Abstract
Approximately 17% of individuals living with HIV/AIDS pass through the correctional system each year. Jails provide a unique opportunity to diagnose and treat HIV infection among high-risk, transient populations with limited access to medical services. In 2007, the US Health Resources and Services Administration funded a multi-site demonstration project entitled Enhancing Linkages to HIV Primary Care in Jail Settings that aims to improve diagnosis and treatment services for HIV-positive jail detainees and link them to community-based medical care and social services upon release. We performed an evaluation of the Rhode Island demonstration site entitled Community Partnerships and Supportive Services for HIV-Infected People Leaving Jail (COMPASS). Through in-depth qualitative interviews among 20 HIV-positive COMPASS participants in Rhode Island, we assessed how COMPASS impacted access to health care and social services utilization. Most individuals were receiving HIV treatment and care services upon enrollment, but COMPASS enhanced linkage to medical care and follow-up visits for HIV and other co-morbidities for most participants. Several participants were successfully linked to new medical services as a result of COMPASS, including one individual newly diagnosed with HIV and another who had been living with HIV for many years and was able to commence highly active antiretroviral therapy (HAART). While many individuals reported that COMPASS support prevented substance abuse relapse, ongoing substance abuse nevertheless remained a challenge for several participants. Most participants enrolled in one or more new social services as a result of COMPASS, including Medicaid, Supplemental Security Income, food assistance, and housing programs. The primary unmet needs of COMPASS participants were access to mental health services and stable housing. Intensive case management of HIV-positive jail detainees enhances access to medical and social support services and helps prevent relapse to substance abuse. Expanding intensive case management programs, public housing, and mental health services for recently released HIV-positive detainees should be public health priorities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
More than one million Americans live with HIV, 25% of whom are unaware of their status.1 Additionally, an estimated one third of those who are aware of their positive status do not receive medical care.2 Approximately 17% of HIV-positive Americans pass through the correctional system every year3 and HIV prevalence among the incarcerated population is nearly 2.5 times general population prevalence.4 The incarcerated population faces increased risk of homelessness, unemployment, and other challenges upon return to the community.5–9 Recently released inmates are also more likely than the general population to engage in HIV risk behaviors such as transactional sex, multiple sexual partnerships, and injection drug use.10–12 These phenomena have detrimental impacts on inmate and community health and frequently limit access to HIV/AIDS treatment and care services.13–17
Jails are the port of entry to the correctional system, including prisons. Almost one quarter of jail detainees are released within 2 weeks,18 creating a highly transient population whose only access to HIV testing and medical care may be in jail. Jails therefore present unique opportunities to diagnose people living with HIV/AIDS and initiate care. Linking HIV-positive jail detainees to clinical and social services upon release can have a significant beneficial impact on the health of these individuals, as well as the public health of the communities to which they return.19–22
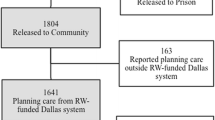
Despite demonstrated success of linkage to care programs for HIV-positive prisoners, few programs link HIV-positive jail detainees to medical and social services upon release from jail. In 2007, the Health Resources and Services Administration funded a multi-site program to expand the diagnosis of HIV during jail incarceration and establish programs to link HIV-positive jail detainees to comprehensive HIV primary care in the community upon release.23 This program, the Enhancing Linkages to HIV Primary Care and Services in Jail Settings,24 has ten demonstration sites in the USA, including the Miriam Hospital in Providence, RI, USA, the largest provider of HIV care in Southern New England. This program at the Miriam Hospital, the Community Partnerships and Support Services for HIV-Infected People Leaving Jail (COMPASS) program, links HIV-positive jail detainees from the Rhode Island Department of Corrections (RIDOC) jail to HIV care and other clinical and social services in the community.
COMPASS community outreach workers are notified by jail staff when a detainee is newly identified as HIV-positive or when persons with chronic HIV infection are incarcerated. COMPASS staff meets with detainees in jail as soon as possible after intake to assess their medical and social support needs. Upon their release from jail, COMPASS staff provides direct case management services to assist with linkage to community HIV services, substance abuse treatment, mental health care services, health insurance programs including the AIDS Drug Assistance Program (ADAP), and other public assistance programs. COMPASS services are provided for 6 months after jail release.
Little scientific literature examines HIV-positive jail inmates’ experiences with medical and social support programs post-release; we found only one study exploring the specific medical and social service needs of this population.25 To our knowledge, no peer-reviewed articles have examined recently released HIV-positive jail inmates’ experiences with programs designed to enhance their participation in medical care and social support services. To fill this gap, we conducted a qualitative assessment with 20 COMPASS participants. This study evaluates how participating in COMPASS in Rhode Island impacted jail inmates’ access to health care and social services.
Methods
Recruitment
COMPASS staff recruited COMPASS participants to participate in the qualitative study soon after release from jail. Eligible participants were active in COMPASS, ≥18 years old, HIV positive, and English speaking. We enrolled the first 20 eligible COMPASS program participants from the RIDOC; enrollment took place between October 2008 and September 2009, during which time a total of 30 jail detainees were enrolled in the COMPASS program. All participants provided written and verbal informed consent. The study was approved by the Miriam Hospital IRB and the RIDOC Medical Research Advisory Group.
Qualitative Interviews
We used a semi-structured interview approach. In this qualitative interviewing method, a trained interviewer uses a loosely structured interview guide that includes a core list of themes to be discussed in the interview. The interview guide includes open-ended questions and allows both the participant and interviewer freedom to introduce topics freely as appropriate, allowing interviewers to probe about participants’ responses. This approach focuses on answering questions included in the subject guide in a conversation that flows naturally rather than in an order pre-determined by the interviewer.26 , 27 Three trained research assistants conducted in-depth qualitative interviews with COMPASS clients between 4 and 12 weeks after their release from jail. Demographic information was also collected.
In semi-structured interviews, participants were asked about their medical and social needs upon release and how the COMPASS program impacted access to clinical and social services in jail and upon release. For example, we asked participants questions such as, “Can you tell us about your experiences with HIV/AIDS-related medical services in jail and upon release?” and “How has the COMPASS program impacted your access to HIV/AIDS care services since your release from jail?” as well as “How has COMPASS program affected your enrollment and access to social services such as housing, food stamps and mental health services?” Participants were also asked about their HIV risk behaviors, including drug and alcohol use and sexual behaviors post-release. For example, we asked patients “Are you currently sexually active? Can you tell me more about your sexual activity since your release from jail?” We also asked participants about whether they were currently engaged in substance use, such as: “Are you currently using drugs of any kind? Can you tell us how drug use, if any, has impacted your participation in HIV/AIDS treatment and care services?” We also asked participants “How could we improve COMPASS services?” These broad, open-ended questions were designed to launch in-depth conversations about the aforementioned subject matter, and trained interviewers then probed about further details when they sought more information than participants offered in initial responses.
Data Analysis
Descriptive statistics of the participant population were tabulated. Interviews were professionally transcribed. Emerging themes related to medical and social service utilization, emotional support, and suggestions for enhancing COMPASS were documented following each interview and informed development of a coding scheme to guide data analysis. To enhance validity and reliability of the study findings, more than one analyst coded each transcript. We encountered only minor discrepancies in coding across analysts; the small discrepancies (approximately 5%) were discussed and resolved among data analysts with the input of the principal investigator. As themes emerged from the data coding process, analytic memos were drafted to summarize the key findings of each interview and systematically link important ideas and themes between respondents. These themes informed the findings we present. This coding and analysis method follows typical convention used in analyzing qualitative interviews.28 , 29
Results
Demographic Data
Participant demographics are summarized in Table 1. The demographic profile of those participating in this study is similar to those enrolled in the COMPASS program in Rhode Island. Three quarters of participants were male and almost all were single; the average participant age was 41 years. Race, education level, and sexual practices varied widely. All participants were unemployed or underemployed, and those with health insurance were enrolled in public health insurance programs. Participants had been incarcerated an average of 15 times during their lifetimes. One participant was newly diagnosed with HIV during her most recent incarceration; the remaining 19 participants had been living with HIV an average of 12 years. Twelve participants were diagnosed with HIV while incarcerated in jail or prison, 11 of whom were diagnosed at the RIDOC.
Linkage to Community-Based Medical Care
HIV/AIDS Care
Most study participants had been living with HIV for many years and 11 were already engaged in HIV/AIDS care upon enrollment. This is primarily attributable to previous incarcerations and participation in Project Bridge, a local program that links HIV-positive prison inmates to care upon release. However, COMPASS helped several participants re-initiate care after long-term lapses. One participant receiving routine HIV care as a result of COMPASS commented:
Sometimes, before I got incarcerated, it was like a year, almost 2 years that I didn’t see the doctor. I didn’t take blood work, I didn’t do anything. I was just out there. And they looked for me. They’d call the house.
Other participants commented that COMPASS helped them keep medical appointments. For example, a participant who had frequently been lost to medical follow-up in the past explained:
I just started this program last month, so I haven’t missed any appointments since last month. I’ve got a doctor’s appointment next month.
One participant newly diagnosed with HIV was linked to care at the Miriam Hospital Immunology Center. She explained how COMPASS helped her improve access to medical and social services:
I don’t do doctors, I don’t do appointments, I don’t do court. Nothing! If it didn’t have to do with from the block of my house to the block where the drug dealer was, I did not go...I had my own little circle of life...if it wasn’t for [COMPASS staff member] or anyone I wouldn’t have anything that I have right now. And I have a lot...I have another appointment. My doctors do want to keep track of me because it’s the beginning. She said for the first couple months she wants to see me every month, and I think that’s to see how I’m getting along emotionally, how I’m coping....
While most individuals were successfully accessing routine HIV care, relapse to substance abuse and re-incarceration interrupted HIV treatment and care services for numerous participants. One participant who re-initiated HIV care through COMPASS explained:
I’ve been ducking my doctor for the past maybe two, three months because it’s been the same, same old story, same old story. “[He’s] relapsed. [He’s] in the hospital. [He’s] in jail.” And I don’t want that....My doctor is going to be so happy to see me.
A few participants identified difficulty accessing transportation as an impediment to attending medical appointments; two mentioned that COMPASS staff had provided transportation and assistance in acquiring bus passes for long-term transportation.
HAART Treatment and Adherence
Nearly all participants (16) reported taking highly active antiretroviral therapy (HAART) at the time of the interview and generally reported high rates of adherence. Others commenced HAART as a result of COMPASS or were linked to the local ADAP. One treatment-naïve participant who had been diagnosed with HIV in 1997 explained how COMPASS influenced her decision to initiate HAART:
I thought, why live? I’m still going to die. That was the way I was thinking. I didn’t want to take medication...So all those years I was with no medication so I got really sick...Now I want to go through medication and I think I do want to live. I want to take my medications. I want to go to the doctor. [COMPASS] brightened up my spirits a little bit...Really, when I got locked up, and I met [COMPASS staff member] and went to the COMPASS program, and being clean, I guess made me just want to keep on living...I’ve been on my medication for 2 months now and I feel much better....I’m loving it.
Among other participants, drug and alcohol use were cited as impediments to adhering to HAART. One respondent commented:
The only time I have a problem is when I relapse. I don’t take them because I don’t eat.
Another individual who reported active cocaine use and poor adherence to HAART remarked:
If you’re going to miss doses they, they [doctors] just tell you not to take the pills at all.
Treatment of Co-Morbidities
Many participants reported histories of sexually transmitted infections (STIs), but none reported recent or current STIs. Hepatitis C (HCV) was the most commonly reported HIV co-morbidity; seven participants were infected with HCV and all were diagnosed prior to COMPASS enrollment. Four participants reported currently being under a physician’s care for HCV, and several participants attributed their access to HCV care to their participation in COMPASS. For example, a participant who had fallen out of HCV care for several years because of substance abuse explained that he commenced HCV care again after enrolling in COMPASS:
In 2005, I went for a liver biopsy and I was supposed to come back for the results in January of 2006, but I relapsed. So I was in the streets again until I overdosed in May, and so [after COMPASS], I started getting back to my appointments.
Mental Health and Counseling Services
Many participants expressed the need for greater access to mental health services. Most participants discussed histories of depression, suicidal ideation and attempts, and other kinds of emotional distress, but did not report a history of formal mental health diagnoses. Individuals attributed these mental health issues to living with HIV/AIDS, drug use and other social challenges. One participant who has been living with HIV for 11 years reported:
To this day I’m still depressed....it still hurts knowing that I’m HIV positive.
Others who had not sought mental health services or counseling through COMPASS commented:
It [my HIV diagnosis] hasn’t been all roses....I don’t cope with reality too well. This is why I need counseling.
[Living with HIV] has led to drug problems, it’s led to loneliness, it’s led to attempted suicide.
However, two participants reported COMPASS staff were actively assisting them access professional mental health services. Another participant who reported long-term depression explained that he was considering seeking new treatment for depression as a result of COMPASS:
I do have metal health problems though...I’ve been on every medication you could possibly name...[COMPASS staff] and I have discussed it and am working on finding treatment options.
Linkage to Social Services in the Community
Fourteen participants were able to access one or more new social services as a result of COMPASS, such as housing, food stamps, employment programs, and other services from local AIDS service organizations. A participant linked to numerous social support services through COMPASS remarked:
I’m obtaining a lot of things from a lot of different facilities—[AIDS Service Organizations], Food Banks—all the resources that are in my area that I knew nothing about. And I haven’t done without anything. Nothing! I mean, I needed cosmetics, soaps and whatever, and I went down to one of the places that [COMPASS staff] said...the food bank only for HIV people. And I thought they were just going to help me out with food services....This woman hands me this big basket...and this is everything I needed! And I thought, ‘Oh wow!’ I haven’t gone without anything since I’ve been talking with everybody [in COMPASS]. And I have a list of names if I have any questions or, or anything, I can call, I have cell phone numbers.
The most frequently reported unmet need was housing assistance. Fourteen participants had unstable or temporary housing, and indicated that permanent housing was the first step to a stable lifestyle, reducing drug use, and accessing health care. One participant explained:
So that’s why most of the time when you get out of jail and you don’t have nowhere to go, people go back to drugs, and back to the same thing. Back to the same circle because they don’t have anywhere else to go...[COMPASS staff member] was going to help me go in a sober house, so I wasn’t really going to go to the streets.
Many described how COMPASS staff helped them access public housing programs:
She’s going to go through the housing lists and see what she can do for me in housing. I’m going to have another meeting with her in two weeks.
Additionally, a few participants noted that COMPASS staff assisted them in addressing legal matters such as child support. One participant noted the important support of the COMPASS staff during his court case after release from jail. Many participants also noted receiving COMPASS assistance in obtaining government identification, such as social security cards, birth certificates, and driver’s licenses.
I’ve got all my papers already, [COMPASS staff] helped me get all the stuff, so I got my ID, my birth certificate already, I got everything.
Five participants did not have medical insurance at the time of the interview, and four of them reported actively working with COMPASS to apply for public health insurance programs. One respondent commented:
I think Miriam Hospital is giving me health insurance. I really don’t have one myself, but they’re helping me over there...[COMPASS staff] took me to the SSI to sign up for social security.
Another participant already enrolled in Medicaid discussed exploring other public insurance options through COMPASS:
In our upcoming meeting we’re going to explore different avenues for better health insurance, and looking at different health insurance options.
COMPASS and Community Transition
Nearly all participants commented that COMPASS facilitated their community transitions upon release from jail. One participant who had been incarcerated over 35 times was newly diagnosed with HIV during her most recent incarceration. She explained how COMPASS improved her community transition and helped her engage in a healthier lifestyle:
The way I transitioned out this time was probably the best transition I’ve had the whole entire time...pretty much I came out looking forward to nothing. I wasn’t going back to the home I was living in, didn’t know if it was still there. Didn’t know if my clothes were still there....But the transition coming out [of jail] this time was the best that I’ve had the whole entire time that I’ve ever done prison time....because the response to my HIV diagnosis was so good...[COMPASS] response team has been a godsend! I know how to hustle and keep a house, but I don’t know how to keep a house without hustling. And for 20 years hustling was all I knew. So I’m actually learning how to actually have a normal life.
Another participant noted:
COMPASS should be an essential part of reentry for people with HIV, instead of just a study.
Many participants commented on the critical role of COMPASS home visits. For example:
[COMPASS staff] made the initiative to contact me when I was released...She called me up, said ‘Guess what? You’re getting in here. You got an appointment with me.’ I said ‘I can’t make it.’ She said ‘Well I’m coming to see you then.’ I was very grateful for that, because I probably wouldn’t have taken the initiative for a little while, made the contact. Her visit gives me the energy to get up in the morning, to know that somebody’s still around that once again cares. Somebody cares.
Nearly all participants explained how COMPASS provided unique emotional support in their daily lives. Several participants explained:
Changes in my daily life are that I’m not walking alone. I’m walking with them [COMPASS staff]. They’re carrying this load that I’m carrying, that I was carrying by myself. I’m opening up to them...It’s good to have people like that. They understand. They don’t judge you. My family judged me right away. They help me one week and if I relapse well, ‘The hell with you. I’m tired with you. You’re never going to change. There’s no hope for you.’ See with [COMPASS], there is hope. They see that. They see potential in me; they see something that I can’t see now. If they can help me, they will help me. Which a lot of people, even my own family, don’t understand; they don’t understand my drug addiction; they don’t understand my disease. And you can’t talk to them. So who do you go to? People like [COMPASS staff member].
[She asked me] What do you need?’ Nobody’s every asked me that! And it’s people like her and programs like this that help me get through life.
Another participant, who discussed how COMPASS provided critical emotional support for him, remarked:
...people that are HIV [positive], their main issues, their emotional issues, their soul issues, their spiritual issues are not being addressed. And those, to me, from my experience and from what I see, are the most critical things.
However, a few participants mentioned that they might not have joined a program like COMPASS at the time of HIV diagnosis, citing emotional turmoil or denial about being HIV positive:
I don’t know if I could have talked to anybody. I talked to the priest because he was a man from God. I could talk to a man like that. But I don’t think I could talk to nobody else, no, I couldn’t. Honestly speaking, I don’t think so. I don’t care what they would have said to me, I would have said, ‘The hell with you, I’m going to die.’
I was real isolated at the time. I didn’t want to speak to nobody. I didn’t want to be involved. I just needed time to heal.
I just started trying to erase it out of my mind that I was sick. I didn’t believe it because I was in prison. I thought these people were playing a trick on my mind. I got out of prison and never followed up. Because I didn’t believe it. Because I felt healthy. I didn’t look sick.
COMPASS and Relapse to Substance Abuse
All 20 participants had a history of illicit drug use. The most commonly used drugs were cocaine and alcohol; other participants reported previous or active heroin use. Many individuals reported substance use as reasons for missing doctor’s appointments and not adhering to medications. Many participants struggled with relapse to drug use, and one participant reporting receiving opiate substitution therapy reported active cocaine use:
I’m on Suboxone now. But I smoke coke every day and I don’t do dope [heroin] anymore...That’s what happens, though, when you have a double addiction. You pick up hard on one when you give the other one up.
Another participant reported relapsing to drug use between his release from jail and the first meeting with COMPASS staff:
I was supposed to meet up with [COMPASS staff] before, but I went off the deep end...I was doing drugs, including crack.
Several participants were already involved in both jail and community-based substance use treatment programs. One participant who reported he had not yet disclosed his ongoing drug use to COMPASS staff stated:
Being incarcerated kind of helped, but I did the [jail-based drug cessation program] while I was there. And they were very helpful...I told my parents and again, they’ve been very supportive. And I’ve gone to a couple of meetings...I’ve gone to Narcotics Anonymous, Alcoholics Anonymous.
Six participants indicated that support from COMPASS staff played a direct role in helping prevent relapse to drug and alcohol use.
A step at a time. First take care of me, my addiction. With the addiction, I can’t do anything. With this drug addiction I cannot move forward, so I’ve got to work on that. So I’m doing the outpatient counseling. And with the support of [COMPASS] and other friends that are very positive people, they’re not using, that I can call and hang around with. So it’s a step at a time. It’s, it’s a process. But I’m willing to try. It’s never too late.
[COMPASS] has given me a sense of direction in terms of learning how to live a productive lifestyle. How to live a safe lifestyle without having to get caught up in drugs. Because when I’m feeling down or feeling like I want to use, I know that I can pick up the phone and call [COMPASS]...I know that they could steer me in the right direction. I can’t get this kind of support hanging at crack houses and shooting galleries because people are doing the same thing you’re doing. They’re getting high, so they don’t really have anything to offer. So it’s important for me to stay plugged into these kinds of programs so that I can live a more productive lifestyle.
Discussion
To our knowledge, this is the first peer-reviewed article to explore the experiences of recently released HIV-positive jail inmates enrolled in a program designed to enhance participation in medical care and social support services. We found that the COMPASS program has positively impacted linkage to HIV care and other services for HIV-positive jail inmates in Rhode Island. However, it is noteworthy that many COMPASS participants who were interviewed were already engaged in HIV/AIDS care prior to enrolling in the program. This is likely attributable to several factors. First, most participants had been living with HIV for over a decade and had previously been linked to care. Additionally, since the early 1990s, Brown University/Miriam Hospital and the RIDOC have worked collaboratively to maintain continuity of HIV care during incarceration and upon community re-entry. This is achieved by having HIV care providers who work both inside the RIDOC and in the community and through similar case-management-based linkage services for HIV-positive prisoners30 Furthermore, the RIDOC has been offering routine opt-out HIV testing upon incarceration since 1991 and 15–30% of all HIV diagnoses in RI have been identified at RIDOC.31 , 32 Consequently, HIV-positive persons interacting with the criminal justice system in RI have likely been engaged in care in the past and are familiar with HIV services inside RIDOC and in the community.
However, our findings suggest that COMPASS enhanced existing programs in several ways. One individual was newly diagnosed in jail and was linked to community HIV/AIDS care at the Miriam Hospital and numerous social services as a result of COMPASS. COMPASS enhanced other individuals’ continuity of HIV/AIDS care through intensive case management, including reminding participants to keep doctors’ appointments and assisting with transportation services. Additionally, COMPASS enhanced linkage to care for important co-morbidities such as hepatitis C, a leading cause of death for people living with HIV/AIDS in the USA.33 Moreover, COMPASS helped link participants to public health insurance programs they might otherwise not have accessed, including ADAP. COMPASS also improved access to social services that are critical to reducing the challenges associated with community re-entry, including access to housing assistance, food stamps, and community programs that provided other necessities. However, it is worth noting that a few participants commented that they might not have responded to COMPASS staff immediately after their HIV diagnosis if such a program had been offered to them. This finding suggests that ongoing outreach and follow-up case management services are critical for linking HIV-positive inmates to care and social services after release.
All study participants had a history of substance use, and several actively used drugs since jail release. Many participants explained that COMPASS helped prevent relapse to substance use since jail release, and relapse prevention has been shown elsewhere to promote adherence to HAART,34 , 35 reduce recidivism and drug-related health harms,36 and enhance secondary HIV prevention.37–39 However, several participants reported actively engaging in substance use and commented that their substance use relapse reduced their adherence to HAART and continuity of medical care. While unsurprising, this finding suggests that preventing relapse to substance use should remain a priority for case management programs that assist HIV-positive persons released from correctional facilities.
The greatest unmet need study participants reported was mental health services. Many study participants reported experiencing emotional distress, depression, or histories of suicidal ideation. While COMPASS staff often provided critical social and emotional support, many participants reported feelings of depression and expressed the need for counseling or psychiatric services. These trends are common among incarcerated inmates; half of all prison and jail inmates have at least one mental health disorder.40 Moreover, inmates with mental health problems are more likely to have used drugs in the month prior to incarceration, be homeless, and have repeat incarcerations.40 , 41 Additionally, HIV-positive prisoners are more likely to have underlying mental health disorders than HIV-negative prisoners.41 These phenomena underscore the critical importance of providing emotional support services and links to mental health services for recently released HIV-positive inmates.
Many participants also reported that unstable housing exacerbated their substance use problems and complicated their community transition. This is consistent with literature demonstrating how stable housing can help reduce relapse to substance abuse following release from jail42 , 43 and enhance adherence to HAART.16 , 44 While COMPASS staff assisted with public housing applications, Rhode Island has a long waiting list for public housing for HIV-positive individuals. However, participants’ comments highlight the downstream medical and social consequences of unstable housing for recently released inmates and suggest that structural factors also play a key role in the health and social stability of recently released HIV-positive inmates.
Our study is subject to several limitations. First, our findings may be subject to some selection bias; study participants may have had more positive experiences with the COMPASS program than individuals who did not enroll in our study. However, given the extensive efforts of COMPASS staff to enroll all eligible participants in the COMPASS program, we estimate any potential bias as relatively minor. Additionally, this evaluation was limited to self-report of medical service uptake, HAART adherence, and substance use. Finally, this study is based on a small sample of individuals recently released from jail in Rhode Island who were enrolled in the COMPASS program. RIDOC’s historical collaboration with community HIV care providers may not be representative of the US correctional system at large.
However, this qualitative study highlights the benefits of intensive case-management programs for HIV-positive jail detainees upon community re-entry. COMPASS enhanced linkage to community HIV care, improved evaluation and treatment of other co-morbidities, improved access to social support programs, reduced relapse to substance use, and provided critical emotional support to clients. This study also underscores the critical need for improved access to mental health services and public housing for HIV-positive inmates upon release from jail. While the Rhode Island COMPASS experience may not be generalizable to all settings, the results of this study support further initiatives to develop and implement programs for HIV-positive jail detainees.
References
Glynn M, Rhodes P. Estimated HIV prevalence in the United States at the end of 2003 [Abstract No. T1-B1101]. National HIV Prevention Conference. Atlanta, GA, June 12–15, 2005.
Fleming P, Byers R, Sweeney P, Karon J, Janssen RS. HIV prevalence in the United States, 2000. Programs and Abstracts of the 9th Conference on Retroviruses and Opportunistic Infections. Seattle, Washington: Abstract 11; February 24–28, 2002.
Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4(11):e7558.
Maruschak L. HIV in prisons, 2006. US Department of Justice, Bureau of Justice Statistics. NCJ-222179.
Visher C, LaVigne N, Travis J. Returning home: understanding the challenges of prisoner reentry. Maryland Pilot Study: findings from Baltimore: Urban Institute, Justice Policy Center; January 2004. JPC Publication CPR04 0122.
Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: imprisonment among the homeless and marginally housed population. Am J Public Health. 2005;95(10):1747–1752.
Cooke CL. Going home: formerly incarcerated African American men return to families and communities. J Fam Nurs. 2005;11(4):388–404.
Courtenay-Quirk C, Pals SL, Kidder DP, Henny K, Emshoff JG. Factors associated with incarceration history among HIV-positive persons experiencing homelessness or imminent risk of homelessness. J Community Health. 2008;33(6):434–443.
Cooke CL. Joblessness and homelessness as precursors of health problems in formerly incarcerated African American men. J Nurs Scholarsh. 2004;36(2):155–160.
Stephenson BL, Wohl DA, McKaig R, et al. Sexual behaviours of HIV-seropositive men and women following release from prison. Int J STD AIDS. 2006;17(2):103–108.
MacGowan RJ, Margolis A, Gaiter J, et al. Predictors of risky sex of young men after release from prison. Int J STD AIDS. 2003;14(8):519–523.
van Olphen J, Eliason MJ, Freudenberg N, Barnes M. Nowhere to go: how stigma limits the options of female drug users after release from jail. Subst Abuse Treat Prev Policy. 2009;4:10.
Clements-Nolle K, Marx R, Pendo M, Loughran E, Estes M, Katz M. Highly active antiretroviral therapy use and HIV transmission risk behaviors among individuals who are HIV infected and were recently released from jail. Am J Public Health. 2008;98(4):661–666.
Stephenson BL, Wohl DA, Golin CE, Tien HC, Stewart P, Kaplan AH. Effect of release from prison and re-incarceration on the viral loads of HIV-infected individuals. Public Health Rep. 2005;120(1):84–88.
Small W, Wood E, Betteridge G, Montaner J, Kerr T. The impact of incarceration upon adherence to HIV treatment among HIV-positive injection drug users: a qualitative study. AIDS Care. 2009;21(6):708–714.
Friedman MS, Marshal MP, Stall R, et al. Associations between substance use, sexual risk taking and HIV treatment adherence among homeless people living with HIV. AIDS Care. 2009;21(6):692–700.
Royal SW, Kidder DP, Patrabansh S, et al. Factors associated with adherence to highly active antiretroviral therapy in homeless or unstably housed adults living with HIV. AIDS Care. 2009;21(4):448–455.
James D. Profile of jail inmates, 2002 US Department of Justice, Office of Justice Programs. Bureau of Justice Statistics, Special Report July 2004 NCJ 201932.
Freudenberg N. Jails, prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78(2):214–235.
Vlahov D, Putnam S. From corrections to communities as an HIV priority. J Urban Health. 2006;83(3):339–348.
Jacob Arriola KR, Braithwaite RL, Holmes E, Fortenberry RM. Post-release case management services and health-seeking behavior among HIV-infected ex-offenders. J Health Care Poor Underserved. 2007;18(3):665–674.
Zaller ND, Holmes L, Dyl AC, et al. Linkage to treatment and supportive services among HIV-positive ex-offenders in Project Bridge. J Health Care Poor Underserved. 2008;19(2):522–531.
Health Resources and Services Administration, US Department of Health and Human Services. The HIV/AIDS Bureau: Special Projects of National Significance (SPNS) Enhancing Linkages to Primary Care and Services in Jail Settings Demonstration Models. Announcement Number: HRSA-07-031. Available at https://grants.hrsa.gov/webExternal/DisplayAttachment.asp?ID=0553C8C6-91DE-4C09-9D5D-1B1BF572F8D7.
Spaulding A, Arriola K, Ramos K. Enhancelink: linking HIV infected jail detainees to care. American Correctional Health Services Association, Southeast Regional 2008 Professional Development Conference. Chattanooga, TN; September 19–21, 2008. Available at http://enhancelink.org/sites/hivjailstudy/ACHSA_fall_08_918.pdf.
Fontana L, Beckerman A. Recently released with HIV/AIDS: primary care treatment needs and experiences. J Health Care Poor Underserved. 2007;18(3):699–714.
Merriam SB. Qualitative research and case study applications in education. 2nd ed. San Francisco: Jossey-Bass; 1998.
Weiss RS. Learning from strangers: the art and method of qualitative interview studies. New York: Free Press; Toronto: Maxwell Macmillan Canada; Maxwell Macmillan International; 1994.
Maxwell JA. Qualitative research design: an interactive approach. 2nd ed. Thousand Oaks: Sage; 2005.
Seidman I. Interviewing as qualitative research: a guide for researchers in education and the social sciences. 3rd ed. New York: Teachers College Press; 2006.
Rich JD, Holmes L, Salas C, et al. Successful linkage of medical care and community services for HIV-positive offenders being released from prison. J Urban Health. 2001;78(2):279–289.
Desai AA, Latta ET, Spaulding A, Rich JD, Flanigan TP. The importance of routine HIV testing in the incarcerated population: the Rhode Island experience. AIDS Educ Prev. 2002;14(5 Suppl B):45–52.
Beckwith CG, Poshkus M, Chowdury S, et al. Routine jail-based HIV testing in Rhode Island, 2000-2007 [Presentation CCT4B-1]. 2009 National HIV Prevention Conference. Atlanta, GA, August 23-26, 2009.
CDC. Coinfection with HIV and hepatitis C virus. Atlanta: CDC; 2010.
Roux P, Carrieri MP, Villes V, et al. The impact of methadone or buprenorphine treatment and ongoing injection on highly active antiretroviral therapy (HAART) adherence: evidence from the MANIF2000 cohort study. Addiction. 2008;103(11):1828–1836.
Kapadia F, Vlahov D, Wu Y, et al. Impact of drug abuse treatment modalities on adherence to ART/HAART among a cohort of HIV seropositive women. Am J Drug Alcohol Abuse. 2008;34(2):161–170.
Greifinger R. Thirty years since Estelle v. Gamble. In: Greifinger R, ed. Public health behind bars: from prisons to communities. New York: Springer International; 2007.
Bruce RD. Methadone as HIV prevention: high volume methadone sites to decrease HIV incidence rates in resource limited settings. Int J Drug Policy. 2010;21(2):122–124.
Sullivan LE, Metzger DS, Fudala PJ, Fiellin DA. Decreasing international HIV transmission: the role of expanding access to opioid agonist therapies for injection drug users. Addiction. 2005;100(2):150–158.
Sullivan LE, Moore BA, Chawarski MC, et al. Buprenorphine/naloxone treatment in primary care is associated with decreased human immunodeficiency virus risk behaviors. J Subst Abuse Treat. 2008;35(1):87–92.
James D, Glaze L. Mental health problems of prison and jail inmates. US Department of Justice, Bureau of Justice Statistics. September 2006:NCJ 213600. Accessed at http://bjs.ojp.usdoj.gov/content/pub/pdf/mhppji.pdf.
Baillargeon JG, Paar DP, Wu H, et al. Psychiatric disorders, HIV infection and HIV/hepatitis co-infection in the correctional setting. AIDS Care. 2008;20(1):124–129.
Des Jarlais DC, Braine N, Friedmann P. Unstable housing as a factor for increased injection risk behavior at US syringe exchange programs. AIDS Behav. 2007;11(6 Suppl):78–84.
Shah NG, Galai N, Celentano DD, Vlahov D, Strathdee SA. Longitudinal predictors of injection cessation and subsequent relapse among a cohort of injection drug users in Baltimore, MD, 1988–2000. Drug Alcohol Depend. 2006;83(2):147–156.
Buchanan D, Kee R, Sadowski LS, Garcia D. The health impact of supportive housing for HIV-positive homeless patients: a randomized controlled trial. Am J Public Health. 2009;99(Suppl 3):S675–S680.
Acknowledgements
This manuscript was supported by the Special Projects of National Significance of the Health Resources and Services Administration (grant H97HA08535), and the Lifespan/Tufts/Brown Center for AIDS Research (grant P30AI42853). In addition, A. Nunn received support from the NIDA grant 5T32DA013911, NIAAA grant 1K01AA020228-01A1, and a Rhode Island Foundation Medical Research Grant. C. Beckwith received support from NIDA grant K23DA021095 and L. Bazerman received support from the Tufts Nutrition Collaborative, A Center for Drug Abuse, and AIDS Research (grant P30DA013868). None of the aforementioned agencies had any role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nunn, A., Cornwall, A., Fu, J. et al. Linking HIV-positive Jail Inmates to Treatment, Care, and Social Services After Release: Results from a Qualitative Assessment of the COMPASS Program. J Urban Health 87, 954–968 (2010). https://doi.org/10.1007/s11524-010-9496-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-010-9496-7