of patients attending an inner-city clinic in Toronto and who also smoke crack. The high prevalence of smoking tobacco and marijuana among our participants is a major confounder for attributing respiratory symptoms to crack smoking alone.
References
Public Health Agency of Canada. I-Track: enhanced surveillance of risk behaviours among people who inject drugs. Phase I report. 2006. http://www.phac-aspc.gc.ca/i-track/sr-re-1/pdf/itrack06_e.pdf. Accessed 28 Sept 2011.
Fischer B, Rehm J, Brissette S, et al. Illicit opioid use in Canada: comparing social, health and drug use characteristics of untreated users in five cities (OPICAN study). J Urban Health. 2005; 82: 250–266.
Khandor E, Mason K. Research bulletin #3: homelessness and crack. In The Street Health Report. Street Health, 2008. http://www.streethealth.ca/Downloads/SHResearchBulletin-3.pdf. Accessed 28 Sept 2011.
Tashkin DP. Airway effects of marijuana, cocaine, and other inhaled illicit agents. Curr Opin Pulm Med. 2001; 7(2): 43–61.
Haim DY, Lippmann ML, Goldberg SK, Walkenstein MD. The pulmonary complications of crack cocaine. A comprehensive review. Chest. 1995; 107(1): 233–240.
Fischer B, Rehm J, Patra J, et al. Crack across Canada: comparing crack users and crack non-users in a Canadian multi-city cohort of illicit opioid users. Addiction. 2006; 101(12): 1760–1770.
Fischer B, Coghlan M. Crack use in North American cities: the neglected ‘epidemic’. Addiction. 2007; 102: 1340–1341.
Butters J, Erickson PG. Meeting the health care needs of female crack users. Women Health. 2003; 37(3): 1–17.
Falck RS, Wang J, Siegal HA, Carlson RG. The prevalence of psychiatric disorder among a community sample of crack cocaine users: an exploratory study with practical implications. J Nerv Ment Dis. 2004; 192: 503–507.
Ross MW, Hwang LY, Zack C, Bull L, Williams ML. Sexual risk behaviours and STIs in drug abuse treatment populations whose drug of choice is crack cocaine. Int J STD AIDS. 2002; 13: 769–774.
Khandor E, Mason K, Chambers C, Rossiter K, Cowan L, Hwang SW. Access to primary health care among homeless adults in Toronto, Canada: results from the Street Health survey. Open Med. 2011; 5(2): e94–e103.
World Health Organization. Policy brief: provision of sterile injecting equipment to reduce HIV transmission. WHO, 2004. http://www.who.int/hiv/pub/idu/e4a-needle/en/index.html. Accessed 28 Sept 2011.
Ministry of Health and Long-Term Care. Ontario public health standards 2008. http://www.health.gov.on.ca/english/providers/program/pubhealth/oph_standards/ophs/progstds/pdfs/ophs_2008.pdf. Accessed 28 Sept 2011.
Strike C, Leonard L, Millson M, Anstice S, Berkeley N, Medd E. Ontario needle exchange programs: best practice recommendations. Ontario Needle Exchange Coordinating Committee, 2006. http://www.health.gov.on.ca/english/providers/pub/aids/reports/ontario_needle_exchange_programs_best_practices_report.pdf. Accessed 28 Sept 2011.
Malchy L, Bungay V, Johnson J. Documenting practices and perceptions of ‘safer’ crack use: a Canadian pilot study. Int J Drug Policy. 2008; 19(4): 339–341.
Leonard L, DeRubeis E, Pelude L, Medd E, Birkett N, Seto J. “I inject less as I have easier access to pipes”: injecting, and sharing of crack-smoking materials, decline as safer crack-smoking resources are distributed. Int J Drug Policy. 2008; 19(3): 255–264.
Haydon E, Fischer B. Crack use as a public health problem in Canada: call for an evaluation of ‘safer crack use kits’. Can J Public Health. 2005; 96(3): 185–188.
Ottaway CA, Erickson PG. Frequent medical visits by cocaine-using subjects in a Canadian community: an invisible problem for health practitioners? J Subst Abuse Treat. 1997; 14(5): 423–429.
Metsch LR, McCoy HV, McCoy CB, Miles CC, Edlin BR, Pereyra M. Use of health care services by women who use crack cocaine. Women Health. 2000; 30(1): 35–51.
Public Health Agency of Canada. Life and Breath: Respiratory Disease in Canada. Ottawa: Public Health Agency of Canada; 2007.
McClure JB, Ludman EJ, Grothaus L, Pabiniak C, Richards J. Impact of spirometry feedback and brief motivational counseling on long-term smoking outcomes: a comparison of smokers with and without lung impairment. Patient Educ Couns. 2010; 80(2): 280–283.
Kaplan A, Stanbrook M. Must family physicians use spirometry in managing asthma patients? YES. Can Fam Physician. 2010; 56(2): 126, 128, 130, 132, discussion e49, e51.
Stanbrook MB, Kaplan A. The error of not measuring asthma. CMAJ. 2008; 179(11): 1099–1102.
Acknowledgments
The University of Toronto, Department of Family and Community Medicine supported this project through the funding allotted to family medicine residents to conduct research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leece, P., Rajaram, N., Woolhouse, S. et al. Acute and Chronic Respiratory Symptoms among Primary Care Patients Who Smoke Crack Cocaine. J Urban Health 90, 542–551 (2013). https://doi.org/10.1007/s11524-012-9780-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-012-9780-9