Abstract
Tumorigenic rearrangements in anaplastic lymphoma kinase (ALK) account for 3–7% of all non-small cell lung cancers (NSCLC). Treatment with targeted tyrosine kinase inhibitors (TKIs) has shown impressive clinical responses. Crizotinib was the first agent approved for front-line therapy of ALK-rearranged NSCLC after it demonstrated superiority to chemotherapy in response rate, duration of response, and progression-free survival. However, eventually all patients progress on crizotinib therapy, with the central nervous system (CNS) being the most common site, which served as the impetus for the development of more potent next-generation ALK inhibitors. Currently, ceritinib, alectinib, and brigatinib are all approved for second-line therapy after progression on or intolerance to crizotinib. Investigations into whether the initiation of a second-generation ALK inhibitor as first-line therapy is the superior treatment paradigm has resulted in the approval of ceritinib as initial therapy. Alectinib has also shown impressive results as front-line therapy, as recently reported in two large randomized studies that compared it to crizotinib. There is a significant need to better understand the drivers of and mechanisms underlying resistance to ALK inhibitors. While specific mutations have been identified, there is currently only limited evidence that the identification of specific mutations should impact selection of the next ALK inhibitor. The best treatment option for patients who become TKI refractory is also unclear, though there is some evidence to suggests that these patients are not responsive to checkpoint inhibitors and may respond better to chemotherapy. Combination therapy with other classes of agents may help to overcome resistance mechanisms and should be investigated further.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Advances in genetic sequencing have revealed that non-small cell lung cancer (NSCLC), previously thought of as a homogenous disease, is actually comprised of multiple genetically distinct entities. This is especially true in adenocarcinoma, where multiple oncogenic ‘driver’ mutations have been identified. These mutations lead to downstream activation of canonical growth pathways, ultimately resulting in tumorigenesis. The use of targeted inhibitors has revolutionized the therapy for advanced NSCLC that harbor these mutations.
ALK (anaplastic lymphoma kinase) rearrangements are the driver mutation in 3–7% of NSCLC [1] with EML4 (echinoderm microtubule-associated protein-like 4) as the most common fusion partner. Soda et al. were the first to demonstrate that EML4-ALK fusion was a distinct oncogenic event in a subset of NSCLC [2]. The fusion proteins lead to constitutive activity of the ALK tyrosine kinase. Several variants of EML4-ALK gene rearrangement based on the location in the EML4 gene involved in the rearrangement have been described, including variant 1 in which the rearrangement occurs with exon 13 of the EML4 gene fused to exon 20 of the ALK gene (E13:A20), variant 2 (E20:A20) and variant 3a/b (E6a/b:A20). In a retrospective analysis of 35 patients, Yoshida et al. showed that efficacy with crizotinib may vary based on the variant in a patient’s tumor, with longer progression-free survival (PFS) observed in patients with variant 1 EML4-ALK gene rearrangement [3]. Whether these variants influence the activity of the next generation of ALK inhibitors is unknown. Also Ou et al. recently reported that the emergence of ALK-resistant mutations occurred more commonly in patients with variant 3 EML4-ALK rearrangement than in patients with variant 1 tumors [4]. Other rarer ALK fusions occur such as KIF5B-ALK [5], KLC1-ALK [6], and ALK-PTPN3 [7], but they collectively are less frequent than the ALK-EML4 rearrangement [8], and therefore little is known about their clinical significance with respects to different response to ALK TKIs. In general, patients with ALK-rearranged NSCLC tend to be younger, never smokers, and have lung adenocarcinoma, though rarely patients with other lung cancer histologies have also been found to harbor this mutation [9]. Unlike mutations in EGFR (epidermal growth factor receptor), where the incidence is higher in patients of Asian descent, the incidence of ALK rearrangements appears to be similar between Western and Asian patients [10]. Other driver mutations rarely co-exist with ALK rearrangements in NSCLC.
2 Testing for Anaplastic Lymphoma Kinase (ALK)
Fluorescence in situ hybridization (FISH) is the current gold standard to detect ALK gene rearrangements [11]. It utilizes complementary DNA probes to the 3′ and 5′ ends that are then visualized with fluorescent microscopy, with a focus on chromosome 2p23, which is the location of the ALK gene. In the native state, the 2p23 region will be seen as either a fusion of two signals or two immediately adjacent signals. Due to its inversion nature, an ALK rearrangement is detected if the two signals are split and are less than two signal distances apart [12]. A joint guideline from the College of American Pathologists, International Association for the Study of Lung Cancer (IASLC), and Association for Molecular Pathology defines a positive ALK FISH as ≥15% of 50 nuclei assessed demonstrating the classic split-signal pattern. Interpretation should occur in areas with good signal, defined as where at least 50% of nuclei are easily analyzable [13]. The Vysis ALK FISH probe kit is US Food and Drug Administration (FDA) approved for the detection of ALK rearrangement. In this assay, a sample is considered to be positive for ALK if >25/50 cells demonstrate the classic signal and negative if <5/50 cells show the signal. In cases where 5–25 cells are positive, it is recommended to add both count readings and calculate an average percentage. If the average percentage is ≥15%, then the sample is considered positive. Immunohistochemistry (IHC) is a more readily available test and can be used to screen for ALK rearrangements, especially as novel antibodies have been developed against chimeric ALK proteins. However, some have raised concerns about the IHC test. Cabillic et al. showed that there was significant discordance between FISH and IHC when they conducted parallel testing on the same samples. Of 3244 cases, 150 were found to be ALK positive by FISH and/or positive by IHC, but only 80 of those samples were found to be positive by both FISH and IHC. They concluded that one-quarter of ALK-positive samples would have been missed had only single FISH or IHC testing been employed [14]. Both these tests are approved for the diagnosis of ALK-positive patients and most institutions use one of the two tests. Some institutions will confirm the IHC positive result with a FISH test. Reverse transcription–polymerase chain reactions (RT-PCR) and next-generation sequencing (NGS) panels are also being used to detect the presence of a variety of potentially targetable mutations. The National Comprehensive Cancer Network (NCCN) guidelines currently recommend confirming the presence of ALK rearrangements using FISH if the initial screen with IHC returned positive. While there are no specific guidelines regarding the use of NGS, it appears to be as sensitive a method as FISH for detecting the presence of ALK rearrangements [15].
3 Therapeutic Options
3.1 Crizotinib
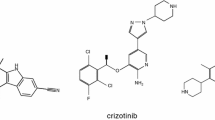
Crizotinib is a small-molecule tyrosine kinase inhibitor (TKI) of ALK, c-MET, and ROS-1. Camidge et al. were the first to report from an expansion phase I trial (PROFILE 1001) that it was a tolerable and safe drug that resulted in durable responses in patients with ALK-rearranged NSCLC [16]. Shaw et al. showed in a randomized phase III trial (PROFILE 1007) that in patients with advanced ALK-rearranged NSCLC that had progression after platinum-based chemotherapy, treatment with crizotinib led to improved PFS compared to chemotherapy [17]. There was a significantly higher response rate to crizotinib (65%) versus chemotherapy (20%). In another randomized phase III trial, Solomon et al. demonstrated the superiority of crizotinib over standard platinum doublet chemotherapy as first-line therapy for ALK-rearranged NSCLC in PROFILE 1014 [18]. In this study, the median PFS (mPFS) for crizotinib was 10.9 months compared with 7.0 months for chemotherapy (hazard ratio [HR] 0.45, p < 0.001). There was a higher response rate with crizotinib (74%) than with chemotherapy (45%, p < 0.001). Response was also more durable on crizotinib (11.3 vs. 5.3 months). There was no difference in overall survival (OS) between the two groups, which is likely due to 70% of patients in the chemotherapy group crossing over to the crizotinib group. As a result of these studies, crizotinib is approved in the USA, European Union (EU), and Japan as front-line therapy for patients with advanced ALK-rearranged NSCLC at a dose of 250 mg orally twice daily. Overall, the drug is well-tolerated. The most common toxicities of crizotinib include visual disturbances (photophobia, floaters, blurry vision), edema, and diarrhea. The most frequent grade 3/4 toxicities are elevated aminotransferases and neutropenia. With regard to these adverse events, most instances of elevated aminotransferases were asymptomatic and resolved with dose interruption or reduction. There were no episodes of febrile neutropenia. There was one grade 5 adverse event in the PROFILE 1014 trial, which was attributed to crizotinib-associated pneumonitis. Pneumonitis/interstitial lung disease of any grade is seen in approximately 2.5% of patients treated with crizotinib [19].
3.1.1 Resistance to Crizotinib
The mPFS for patients on crizotinib for ALK-rearranged NSCLC is about 8–11 months based on PROFILE 1007 and PROFILE 1014. Mechanisms of resistance to crizotinib can be divided into three categories: (1) development of secondary resistance mutation in the ALK kinase domain leading to steric hindrance of crizotinib binding or amplification of the ALK gene; (2) activation of alternative bypass pathways that liberate tumoral reliance on ALK signaling; and (3) limited penetrance into sanctuary sites, in particular the central nervous system (CNS) [20]. In one review, about 38% of patients had either a secondary mutation or amplification of the ALK locus; the most common point mutations being L1196M and G1269A [21]. Bypass tract activation include EGFR mutations, MET amplification, and KRAS mutations. However, the exact mechanism of resistance is still unknown in a large proportion of patients.
The most common site of disease progression while on crizotinib is the CNS. In a retrospective review of two clinical trials, 72% of patients who had previously treated brain metastases had secondary progression of CNS disease while on crizotinib. In patients who did not have evidence of brain metastases at baseline, 20% developed brain metastases while on therapy [22]. This observation can be partly explained by limited penetrance of crizotinib into the cerebrospinal fluid (CSF) (blood–brain barrier) as suggested by Costa et al. who showed in a patient with intracranial progression on crizotinib that the CSF concentration of the drug was nearly 1000 times lower than the plasma concentration [23].
3.2 Next-Generation ALK Inhibitors in the Post-Crizotinib Setting
Given the inevitable progression of disease while on crizotinib, next-generation ALK inhibitors have been developed to overcome crizotinib resistance. There are currently three second-generation ALK inhibitors, ceritinib, alectinib, and brigatinib, that are FDA approved for use in ALK-rearranged NSCLC following progression on or intolerance to crizotinib. All of these drugs are more potent inhibitors of ALK than crizotinib in the pre-clinical setting. Table 1 provides a summary of the studies with these agents in the post-crizotinib setting. Active trials are ongoing with lorlatinib, a third-generation ALK inhibitor, as well as the ALK inhibitors entrectinib and ensartinib.
3.2.1 Ceritinib
The initial phase I trial (ASCEND-1) of ceritinib showed a response rate of 56% in NSCLC patients who were previously treated with crizotinib [28]; response in CNS lesions were also seen. The ASCEND-2 trial specifically examined intracranial response along with whole-body response in patients who had previously received platinum chemotherapy and crizotinib. The overall response rate (ORR) in patients with baseline brain metastases was 33%, with a disease control rate (DCR) of 74% [29]. The most common adverse events associated with ceritinib include nausea, vomiting, diarrhea, as well as rise in liver function tests, which required dose adjustment/treatment interruption in 80% of patients. The FDA-approved dosing for ceritinib is 750 mg orally daily, which is the same in the EU and Japan.
3.2.2 Alectinib
A phase I/II study of alectinib in previously crizotinib-treated patients showed a response rate of 55% with an intracranial response rate of 52%, which included a patient with leptomeningeal carcinomatosis [30]. In a single-group, multicenter phase II study conducted in the USA and Canada, the ORR was 52% with a median duration of 13.5 months [25]. Furthermore, 75% of patients with measurable CNS metastases achieved a response with a median duration of 11.1 months. Ou et al. conducted a global phase II study with alectinib, which yielded similar results, showing an ORR of 50% with a median duration of response of 11.2 months [26]. Of the patients with baseline CNS metastases, 57% achieved a response with a median duration of 10.3 months. Alectinib was overall well-tolerated with the most common adverse effects of constipation, fatigue, and myalgia occurring in approximately 30% of patients and all being grade 1 or 2. The approved dosing for alectinib in the USA and EU is 600 mg orally twice daily. The approved dose in Japan, however, is 300 mg orally twice daily. In studies conducted in Japan, dose escalation beyond 300 mg twice daily was not carried out due to limitations in Japan on the quantity of an additive present in alectinib capsules [31].
3.2.3 Brigatinib
Preclinical work showed that brigatinib was more potent and maintained activity against 17 secondary ALK mutations, with superior inhibitory activity compared to crizotinib, ceritinib, and alectinib [32]. The phase I/II trial showed an ORR of 72% in previously crizotinib-treated ALK-rearranged NSCLC patients with an intracranial response rate of 53% [33]. Updated data presented at the 2016 World Conference on Lung Cancer (WCLC) showed a mPFS of 13.4 months in crizotinib-refractory patients, which is longer than for ceritinib and alectinib in this setting [34]. An AE unique to brigatinib is early pulmonary events, including cough, dyspnea, pneumonia/pneumonitis, and hypoxia, which occurred in 6–8% of patients [33, 35] with onset typically within 7 days after initiation of brigatinib therapy. The phase II ALTA trial therefore looked at two different dosing schedules at either 90 mg daily (group A) or 90 mg daily with escalation to 180 mg daily after 7 days (group B). The ORR was 45% in group A and 54% in group B [27]. The median duration of response was 13.8 months in group A and 11.1 months in group B. Furthermore, the intracranial response was also robust at 42% in group A and 67% in group B. The cumulative incidence of early pulmonary AEs was 6%, occurring at 90 mg daily in both groups, without any occurrence after successful escalation to the 180 mg dose. The pulmonary AEs were managed with dose reduction. The FDA therefore approved brigatinib dosing as per group B in the ALTA trial. Brigatinib has not yet been approved in the EU or Japan.
3.2.4 Lorlatinib
Lorlatinib is the only third-generation ALK inhibitor. Preclinical data shows that it is more potent than crizotinib, ceritinib, and alectinib with in vivo activity against the highly resistant G1202R mutation, which is resistant to the other TKIs, including brigatinib [36]. At the 2017 American Society for Clinical Oncology (ASCO) meeting, Shaw et al. presented the preliminary data for the phase I/II trial of lorlatinib in ALK-positive patients who had received one or more prior ALK TKI. Lorlatinib demonstrated impressive activity in heavily pretreated patients; the relative risk (RR) ranged from 31% in patients who received three prior TKIs with or without chemotherapy to 57% in patients who only received previous crizotinib [37]. The intracranial RR also ranged from 43% to 60%, with on overall RR of 48.1%. Lorlatinib appeared to be well-tolerated with the most significant treatment-related AEs being hypercholesterolemia and hypertriglyceridemia. Only 3.4% of patients discontinued treatment due to AEs. AEs unique to lorlatinib are cognitive defects (19% of patients) and mood effects (13% of patients). According to the investigators, the majority were grade 1 and were transient/reversible.
3.2.5 Entrectinib and Ensartinib
Entrectinib is an oral inhibitor of TRK A/B/C, ROS1, and ALK. The results of two phase I studies with 119 patients have been published, with 71 of these patients having NSCLC [38]. No responses were observed in patients who had previously received an ALK TKI. The ORR was 57% in ALK-rearranged solid tumors, which included NSCLC.
Ensartinib is an oral inhibitor of ALK with activity also against MET, ABL, ROS1, Axl, EPHA2, LTK, and SLK. The results of the phase I/II study with ensartinib in patients with NSCLC that were either TKI-naïve or resistant to crizotinib were presented at the IASLC 2016 conference [39]. Responses were seen in patients who are crizotinib naïve (77%) and crizotinib resistant (73%).
3.3 Next-Generation ALK Inhibitors as First-Line Therapy
As progression on crizotinib eventually occurs, particularly in the CNS, there is great interest in understanding whether the initiation of second-generation ALK inhibitors as first-line therapy is a superior treatment paradigm.
3.3.1 Ceritinib
The phase III ASCEND-4 trial demonstrated the superiority of ceritinib as first-line therapy for ALK-rearranged NSCLC over platinum–pemetrexed doublet, including improved ORR in the CNS of 72.7% compared to 27.3% [40]. The mPFS as assessed by an independent committee was 16.6 months for ceritinib and 8.1 months for chemotherapy with a HR of 0.55 (p < 0.00001). The efficacy appeared to differ based on the presence of brain metastases at baseline. The mPFS in patients without baseline brain metastases was 26.3 months for ceritinib compared to 8.3 months for chemotherapy (HR 0.48). In contrast, in patients with baseline brain metastases, the mPFS was 10.7 months for ceritinib and 6.7 months for chemotherapy (HR 0.70). Ceritinib was approved in May 2017 for the front-line treatment of ALK-positive NSCLC but has not been compared head-to-head against crizotinib in the front-line setting. Looking at two different trials, in patients that progressed on crizotinib who then were switched to ceritinib therapy, the combined mPFS was 17.4 months [41] compared to 16.6 months with ceritinib alone [40].
In the ASCEND-5 phase III trial, ceritinib was compared to chemotherapy in patients with disease progression after one to two lines of chemotherapy and crizotinib. The response rate for the ceritinib group was 39.1% compared to 6.9% in the chemotherapy group [24]. While the FDA-approved dose of ceritinib is 750 mg orally daily, 80% of patients in the ASCEND-5 trial required dose adjustment, interruption, or delay, with 61% requiring at least one dose reduction. The most common adverse symptoms that led to dose reduction include nausea, vomiting, and diarrhea. Given the concern regarding poor tolerance of ceritinib, the ASCEND-8 trial sought to evaluate whether lower doses of ceritinib at 450 mg and 600 mg given with a low-fat meal could reduce the adverse gastrointestinal effects of ceritinib 750 mg taken on an empty stomach. Ceritinib 450 mg taken with a low-fat meal demonstrated similar pharmacokinetics as 750 mg fasting, with less gastrointestinal (GI) adverse effects and no grade 3 GI events [42]. However, the overall rate of suspected drug-related adverse events occurred in 41% of patients at the 450 mg dose and no efficacy data with this dose is as yet available. These data suggest that modification of the approved dose may allow greater tolerability of the drug.
3.3.2 Alectinib
The preliminary results of the phase III J-ALEX trial comparing upfront alectinib versus crizotinib in treatment-naïve patients with ALK NSCLC were presented at ASCO 2016; there was a significantly increased mPFS favoring alectinib over crizotinib (HR 0.34, p < 0.0001) [43]. This study was updated at ASCO 2017 and immediately published thereafter. The mPFS was not assessable on alectinib compared to 10.2 months on crizotinib [44]. Response rate also favored alectinib at 85% compared to 70% with crizotinib. However, as the study was conducted exclusively in Japan, the practice was not widely adapted given concerns regarding applicability with respect to the patient population and different dosage used at 300 mg orally twice daily. At ASCO 2017, Shaw et al. reported results of the phase III global ALEX trial, which was subsequently published. In this study, the dosage of alectinib was 600 mg orally twice daily. Alectinib led to a significant reduction in risk of progression/death with HR 0.47 (p < 0.0001); the mPFS for crizotinib was 11.1 months, but had not yet been reached for alectinib [45, 46]. The intracranial response for patients with measurable CNS lesions at baseline was 50% for crizotinib and 81% for alectinib; the time to progression in the CNS also favored alectinib with a HR of 0.16 (p < 0.0001). Grade 3/4 AEs were also less frequent with alectinib than with crizotinib (41% vs. 50%, respectively). While the FDA has not yet approved alectinib as front-line therapy for patients with ALK-positive NSCLC, the results of the J-ALEX and ALEX trials suggest that front-line treatment with alectinib leads to a significantly longer PFS than crizotinib and appears to be better tolerated. The results of the two trials also suggest that front-line alectinib does not have an inferior PFS compared to sequential crizotinib followed by alectinib. Table 2 summarizes current data on ALK inhibitors used in the front-line setting.
3.4 Sequence of ALK Inhibitors
While it is not yet known which ALK inhibitor is the ideal first-line therapy, there are more data to guide selection of the next-generation ALK inhibitor post-crizotinib. As ceritinib was only recently approved as initial therapy, there is little data regarding front-line progression on this drug. With advancements in sequencing technology, multiple mutations in ALK have been discovered that convey either resistance or sensitivity. The mutation profile coverage varies among the next-generation ALK inhibitors [47]. Currently, knowing the resistance mutation does not impact the choice of post-crizotinib therapy, especially as mutations account for only one-third of resistance mechanisms. But, given the availability of several next-generation ALK inhibitors, the presence of a specific resistance mutation, as well as the cost and adverse effect profile of each drug, can help guide therapy.
Gainor et al. evaluated post-progression biopsies of patients treated with second-generation ALK inhibitors and found that ALK resistance mutations were present in 56% of patients who progressed on second-generation ALK TKIs (compared to 20% of patients who progressed on crizotinib), with the most common being the G1202R mutation [47]. They proposed that in the setting of progression on a second-generation ALK inhibitor, repeat biopsy to assess for ALK mutations should be strongly considered as the presence of an ALK resistance mutation suggests that it remains the main oncogenic driver and the patient should be considered for further ALK-directed therapy. However, should the tumors not harbor ALK mutations, then other treatment strategies (i.e., combination chemotherapy) should be considered over ALK TKI monotherapy [8]. The data generated by Gainor et al. is in patients who received next-generation ALK inhibitors after having received crizotinib. It is currently not known if the profile of resistance mechanisms in patients who receive these agents as front-line therapy will be the same.
The L1198F mutation is worthy of further discussion as it conveys sensitivity to crizotinib but not likely to any of the other next-generation ALK inhibitors. This was first presented by Shaw et al., who described a patient with metastatic ALK-rearranged NSCLC who received lorlatinib through a clinical trial after progression of disease on crizotinib, ceritinib, and carboplatin–pemetrexed chemotherapy [48]. At time of progression on lorlatinib, she underwent biopsy of a resistant liver lesion which demonstrated the presence of C1156Y (previously detected) and L1198F mutations. Pharmacodynamic studies revealed increased binding affinity to crizotinib of this specific mutation compared to other ALK inhibitors. The patient was re-challenged with crizotinib and exhibited a significant radiographic response. This case report demonstrates the role for evaluating resistance mutations at time of progression, particularly in patients who have had two or more ALK inhibitors.
4 Post-ALK Inhibitor Therapy
There has not been any data published on the efficacy of chemotherapy for patients with ALK-rearranged NSCLC after progression on two or more ALK inhibitors. The phase III trials of ceritinib and crizotinib showed response rates of 27–45% to chemotherapy in patients with ALK-rearranged NSCLC. In a large retrospective study, however, the RR to platinum-based chemotherapy was shown to be only 18% in treatment-naïve ALK-rearranged patients [49]. The results of the ASCEND-5 trial showed that the response rate to ceritinib was significantly better than to chemotherapy as second-line therapy (39.1% vs. 6.9%) [41]. In this study, however, the patients received second-line single agent docetaxel or pemetrexed as they had all previously received front-line platinum-based chemotherapy. An earlier retrospective review by Shaw et al. showed that in comparison to ALK-negative patients, ALK-positive patients had a similar improved mPFS when treated with a platinum–pemetrexed doublet [50]. While the efficacy of the platinum–pemetrexed doublet in ALK TKI-refractory patients who are chemotherapy-naïve has not been explicitly reported, existing data suggest that it is a combination that is worthy of consideration.
The PD-1 (programmed cell death-1) inhibitors nivolumab and pembrolizumab as well as the PD-L1 (programmed cell death ligand-1) inhibitor atezolizumab are all approved for the treatment of advanced NSCLC after large trials demonstrated their superiority to docetaxel chemotherapy in patients that have progressed on standard platinum-based doublet chemotherapy [51,52,53,54]. Pembrolizumab has also been approved as initial therapy for patients with metastatic NSCLC with PD-L1 expression ≥50% as evaluated by IHC [55] or in conjunction with carboplatin and pemetrexed as first-line therapy for all non-squamous histologies irrespective of PD-L1 expression [58]. While PD-L1 expression is not an absolute indicator of response to checkpoint inhibition, there are data to suggest that increased PD-L1 is associated with improved response to these agents [56].
Preclinical data suggested that ALK-rearranged and EGFR-mutant NSCLC cells had significantly higher PD-L1 expression than their wild-type counterparts, suggesting that they may be responsive to checkpoint inhibitors [57]. However, preclinical data also showed that EGFR TKIs such as gefitinib decreased PD-L1 expression [58]. Therefore, one mechanism of ‘resistance’ to checkpoint inhibitors in TKI-refractory tumors could be through the down-regulation of PD-L1 expression by the TKI. Gainor et al. conducted a retrospective review on EGFR-mutated and ALK-rearranged NSCLC patients treated with PD-1/PD-L1 inhibitors after progression on TKIs. Though their sample size was small, zero of six patients with ALK-rearranged NSCLC had an objective radiographic response to checkpoint inhibition [59]. They also assessed PD-L1 expression in ALK-rearranged NSCLC prior to crizotinib and at the time of crizotinib resistance. They found that 47% of crizotinib-naïve patients had PD-L1 ≥5% and 25% of crizotinib-resistant patients had PD-L1 ≥5%. Recently, Garassino et al. presented the results from the ATLANTIC study that included a cohort of EGFR- and ALK-positive patients treated with durvalumab, a PD-L1-directed antibody [60]. All patients had received at least two prior treatments, including a TKI and platinum-based chemotherapy. The response rate observed was 12.2% in patients whose tumors had high PD-L1 expression (n = 74) and 3.6% in patients who had low or negative PD-L1-expressing tumors (n = 28). The mPFS was 1.9 months in all patients, with a median survival ranging from 9.9 to 13.3 months.
Lack of activity of PD-1/PD-L1-directed agents has also been observed in patients who are never smokers and in patients with EGFR mutation-positive NSCLC [51, 52, 61]. It has been shown that NSCLC patients with tumors that have a high mutational burden have a greater probability of benefit from checkpoint inhibition [62]. It is hypothesized that tumors with high mutational burden express more novel neoantigens that can be targeted by an activated immune system, whereas tumors with low mutational burden may express far fewer neoantigens, limiting the anti-tumor efficacy of the immune system. It is well-recognized that tumors in never smokers and ALK-positive and EGFR-mutated NSCLC patients have low mutational burden. This observation may also help to explain the limited efficacy of checkpoint inhibitors in these patients.
While there are no trials comparing immunotherapy with ALK TKIs as upfront treatment of ALK-rearranged NSCLC, the data at least suggest that PD-1/PD-L1 inhibitors are not effective in a high proportion of ALK-positive patients who have progressed on TKI therapy. It is unclear if combination immune therapy such as combination of an anti-CTLA4 (cytotoxic T lymphocyte-associated molecule-4) and anti-PD-1/PD-L1 antibodies or combination of PD-1-directed agents with chemotherapy will provide greater benefit in these patients.
5 Localized Therapy for Brain Metastases
While next-generation ALK TKIs can delay intracranial progression, it eventually does occur and therefore it is important to consider other localized therapy for the treatment of brain metastases, including radiation and surgery. Maximum preservation of cognitive function must be considered, especially as patients with ALK-rearranged NSCLC tend to be younger. Stereotactic radiosurgery (SRS) is recommended if there are a few discrete lesions, but whole brain radiation (WBRT) must be considered for greater burden of disease. It is currently unknown if concurrent administration of radiation while on an ALK TKI is safe and therefore it has been accepted practice to have patients suspend taking the drug during radiation treatment [63]. Mak et al. assessed the impact of genetic alterations on survival after receiving radiation therapy for brain metastases in NSCLC. They found a significantly improved OS of 26.3 months for patients with ALK-rearranged NSCLC compared with 5.5 months for patients without any identifiable genetic alterations (p = 0.001) [64]. It is thought that radiation can increase the permeability of the blood–brain barrier, thereby rendering TKI more effective. One retrospective study showed that patients with only intracranial progression had a continued mPFS of 7.1 months when resumed on crizotinib post-radiation [65]. While it is generally recommended to continue the same TKI post-radiation, the benefit of switching TKI at that time has not been specifically addressed.
6 Future Directions
The development and approval of the next-generation ALK inhibitors have improved the options for patients with ALK-rearranged NSCLC. Crizotinib was the first FDA-approved agent for initial therapy of ALK-rearranged NSCLC. However, the results of the J-ALEX, ALEX, and ASCEND-4 trials suggest that patients derive greater clinical benefits by starting on next-generation ALK inhibitors compared to crizotinib, leading to the recent approval of ceritinib as initial therapy. We also expect that alectinib will soon receive the same approval. With the approval of a second-generation ALK inhibitor as initial therapy, it is unclear if the patient would be a candidate for an alternative second-generation inhibitor at progression. The different mutation profiles suggest that switching between second-generation inhibitors may be a possible therapeutic option, but it is not known if the same resistance mutations will develop. Further investigation is therefore needed to better understand the mechanisms that drive the development of resistance in patients who start on the next generation of ALK inhibitors.
The optimal treatment for TKI-resistant ALK-rearranged NSCLC is also unclear. While the data for either platinum-based chemotherapy or immunotherapy does not appear to be favorable, prospective data are needed. A strategy that should be considered is combination therapy with other agents, as most of the work in overcoming ALK resistance thus far has focused on monotherapy with more potent next-generation ALK inhibitors. Combining an ALK TKI with a second TKI that targets bypass tracts (i.e., EGFR, cKIT, MEK) could be a viable strategy in tumors where the resistance pathway has been identified [66]. While checkpoint inhibitors as monotherapy does not seem to be efficacious, the combination should be examined given pre-clinical data suggesting the up-regulation of PD-L1 expression by TKIs, which if used in combination with a checkpoint inhibitor may result in greater response. This approach has been attempted in EGFR-mutated NSCLC with the combination of osimertinib (EGFR TKI) and durvalumab (PD-L1 inhibitor), but the trial was discontinued due to an increased incidence of pneumonitis [66]. It is not known whether the same adverse effects would be observed with the combination of an ALK TKI and a checkpoint inhibitor.
7 Summary
From the discovery of the ALK-EML4 fusion as an oncogenic driver in a subset of NSCLC one decade ago to today, significant advancements have been made in the treatment of patients with ALK-rearranged NSCLC. With the arrival of next-generation ALK inhibitors, some of which have moved into the front line as initial therapy, patients have been able to derive greater clinical benefit. However, there is a significant need to understand the drivers of and mechanisms underlying resistance as it inevitably occurs in patients treated with TKIs. The development of novel agents that target other oncogenic pathways raises the possibility for combination therapy or salvage therapy for TKI-refractory patients. The progress that has been made in the treatment of ALK-rearranged NSCLC highlights the importance of understanding molecular drivers of cancer as we enter the era of precision oncology.
References
Tsao AS, Scagliotti GV, Bunn PA, Carbone DP, Warren GW, Bai C, et al. Scientific advances in lung cancer 2015. J Thorac Oncol. 2016;11:613–38.
Soda M, Choi YL, Enomoto M, Takada S, Yamashita Y, Ishikawa S, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature. 2007;448:561–6.
Yoshida T, Oya Y, Tanaka K, Shimizu J, Horio Y, Kuroda H, et al. Differential crizotinib response duration among ALK fusion variants in ALK-positive non-small-cell lung cancer. J Clin Oncol. 2016;34:3383–9.
Ou S-HI, Schrock AB, Gowen K, Stephens PJ, Ross JS, Johnson ML, et al. Association of ALK resistance mutations by EML4-ALK variant (v3 vs. non-v3) in ALK+ non-small cell lung cancer (NSCLC). J Clin Oncol. 2017;35(Suppl 15):9010.
Takeuchi K, Choi YL, Togashi Y, Soda M, Hatano S, Inamura K, et al. KIF5B-ALK, a novel fusion oncokinase identified by an immunohistochemistry-based diagnostic system for ALK-positive lung cancer. Clin Cancer Res. 2009;15:3143–9.
Togashi Y, Soda M, Sakata S, Sugawara E, Hatano S, Asaka R, et al. KLC1-ALK: a novel fusion in lung cancer identified using a formalin-fixed paraffin-embedded tissue only. PLoS One. 2012;7:e31323.
Jung Y, Kim P, Jung Y, Keum J, Kim S-N, Choi YS, et al. Discovery of ALK-PTPN3 gene fusion from human non-small cell lung carcinoma cell line using next generation RNA sequencing. Genes Chromosom Cancer. 2012;51:590–7.
Lin JJ, Riely GJ, Shaw AT. Targeting ALK: precision medicine takes on drug resistance. Cancer Discov. 2017;7:137–55.
Fan L, Feng Y, Wan H, Shi G, Niu W. Clinicopathological and demographical characteristics of non-small cell lung cancer patients with ALK rearrangements: a systematic review and meta-analysis. PLoS One. 2014;9:e100866.
Solomon B, Varella-Garcia M, Camidge DR. ALK gene rearrangements: a new therapeutic target in a molecularly defined subset of non-small cell lung cancer. J Thorac Oncol. 2009;4:1450–4.
Guérin A, Sasane M, Zhang J, Macalalad AR, Galebach P, Jarvis J, et al. ALK rearrangement testing and treatment patterns for patients with ALK-positive non-small cell lung cancer. Cancer Epidemiol. 2015;39:307–12.
Wallander ML, Geiersbach KB, Tripp SR, Layfield LJ. Comparison of reverse transcription-polymerase chain reaction, immunohistochemistry, and fluorescence in situ hybridization methodologies for detection of echinoderm microtubule-associated proteinlike 4-anaplastic lymphoma kinase fusion-positive non-small cell lung carcinoma: implications for optimal clinical testing. Arch Pathol Lab Med. 2012;136:796–803.
Lindeman NI, Cagle PT, Beasley MB, Chitale DA, Dacic S, Giaccone G, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol. 2013;8:823–59.
Cabillic F, Gros A, Dugay F, Begueret H, Mesturoux L, Chiforeanu DC, et al. Parallel FISH and immunohistochemical studies of ALK status in 3244 non-small-cell lung cancers reveal major discordances. J Thorac Oncol. 2014;9:295–306.
Abel HJ, Al-Kateb H, Cottrell CE, Bredemeyer AJ, Pritchard CC, Grossmann AH, et al. Detection of gene rearrangements in targeted clinical next-generation sequencing. J Mol Diagn. 2014;16:405–17.
Camidge DR, Bang Y-J, Kwak EL, Iafrate AJ, Varella-Garcia M, Fox SB, et al. Activity and safety of crizotinib in patients with ALK-positive non-small-cell lung cancer: updated results from a phase 1 study. Lancet Oncol. 2012;13:1011–9.
Shaw AT, Kim D-W, Nakagawa K, Seto T, Crinó L, Ahn M-J, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368:2385–94.
Solomon BJ, Mok T, Kim D-W, Wu Y-L, Nakagawa K, Mekhail T, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371:2167–77.
Maka VV, Krishnaswamy UM, Anil Kumar N, Chitrapur R, Kilara N. Acute interstitial lung disease in a patient with anaplastic lymphoma kinase-positive non-small-cell lung cancer after crizotinib therapy. Oxf Med Case Rep. 2014;2014:11–2.
Steuer CE, Ramalingam SS. ALK-positive non-small cell lung cancer: mechanisms of resistance and emerging treatment options. Cancer. 2014;120:2392–402.
Awad MM, Shaw AT. ALK inhibitors in non-small cell lung cancer: crizotinib and beyond. Clin Adv Hematol Oncol. 2014;12:429–39.
Costa DB, Shaw AT, Ou S-HI, Solomon BJ, Riely GJ, Ahn M-J, et al. Clinical experience with Crizotinib in patients with advanced ALK-rearranged non-small-cell lung cancer and brain metastases. J Clin Oncol. 2015;33:1881–8.
Costa DB, Kobayashi S, Pandya SS, Yeo W-L, Shen Z, Tan W, et al. CSF concentration of the anaplastic lymphoma kinase inhibitor crizotinib. J Clin Oncol. 2011;29:e443–5.
Shaw AT, Kim TM, Crinò L, Gridelli C, Kiura K, Liu G, et al. Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2017;18:874–86.
Shaw AT, Gandhi L, Gadgeel S, Riely GJ, Cetnar J, West H, et al. Alectinib in ALK-positive, crizotinib-resistant, non-small-cell lung cancer: a single-group, multicentre, phase 2 trial. Lancet Oncol. 2016;17:234–42.
Ou S-HI, Ahn JS, De Petris L, Govindan R, Yang JC-H, Hughes B, et al. Alectinib in Crizotinib-refractory ALK-rearranged non-small-cell lung cancer: a phase II global study. J Clin Oncol. 2016;34:661–8.
Kim D-W, Tiseo M, Ahn M-J, Reckamp KL, Hansen KH, Kim S-W, et al. Brigatinib in patients with Crizotinib-refractory Anaplastic lymphoma Kinase-positive non-small-cell lung cancer: a randomized, multicenter phase II trial. J Clin Oncol. 2017;35:2490–8.
Shaw AT, Kim D-W, Mehra R, Tan DSW, Felip E, Chow LQM, et al. Ceritinib in ALK-rearranged non-small-cell lung cancer. N Engl J Med. 2014;370:1189–97.
Crinò L, Ahn M-J, De Marinis F, Groen HJM, Wakelee H, Hida T, et al. Multicenter phase II study of whole-body and intracranial activity with Ceritinib in patients with ALK-rearranged non-small-cell lung cancer previously treated with chemotherapy and crizotinib: results from ASCEND-2. J Clin Oncol. 2016;34:2866–73.
Gadgeel SM, Gandhi L, Riely GJ, Chiappori AA, West HL, Azada MC, et al. Safety and activity of alectinib against systemic disease and brain metastases in patients with crizotinib-resistant ALK-rearranged non-small-cell lung cancer (AF-002JG): results from the dose-finding portion of a phase 1/2 study. Lancet Oncol. 2014;15:1119–28.
Seto T, Kiura K, Nishio M, Nakagawa K, Maemondo M, Inoue A, et al. CH5424802 (RO5424802) for patients with ALK-rearranged advanced non-small-cell lung cancer (AF-001JP study): a single-arm, open-label, phase 1-2 study. Lancet Oncol. 2013;14:590–8.
Zhang S, Anjum R, Squillace R, Nadworny S, Zhou T, Keats J, et al. The potent ALK inhibitor Brigatinib (AP26113) overcomes mechanisms of resistance to first- and second-generation ALK inhibitors in preclinical models. Clin Cancer Res. 2016;22:5527–38.
Gettinger SN, Bazhenova LA, Langer CJ, Salgia R, Gold KA, Rosell R, et al. Activity and safety of brigatinib in ALK-rearranged non-small-cell lung cancer and other malignancies: a single-arm, open-label, phase 1/2 trial. Lancet Oncol. 2016;17:1683–96.
Rosell R, Gettinger SN, Bazhenova LA, Langer CJ, Salgia R, Shaw AT, et al. 1330: Brigatinib efficacy and safety in patients (pts) with anaplastic lymphoma kinase (ALK)-positive (ALK+) non-small cell lung cancer (NSCLC) in a phase 1/2 trial. J Thorac Oncol. 2016;11:S114.
Kim D-W, Tiseo M, Ahn M-J, Reckamp KL, Hansen KH, Kim S-W, et al. Brigatinib (BRG) in patients (pts) with crizotinib (CRZ)-refractory ALK+ non-small cell lung cancer (NSCLC): First report of efficacy and safety from a pivotal randomized phase (ph) 2 trial (ALTA). J Clin Oncol. 2016;34(Suppl 15):9007.
Zou HY, Friboulet L, Kodack DP, Engstrom LD, Li Q, West M, et al. PF-06463922, an ALK/ROS1 inhibitor, overcomes resistance to first and second generation ALK inhibitors in preclinical models. Cancer Cell. 2015;28:70–81.
Shaw AT, Ignatius Ou S-H, Felip E, Bauer TM, Besse B, Gadgeel SM. Efficacy and safety of lorlatinib in patients (pts) with ALK+ non-small cell lung cancer (NSCLC) with one or more prior ALK tyrosine kinase inhibitor (TKI): a phase I/II study. J Clin Oncol. 2017;35(Suppl 15):9006.
Drilon A, Siena S, Ou S-HI, Patel M, Ahn MJ, Lee J, et al. Safety and antitumor activity of the multitargeted pan-TRK, ROS1, and ALK inhibitor Entrectinib: combined results from two phase I trials (ALKA-372-001 and STARTRK-1). Cancer Discov. 2017;7:400–9.
Horn L, Wakelee H, Reckamp KL, Blumenschein G, Infante JR, Carter CA, et al. MINI01.02: response and plasma genotyping from phase I/II trial of Ensartinib (X-396) in patients (pts) with ALK+ NSCLC: topic: medical oncology. J Thorac Oncol. 2016;11:S256–7.
Soria J-C, Tan DSW, Chiari R, Wu Y-L, Paz-Ares L, Wolf J, et al. First-line ceritinib versus platinum-based chemotherapy in advanced ALK-rearranged non-small-cell lung cancer (ASCEND-4): a randomised, open-label, phase 3 study. Lancet. 2017;389:917–29.
Gainor JF, Tan DSW, De Pas T, Solomon BJ, Ahmad A, Lazzari C, et al. Progression-free and overall survival in ALK-positive NSCLC patients treated with sequential crizotinib and ceritinib. Clin Cancer Res. 2015;21:2745–52.
Cho BC, Kim D-W, Bearz A, Laurie SA, McKeage M, Borra G, et al. ASCEND-8: a randomized phase 1 study of ceritinib 450 mg or 600 mg taken with a low-fat meal versus 750 mg in fasted state in patients with anaplastic lymphoma kinase (ALK)-rearranged metastatic non-small cell lung cancer (NSCLC). J Thorac Oncol. 2017;12(9):1357-67.
Nokihara H, Hida T, Kondo M, Kim YH, Azuma K, Seto T, et al. Alectinib (ALC) versus crizotinib (CRZ) in ALK-inhibitor naive ALK-positive non-small cell lung cancer (ALK+ NSCLC): Primary results from the J-ALEX study. J Clin Oncol. 2016;34(Suppl 15):9008.
Hida T, Nokihara H, Kondo M, Kim YH, Azuma K, Seto T, et al. Alectinib versus crizotinib in patients with ALK-positive non-small-cell lung cancer (J-ALEX): an open-label, randomised phase 3 trial. Lancet. 2017;390:29–39.
Shaw AT, Peters S, Mok T, Gadgeel SM, Ahn JS, Ou S-HI. Alectinib versus crizotinib in treatment-naive advanced ALK-positive non-small cell lung cancer (NSCLC): primary results of the global phase III ALEX study. J Clin Oncol. 2017;35. http://abstracts.asco.org/199/AbstView_199_185951.html. Accessed 13 Aug 2006.
Peters S, Camidge DR, Shaw AT, Gadgeel S, Ahn JS, Kim D-W, et al.; ALEX Trial Investigators. Alectinib versus crizotinib in untreated ALK-positive non-small-cell lung cancer. N Engl J Med. https://doi.org/10.1056/NEJMoa1704795.
Gainor JF, Dardaei L, Yoda S, Friboulet L, Leshchiner I, Katayama R, et al. Molecular mechanisms of resistance to first- and second-generation ALK inhibitors in ALK-rearranged lung cancer. Cancer Discov. 2016;6:1118–33.
Shaw AT, Friboulet L, Leshchiner I, Gainor JF, Bergqvist S, Brooun A, et al. Resensitization to crizotinib by the lorlatinib ALK resistance mutation L1198F. N Engl J Med. 2016;374:54–61.
Morodomi Y, Takenoyama M, Inamasu E, Toyozawa R, Kojo M, Toyokawa G, et al. Non-small cell lung cancer patients with EML4-ALK fusion gene are insensitive to cytotoxic chemotherapy. Anticancer Res. 2014;34:3825–30.
Shaw AT, Varghese AM, Solomon BJ, Costa DB, Novello S, Mino-Kenudson M, et al. Pemetrexed-based chemotherapy in patients with advanced, ALK-positive non-small cell lung cancer. Ann Oncol. 2013;24:59–66.
Herbst RS, Baas P, Kim D-W, Felip E, Pérez-Gracia JL, Han J-Y, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–50.
Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, et al. Nivolumab versus Docetaxel in advanced Nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373:1627–39.
Brahmer J, Reckamp KL, Baas P, Crinò L, Eberhardt WEE, Poddubskaya E, et al. Nivolumab versus docetaxel in advanced Squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373:123–35.
Fehrenbacher L, Spira A, Ballinger M, Kowanetz M, Vansteenkiste J, Mazieres J, et al. Atezolizumab versus docetaxel for patients with previously treated non-small-cell lung cancer (POPLAR): a multicentre, open-label, phase 2 randomised controlled trial. Lancet. 2016;387:1837–46.
Reck M, Rodríguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fülöp A, et al.; KEYNOTE-024 Investigators. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 2016;375(19):1823–33
Brahmer JR, Tykodi SS, Chow LQM, Hwu W-J, Topalian SL, Hwu P, et al. Safety and activity of anti-PD-L1 antibody in patients with advanced cancer. N Engl J Med. 2012;366:2455–65.
Ota K, Azuma K, Kawahara A, Hattori S, Iwama E, Tanizaki J, et al. Induction of PD-L1 expression by the EML4-ALK Oncoprotein and downstream signaling pathways in non-small cell lung cancer. Clin Cancer Res. 2015;21:4014–21.
Abdelhamed S, Ogura K, Yokoyama S, Saiki I, Hayakawa Y. AKT-STAT3 pathway as a downstream target of EGFR signaling to regulate PD-L1 expression on NSCLC cells. J Cancer. 2016;7:1579–86.
Gainor JF, Shaw AT, Sequist LV, Fu X, Azzoli CG, Piotrowska Z, et al. EGFR mutations and ALK rearrangements are associated with low response rates to PD-1 pathway blockade in non-small cell lung cancer: a retrospective analysis. Clin Cancer Res. 2016;22:4585–93.
Garassino MC, Cho B-C, Gray JE, Mazières J, Park K, Soo RA, et al. 82O. Durvalumab in ≥ 3rd-line EGFR mutant/ALK+, locally advanced or metastatic NSCLC: results from the phase 2 ATLANTIC study. Ann Oncol. 2017;28(Suppl 2):ii28-51.
Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–65.
Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–8.
Zhang I, Zaorsky NG, Palmer JD, Mehra R, Lu B. Targeting brain metastases in ALK-rearranged non-small-cell lung cancer. Lancet Oncol. 2015;16:e510–21.
Mak KS, Gainor JF, Niemierko A, Oh KS, Willers H, Choi NC, et al. Significance of targeted therapy and genetic alterations in EGFR, ALK, or KRAS on survival in patients with non-small cell lung cancer treated with radiotherapy for brain metastases. Neuro-Oncology. 2015;17:296–302.
Weickhardt AJ, Scheier B, Burke JM, Gan G, Lu X, Bunn PA, et al. Local ablative therapy of oligoprogressive disease prolongs disease control by tyrosine kinase inhibitors in oncogene addicted non-small cell lung cancer. J Thorac Oncol. 2012;7:1807–14.
Katayama R, Lovly CM, Shaw AT. Therapeutic targeting of anaplastic lymphoma kinase in lung cancer: a paradigm for precision cancer medicine. Clin Cancer Res. 2015;21:2227–35.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Angel Qin is supported by the National Institute of Health Oncology Research Training Grant 5T32CA009357-35.
Conflicts of Interest
Angel Qin has no conflicts of interest to declare. Shirish Gadgeel has received consulting fees or honorarium from Genentech/Roche, Ariad, Pfizer, Novartis, and Astra-Zeneca.
Rights and permissions
About this article
Cite this article
Qin, A., Gadgeel, S. The Current Landscape of Anaplastic Lymphoma Kinase (ALK) in Non-Small Cell Lung Cancer: Emerging Treatment Paradigms and Future Directions. Targ Oncol 12, 709–718 (2017). https://doi.org/10.1007/s11523-017-0526-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-017-0526-1