Abstract
Most studies of socioeconomic status (SES) and chronic disease risk factors have been conducted in high-income countries, and most show inverse social gradients. Few studies examine these patterns in lower- or middle-income countries. Using cross-sectional data from a 2005 national risk factor survey in Argentina (a middle-income country), we investigated the associations of individual- and area-level SES with chronic disease risk factors (body mass index [BMI], hypertension, and diabetes) among residents of Buenos Aires. Associations of risk factors with income and education were estimated after adjusting for age, sex (except in sex-stratified models), and the other socioeconomic indicators. BMI and obesity were inversely associated with education and income for women, but not for men (e.g., mean differences in BMI for lowest versus highest education level were 1.55 kg/m2, 95%CI = 0.72–2.37 in women and 0.17 kg/m2, 95%CI = −0.72–1.06 in men). Low education and income were also associated with increased odds of hypertension diagnosis in all adults (adjusted odds ratio [AOR] = 1.48, 95%CI = 0.99–2.20 and AOR = 1.50, 95%CI = 0.99–2.26 for the lowest compared to the highest education and income categories, respectively). Lower education was strongly associated with increased odds of diabetes diagnosis (AOR = 4.12, 95%CI = 1.85–9.18 and AOR = 2.43, 95%CI = 1.14–5.20 for the lowest and middle education categories compared to highest, respectively). Area-level education also showed an inverse relationship with BMI and obesity; these results did not vary by sex as they did at the individual level. This cross-sectional study of a major urban area provides some insight into the global transition with a trend toward concentrations of risk factors in poorer populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Globally, chronic diseases are the primary cause of mortality, and their significance relative to injuries and communicable diseases is projected to increase over the next two decades.1,2 While chronic diseases are traditionally thought to be more important in developed than in developing countries, the majority of the increase in these diseases globally is occurring in developing countries.3 In fact, cardiovascular disease already causes more deaths than any other disease in developing countries.4
Although economic development is associated with some improvements in health outcomes, economic growth and industrialization are also major contributors to the increase of chronic disease risk factors. Risk is changing due to increased availability of tobacco products, saturated fat, and sugars; changes in the way food is produced and distributed; and decreased physical activity at work and home.1,5,6 Urbanization, which is often closely linked to economic growth and industrialization, also plays a key role in these processes. By 2008, more than half of the world’s population will live in urban areas; by 2030, 80% of the urban population will live in developing countries. A large proportion of this urban population growth will be due to growth in the urban poor.7
Urbanization may affect human health through conditions in which people live, where they work, the food they eat, and the environmental factors to which they are exposed.8 However, these effects may not be similar for all social groups. While those in urban settings who are better off financially may be able to change their levels of risk factors (e.g., tobacco, excess calories from saturated fats and sugars), the poor may find it difficult to live healthy lives in urban areas.8 Documenting the social patterning of chronic disease risk factors is important for understanding the causes of increases in developing countries and for targeting specific populations for the most effective interventions. While socioeconomic inequalities in chronic diseases and their risk factors have been studied extensively in high-income countries,9 very few studies have investigated social inequalities in chronic disease risk factors in low- or middle-income countries. We used data from a recent population-based survey to investigate the social patterning of chronic disease risk factors in one large Latin American city: Buenos Aires, Argentina.
Methods
In 2005, the Argentine government conducted a National Survey of Risk Factors for Non-communicable Diseases to determine the prevalence of chronic disease risk factors among adults 18 years and older. The study consisted of a four-stage probabilistic sample design with agglomerations of at least 5,000 inhabitants sampled at the first stage, censal radios (with an average of 300 housing units) or clusters of censal radios sampled at the second stage, housing units sampled at the third stage, and an individual 18 years or older randomly sampled from all households within each housing unit at the fourth stage. The sample represents 96% of adults living in urban areas (with at least 5,000 inhabitants). Nationally, the effective response rate of the sampled households was 89.6%. The analyses reported in this study are for the city of Buenos Aires where the effective household response rate was 79.3%. The city of Buenos Aires is at the core of the largest metropolitan area in the country. In the 2001 census, the city of Buenos Aires had 2.8 million residents and the metropolitan area had more than 11 million residents.10 A total of 1,510 residents in the city of Buenos Aires participated in the survey. Surveys were completed by trained interviewers who visited sampled households at varying times of the day.
Participants responded to a questionnaire concerning their height, weight, high blood pressure status, diabetes status, diet, physical activity, and smoking history. Questionnaire items were modeled or adapted from standard surveys such as the Behavioral Risk Factor Surveillance System.11 Height and weight were self-reported by participants and were used to calculate body mass index (BMI; weight divided by height squared; in kilograms per meter squared). Participants were classified as obese if they had a BMI ≥ 30 kg/m2. Participants were classified as having high blood pressure or diabetes if they reported they had ever been diagnosed with these conditions by a health professional. Diet was measured using a question on frequency of fruit and vegetable intake: “How many days in the last week, in your house or outside of your house, did you eat or drink …fruit (not including fruit juice)? …vegetables?” Participants were categorized as having high intake of fruits and vegetables if they reported eating fruits and vegetables at least 5 days/week. The amount of fruits and vegetables consumed on each of those days was not assessed. Physical activity was assessed using a standardized questionnaire: “In the last week, how many days did you participate in intense physical activity/moderate physical activity/walking, lasting at least 10 min”? and “Time of intense physical activity/moderate physical activity/walking in minutes.” Based on responses, physical activity was categorized into three levels: intense (participants who engaged in at least 3 days/week of intense physical activity [defined as activity resulting in much faster breathing and major physical exertion] for a total of at least 1,500 metabolic equivalent (MET)-minutes per week or 7 days of any combination of exercise for at least 3,000 MET-minutes per week); moderate (at least 3 days/week of intense activity for 20 min/day or at least 5 days of moderate activity [defined as activity resulting in faster breathing and some physical exertion] or walking for at least 30 min/day or at least 5 days of any combination yielding at least 600 MET-minutes per week); and low otherwise. A MET is defined as the caloric consumption of a person while at complete rest (1 kcal/kg/h). The physical activity questions did not distinguish leisure-time activity from other kinds of activities. Current smoking status was reported by participants in response to the question: “At the moment, do you smoke cigarettes every day/some days/you don’t smoke.” Each of the seven chronic disease risk factors (BMI, obesity, high blood pressure diagnosis, diabetes diagnosis, high fruit and vegetable intake, low physical activity level, and current smoking status) was examined separately.
The socioeconomic variables examined included education, income, and area-based socioeconomic measures. Participants self-reported their education levels in response to the question “Level of education—no education/primary incomplete/primary complete/secondary incomplete/secondary complete/tertiary or university incomplete/tertiary or university complete or more/special education” and were classified as having incomplete secondary education (<12 years), complete secondary education/incomplete tertiary (12–13 years), or complete tertiary/university education (14 years or more). Monthly household income in pesos was reported in response to the question: “Range of total monthly household income in pesos—no income, 1–100, 101–200, …, 1,001–1,250, 1,251–1,500, …, 2,001–3,000, …, 5,001 and more” and categorized according to approximate tertiles with an additional category for unknown income. Area socioeconomic position was defined based on the participant’s censal fraction of residence. Censal fractions were defined by the Argentine National Institute of Statistics and Censuses and included an average of approximately 3,600 residents. We used the percentage of residents per censal fraction with incomplete secondary education as the key area-level socioeconomic measure.
Analyses
After descriptive and bivariate analyses, we ran running multivariable linear and logistic regression models for the seven chronic disease risk factors to determine their social patterning at the individual level. All of these models were adjusted for age and sex and were mutually adjusted for individual education and household monthly income. We tested interaction terms for sex with education and with income for each outcome and presented stratified analyses when the interaction terms were statistically significant based on a 0.05 level of significance. We used five-level categories for education and income when calculating the Spearman correlation and P values for interaction terms and tests for trend in order to maximize power. However, the additional categories did not add any qualitative advantage to the three-level categories, and so we kept only three levels for the relevant figures and tables for simplicity.
Generalized estimating equations12 were used to account for the clustering at the censal fraction level when conducting the area-level analyses with censal fraction education levels as the predictor of interest. Survey weights were used to account for the complex sampling design in all analyses.
Results
Of the 284 censal fractions in Buenos Aires, 155 were represented in the survey. The total sample size was 615 men and 895 women. The mean number of participants per censal fraction was 9.74 with a median of 9 people and an interquartile range (25th–75th percentiles) of 7–10. When compared to the 129 censal fractions not sampled, the 155 censal fractions were similar in terms of characteristics such as the percentage of female residents, the proportion of people without health care coverage, the proportion of people with incomplete secondary education, and the proportion of households with two or more people per room (results not shown).
Table 1 displays selected individual characteristics of the sample, stratified by sex. The mean ages of the respondents were 45.5 years for men and 49.6 years for women. The majority of the respondents had at least a secondary school education (71% men, 68% women). Men reported higher household monthly incomes than women (35% of men reported incomes more than 1,750 pesos per month compared to 25% of women). Income and education were positively although not highly correlated (Spearman correlation between the two five-level categorizations=0.48). The percentage of obese respondents was 10% for women and 12% for men. Both men and women reported being diagnosed with high blood pressure (30% and 31%, respectively) more often than diabetes (12% and 7%, respectively). A higher percentage of women than men reported eating fruit and vegetables at least 5 days/week (45% women, 27% men). Physical activity levels were similar for men and women with most people (56%) having moderate or low levels. The percentage of people who had ever smoked was 55% for women and 71% for men, but 26% of women and 31% of men said they were current smokers. Men and women resided in censal fractions with an average of 37.9% and 38.3% of residents with incomplete secondary school education, respectively.
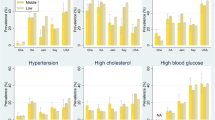
Figure 1 shows age-adjusted prevalences or mean levels of selected risk factors by socioeconomic status (SES), weighted to account for sampling design. BMI was inversely associated with income and education in women but not in men. Reported diagnoses of high blood pressure and diabetes generally tended to decrease with increasing education and income. The prevalence of eating fruits and vegetables five times a week increased with increasing education and income for both men and women. In general, socioeconomic gradients in high blood pressure, diabetes, and diet were more consistent and were more likely to be statistically significant or approach statistical significance in women than in men. Weaker and less consistent patterns were observed for physical activity or smoking: the prevalence of current smoking decreased slightly with increasing education and income in men but not in women and the prevalence of low physical activity tended to increase with increasing education and income for both sexes. However, none of the trends were statistically significant.
Table 2 shows the odds ratios (OR) of hypertension, diabetes, eating fruits and vegetables at least 5 days/week, low physical activity, and current smoking by education and income adjusted for each other in addition to age and sex. There was no evidence that the associations differed significantly by sex (P for multiplicative interaction > 0.05), so pooled results adjusted for sex are shown. Low income and education were associated with increased odds of hypertension in a graded fashion although the trend was not statistically significant at the 0.05 level for education (OR = 1.48, 95%CI = 0.99–2.20 and OR = 1.50, 95%CI = 0.99–2.26 for the lowest compared to the highest education and income categories, respectively). Lower education was strongly associated with increased odds of diabetes in a graded fashion (OR = 4.12, 95%CI = 1.85–9.18 and OR = 2.43, 95%CI = 1.14–5.20 for the lowest and middle education categories compared to the highest, respectively). The odds of eating fruits and vegetables 5 days/week was positively associated with income (OR = 0.58, 95%CI = 0.39–0.84 for the lowest category compared to the highest category). Physical activity was not patterned by income or education. There was some evidence of increased odds of smoking in the lowest educational categories, although this difference was not statistically significant (OR = 1.26, 95%CI = 0.85–1.85 for lowest versus highest category).
Table 3 displays adjusted mean differences in BMI and OR of obesity by education and income, stratified by sex. Sex-stratified results are shown because there was evidence of significant heterogeneity of the effects of education and income on BMI by sex (P for additive interaction 0.0235 for sex and education and 0.0252 for sex and income). For women, BMI increased with decreasing levels of education and household income. BMI shows no clear trend for men by education or income. A similar pattern was observed when a dichotomous obesity was examined: the odds of obesity increased with decreasing income and education in a graded fashion in women, but no clear patterns were observed in men.
Figure 2 displays the age-adjusted mean BMI by sex for the different levels of censal fraction education. Mean BMI tended to increase as the percentage of residents with incomplete secondary education increase. Associations of censal fraction education with the risk factors after adjusting for age, sex, education, and income are shown in Table 4. There was no evidence that high blood pressure, diabetes, fruit and vegetable intake, physical activity, or smoking was associated with area characteristics after accounting for individual-level income and education. However, living in an area with a higher percentage of residents with incomplete secondary school was significantly associated with greater mean BMI and greater odds of obesity with no evidence that these associations differed by sex.
Discussion
This study offers insight into the social patterning of chronic disease risk factors in a major Latin American city. We found evidence that BMI and obesity are inversely associated with education and income in women but not men. In addition, among all adults, having a high blood pressure diagnosis was inversely associated with income and education (although trends by education were not statistically significant) and having a diabetes diagnosis was inversely associated with education. The diabetes results were particularly striking: adults who had complete secondary education but incomplete tertiary or university education had more than two times the odds of reporting a diabetes diagnosis when compared to those with complete tertiary or university education, and those with less than a secondary school education had more than four times the odds of reporting a diabetes diagnosis when compared to the same group. Considering that, in many countries (including Latin America), people of lower socioeconomic status may be less likely to have access to a medical professional13–15 to diagnose either high blood pressure or diabetes, it is likely that the associations between low social position and higher odds of diabetes and hypertension are underestimated. In contrast to results for BMI, high blood pressure, and diabetes, the behavioral risk factors of diet, physical activity, and smoking were not consistently patterned by education or income, except for a positive association of fruit and vegetable intake with income.
Most studies of socioeconomic status and chronic disease risk factors have been conducted in high-income economies, and most show inverse social gradients.9 However, evidence suggests that the social patterning may vary depending on the social and economic context of the country. In lower-income countries, higher levels of socioeconomic resources may be associated with lifestyle characteristics conducive to higher levels of chronic disease risk factors. However, a reversal of this social gradient may occur over time as those of higher social classes recognize that their lifestyles are not conducive to a healthy life and have the resources to change their behaviors and potentially their environments.16–18
A limited number of studies have investigated social gradients in chronic disease risk factors in developing countries. Most work has focused on BMI and obesity. A recent review of the socioeconomic patterning of obesity19 reported that, for women, stronger inverse associations between BMI and indicators of education, occupation, income, or material resources emerged as country-level development increased. In men, results were more mixed: associations of socioeconomic factors were often not statistically significant and were sometimes curvilinear.19 Likewise, a cross-national study of obesity among women from 27 developing countries found that SES, measured by education, was positively associated with obesity in low-income economies, but negatively associated with obesity in upper- to middle-income developing countries.20 A recent review on SES and obesity in developing countries supports these findings, noting that, as economies develop, obesity becomes more prominent among lower SES groups with this shift occurring earlier for women than men.21 Our findings are consistent with prior work: we found an inverse social gradient in BMI and obesity for women, but not for men, using both education and income. These results would be expected given that Argentina is a middle-income country, and urban areas are often the first to undergo these transitions to inverse social gradients. The reasons for the stronger social patterning in women than in men (which has been consistently reported also in developed countries19) remain to be determined.
Studies investigating the social patterning of hypertension and diabetes have reported both positive and inverse associations with socioeconomic position. For example, hypertension and diabetes have been found to be both inversely and positively associated with socioeconomic factors in countries of Asia and Africa.22–30 In Latin America and the Caribbean, hypertension was inversely associated with SES in a major city in Chile31 and systolic blood pressure was inversely associated with income and education in Trinidad and Tobago.32 However, in other areas, the association depended on gender. Studies in urban areas of Cuba and Peru found that hypertension was inversely associated with socioeconomic factors in women, but positively associated with socioeconomic factors in men.33,34 Diabetes was inversely associated with socioeconomic factors in urban Bolivia,35 Peru,34 and Mexico.36 In a study of elderly in seven cities in Latin America and the Caribbean, diabetes mellitus was inversely associated with education in Buenos Aires and Montevideo, but showed no patterning in Bridgetown, São Paulo, Santiago, Havana, or Mexico City.37 Diabetes also showed no association with SES in Valparaiso, Chile.31
We found inverse associations of income and education with hypertension and of education with diabetes in a large urban area in Argentina. These results suggest that the social patterning of hypertension and diabetes may vary substantially across developing countries by level of development and level of urbanization. However, given the emerging associations between BMI and social position as countries develop and the fact that BMI is a strong risk factor for both diabetes and hypertension, it is to be expected that strong inverse social gradients in diabetes and hypertension are likely to emerge, especially in women.
With the exception of smoking, few studies have examined the social patterning of health behaviors in developing countries. Like hypertension and diabetes, the social patterning of smoking is not invariant. Both inverse and positive associations of socioeconomic factors with smoking have been reported in countries of Asia and Africa.23,24,27,38 The direction of the association between smoking and SES depended on urban/rural status among older adults in Mexico, exhibiting a positive association with income in urban areas but a negative association with wealth in less-urban areas.39 In a Chilean city, current smoking was not associated with SES, but being sedentary in leisure time was inversely associated with SES.31 A recent study in Rio de Janeiro found that a composite measure of cardiovascular disease risk (based on BMI, fat location, smoking, hypertension, sedentary lifestyle, and alcohol consumption) was inversely associated with education in men and women and with income in men.40
We found some evidence of a positive association between income and eating fruit and vegetables, but no evidence of strong social gradients in physical activity or smoking in the city of Buenos Aires. Behaviors such as diet and physical activity are notoriously difficult to measure and the questions available to asses these behaviors were very limited. Physical activity, for example, includes both occupational and leisure-time activity (which likely vary by gender), and fruit and vegetable intake is measured by days consumed rather than the amounts consumed on each of those days. Detailed assessment of physical activity and diet was not available in this survey. This could have affected our ability to detect stronger or more consistent social patterning of these behaviors. We did detect some social patterning of diet, and it is plausible that, in developing countries, low socioeconomic position is still associated with greater occupational physical activity, resulting in no gradient in physical activity. Our questionnaire did not allow us to distinguish between these different types of activity. On the other hand, it is possible that, in developing countries, behaviors such as being sedentary and smoking are still as common in the higher as in the lower socioeconomic groups for a variety of social and cultural reasons. For example, price may be a deterrent to smoking among low SES groups in some developing countries, although transnational tobacco companies are increasing marketing and availability to larger sections of the population.1,5 It is plausible that inverse gradients will emerge over time as they have in other countries.9
Despite the limitations of the self-reported measures, the outcomes of physician-diagnosed diabetes and hypertension and self-reported BMI may be better markers of the cumulative effects of a variety of difficult-to-measure behaviors and exposures that are patterned by SES, hence the stronger associations of SES with these factors that we observed in our data. The fact that hypertension and diabetes were inversely associated with socioeconomic position in both genders despite the absence of BMI differences in men suggests that BMI is not the only factor driving these differences.
We also found that lower area-level education was associated with higher BMI after controlling for individual-level education and income. Area-level was correlated with other area-level measures, such as inadequate housing and percentage of the population with unmet basic needs, and was used as a proxy for a variety of socioeconomic conditions. Although area effects have received much attention in industrialized countries,41,42 they have been rarely investigated in nonindustrialized countries. One multilevel study in rural China found inverse associations of community socioeconomic characteristics with smoking, waist-to-hip ratio, systolic blood pressure and BMI.43 Our results for BMI are consistent with those reported in China, but we did not find area-level effects for other risk factors. Interestingly, area effects were present for both women and men despite the absence of social gradients in BMI in men at the individual level. It has been argued that a variety of area features including access to walkable environments, healthy foods, and sources of chronic stress could contribute to area differences in BMI.44,45 It is plausible that limitations in our measures of physical activity and diet make it difficult to detect area effects on these behaviors. Moreover, the extent of which area characteristics relevant to health behaviors covary with area SES in developing countries requires further research.
A limitation of our analyses is the use of self-reported measures of risk factors which undoubtedly introduced measurement error. For instance, the assessment of diabetes and hypertension was based on self-reports; height and weight were also self-reported possibly resulting in misclassification.46–51 Nevertheless, many population surveys, including surveys in high-income countries such as the Behavioral Risk Factor Surveillance System11 in the US, rely on self-reported measures for the surveillance of risk factors. In addition, these data from a large urban area may not be generalizable to less-urban or rural areas. The cross-sectional nature of our analyses obviously does not allow us to examine trends over time in the social patterning of risk factors. Limitations in the measures used also do not allow us to draw firm conclusions regarding the relative importance of income and education. Also, we did not assess the impact of other individual and area socioeconomic variables, such as occupation, wealth, and area-level poverty, which may also yield important insights into the burden of these risk factors by social factors.
Our study adds to the paucity of data on the individual and area-level social patterning of chronic disease risk in developing countries. We found that BMI was clearly inversely associated with SES in women and that diabetes and hypertension were inversely associated with SES in women than in men. In addition, lower area-level education was associated with higher BMI in both genders. Stronger inverse social patterning is likely to emerge over time in urban areas like the one we investigated. The presence of these inequalities needs to be considered by policy makers and public health workers both in terms of understanding the causes of chronic diseases and designing appropriate interventions.
References
Yach D, Hawkes C, Gould CL, Hofman KJ. The global burden of chronic diseases—overcoming impediments to prevention and control. JAMA. 2004;291(21):2616–2622 doi:10.1001/jama.291.21.2616.
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442 doi:10.1371/journal.pmed.0030442.
Murray CJL, Lopez AD, Harvard School of Public Health, World Health Organization, World Bank. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Cambridge, MA: Published by the Harvard School of Public Health on behalf of the World Health Organization and the World Bank; Distributed by Harvard University Press; 1996.
World Health Organization. The world health report 2003: shaping the future. Geneva: World Health Organization; 2003.
Beaglehole R, Yach D. Globalisation and the prevention and control of non-communicable disease: the neglected chronic diseases of adults. Lancet. 2003;362(9387):903–908 doi:10.1016/S0140-6736(03)14335-8.
World Health Organization. The world health report 2002: reducing risks, promoting healthy life. Geneva: World Health Organization; 2002.
Greenhalgh S, Montgomery M, Segal SJ, Todaro MP, UN Population Fund. State of world population 2007: unleashing the potential of urban growth. Popul Dev Rev. 2007;33(3):639–640.
Phillips DR. Urbanization and Human Health. Parasitology. 1993;106:S93–S107.
Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4):1973–1998.
Censo Nacional de Población. Hogares y Viviendas del año 2001. http://www.indec.gov.ar/webcenso/index.asp. Accessed January 8, 2008.
Behavioral Risk Factor Surveillance System. http://www.cdc.gov/brfss/. Accessed August 18, 2008.
Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22 doi:10.1093/biomet/73.1.13.
Dachs JN, Ferrer M, Florez CE, Barros AJ, Narvaez R, Valdivia M. Inequalities in health in Latin America and the Caribbean: descriptive and exploratory results for self-reported health problems and health care in twelve countries. Rev Panam Salud Publica. 2002;11(5–6):335–355.
Noronha KV, Andrade MV. Social inequality in health and the utilization of health services among the elderly in Latin America. Rev Panam Salud Publica. 2005;17(5–6):410–418 doi:10.1590/S1020-49892005000500013.
Wallace SP, Gutierrez VF. Equity of access to health care for older adults in four major Latin American cities. Rev Panam Salud Publica. 2005;17(5–6):394–409 doi:10.1590/S1020-49892005000500012.
Leeder S, Raymond S, Greenberg H, Liu H, Esson K. A race against time: the challenge of cardiovascular disease in developing economies. New York City, NY: Columbia University; 2004.
Reddy KS. Emerging epidemic of cardiovascular disease in the developing countries. Atherosclerosis. 1999;144:143–143.
Singh RB, Pella D, Mechirova V, et al. Prevalence of obesity, physical inactivity and undernutrition, a triple burden of diseases during transition in a developing economy. The Five City Study Group. Acta Cardiol. 2007;62(2):119–127 doi:10.2143/AC.62.2.2020231.
McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:29–48 doi:10.1093/epirev/mxm001.
Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. Int J Obes Relat Metab Disord. 2004;28(9):1181–1186 doi:10.1038/sj.ijo.0802716.
Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ. 2004;82(12):940–946.
Lang T, Pariente P, Salem G, Tap D. Social, professional conditions and arterial hypertension: an epidemiological study in Dakar, Senegal. J Hypertens. 1988;6(4):271–276 doi:10.1097/00004872-198804000-00002.
Pappas G, Akhtar T, Gergen PJ, Hadden WC, Khan AQ. Health status of the Pakistani population: a health profile and comparison with the United States. Am J Public Health. 2001;91(1):93–98.
Singh RB, Sharma JP, Rastogi V, et al. Social class and coronary disease in rural population of north India. The Indian Social Class and Heart Survey. Eur Heart J. 1997;18(4):588–595.
Singh RB, Niaz MA, Thakur AS, Janus ED, Moshiri M. Social class and coronary artery disease in a urban population of North India in the Indian Lifestyle and Heart Study. Int J Cardiol. 1998;64(2):195–203 doi:10.1016/S0167-5273(98)00048-5.
Singh RB, Beegom R, Mehta AS, et al. Social class, coronary risk factors and undernutrition, a double burden of diseases, in women during transition, in five Indian cities. Int J Cardiol. 1999;69(2):139–147 doi:10.1016/S0167-5273(99)00010-8.
Hoang VM, Byass P, Dao LH, Nguyen TK, Wall S. Risk factors for chronic disease among rural Vietnamese adults and the association of these factors with sociodemographic variables: findings from the WHO STEPS survey in rural Vietnam, 2005. Prev Chronic Dis. 2007;4(2):A22.
Schooling CM, Jiang CQ, Lam TH, Zhang WS, Cheng KK, Leung GM. Life-course origins of social inequalities in metabolic risk in the population of a developing country. Am J Epidemiol. 2008;167(4):419–428 doi:10.1093/aje/kwm329.
abu Sayeed M, Ali L, Hussain MZ, Rumi MA, Banu A, Azad Khan AK. Effect of socioeconomic risk factors on the difference in prevalence of diabetes between rural and urban populations in Bangladesh. Diabetes Care. 1997;20(4):551–555 doi:10.2337/diacare.20.4.551.
Singh RB, Singh V, Kulshrestha SK, et al. Social class and all-cause mortality in an urban population of North India. Acta Cardiol. 2005;60(6):611–617 doi:10.2143/AC.60.6.2004933.
Vega J, Jadue L, Escobar MC, et al. Prevalence of hypertension in Valparaiso. Results of the base survey of the CARMEN project (Set of measures for the multifactorial reduction of non-transmissible diseases). Rev Med Chile. 1999;127(6):729–738.
Gulliford MC, Mahabir D, Rocke B. Socioeconomic inequality in blood pressure and its determinants: cross-sectional data from Trinidad and Tobago. J Hum Hypertens. 2004;18(1):61–70 doi:10.1038/sj.jhh.1001638.
Ordunez P, Munoz JL, Espinosa-Brito A, Silva LC, Cooper RS. Ethnicity, education, and blood pressure in Cuba. Am J Epidemiol. 2005;162(1):49–56 doi:10.1093/aje/kwi163.
Goldstein J, Jacoby E, del Aguila R, Lopez A. Poverty is a predictor of non-communicable disease among adults in Peruvian cities. Prev Med. 2005;41(3–4):800–806 doi:10.1016/j.ypmed.2005.06.001.
Barcelo A, Daroca MC, Ribera R, Duarte E, Zapata A, Vohra M. Diabetes in Bolivia. Rev Panam Salud Publica. 2001;10(5):318–323.
Posadas-Romero C, Yamamoto-Kimura L, Lerman-Garber I, et al. The prevalence of NIDDM and associated coronary risk factors in Mexico City. Diabetes Care. 1994;17(12):1441–1448 doi:10.2337/diacare.17.12.1441.
Barcelo A, Pelaez M, Rodriguez-Wong L, Pastor-Valero M. The prevalence of diagnosed diabetes among the elderly of seven cities in Latin America and the Caribbean: the Health Wellbeing and Aging (SABE) Project. J Aging Health. 2006;18(2):224–239 doi:10.1177/0898264305285728.
Pampel F. Tobacco use in sub-Sahara Africa: estimates from the demographic health surveys. Soc Sci Med. 2008;66(8):1772–1783 doi:10.1016/j.socscimed.2007.12.003.
Smith KV, Goldman N. Socioeconomic differences in health among older adults in Mexico. Soc Sci Med. 2007;65(7):1372–1385 doi:10.1016/j.socscimed.2007.05.023.
Marins VM, Almeida RM, Pereira RA, Sichieri R. The association between socioeconomic indicators and cardiovascular disease risk factors in Rio de Janeiro, Brazil. J Biosoc Sci. 2007;39(2):221–229.
Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003;80(4):569–589 doi:10.1093/jurban/jtg065.
Stafford M, Cummins S, Ellaway A, Sacker A, Wiggins RD, Macintyre S. Pathways to obesity: identifying local, modifiable determinants of physical activity and diet. Soc Sci Med. 2007;65(9):1882–1897 doi:10.1016/j.socscimed.2007.05.042.
Le C, Chongsuvivatwong V, Geater A. Contextual socioeconomic determinants of cardiovascular risk factors in rural south-west China: a multilevel analysis. BMC Public Health. 2007;7:72 doi:10.1186/1471-2458-7-72.
Booth KM, Pinkston MM, Poston WS. Obesity and the built environment. J Am Diet Assoc. 2005;105(5 Suppl 1):S110–S117 doi:10.1016/j.jada.2005.02.045.
Ellen IG, Mijanovich T, Dillman KN. Neighborhood effects on health: exploring the links and assessing the evidence. J Urban Aff. 2001;23(3–4):391–408 doi:10.1111/0735-2166.00096.
Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101(1):28–34 (quiz 35–26) doi:10.1016/S0002-8223(01)00008-6.
Gillum RF, Sempos CT. Ethnic variation in validity of classification of overweight and obesity using self-reported weight and height in American women and men: the Third National Health and Nutrition Examination Survey. Nutr J. 2005;4:27 doi:10.1186/1475-2891-4-27.
Bostrom G, Diderichsen F. Socioeconomic differentials in misclassification of height, weight and body mass index based on questionnaire data. Int J Epidemiol. 1997;26(4):860–866 doi:10.1093/ije/26.4.860.
LeJarraga H, Laspuir M, Adamo P. Validity of reported parental height in outpatient growth clinics in Buenos Aires city. Ann Hum Biol. 1995;22(2):163–166 doi:10.1080/03014469500003812.
Avila-Funes JA, Gutierrez-Robledo LM, Ponce De Leon Rosales S. Validity of height and weight self-report in Mexican adults: results from the national health and aging study. J Nutr Health Aging. 2004;8(5):355–361.
Schmidt MI, Duncan BB, Tavares M, Polanczyk CA, Pellanda L, Zimmer PM. Validity of self-reported weight—a study of urban Brazilian adults. Rev Saude Publica. 1993;27(4):271–276 doi:10.1590/S0034-89101993000400007.
Acknowledgement
This work was supported by RO3 TW007020 from the Fogarty Institute and the National Institutes of Health (Diez Roux PI).
Author information
Authors and Affiliations
Corresponding author
Additional information
Fleischer and Diez Roux are with the Center for Social Epidemiology and Population Health, Department of Epidemiology, University of Michigan, Ann Arbor, MI, USA; Alazraqui and Spinelli are with the National University of Lanus, Buenos Aires, Argentina.
Rights and permissions
About this article
Cite this article
Fleischer, N.L., Diez Roux, A.V., Alazraqui, M. et al. Social Patterning of Chronic Disease Risk Factors in a Latin American City. J Urban Health 85, 923–937 (2008). https://doi.org/10.1007/s11524-008-9319-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-008-9319-2