Abstract
We applied our previously developed estimation equation to predict EQ-5D index scores from the Centers for Disease Control and Prevention’s Healthy Days measures for the New York City (NYC) adult population from 1995 to 2006 and compared these trends over time with the US general population. Such scores enabled us to examine the burden of disease attributable to smoking and overweight/obesity at both the local and national levels. We employed the estimation equation to the 1993–2007 Behavioral Risk Factor Surveillance System (BRFSS) data to obtain EQ-5D index scores for all survey respondents based on their age, self-rated health status, and overall number of unhealthy days. With the combination of mortality data, we calculated trends of quality-adjusted life years (QALYs), life expectancy (LE), and quality-adjusted life expectancy (QALE) as well as the percent of QALYs and QALE lost contributed by smoking and overweight/obesity. Mean EQ-5D index scores for NYC adults decreased from 0.874 to 0.852 but, more recently, have increased to 0.869. The LE of an 18-year-old living in NYC increased 4.7 years and QALE increased 2.6 years. The contribution of smoking to the proportion of QALYs lost decreased from 6.7% to 3.5%, while the contribution of overweight/obesity to the proportion of QALYs lost increased from 4.5% to 16.9%. The proportion of QALEs lost due to smoking decreased from 5.5% to 4.5%, while the proportion of QALEs lost due to overweight/obesity increased from 3.5% to 11.8%. Because the Healthy Days measures have been included in the BRFSS since 1993, translating Healthy Days Measures to a preference-based measure is a useful method for longitudinal tracking of population health at the local, state, and national level.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In order to set priorities for prevention in a given population and document progress over time, policy makers should be able to measure and track health-related quality of life (HRQOL) and the resultant burden of disease due to determinants that strongly impact population health outcomes at the national, state, and local (community) levels. Given that many interventions are implemented at the state and local levels, decision makers need tools that allow them to examine the mean (overall) health for the general population as well as make comparisons according to the region(s) where a given policy has been implemented.1 However, although measures of HRQOL may be useful in tracking changes in burden of disease, these measures have been administered on a cross-sectional basis in the USA and cannot examine trends over time.
In terms of trend data, since 1993, the Centers for Disease Control and Prevention (CDC) has incorporated the Healthy Days measures as part of the annual Behavioral Risk Factor Surveillance System (BRFSS).2 , 3 These measures define HRQOL as “perceived physical and mental health over time” and ask respondents about their recent number of poor health days. The BRFSS was designed to provide reliable state-level estimates and estimates for some sub-state areas or detailed annual and monthly estimates for large geographic areas.2 – 4 However, Healthy Days measures are not preference-based (utility) measures of morbidity, thereby preventing quality-adjusted life years (QALYs) to be calculated and burden of disease and cost-effectiveness analyses to be conducted.5 To solve this problem, we previously developed an estimation equation of EQ-5D scores from the Healthy Days measures to generate utility scores.6 , 7 Because of the availability of multiple years of data contained in the BRFSS and lack of longitudinal data that contain utilities, additional analyses would provide data at the local level and over time for the use in burden of disease and cost-effectiveness studies.
In the USA, two behavioral risk factors, smoking and overweight/obesity, have the greatest impact on both morbidity and mortality, contributing to more than one third of premature deaths.8 , 9 In an effort to increase both the quality and years of healthy life, public health practitioners, policy makers, and clinicians have targeted both risk behaviors by implementing various interventions at multiple levels.10 , 11 Although the prevalence of tobacco use has declined, and, more recently, stabilized,12 , 13 the prevalence of overweight/obesity has continued to rise over time.14 – 16
At the local level, New York City has embarked on policy-based and health care initiatives aimed to decrease the prevalence of tobacco use and promote a healthy diet and physical activity. However, to date, the tobacco initiative has been associated with declines in the prevalence of smoking, while the prevalence of obesity continues to increase.17 – 19 Viewing data from the New York City Community Health Survey (CHS), which is based on the BRFSS, between 2002 and 2006, a 19% decline in the prevalence of smoking was observed among NYC adults, from 21.5% to 17.5%, respectively.19 By contrast, CHS data indicated that the prevalence of obesity increased 17% in New York City, from 19.5% in 2002 to 22.8% in 2004 compared with a 6% increase in the prevalence of obesity nationally during the same time period.20
Although prevalence data are available for smoking and overweight/obesity, such data fail to provide information on the HRQOL and resultant burden of disease experienced by individuals in terms of lost health. In this study, we will (1) examine the HRQOL for a representative sample of New York City adults and compare this with the US adult general population over the period from 1994 to 2007; (2) examine QALYs, life expectancy (LE), and quality-adjusted life expectancy (QALE) both for NYC adults and the general US population from 1995 to 2006; and (3) determine the percentage of QALYs and QALE lost attributed to smoking and overweight/obesity. We provide this information as a model of the way that the BRFSS can generate QALYs and QALE with which to longitudinally track the burden of disease at various population levels.
Methods
Data and Measurements
Data were from the 1993–2007 BRFSS, an ongoing state-based survey of representative samples of non-institutionalized civilian adult residents from each of the 50 states and the District of Columbia.3 , 21 The BRFSS began with a set of questions, the Healthy Days measures, that asked respondents about their self-rated general health and number of physically unhealthy days, mentally unhealthy days, and activity limitation days. The overall unhealthy days was calculated by adding physically and mentally unhealthy days, with a logical maximum of 30 unhealthy days.4
We constructed EQ-5D scores from the Healthy Days measures.7 The EQ-5D comprises a descriptive system and a visual analog scale (EQ VAS) intended to assess health today. The descriptive system enables respondents to classify their health on one of three levels according to five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), thereby generating 243 unique health states. The data may be used to represent a profile of health status or converted into a single summary index (EQ-5D index) by applying scores from a valuation set.22 Health state values range from the most severe impairment on all five dimensions (value = −0.109) to no problems on any dimension (value = 1.0). Our algorithm predicts respondents’ EQ-5D index scores based on their number of overall unhealthy days, self-rated health status, and age. For example, the estimated EQ-5D index is 0.841 for a 30-year-old person who reports three overall unhealthy days and “good” self-rated health (Appendix). Our previous manuscript estimated the validity of estimates by ecological analyses of mean scores in different population subgroups and by simulations.7 Our validations demonstrated that the algorithm can provide an accurate estimation of mean EQ-5D scores in a number of population subgroups that differ with regard to age, race/ethnicity, gender, education, body mass index (BMI), self-rated health, activity limitation, and selected chronic diseases.
Detailed mortality data (by age and gender in 1-year intervals) for NYC and for the USA were used to construct life tables for the calculation of life expectancy and quality adjusted life expectancy. Data are compiled by the CDC and available for the public at http://wonder.cdc.gov. Life tables were constructed using a hypothetical cohort of 100,000 individuals exposed to a risk of death over each year interval starting at age 18. For instance, if the risk of death between age 18 and 19 is 0.00086, then 86 persons will die over this interval, leaving 100,000 − 86 = 99,914 persons to be exposed to the risk of death in the next age interval (age 19–20).
Analyses
We applied the estimation equation to the 1993–2007 BRFSS data to obtain EQ-5D index scores for all NYC survey respondents based on their age, self-rated health status, and overall number of unhealthy days. We obtained QALYs with 1995–2006 estimates using a 3-year moving average. New York City mortality data from 1994 to 2005 were used to estimate LE and QALE contributed by smoking and overweight/obesity. We then compared these scores with the US general population.
The total QALYs were defined as the product of utility score and population.23 , 24 The QALYs lost contributed by a risk factor is calculated as:
where \(x_{ij}^0 \) and \(x_{ij}^k \) are the average EQ-5D scores of the reference group and for the kth level of the risk factor, respectively, for age i and gender j, and \(p_{ij}^k \) is the proportion of the population in the same demographic subgroup and risk factor category k. Using the impact of obesity as an example, \(x_{ij}^0 \) is the average EQ-5D score of those with normal weight (i.e., BMI 18.5–24.9 kg/m2), and \(x_{ij}^k \) is the average EQ-5D score at each category of BMI. The proportion of explainable QALYs lost contributed from the risk factor is:
Let A i be the number surviving to age i and B i be the life years between age i and i + 1. The life expectancy at age i is the ratio of total life years above age i and the number of population surviving to age i or \(LE_i = \sum\limits_{j \geq i} {{{B_j } \mathord{\left/ {\vphantom {{B_j } {A_i }}} \right. \kern-\nulldelimiterspace} {A_i }}} \).25 The quality-adjusted life years between age i and i + 1 is B i x i and the QALE at age i is \( QALE = {\sum\limits_{j \geqslant i} {{B_{j} x_{j} } \mathord{\left/ {\vphantom {{B_{j} x_{j} } {A_{i} }}} \right. \kern-\nulldelimiterspace} {A_{i} }} } \).26 , 27 Similar to the QALYs lost, the QALE lost contributing to a risk factor is
and the proportion of explainable QALE lost contributing to the factor is
Results
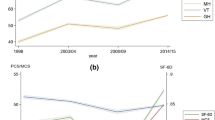
Figure 1 illustrates mean EQ-5D index scores over time for both NYC adults and the general US population. Mean EQ-5D index scores for NYC adults decreased from 0.874 (1994) to 0.852 (2003) but, more recently, have increased to 0.869 (2006). For the US general population, mean EQ-5D index scores decreased, from 0.883 in 1994 to 0.866 in 2006, but unlike scores for persons living in NYC, mean scores did not show a recent “rebound effect.”
Although mean EQ-5D index scores declined, Fig. 2 illustrates that LE and QALE increased both for the NYC and general US population, with gains being greater for adults in NYC. In particular, the LE of an 18-year-old living in NYC increased 4.7 years from 56.8 (1995) to 61.5 (2004) and QALE increased 2.6 years from 49.0 to 51.6 over this same time period. For the general US population, the LE of an 18-year-old increased 1.8 years from 58.6 (1995) to 60.4 (2004) and QALE increased 0.7 years from 50.9 to 51.6.
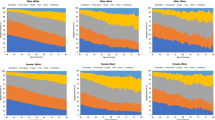
Mean EQ-5D scores varied in an expected manner according to category of BMI (with scores decreasing from normal weight to overweight to obese) and smoking status (with scores decreasing from never smoker to quit smoking to current smoker; data not shown). Figure 3 illustrates the percentage of QALYs attributable to smoking and overweight/obesity over time among adults living in NYC and the general US population. For adults living in NYC, the contribution of smoking to the proportion of QALYs lost decreased from 6.7% (1995) to 3.5% (2006), or 48%, while the contribution of overweight/obesity to the proportion of QALYs lost increased from 4.5% (1995) to 16.9% (2006), or more than 275%. By contrast, for the general US population, the contribution of smoking to the proportion of QALYs lost remained stable over time (6.7% in 1995 and 7.1% in 2006), while similar to the pattern seen for NYC, the contribution of overweight/obesity to the proportion of QALYs lost increased over time, from 8.7% (1995) to 13.1% (2006), or an approximately 51% increase. For NYC adults, the proportion of QALEs lost attributed to smoking decreased 19% [i.e., from 5.5% (1995) to 4.5% (2004)], while the proportion of QALEs lost due to overweight/obesity increased from 3.5% (1995) to 11.8% (2004), representing a 236% increase. By contrast, for the general US population, the proportion of QALEs lost due to smoking increased by 27%, and although the proportion of QALEs lost due to obesity also increased, the increase was only by 60% [from 7.3% (1995) to 11.6% (2004)] (Fig. 4).
Discussion
Although the two overarching goals of Healthy People are to increase the quality and years of healthy life and eliminate health disparities, Healthy People 2010 did not delineate a mechanism to quantify the degree that progress has been made toward these goals.1 , 10 Our method would enable specified determinants of health to be examined in a manner amenable to conducting burden of disease and cost-effectiveness analyses (i.e., through an examination of QALYs, LE, and QALE) at multiple levels. This tool follows in the tradition of the Years of Healthy Life measure that was developed for Healthy People 200028 and can fulfill that promise at the local and state levels as well as the national level.
Although burden of disease and cost-effectiveness studies have been conducted with increasing frequency in the USA, such analyses have tended to be cross-sectional, or, when longitudinal, comprised a clinical cohort rather than a population group. Use of the BRFSS enabled us to examine the time trends for the general population and at the local level (New York City) with regard to improving the quality and years of healthy life as well as making comparisons at the national and local levels for two potentially modifiable behavioral risk factors (smoking and overweight/obesity). Because of the availability of trend data that will continue to provide detailed annual and monthly estimates and is able to be modified at the statewide and county level, the BRFSS can measure the progress toward Healthy People at the national, state, and local levels and allow the impact of interventions to be examined at the relevant level in a timely manner.3
Our study indicated similarities and differences between trends over time for the general US population and New York City that might not have been apparent if only cross-sectional data had been obtained a decade apart. For example, overall mean EQ-5D scores decreased from 1995 to 2006 for both groups, but although mean EQ-5D scores for NYC adults initially decreased, more recently, mean scores have increased. Although attribution to any particular public health intervention is difficult, we note that a decline also was observed in nonspecific psychological distress among adults living in New York City between 2002 and 2003.29 In addition, beginning in 2002, the New York City health department began a series of initiatives to address chronic disease prevention and control and help New Yorkers live longer and healthier lives.18 , 30
The overall worsening trends in HRQOL were observed in all major subpopulations (i.e., age, race/ethnicity, gender; data not shown). Although mean differences in EQ-5D index scores over time were not of a magnitude generally considered to be clinically important for indiviudals,31 , 32 such differences might be important for monitoring population health, especially among certain population subgroups. Despite mean EQ-5D scores decreasing over time, however, life expectancy and quality-adjusted life expectancy increased for the general US population and NYC adults.
This pattern of HRQOL declining over time is consistent with findings from other investigators in the USA and abroad.33 – 36 Understanding the deterioration of HRQOL in light of increasing life expectancy is crucial, given the aging of the population and the overarching goals of Healthy People.10 A number of explanations have been provided for these findings, including an increased prevalence of obesity, increases in non-fatal conditions, and technological advances in medicine that offer lifesaving treatments for persons in poor health.34 , 35 Regarding obesity, the prevalence of overweight or obesity, as assessed in the BRFSS, increased by 29% (i.e., from 48.7% in 1993 to 62.8% in 2007). Additionally, the mean age of the BRFSS sample increased from 43.7 in 1993 to 46.1 in 2007, and such a change would be expected to contribute to the trend of worsened HRQOL.
This study has a number of limitations. With regard to the application of the estimation equation, detailed mortality data only were available through 2005. We were unable to calculate LE and QALE for 2006 or beyond, and because we used a 3-year moving average for NYC, we only have LE/QALE data through 2004. However, since the BRFSS data are released to users in a timely manner, this lag in data still may compare with other surveys that tend to take longer to release data. In addition, given the smaller sample size of the BRFSS for NYC in earlier years, particularly between 1994 and 1996, estimates in these years may be unreliable. However, the BRFSS sample size for NYC is larger than other national data sets. Of note, 2002 estimates also should be interpreted with caution. During this year, 29 states in the BRFSS did not ask all of the Healthy Days questions and had to be excluded from the analysis, thereby potentially producing unmeasured differences in HRQOL, and the Healthy Days measures were moved from the beginning to the end of the BRFSS, thereby leading to a possible order effect.
Other limitations include that this analysis relies on the validity of the EQ-5D estimates from the Healthy Days measures. However, we previously demonstrated that mean scores of the estimated EQ-5D index matched well to the true mean scores; therefore, the estimated QALY and QALE should have acceptable accuracy.6 Furthermore, our calculation of QALY and QALE did not account for the loss to premature death resulting from each modifiable factor due to the lack of data on excess death from each risk factor. However, data from a previous study23 showed that the QALYs lost due to both morbidity and mortality were only 17.6% more than the QALYs lost due to morbidity alone for those below poverty level. Therefore, we do not expect that adding QALY lost due to mortality will change our results significantly, particularly when our results were in proportions.
Because the Healthy Days measures have been included in the BRFSS since 1993, translating Healthy Days Measures to a preference-based measure might be particularly useful as a stop gap method when examining trends over time and the impact of interventions on such trends. Comparisons could be made at multiple levels in order to assess the particular area that was impacted by a given intervention. In addition, different (and more local) interventions might be compared with one another with regard to the impact on those given populations/regions. This is particularly important, as the prevalence of risk factors tends to change over time (i.e., both increasing and decreasing) in different geographic areas and the effect of an intervention might be immediate (and either transient or sustained) or delayed. However, for the long term, the CDC should consider adding an existing validated instrument such as the EQ-5D that has had widespread use in clinical settings and increasing use in measuring population health.
References
Kindig DA, Asada Y, Booske B. A population health framework for setting national and state health goals. JAMA. 2008;299(17):2081–3. doi:10.1001/jama.299.17.2081.
Moriarty DG, Zack MM, Kobau R. The Centers for Diseases Control and Prevention’s Healthy Days Measures—population tracking of perceived physical and mental health over time. Health Qual Life Outcomes. 2003;1:37. doi:10.1186/1477-7525-1-37.
Mokdad AH, Stroup DF, Giles WH, Behavioral Risk Factor Surveillance Team. Public health surveillance for behavioral risk factors in a changing environment. Recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recomm Rep.. 2003;52(RR-9):1–12.
CDC. Measuring Healthy Days: population assessment of health-related quality of life. US Department of Health and Human Services. Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion. Division of Adult and Community Health; 2000.
Gold MR, Siegel JE, Russell LB, Weinstein MC, eds. Cost-effectiveness in Health and Medicine. New York: Oxford University Press; 1996.
Jia H, Lubetkin EI, Moriarty DG, Zack MM. A comparison of Healthy Days and EuroQol EQ-5D measures in two US adult samples. Appl Res Qual Life. 2007;2:209–21. doi:10.1007/s11482-008-9039-5.
Jia H, Lubetkin EI. Estimating EuroQol EQ-5D scores from population Healthy Days data. Med Decis Making. 2008;28(4):491–9. doi:10.1177/0272989X07312708.
Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–45. doi:10.1001/jama.291.10.1238.
Sturm R, Wells KB. Does obesity contribute as much to morbidity as poverty or smoking? Public Health. 2001;115(3):229–35. doi:10.1016/S0033-3506(01)00449-8.
US Department of Health and Human Services. Healthy People 2010. 2nd ed. With understanding and improving health and objectives for improving health (2 vols). Washington, DC: US Government Printing Office; 2000.
McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Aff (Millwood). 2002;21(2):78–93. doi:10.1377/hlthaff.21.2.78.
Centers for Disease Control and Prevention (CDC). Tobacco use—United States, 1900–1999. MMWR Morb Mortal Wkly Rep.. 1999;48(43):986–93.
Frieden TR, Mostashari F, Kerker BD, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. Am J Public Health. 2005;95(6):1016–23. doi:10.2105/AJPH.2004.058164.
Centers for Disease Control and Prevention (CDC). State-specific prevalence of obesity among adults—United States, 2007. MMWR Morb Mortal Wkly Rep.. 2008;57(28):765–8.
Kuczmarski RJ, Flegal KM, Campbell SM, Johnson CL. Increasing prevalence of overweight among US adults. The National Health and Nutrition Examination Surveys, 1960 to 1991. JAMA. 272(3):205–211.
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–55. doi:10.1001/jama.295.13.1549.
Centers for Disease Control and Prevention (CDC). Cigarette smoking among adults—United States, 2006. MMWR Morb Mortal Wkly Rep.. 2007;56(44):1157–61.
Frieden TR, Bassett MT, Thorpe LE, Farley TA. Public health in New York City, 2002–2007: confronting epidemics of the modern era. Int J Epidemiol. 2008;37(5):966–77. doi:10.1093/ije/dyn108.
Centers for Disease Control and Prevention (CDC). Decline in smoking prevalence—New York City, 2002–2006. MMWR Morb Mortal Wkly Rep.. 2007;56(24):604–8.
Van Wye G, Kerker BD, Matte T, et al. Obesity and diabetes in New York City, 2002 and 2004. Prev Chronic Dis. 2008;5(2):A48.
Frazier EL, Franks AL, Sanderson LM, Using behavioral risk factor surveillance data. In: Using chronic disease data: a handbook for public health practitioners. Atlanta GA: Centers for Disease Control and Prevention, 1992:4.1–4.17.
Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: development and testing of the D1 valuation model. Med Care. 2005;43(3):203–20. doi:10.1097/00005650-200503000-00003.
Muennig P, Franks P, Jia H, Lubetkin E, Gold MR. The income-associated burden of disease in the United States. Soc Sci Med. 2005;61(9):2018–26. doi:10.1016/j.socscimed.2005.04.005.
Muennig P, Lubetkin E, Jia H, Franks P. Gender and the burden of disease attributable to obesity. Am J Public Health. 2006;96(9):1662–8. doi:10.2105/AJPH.2005.068874.
Anderson RN. Method for constructing complete annual U.S. life tables. National Center for Health Statistics. Vital Health Stat 2. 1999;(129).
Brønnum-Hansen H, Juel K, Davidsen M, Sørensen J. Impact of selected risk factors on quality-adjusted life expectancy in Denmark. Scand J Public Health. 2007;35(5):510–5. doi:10.1080/14034940701271908.
Rosenberg MA, Fryback DG, Lawrence WF. Computing population-based estimates of health-adjusted life expectancy. Med Decis Making. 1999;19(1):90–7. doi:10.1177/0272989X9901900111.
Public Health Service. Healthy People 2000: National Health Promotion and Disease Prevention Objectives and Full Report, with Commentary. Washington, DC: US Department of Health and Human Services, Public Health Service, 1991; DHHS publication no. (PHS) 91-50212.
McVeigh KH, Galea S, Thorpe LE, Maulsby C, Henning K, Sederer LI. The epidemiology of nonspecific psychological distress in New York City, 2002 and 2003. J Urban Health. 2006;83(3):394–405. doi:10.1007/s11524-006-9049-2.
Roth D, Cohen L, Frieden TR. Take Care New York: Third Year Progress Report. New York City Department of Health and Mental Hygiene; 2007
Sullivan PW, Lawrence WF, Ghushchyan V. A national catalog of preference-based scores for chronic conditions in the United States. Med Care. 2005;43(7):736–49. doi:10.1097/01.mlr.0000172050.67085.4f.
Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res.. 2005;14(6):1523–32. doi:10.1007/s11136-004-7713-0.
Zack MM, Moriarty DG, Stroup DF, Ford ES, Mokdad AH. Worsening trends in adult health-related quality of life and self-rated health-United States, 1993–2001. Public Health Rep.. 2004;119(5):493–505. doi:10.1016/j.phr.2004.07.007.
Martin LG, Schoeni RF, Freedman VA, Andreski P. Feeling better? Trends in general health status. J Gerontol B Psychol Sci Soc Sci.. 2007;62(1):S11–S21.
Lakdawalla DN, Bhattacharya J, Goldman DP. Are the young becoming more disabled? Health Aff (Millwood). 2004;23(1):168–76. doi:10.1377/hlthaff.23.1.168.
Burström K, Johannesson M, Rehnberg C. Deteriorating health status in Stockholm 1998–2002: results from repeated population surveys using the EQ-5D. Qual Life Res. 2007;16(9):1547–53. doi:10.1007/s11136-007-9243-z.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Healthy Days | Excellent self rated general health | Very good self-rated general health | Good self-rated general health | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
18–24 | 25–44 | 45–64 | 65–74 | 75+ | 18–24 | 25–44 | 45–64 | 65–74 | 75+ | 18–24 | 25–44 | 45–64 | 65–74 | 75+ | |
30 | 1.000 | 1.000 | 1.000 | 0.999 | 0.999 | 1.000 | 1.000 | 0.998 | 0.990 | 0.894 | 1.000 | 0.994 | 0.891 | 0.864 | 0.843 |
29 | 1.000 | 0.999 | 0.996 | 0.856 | 0.835 | 1.000 | 0.991 | 0.867 | 0.852 | 0.829 | 0.999 | 0.855 | 0.851 | 0.829 | 0.817 |
28 | 1.000 | 0.994 | 0.870 | 0.845 | 0.832 | 1.000 | 0.979 | 0.858 | 0.845 | 0.823 | 0.889 | 0.848 | 0.840 | 0.819 | 0.809 |
27 | 1.000 | 0.990 | 0.860 | 0.838 | 0.828 | 0.999 | 0.852 | 0.842 | 0.838 | 0.817 | 0.877 | 0.841 | 0.832 | 0.813 | 0.799 |
26 | 0.999 | 0.857 | 0.851 | 0.832 | 0.825 | 0.999 | 0.848 | 0.835 | 0.831 | 0.812 | 0.869 | 0.835 | 0.826 | 0.808 | 0.792 |
25 | 0.999 | 0.854 | 0.843 | 0.824 | 0.815 | 0.881 | 0.843 | 0.829 | 0.821 | 0.806 | 0.863 | 0.828 | 0.820 | 0.803 | 0.785 |
24 | 0.999 | 0.852 | 0.836 | 0.818 | 0.809 | 0.875 | 0.837 | 0.825 | 0.816 | 0.801 | 0.857 | 0.822 | 0.815 | 0.797 | 0.780 |
23 | 0.882 | 0.850 | 0.832 | 0.813 | 0.804 | 0.870 | 0.834 | 0.821 | 0.812 | 0.795 | 0.852 | 0.817 | 0.810 | 0.790 | 0.776 |
22 | 0.877 | 0.847 | 0.829 | 0.809 | 0.797 | 0.865 | 0.830 | 0.817 | 0.808 | 0.788 | 0.847 | 0.811 | 0.806 | 0.782 | 0.768 |
21 | 0.875 | 0.846 | 0.828 | 0.807 | 0.794 | 0.863 | 0.829 | 0.815 | 0.806 | 0.786 | 0.844 | 0.808 | 0.803 | 0.778 | 0.766 |
20 | 0.871 | 0.841 | 0.825 | 0.803 | 0.786 | 0.859 | 0.826 | 0.810 | 0.803 | 0.783 | 0.841 | 0.803 | 0.799 | 0.766 | 0.751 |
19 | 0.867 | 0.835 | 0.823 | 0.798 | 0.779 | 0.856 | 0.822 | 0.806 | 0.798 | 0.747 | 0.840 | 0.798 | 0.795 | 0.759 | 0.741 |
18 | 0.866 | 0.834 | 0.822 | 0.797 | 0.779 | 0.854 | 0.821 | 0.804 | 0.796 | 0.746 | 0.838 | 0.796 | 0.793 | 0.757 | 0.740 |
17 | 0.865 | 0.833 | 0.821 | 0.796 | 0.778 | 0.852 | 0.820 | 0.803 | 0.794 | 0.745 | 0.836 | 0.794 | 0.791 | 0.753 | 0.739 |
16 | 0.862 | 0.831 | 0.820 | 0.790 | 0.775 | 0.849 | 0.818 | 0.801 | 0.783 | 0.742 | 0.834 | 0.790 | 0.788 | 0.745 | 0.731 |
15 | 0.858 | 0.828 | 0.812 | 0.770 | 0.746 | 0.843 | 0.810 | 0.796 | 0.768 | 0.737 | 0.827 | 0.780 | 0.778 | 0.729 | 0.718 |
14 | 0.855 | 0.825 | 0.805 | 0.766 | 0.738 | 0.837 | 0.803 | 0.792 | 0.761 | 0.733 | 0.821 | 0.772 | 0.748 | 0.723 | 0.713 |
13 | 0.853 | 0.824 | 0.804 | 0.765 | 0.737 | 0.835 | 0.801 | 0.790 | 0.759 | 0.732 | 0.819 | 0.769 | 0.745 | 0.722 | 0.712 |
12 | 0.851 | 0.824 | 0.802 | 0.765 | 0.736 | 0.833 | 0.800 | 0.787 | 0.756 | 0.731 | 0.816 | 0.767 | 0.743 | 0.720 | 0.711 |
11 | 0.849 | 0.823 | 0.802 | 0.764 | 0.735 | 0.831 | 0.799 | 0.785 | 0.753 | 0.731 | 0.815 | 0.765 | 0.741 | 0.719 | 0.711 |
10 | 0.841 | 0.821 | 0.800 | 0.763 | 0.729 | 0.828 | 0.796 | 0.779 | 0.730 | 0.724 | 0.809 | 0.759 | 0.737 | 0.711 | 0.708 |
9 | 0.835 | 0.814 | 0.797 | 0.758 | 0.724 | 0.824 | 0.792 | 0.771 | 0.723 | 0.716 | 0.802 | 0.745 | 0.732 | 0.704 | 0.640 |
8 | 0.833 | 0.810 | 0.796 | 0.750 | 0.721 | 0.821 | 0.789 | 0.768 | 0.719 | 0.713 | 0.798 | 0.730 | 0.721 | 0.702 | 0.636 |
7 | 0.832 | 0.809 | 0.795 | 0.748 | 0.720 | 0.817 | 0.788 | 0.765 | 0.718 | 0.712 | 0.794 | 0.728 | 0.717 | 0.702 | 0.636 |
6 | 0.831 | 0.808 | 0.795 | 0.746 | 0.720 | 0.814 | 0.787 | 0.764 | 0.717 | 0.712 | 0.793 | 0.727 | 0.714 | 0.701 | 0.633 |
5 | 0.829 | 0.806 | 0.793 | 0.742 | 0.718 | 0.810 | 0.783 | 0.761 | 0.713 | 0.709 | 0.789 | 0.724 | 0.710 | 0.699 | 0.628 |
4 | 0.827 | 0.804 | 0.791 | 0.737 | 0.715 | 0.808 | 0.778 | 0.757 | 0.708 | 0.707 | 0.785 | 0.720 | 0.706 | 0.696 | 0.624 |
3 | 0.825 | 0.804 | 0.790 | 0.736 | 0.714 | 0.806 | 0.774 | 0.755 | 0.707 | 0.705 | 0.782 | 0.718 | 0.704 | 0.695 | 0.623 |
2 | 0.822 | 0.802 | 0.787 | 0.723 | 0.668 | 0.804 | 0.754 | 0.749 | 0.706 | 0.665 | 0.775 | 0.701 | 0.694 | 0.644 | 0.621 |
1 | 0.815 | 0.800 | 0.781 | 0.718 | 0.659 | 0.801 | 0.745 | 0.719 | 0.703 | 0.649 | 0.759 | 0.697 | 0.690 | 0.616 | 0.614 |
0 | 0.690 | 0.634 | 0.629 | 0.586 | 0.533 | 0.644 | 0.603 | 0.538 | 0.526 | 0.507 | 0.548 | 0.504 | 0.492 | 0.484 | 0.461 |
Healthy Days | Fair self-rated general health | Poor self-rated general health |
| ||||||||||||
18–24 | 25–44 | 45–64 | 65–74 | 75+ | 18–24 | 25–44 | 45–64 | 65–74 | 75+ | ||||||
30 | 0.999 | 0.981 | 0.867 | 0.852 | 0.834 | 0.904 | 0.857 | 0.851 | 0.849 | 0.828 | |||||
29 | 0.889 | 0.846 | 0.836 | 0.823 | 0.807 | 0.879 | 0.830 | 0.829 | 0.818 | 0.798 | |||||
28 | 0.884 | 0.838 | 0.829 | 0.818 | 0.798 | 0.871 | 0.826 | 0.823 | 0.813 | 0.794 | |||||
27 | 0.876 | 0.829 | 0.820 | 0.810 | 0.789 | 0.865 | 0.820 | 0.816 | 0.807 | 0.789 | |||||
26 | 0.867 | 0.820 | 0.814 | 0.805 | 0.786 | 0.859 | 0.815 | 0.811 | 0.802 | 0.783 | |||||
25 | 0.857 | 0.812 | 0.807 | 0.799 | 0.780 | 0.853 | 0.810 | 0.803 | 0.795 | 0.776 | |||||
24 | 0.853 | 0.806 | 0.801 | 0.793 | 0.776 | 0.848 | 0.805 | 0.799 | 0.782 | 0.769 | |||||
23 | 0.849 | 0.801 | 0.796 | 0.783 | 0.772 | 0.843 | 0.800 | 0.794 | 0.760 | 0.755 | |||||
22 | 0.844 | 0.797 | 0.789 | 0.772 | 0.753 | 0.837 | 0.791 | 0.787 | 0.749 | 0.732 | |||||
21 | 0.842 | 0.794 | 0.785 | 0.770 | 0.750 | 0.834 | 0.786 | 0.781 | 0.748 | 0.728 | |||||
20 | 0.840 | 0.787 | 0.779 | 0.760 | 0.745 | 0.830 | 0.771 | 0.762 | 0.744 | 0.722 | |||||
19 | 0.836 | 0.773 | 0.768 | 0.751 | 0.732 | 0.825 | 0.763 | 0.752 | 0.740 | 0.718 | |||||
18 | 0.834 | 0.771 | 0.756 | 0.749 | 0.729 | 0.823 | 0.760 | 0.750 | 0.739 | 0.717 | |||||
17 | 0.832 | 0.769 | 0.751 | 0.747 | 0.726 | 0.821 | 0.756 | 0.749 | 0.738 | 0.716 | |||||
16 | 0.829 | 0.765 | 0.747 | 0.736 | 0.723 | 0.814 | 0.750 | 0.745 | 0.735 | 0.714 | |||||
15 | 0.822 | 0.754 | 0.739 | 0.727 | 0.714 | 0.802 | 0.738 | 0.731 | 0.725 | 0.708 | |||||
14 | 0.815 | 0.734 | 0.721 | 0.715 | 0.707 | 0.792 | 0.732 | 0.716 | 0.713 | 0.702 | |||||
13 | 0.810 | 0.732 | 0.716 | 0.710 | 0.706 | 0.784 | 0.731 | 0.712 | 0.709 | 0.701 | |||||
12 | 0.806 | 0.731 | 0.713 | 0.706 | 0.702 | 0.754 | 0.729 | 0.708 | 0.701 | 0.700 | |||||
11 | 0.804 | 0.729 | 0.710 | 0.705 | 0.666 | 0.748 | 0.728 | 0.705 | 0.699 | 0.654 | |||||
10 | 0.798 | 0.724 | 0.705 | 0.698 | 0.645 | 0.737 | 0.721 | 0.699 | 0.694 | 0.640 | |||||
9 | 0.790 | 0.715 | 0.697 | 0.688 | 0.638 | 0.720 | 0.706 | 0.690 | 0.676 | 0.632 | |||||
8 | 0.783 | 0.699 | 0.692 | 0.652 | 0.635 | 0.704 | 0.684 | 0.681 | 0.629 | 0.616 | |||||
7 | 0.763 | 0.681 | 0.668 | 0.644 | 0.634 | 0.684 | 0.643 | 0.629 | 0.628 | 0.612 | |||||
6 | 0.753 | 0.675 | 0.640 | 0.635 | 0.621 | 0.637 | 0.637 | 0.627 | 0.609 | 0.603 | |||||
5 | 0.742 | 0.632 | 0.628 | 0.620 | 0.599 | 0.627 | 0.624 | 0.603 | 0.593 | 0.571 | |||||
4 | 0.732 | 0.629 | 0.619 | 0.613 | 0.580 | 0.619 | 0.619 | 0.596 | 0.558 | 0.556 | |||||
3 | 0.726 | 0.628 | 0.616 | 0.612 | 0.569 | 0.618 | 0.617 | 0.594 | 0.554 | 0.548 | |||||
2 | 0.715 | 0.626 | 0.611 | 0.610 | 0.548 | 0.615 | 0.610 | 0.589 | 0.550 | 0.531 | |||||
1 | 0.703 | 0.621 | 0.604 | 0.571 | 0.516 | 0.605 | 0.568 | 0.550 | 0.546 | 0.511 | |||||
0 | 0.487 | 0.443 | 0.434 | 0.431 | 0.416 | 0.475 | 0.431 | 0.386 | 0.350 | 0.325 | |||||
Rights and permissions
About this article
Cite this article
Lubetkin, E.I., Jia, H. Health-Related Quality of Life, Quality-Adjusted Life Years, and Quality-Adjusted Life Expectancy in New York City from 1995 to 2006. J Urban Health 86, 551–561 (2009). https://doi.org/10.1007/s11524-009-9344-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-009-9344-9