Abstract
Despite the development of novel effective therapeutic strategies, metastatic castration-resistant prostate cancer (mCRPC) remains a disease with a lethal course and a high biological and molecular heterogeneity. To date, germline mutations in the BRCA gene represent one of the main risk factors for developing prostate cancer, with a strong association with aggressive phenotype and poor clinical outcomes. A better understanding of the genomic landscape of prostate cancer has strengthened the idea that “synthetic lethality” of this disease might be useful in cancer-drug discovery, focusing on agents such as platinum compounds and poly (adenosine diphosphate [ADP]-ribose) polymerase inhibitors (PARPi). In this review, we summarize the main data available on BRCA mutations and discuss the clinical implications of these genomic aberrations in the management of prostate cancer, stressing the need to identify prognostic and predictive biomarkers and to deeply understand the mechanisms of treatment resistance, in order to maximize personalized medicine protocols and therefore clinical benefit.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Prostate cancer is the second most commonly diagnosed malignant tumor in men and a major cause of mortality, with an estimated 385,560 deaths globally projected for 2020 [1]. Androgen deprivation therapy (ADT), either by medical or surgical castration, represents the gold standard treatment for the management of prostate cancer patients who have relapsed after local therapy or who are affected by metastatic disease. However, disease is usually temporarily controlled, and despite early response to ADT exceeding 80–90 %, progression typically occurs within 12–24 months, a state now referred to as castration-resistant prostate cancer (CRPC) [2, 3]. Until 2010, docetaxel was the only agent to demonstrate a survival benefit in metastatic CRPC (mCRPC) [4, 5]. Since then, the therapeutic landscape of mCRPC has rapidly changed and several new drugs have been approved by regulatory authorities after demonstrating improved overall survival (OS) and maintaining patients’ quality of life in different pivotal trials, widely increasing the therapeutic armamentarium [6]. These include the tubulin targeting chemotherapy cabazitaxel [7], the second-line hormonal compounds abiraterone acetate [8, 9] and enzalutamide [10–12], the immunotherapy sipuleucel-T [13] and the alpha-emitting radiopharmaceutical radium-223 [14]. The availability of these new agents has led to the possibility of using them sequentially in order to achieve a cumulative survival benefit. To this end, several studies have tried to analyze patient cohorts receiving a sequence of two different new agents after docetaxel, but the retrospective nature, the small sample size and the short follow-up do not allow to obtain definitive conclusions regarding the best treatment strategy. In addition, differences in disease setting, criteria for selection of patients, comparator arms and definition of objective endpoints make it difficult to perform head-to-head comparisons between the different therapeutic strategies. Without such data and being evidence of possible cross-resistance between taxanes and new hormonal agents [15], the choice of the best therapeutic sequence remains difficult and treatment decisions are often based on characteristics of the individual patients. It is therefore clear, despite the recent progress, that mCRPC remains a disease with a lethal outcome and a median survival of approximately 18–36 months [16]. Identifying new treatments that provide durable disease control and further improvement in OS represents an important unmet medical need in order to maximize patient benefit and reduce costs and unnecessary toxicities.
2 Clinical and Molecular Heterogeneity in Prostate Cancer: The Impact of BRCA Mutations
It is now known that in prostate cancer the different patient responses to treatments and clinical outcomes is in part due to the high biological and molecular heterogeneity of this disease [17–20]. In the last few years, next-generation sequencing has led to significant advances in understanding the genomic landscape of this tumor [17, 21, 22], but, to date, none of the published phase III trials have shown a correlation between patients stratification on the basis of molecular profile and survival benefit. Therefore, a better understanding of the biological and clinical relevance of the molecular sub-classification may have a critical role in the development of new therapeutic approaches, representing a promising and engaging area of prostate cancer research. The identification of prognostic and predictive biomarkers will help in patient selection strategy in order to maximize personalized medicine protocols and therefore clinical benefit, avoiding needless side effects in patients who are unlikely to respond. In this direction, a variety of genomic aberrations have been evaluated and some of them have been discovered as common, including the transcription factor fusion of transmembrane protease serine 2-E26 transformation specific (TMPRSS2-ETS) and mutations in TP53, androgen receptor (AR), retinoblastoma 1 (RB1), phosphatase and tensin homolog/phosphatidylinositol-3-kinase (PTEN/PIK3CA) genes [17, 22]. In addition, it has recently been shown that alterations in DNA repair genes, such as the breast related cancer antigen (BRCA) and the ataxia-telangiectasia mutated (ATM), are present in about 23 % of prostate tumors [22] and seem to characterize a subgroup of patients with sensitivity to some drugs, becoming a source of interest for future research.
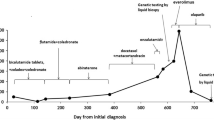
BRCA1 and BRCA2 are tumor-suppressor genes that are among the best-known cancer-susceptibility genes, characterized by an autosomal dominant inheritance pattern with incomplete penetrance. Although germline BRCA1 and BRCA2 mutations are present in only 0.44 % and 1–2 % of sporadic prostate cancer cases, respectively [23, 24], it has been described that about 15 % of mCRPC carry somatic point mutations or bi-allelic loss of BRCA1 or BRCA2 [22]. More recently, at the 2016 Genitourinary Cancers Symposium, Myers et al. reported the incidence of somatic BRCA mutations in a population of 85 advanced prostate cancer patients. Of interest, BRCA2 mutations were more frequent (12 %; 10/85) than BRCA1 (2 %; 2/85) and the concurrent mutations in BRCA1 and BRCA2 were found in 17 % (2/12) of patients [25]. This suggests that in advanced disease, genetic aberrations seem to occur at substantially higher frequency compared to primary prostate tumors (Fig. 1). Both genes encode proteins involved in maintenance of genomic stability by promoting efficient and precise repair of DNA double-strand breaks (DSBs) through the homologous recombination (HR) process [27]. Thus, cells deficient in functional BRCA1/2 become unable to repair DSBs, resulting in chromosomal instability, cell cycle arrest and apoptosis, underlining the increased cancer-susceptibility in BRCA mutation carriers. In addition, BRCA1 has been linked to other cellular processes, such as transcriptional regulation and chromatin modelling, while BRCA2 seems to be limited to DNA recombination and repair processes, being of particular importance in the regulation of recombinase RAD51 activity [28–31]. It is now known that germline presence of a single mutated copy of BRCA1/2 allele is associated with increased susceptibility to develop cancers, including breast and ovarian cancer in women and prostate cancer in men [32, 33]. Therefore, the loss of the wild-type copy (via somatic mutations or epigenetic mechanisms) in cells carrying heterozygous loss-of-function BRCA mutations is always required to support carcinogenesis, due to deficient HR DNA repair [34]. More recently, it has been shown that BRCA2 carriers have a significantly greater incidence of prostate cancer than the general population (standardized incidence ratios = 4.9, p = 0.002) [35] and that germline mutations in BRCA2 gene may confer the highest risk to develop this type of cancer (8.6-fold in men < 65 years compared to 3.4-fold in BRCA1 carriers) [23, 24]. In addition, BRCA2 aberrations may closely linked to a relative risk to develop prostate cancer at an early age (< 56 years) of about 23-fold compared to noncarriers [36, 37], although some authors reported no differences in mean age of presentation [38, 39]. However, despite that some hypotheses have emerged, the specific role of BRCA1 and BRCA2 in the development and progression of prostate cancer has not been yet elucidated. Evidence would seem to demonstrate that BRCA1 could play a role as a co-regulator of the AR and a mediator of IGF-1R in an AR-dependent manner [40], while the downregulation of BRCA2 expression may promote the metastatic potential of neoplastic cells by upregulation of matrix metalloproteinase 9 (MMP-9) [41]. More interestingly, recent studies have associated the presence of the deleterious BRCA2 germline mutations with a more poorly differentiated phenotype, nodal involvement and poor survival in prostate cancer [39, 42, 43]. In particular, Tryggvadottir et al. analyzed the prevalence of the BRCA2 999del5 mutation in prostate cancer patients belonging to the Icelandic population [42]. Compared with noncarriers, the presence of this truncating mutation was associated not only with a lower mean age at diagnosis, but also with a higher histologic grade, a more advanced tumor stage and a shorter median survival, underlining a strong potential correlation with a rapidly progressing lethal disease. Notably, the poor prognosis of this subset of patients was confirmed by other subsequent studies [44–46]. Edwards and colleagues performed an analysis on 21 BRCA2-mutation carriers and matched control unselected for family history and found that median OS of all prostate cancer cases with a germline mutation was significantly shorter that of controls (4.8 versus 8.5 years, respectively; p = 0.003) [45]. The multivariate analysis confirmed that the worse outcome was associated with the germline BRCA2 mutation per se, establishing it as an independent negative prognostic factor for survival in all stages of prostate cancer including localized disease. In addition, Thorne et al. evaluated the impact of the BRCA2 mutations in a setting of men ascertained from families at high risk of breast/ovarian cancer [46]. When comparing the carriers with noncarriers, BRCA2 mutation status was shown to be a significant prognostic predictor of both OS and prostate cancer-specific survival.
More recently, two studies from Castro’s group have provided relevant insights about the clinical implications of BRCA2 mutation. In the first study [47], the prognostic value of BRCA1/2 status was analyzed in a large series of patients with prostate cancer (2019 patients: 18 BRCA1 carriers, 61 BRCA2 carriers and 1940 noncarriers), confirming that the presence of this mutation predispose to a more aggressive phenotype, with a higher probability of nodal involvement and distant metastases. In addition, patients with BRCA mutations had poor survival outcomes, although subgroup analyses suggested that this association was mostly dependent on BRCA2, whereas the contribution of BRCA1 mutations remains unclear, probably due to the limited size and follow-up in this subgroup. Subsequently, in the study published in the 2015 [48], the outcomes of prostate cancer patients (both carriers and noncarriers) who underwent radical treatment for localized disease were evaluated, underscoring that BRCA2 mutation status resulted to be an independent prognostic factor for metastases-free survival and cause-specific survival, even after adjusting for cancer grade, stage and prostate-specific antigen (PSA) level in multivariate analysis. Similar results were obtained by Kim and colleagues [49]. In order to investigate the cytoplasmic protein expression of BRCA1 and BRCA2 in prostate cancer patients undergoing radical prostatectomy using immunohistochemical (IHC) analysis, they showed that overexpression of these proteins were significant independent prognostic factors for biochemical recurrence. Despite all these data, further large-scale studies are needed to confirm the association with histology and clinical outcome reported, and to determine if these findings can be generalized to the entire population.
Incidence of BRCA2 mutation in: (a) men with prostate cancer diagnosis before 65 years (1.2 %) [24], and (b) men with metastatic castration-resistant prostate cancer (mCRPC; 12.7 %) [22]. (c) Higher incidence of DNA-repair defects was found in mCRPC if, in addition to BRCA2, other mutations were included, such as BRCA1, FANCA, ATM, CHEK2, PALB2, HDAC2, MLH3, ERCC3, MRE11 and NBN (33 %) [69]
3 Medical Treatment of BRCA Mutation Carriers
3.1 Platinum-Based Chemotherapy
A better understanding of the genomic landscape of prostate cancer achieved in the last few years has strengthened the idea that “synthetic lethality” of this disease might be useful in cancer-drug discovery [50], despite that precision medicine is not yet feasible and the therapeutic relevance of findings remains unclear. Previous studies have demonstrated that BRCA1/2 mutations are associated with response to platinum-based chemotherapy in some types of cancer, notably in breast and ovarian cancer [51–53], suggesting a high sensitivity of these tumors to platinum agents. To date, platinum chemotherapy is used only for prostate cancer with neuroendocrine differentiation [54]. Nevertheless, phase II trials have shown that use of platinum-based chemotherapy in the post-docetaxel mCRPC setting may provide encouraging biochemical or radiological objective response rates (45–60 %) and a median progression free survival (PFS) of 4–9.5 months [55, 56]. Similarly, in a phase III study, Sternberg et al. have assessed the efficacy of the oral platinum analog satraplatin in patients with mCRPC previous treated with chemotherapy (the SPARC trial), showing a 33 % statistically significant reduction in the risk of progression compared to placebo, although a significant OS benefit has not been demonstrated [57]. This lack of survival advantage can be partly explained by the interpatient molecular heterogeneity and the absence of an optimal selection of patients. It is known that platinum compounds act to induce inter-strand and intra-strand DNA cross-links, with consequently increased DSBs and tumor cell death, due to destruction of the DNA repair machinery in HR repair deficient tumors. Therefore, it seems biologically reasonable to assume that mCRPC with BRCA mutations are more likely to respond to DNA cross-linking agents such as platinum analogues, as already demonstrated in ovarian and breast cancer [53, 58, 59]. Of interest, Cheng and colleagues have recently reported three cases of mCRPC with an exceptional response to platinum chemotherapy [60]. They assessed 14 patients with mCRPC treated with docetaxel and carboplatin, most of which had aggressive features such as visceral involvement, but none with evidence of neuroendocrine differentiation, and identified three patients with a complete or partial response to therapy. Using retrospectively targeted next-generation sequencing on tumor DNA assay, they found that all three patients had bi-allelic inactivation of BRCA2. Notably, two patients carried germline mutation (of which only one had family history of cancer) and the third patient had somatic homozygous BRCA copy loss; all three had somatic loss of function in the second allele in their metastases. Despite the small size and the retrospective nature of this report, it is the first to provide evidence that inactivation of BRCA2 may confer sensitivity to platinum agents in mCRPC unselected for a priori mutation and could be clinically useful as predictive biomarker of platinum response, supporting genetic testing in this disease.
3.2 PARP Inhibitors
The poly (adenosine diphosphate [ADP]-ribose) polymerases (PARPs) are a large family of multifunctional enzymes, the most common of which is PARP1 [61]. It is a zinc-finger DNA-binding enzyme, involved in the repair of DNA single-strand breaks through the repair of base excisions [62]. In cancer cells with BRCA mutation, this mechanism of DNA repair can compensate the loss of HR, but if PARPs are inhibited, cells are unable to repair DNA damage and accumulation of DSBs with consequent chromosomal instability, cell cycle arrest and apoptosis occur [63, 64] (Fig. 2). Therefore, similarly to platinum compounds, PARP inhibitors (PARPi) could induce selective tumor cytotoxicity, representing a potential and promising therapeutic approach in BRCA carriers [65, 66]. In support of this concept, it has been demonstrated that BRCA1/2 deficient cells are characterized by more PARPi responsiveness than normal cells in vitro [63, 67]. Based on these findings, several studies have assessed the efficacy and tolerability of some PARPi in different tumors. One of the most studied is olaparib (AZD2281 or KU-0059436), an oral potent and selective PARPi, which has shown significant monotherapy activity in tumors from BRCA mutation carriers, with an acceptable safety profile [26, 68]. More recently, consistent with findings reported for other tumor types, Mateo et al. conducted a phase II trial, the TOPARP-A trial, demonstrating a 33 % overall response rate to PARPi olaparib in sporadic cases of terminal mCRPC previously treated with standard treatments. Notably, next-generation sequencing showed that patients with DNA-repair gene defects had an impressive response rate (88 %) [69], underscoring that a subset of mCRPC could be molecularly stratified for treatment. Similar to that reported for olaparib, another PARPi, niraparib (MK4827), has shown antitumor activity in carriers of BRCA1/2 mutations and in patients with sporadic cancers [70], expanding the number of available inhibitors. All these encouraging results, both in term of activity and tolerability, have provided the rationale for PARPi-based combination therapies with the goal to maximize prostate cancer treatment, leading to design of studies combining PARPi with cytotoxic chemotherapy and hormonal therapy. In this direction, Hussain et al. conducted a phase I pilot trial in which veliparib (ABT-888), an oral PARPi, was combined with temozolomide in mCRPC patients who have progressed after docetaxel chemotherapy [71]. Despite the promising preclinical activity, only two of the 25 evaluable patients achieved the primary endpoint of PSA response rate (decline ≥ 30 %), showing a very modest activity of the combination.
Higher expectations seem to be pinned on the combinations with hormonal drugs. Based on the emerging role of PARP1 in mediating transcriptional regulation by AR and ETS fusion protein [72, 73], two randomized, placebo-controlled phase II trials are evaluating the efficacy, safety and tolerability of PARPi (olaparib or veliparib) in combination with abiraterone acetate and prednisone in mCRPC (NCT01972217 and NCT01576172, respectively). In particular, at 2016 ASCO Annual Meeting, Hussain et al. presented the first results of a University of Chicago phase II consortium trial. On the assumption that co-targeting PARP and AR might be superior to AR inhibition, with ETS gene fusion as a predictive biomarker, they randomized 153 mCRPC patients to the combination of abiraterone acetate/prednisone and veliparib or to abiraterone alone and stratified them by ETS status. Although there was no statistically significant difference in PSA response rate (the primary end point; ≥ 50 % decline) between the two arms or by ETS status, the trend was in favor of experimental group (abiraterone plus veliparib) with regard to PSA response rate, objective response rate, therapy duration and median PFS. Interestingly, exploratory analysis suggested that patients with DNA damage repairs defects (25 %) had better and more durable responses, providing the foundation for an update of clinical data and further analysis in mCRPC preselected for DNA damage repair defects (NCT01576172) [74]. Likewise, the combination of enzalutamide and the PARPi niraparib is under investigation in the same subset of patients (NCT02500901).
Table 1 summarizes the completed phase I-II clinical trials and the selected ongoing studies of PARPi in prostate cancer.
4 Conclusions
Despite the development of novel effective therapeutic strategies, mCRPC remains a disease with a lethal course and a high biological and molecular heterogeneity. The thorough understanding of the genomic landscape has strengthened the idea that “synthetic lethality” of this tumor might be useful in cancer-drug discovery, and underlined that germline mutations in BRCA gene represent one of the strongest risk factors in developing prostate cancer. The molecular basis underlying the poor clinical outcomes of the BRCA2-associated prostate carcinomas is not yet entirely elucidated. A possible explanation can rely on inherent differences in tumor biology, given the more aggressive tumor behavior of germline BRCA2-mutated prostate cancers. For these reasons, routine-screening tests and recommendations for treatment of BRCA-associated prostate cancer should be individualized to define the risk associated with BRCA2 mutations and maximize personalized medicine protocols. With this purpose, Bancroft and colleagues performed for the first time an international, multicenter consortium evaluating the role of PSA-based selection in BRCA mutation carriers in order to identify prostate cancer in nonsymptomatic patients (the IMPACT study) [75, 76]. Two thousand, four hundred and eighty-one men aged 40–69 years with germline BRCA1/2 and a control group of men noncarriers were recruited; all patients underwent PSA testing at enrolment and those with PSA > 3 ng/mL (81 %) proceeding to biopsy. Respectively, more than two-thirds of the prostate cancer detected in the BRCA2 carriers and 61 % in the BRCA1 carriers were classified as intermediate or high risk, supporting previous reports of a more aggressive phenotype in this group and the potential use of PSA screening for BRCA carriers. Although there is a lack of statistically significant differences in prostate cancer detection rates between carriers and controls, the trend is clear and a longer follow-up may sustain these preliminary results. It is therefore clear that further studies designed to identify genetic markers useful in selection of patients at higher risk of prostate cancer are needed. The impressive response rates achieved with platinum agents and PARPi highlight their potential selective anti-tumor activity in BRCA-mutated prostate cancer patients, paving the way for a promising therapeutic approach. Trials analyzing the response of prostate cancer BRCA-carriers and molecular studies to identify the key drivers and therapeutic targets of this specific prostate cancer subgroup are imperative for highly tailored treatment management. Notably, not all BRCA carriers had a response to PARPi, probably due to pre-existing genetic resistance. In this context, secondary intragenic BRCA2 mutations may restore BRCA function and therefore homologous recombination, acting as the major mediator of acquired resistance to platinum compounds and PARPi [77, 78]. These findings suggest that PARPi alone may not be sufficient to control metastatic disease, shifting the focus on mutational signatures (genomic scars) as predictive biomarkers for response to treatment [79]. On the basis of all these evidences, further studies of PARPi in prostate cancer are strongly required to address critical issues, including the identification of predictive biomarkers of HR defects, the definition of biomarkers of efficacy beyond PSA and the deep understanding of mechanisms of treatment resistance. The optimal treatment strategy may require integrated approaches to overcome the tumor genetic complexity and avert the onset of resistance, such as concurrent use of multiple therapies.
References
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86. doi:10.1002/ijc.29210.
Galsky MD, Vogelzang NJ. Docetaxel-based combination therapy for castration-resistant prostate cancer. Ann Oncol. 2010;21(11):2135–44. doi:10.1093/annonc/mdq050.
Eisenberger MA, Walsh PC. Early androgen deprivation for prostate cancer? N Engl J Med. 1999;341(24):1837–8. doi:10.1056/NEJM199912093412409.
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351(15):1502–12. doi:10.1056/NEJMoa040720.
Petrylak DP, Tangen CM, Hussain MH, Lara Jr PN, Jones JA, Taplin ME, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med. 2004;351(15):1513–20. doi:10.1056/NEJMoa041318.
Bracarda S, Sisani M, Marrocolo F, Hamzaj A, Del Buono S, Altavilla A. Clinical implications for a treatment algorithm and differential indication to hormone therapy and chemotherapy options in metastatic castrate-resistant prostate cancer: a personal view. Expert Rev Anticancer Ther. 2014;14(11):1283–94. doi:10.1586/14737140.2014.965686.
de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376(9747):1147–54. doi:10.1016/S0140-6736(10)61389-X.
Fizazi K, Scher HI, Molina A, Logothetis CJ, Chi KN, Jones RJ, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012;13(10):983–92. doi:10.1016/S1470-2045(12)70379-0.
Ryan CJ, Smith MR, Fizazi K, Saad F, Mulders PF, Sternberg CN, et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2015;16(2):152–60. doi:10.1016/S1470-2045(14)71205-7.
Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367(13):1187–97. doi:10.1056/NEJMoa1207506.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371(5):424–33. doi:10.1056/NEJMoa1405095.
Beer TM, Armstrong AJ, Sternberg CN, Higano CS, Rathkopf DE, Loriot Y, et al. Enzalutamide (ENZA) in men with chemotherapy-Naive metastatic castration-resistant prostate cancer (mCRPC): Final analysis of the phase 3 PREVAIL study. J Clin Oncol 33, 2015 (suppl; abstr 5036).
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411–22. doi:10.1056/NEJMoa1001294.
Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fossa SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369(3):213–23. doi:10.1056/NEJMoa1213755.
van Soest RJ, van Royen ME, de Morree ES, Moll JM, Teubel W, Wiemer EA, et al. Cross-resistance between taxanes and new hormonal agents abiraterone and enzalutamide may affect drug sequence choices in metastatic castration-resistant prostate cancer. Eur J Cancer. 2013;49(18):3821–30. doi:10.1016/j.ejca.2013.09.026.
Bahl A, Masson S, Birtle A, Chowdhury S, de Bono J. Second-line treatment options in metastatic castration-resistant prostate cancer: a comparison of key trials with recently approved agents. Cancer Treat Rev. 2014;40(1):170–7. doi:10.1016/j.ctrv.2013.06.008.
Berger MF, Lawrence MS, Demichelis F, Drier Y, Cibulskis K, Sivachenko AY, et al. The genomic complexity of primary human prostate cancer. Nature. 2011;470(7333):214–20. doi:10.1038/nature09744.
Attard G, Swennenhuis JF, Olmos D, Reid AH, Vickers E, A’Hern R, et al. Characterization of ERG, AR and PTEN gene status in circulating tumor cells from patients with castration-resistant prostate cancer. Cancer Res. 2009;69(7):2912–8. doi:10.1158/0008-5472.CAN-08-3667.
Reid AH, Attard G, Ambroisine L, Fisher G, Kovacs G, Brewer D, et al. Molecular characterisation of ERG, ETV1 and PTEN gene loci identifies patients at low and high risk of death from prostate cancer. Br J Cancer. 2010;102(4):678–84. doi:10.1038/sj.bjc.6605554.
Mehra R, Han B, Tomlins SA, Wang L, Menon A, Wasco MJ, et al. Heterogeneity of TMPRSS2 gene rearrangements in multifocal prostate adenocarcinoma: molecular evidence for an independent group of diseases. Cancer Res. 2007;67(17):7991–5. doi:10.1158/0008-5472.CAN-07-2043.
Grasso CS, Wu YM, Robinson DR, Cao X, Dhanasekaran SM, Khan AP, et al. The mutational landscape of lethal castration-resistant prostate cancer. Nature. 2012;487(7406):239–43. doi:10.1038/nature11125.
Robinson D, Van Allen EM, Wu YM, Schultz N, Lonigro RJ, Mosquera JM, et al. Integrative clinical genomics of advanced prostate cancer. Cell. 2015;161(5):1215–28. doi:10.1016/j.cell.2015.05.001.
Leongamornlert D, Mahmud N, Tymrakiewicz M, Saunders E, Dadaev T, Castro E, et al. Germline BRCA1 mutations increase prostate cancer risk. Br J Cancer. 2012;106(10):1697–701. doi:10.1038/bjc.2012.146.
Kote-Jarai Z, Leongamornlert D, Saunders E, Tymrakiewicz M, Castro E, Mahmud N, et al. BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: implications for genetic testing in prostate cancer patients. Br J Cancer. 2011;105(8):1230–4. doi:10.1038/bjc.2011.383.
Myers CE, Feldman R, Abbott BL, Reddy SK, Castro M. Frequency of BRCA mutations and co-occurring alterations in prostate cancer. J Clin Oncol 34, 2016 (suppl 2S; abstr 289).
Kaufman B, Shapira-Frommer R, Schmutzler RK, Audeh MW, Friedlander M, Balmana J, et al. Olaparib monotherapy in patients with advanced cancer and a germline BRCA1/2 mutation. J Clin Oncol Off J Am Soc Clin Oncol. 2015;33(3):244–50. doi:10.1200/JCO.2014.56.2728.
Gudmundsdottir K, Ashworth A. The roles of BRCA1 and BRCA2 and associated proteins in the maintenance of genomic stability. Oncogene. 2006;25(43):5864–74. doi:10.1038/sj.onc.1209874.
Boulton SJ. Cellular functions of the BRCA tumour-suppressor proteins. Biochem Soc Trans. 2006;34(Pt 5):633–45. doi:10.1042/BST0340633.
Venkitaraman AR. Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell. 2002;108(2):171–82.
Thorslund T, West SC. BRCA2: a universal recombinase regulator. Oncogene. 2007;26(56):7720–30. doi:10.1038/sj.onc.1210870.
Yoshida K, Miki Y. Role of BRCA1 and BRCA2 as regulators of DNA repair, transcription, and cell cycle in response to DNA damage. Cancer Sci. 2004;95(11):866–71.
Martin AM, Blackwood MA, Antin-Ozerkis D, Shih HA, Calzone K, Colligon TA, et al. Germline mutations in BRCA1 and BRCA2 in breast-ovarian families from a breast cancer risk evaluation clinic. J Clin Oncol. 2001;19(8):2247–53.
Wooster R, Weber BL. Breast and ovarian cancer. N Engl J Med. 2003;348(23):2339–47. doi:10.1056/NEJMra012284.
Gudmundsson J, Johannesdottir G, Bergthorsson JT, Arason A, Ingvarsson S, Egilsson V, et al. Different tumor types from BRCA2 carriers show wild-type chromosome deletions on 13q12-q13. Cancer Res. 1995;55(21):4830–2.
Mersch J, Jackson MA, Park M, Nebgen D, Peterson SK, Singletary C, et al. Cancers associated with BRCA1 and BRCA2 mutations other than breast and ovarian. Cancer. 2015;121(2):269–75. doi:10.1002/cncr.29041.
Edwards SM, Kote-Jarai Z, Meitz J, Hamoudi R, Hope Q, Osin P, et al. Two percent of men with early-onset prostate cancer harbor germline mutations in the BRCA2 gene. Am J Hum Genet. 2003;72(1):1–12.
Agalliu I, Karlins E, Kwon EM, Iwasaki LM, Diamond A, Ostrander EA, et al. Rare germline mutations in the BRCA2 gene are associated with early-onset prostate cancer. Br J Cancer. 2007;97(6):826–31. doi:10.1038/sj.bjc.6603929.
Giusti RM, Rutter JL, Duray PH, Freedman LS, Konichezky M, Fisher-Fischbein J, et al. A twofold increase in BRCA mutation related prostate cancer among Ashkenazi Israelis is not associated with distinctive histopathology. J Med Genet. 2003;40(10):787–92.
Gallagher DJ, Gaudet MM, Pal P, Kirchhoff T, Balistreri L, Vora K, et al. Germline BRCA mutations denote a clinicopathologic subset of prostate cancer. Clin Cancer Res. 2010;16(7):2115–21. doi:10.1158/1078-0432.CCR-09-2871.
Schayek H, Haugk K, Sun S, True LD, Plymate SR, Werner H. Tumor suppressor BRCA1 is expressed in prostate cancer and controls insulin-like growth factor I receptor (IGF-IR) gene transcription in an androgen receptor-dependent manner. Clin Cancer Res. 2009;15(5):1558–65. doi:10.1158/1078-0432.CCR-08-1440.
Moro L, Arbini AA, Yao JL, di Sant’Agnese PA, Marra E, Greco M. Loss of BRCA2 promotes prostate cancer cell invasion through up-regulation of matrix metalloproteinase-9. Cancer Sci. 2008;99(3):553–63. doi:10.1111/j.1349-7006.2007.00719.x.
Tryggvadottir L, Vidarsdottir L, Thorgeirsson T, Jonasson JG, Olafsdottir EJ, Olafsdottir GH, et al. Prostate cancer progression and survival in BRCA2 mutation carriers. J Natl Cancer Inst. 2007;99(12):929–35. doi:10.1093/jnci/djm005.
Agalliu I, Gern R, Leanza S, Burk RD. Associations of high-grade prostate cancer with BRCA1 and BRCA2 founder mutations. Clin Cancer Res. 2009;15(3):1112–20. doi:10.1158/1078-0432.CCR-08-1822.
Narod SA, Neuhausen S, Vichodez G, Armel S, Lynch HT, Ghadirian P, et al. Rapid progression of prostate cancer in men with a BRCA2 mutation. Br J Cancer. 2008;99(2):371–4. doi:10.1038/sj.bjc.6604453.
Edwards SM, Evans DG, Hope Q, Norman AR, Barbachano Y, Bullock S, et al. Prostate cancer in BRCA2 germline mutation carriers is associated with poorer prognosis. Br J Cancer. 2010;103(6):918–24. doi:10.1038/sj.bjc.6605822.
Thorne H, Willems AJ, Niedermayr E, Hoh IM, Li J, Clouston D, et al. Decreased prostate cancer-specific survival of men with BRCA2 mutations from multiple breast cancer families. Cancer Prev Res. 2011;4(7):1002–10. doi:10.1158/1940-6207.CAPR-10-0397.
Castro E, Goh C, Olmos D, Saunders E, Leongamornlert D, Tymrakiewicz M, et al. Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol. 2013;31(14):1748–57. doi:10.1200/JCO.2012.43.1882.
Castro E, Goh C, Leongamornlert D, Saunders E, Tymrakiewicz M, Dadaev T, et al. Effect of BRCA mutations on metastatic relapse and cause-specific survival after radical treatment for localised prostate cancer. Eur Urol. 2015;68(2):186–93. doi:10.1016/j.eururo.2014.10.022.
Kim SH, Park WS, Yun SI, Joo J, Joung JY, Seo HK, et al. Overexpression of BRCA1 or BRCA2 in prostatectomy specimens is predictive of biochemical recurrence after radical prostatectomy. Histopathology. 2015. doi:10.1111/his.12809.
Hartwell LH, Szankasi P, Roberts CJ, Murray AW, Friend SH. Integrating genetic approaches into the discovery of anticancer drugs. Science. 1997;278(5340):1064–8.
Byrski T, Gronwald J, Huzarski T, Grzybowska E, Budryk M, Stawicka M, et al. Pathologic complete response rates in young women with BRCA1-positive breast cancers after neoadjuvant chemotherapy. J Clin Oncol. 2010;28(3):375–9. doi:10.1200/JCO.2008.20.7019.
Yang D, Khan S, Sun Y, Hess K, Shmulevich I, Sood AK, et al. Association of BRCA1 and BRCA2 mutations with survival, chemotherapy sensitivity, and gene mutator phenotype in patients with ovarian cancer. JAMA. 2011;306(14):1557–65. doi:10.1001/jama.2011.1456.
Tan DS, Rothermundt C, Thomas K, Bancroft E, Eeles R, Shanley S, et al. “BRCAness” syndrome in ovarian cancer: a case–control study describing the clinical features and outcome of patients with epithelial ovarian cancer associated with BRCA1 and BRCA2 mutations. J Clin Oncol. 2008;26(34):5530–6. doi:10.1200/JCO.2008.16.1703.
Beltran H, Tomlins S, Aparicio A, Arora V, Rickman D, Ayala G, et al. Aggressive variants of castration-resistant prostate cancer. Clin Cancer Res. 2014;20(11):2846–50. doi:10.1158/1078-0432.CCR-13-3309.
Sella A, Yarom N, Zisman A, Kovel S. Paclitaxel, estramustine and carboplatin combination chemotherapy after initial docetaxel-based chemotherapy in castration-resistant prostate cancer. Oncology. 2009;76(6):442–6. doi:10.1159/000217264.
Birtle AJ, Newby JC, Harland SJ. Epirubicin carboplatin and 5-fluorouracil (ECarboF) chemotherapy in metastatic hormone refractory prostate cancer. Br J Cancer. 2004;91(8):1472–6. doi:10.1038/sj.bjc.6602177.
Sternberg CN, Petrylak DP, Sartor O, Witjes JA, Demkow T, Ferrero JM, et al. Multinational, double-blind, phase III study of prednisone and either satraplatin or placebo in patients with castrate-refractory prostate cancer progressing after prior chemotherapy: the SPARC trial. J Clin Oncol. 2009;27(32):5431–8. doi:10.1200/JCO.2008.20.1228.
Scott CL, Swisher EM, Kaufmann SH. Poly (ADP-ribose) polymerase inhibitors: recent advances and future development. J Clin Oncol. 2015;33(12):1397–406. doi:10.1200/JCO.2014.58.8848.
Fong PC, Yap TA, Boss DS, Carden CP, Mergui-Roelvink M, Gourley C, et al. Poly(ADP)-ribose polymerase inhibition: frequent durable responses in BRCA carrier ovarian cancer correlating with platinum-free interval. J Clin Oncol. 2010;28(15):2512–9. doi:10.1200/JCO.2009.26.9589.
Cheng HH, Pritchard CC, Boyd T, Nelson PS, Montgomery B. Biallelic inactivation of BRCA2 in platinum-sensitive metastatic castration-resistant prostate cancer. Eur Urol. 2015. doi:10.1016/j.eururo.2015.11.022.
Ame JC, Spenlehauer C, de Murcia G. The PARP superfamily. BioEssays News Rev Mol Cell Dev Biol. 2004;26(8):882–93. doi:10.1002/bies.20085.
Dantzer F, de La Rubia G, Menissier-De Murcia J, Hostomsky Z, de Murcia G, Schreiber V. Base excision repair is impaired in mammalian cells lacking Poly(ADP-ribose) polymerase-1. Biochemistry. 2000;39(25):7559–69.
Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature. 2005;434(7035):913–7. doi:10.1038/nature03443.
Ashworth A. A synthetic lethal therapeutic approach: poly(ADP) ribose polymerase inhibitors for the treatment of cancers deficient in DNA double-strand break repair. J Clin Oncol. 2008;26(22):3785–90. doi:10.1200/JCO.2008.16.0812.
Tutt AN, Lord CJ, McCabe N, Farmer H, Turner N, Martin NM, et al. Exploiting the DNA repair defect in BRCA mutant cells in the design of new therapeutic strategies for cancer. Cold Spring Harb Symp Quant Biol. 2005;70:139–48. doi:10.1101/sqb.2005.70.012.
Brody LC. Treating cancer by targeting a weakness. N Engl J Med. 2005;353(9):949–50. doi:10.1056/NEJMcibr052331.
Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434(7035):917–21. doi:10.1038/nature03445.
Fong PC, Boss DS, Yap TA, Tutt A, Wu P, Mergui-Roelvink M, et al. Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med. 2009;361(2):123–34. doi:10.1056/NEJMoa0900212.
Mateo J, Carreira S, Sandhu S, Miranda S, Mossop H, Perez-Lopez R, et al. DNA-repair defects and olaparib in metastatic prostate cancer. N Engl J Med. 2015;373(18):1697–708. doi:10.1056/NEJMoa1506859.
Sandhu SK, Schelman WR, Wilding G, Moreno V, Baird RD, Miranda S, et al. The poly(ADP-ribose) polymerase inhibitor niraparib (MK4827) in BRCA mutation carriers and patients with sporadic cancer: a phase 1 dose-escalation trial. Lancet Oncol. 2013;14(9):882–92. doi:10.1016/S1470-2045(13)70240-7.
Hussain M, Carducci MA, Slovin S, Cetnar J, Qian J, McKeegan EM, et al. Targeting DNA repair with combination veliparib (ABT-888) and temozolomide in patients with metastatic castration-resistant prostate cancer. Investig New Drugs. 2014;32(5):904–12. doi:10.1007/s10637-014-0099-0.
Brenner JC, Ateeq B, Li Y, Yocum AK, Cao Q, Asangani IA, et al. Mechanistic rationale for inhibition of poly(ADP-ribose) polymerase in ETS gene fusion-positive prostate cancer. Cancer Cell. 2011;19(5):664–78. doi:10.1016/j.ccr.2011.04.010.
Schiewer MJ, Goodwin JF, Han S, Brenner JC, Augello MA, Dean JL, et al. Dual roles of PARP-1 promote cancer growth and progression. Cancer Dis. 2012;2(12):1134–49. doi:10.1158/2159-8290.CD-12-0120.
Hussain M, Daignault S, Twardowski P, Albany C, Stein MN, Kunju LP, et al. Co-targeting androgen receptor (AR) and DNA repair: a randomized ETS gene fusion-stratified trial of abiraterone + prednisone (Abi) +/− the PARP1 inhibitor veliparib for metastatic castration-resistant prostate cancer (mCRPC) patients (pts) (NCI9012)--a University of Chicago phase II consortium trial. J Clin Oncol 34, 2016 (suppl; abstr 5010).
Bancroft EK, Page EC, Castro E, Lilja H, Vickers A, Sjoberg D, et al. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study. Eur Urol. 2014;66(3):489–99. doi:10.1016/j.eururo.2014.01.003.
Bancroft EK, Eeles RA. Corrigendum to “targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study” [Eur Urol 2014;66:489–99]. Eur Urol. 2015;67(6):e126. doi:10.1016/j.eururo.2014.12.001.
Sakai W, Swisher EM, Karlan BY, Agarwal MK, Higgins J, Friedman C, et al. Secondary mutations as a mechanism of cisplatin resistance in BRCA2-mutated cancers. Nature. 2008;451(7182):1116–20. doi:10.1038/nature06633.
Edwards SL, Brough R, Lord CJ, Natrajan R, Vatcheva R, Levine DA, et al. Resistance to therapy caused by intragenic deletion in BRCA2. Nature. 2008;451(7182):1111–5. doi:10.1038/nature06548.
Helleday T, Eshtad S, Nik-Zainal S. Mechanisms underlying mutational signatures in human cancers. Nat Rev Genet. 2014;15(9):585–98. doi:10.1038/nrg3729.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of Interest
Alessandra Modena, Roberto Iacovelli, Aldo Scarpa, Matteo Brunelli, Chiara Ciccarese, Emanuela Fantinel, Davide Bimbatti, Francesco Massari, Guido Martignoni, and Giampaolo Tortora declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Modena, A., Iacovelli, R., Scarpa, A. et al. Investigating BRCA Mutations: A Breakthrough in Precision Medicine of Castration-Resistant Prostate Cancer. Targ Oncol 11, 569–577 (2016). https://doi.org/10.1007/s11523-016-0450-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-016-0450-9