Abstract
Rotator cuff (RC) tears have a high prevalence, and RC repair surgery is frequently performed. Evaluation of deltoid activation has been reported as an easy to measure proxy for RC functionality. Our goal was to test the success of RC repair in restoring muscle function, by assessing deltoid activation with varying arm abduction moment loading tasks in controls and in RC tear patients before and 1 year after RC repair. Averaged rectified electromyography recordings (rEMG) of the deltoid during 2-s isometric arm abduction tasks were assessed in 22 controls and 33 patients before and after RC repair. Changes in deltoid activation as a response to increased arm abduction moment loading (large vs. small moment), without changing task force magnitude, were expressed as: R = (rEMGLarge − rEMGSmall)/(rEMGLarge + rEMGSmall), where R > 0 indicates an increase in muscle activation with larger moment loading. In controls, a significant increase in deltoid activation was observed with large abduction moment loading: R = 0.11 (95 % CI 0.06–0.16). In patients, R was larger: 0.20 (95 % CI 0.13–0.27) preoperatively and 0.16 (95 % CI 0.09–0.22) postoperatively. Increased compensatory deltoid activation was found in pre-operative RC tear patients. The post-operative decrease in compensatory deltoid activation, although not significant, could indicate (partially) restored RC function in at least some patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Rotator cuff (RC) tears have a high prevalence and are often diagnosed in patients with shoulder symptoms [17, 22]. RC repair surgery is a frequently performed surgical procedure for the treatment of symptomatic RC tears [19]. However, there are many uncertainties with respect to RC tears and their treatment: 54 % of the population over 60 years have asymptomatic RC tears [21], only around 50 % progress to symptomatic tears within 2–3 years [14, 30], treatment results are highly variable [19], and the functional status and recovery of the RC and other shoulder muscles after RC repair surgery has been scarcely investigated [6].
Insight into shoulder muscle function is crucial to gain understanding of these heterogeneities and to assess whether RC repair restores shoulder muscle function. It is, however, hard to quantify the effect of cuff repair surgery on the abduction function of the RC. Assessing the activation of the supraspinatus muscle and the superior portions of the infraspinatus and the subscapularis muscles requires invasive fine-wire electromyography (EMG). This clinically hampers measurements and functionally requires additional assumptions about the contribution of the active muscles to the abduction forces onto the humerus. The latter is specifically complex in case of RC tears and (incomplete) surgical repair.
In a study assessing muscle functions in RC tear patients and healthy controls, Steenbrink et al. [27] demonstrated a larger increase in deltoid (DE) activation as a response to increased arm abduction moment loading in patients compared to controls. They suggested that in RC tear patients, the deltoid compensates for lost RC function, as has been reported by others as well [9, 10, 15, 18, 20, 24]. As a compensator for lost RC function, assessing deltoid activity is a potential proxy for easy indirect assessment of the functional status of the deeply positioned RC muscles. In the current study, we applied this previously introduced non-invasive experimental method to indirectly test RC function by assessing the activation of the deltoid muscles [27].
Our study goal was to quantify the contribution of the RC to arm abduction in controls and cuff tear patients before and after surgical cuff repair, by assessment of changes in deltoid activation in response to variations in arm abduction moment loading. Our hypotheses were that (1) an increase in arm abduction moment loading leads to a relative increase in deltoid activation in all subjects; (2) this relative increase will be larger in RC tear patients before surgery (compensatory deltoid activation) compared to controls; (3) RC repair leads to a decrease in compensatory deltoid activation compared to pre-operative measurements; and (4) RC repair leads to a decrease in compensatory deltoid activation, more in the range of control subjects’ measurements.
2 Materials and methods
2.1 Subjects
From March 2010 until April 2011, RC tear patients who were planned for surgical RC repair by one of two experienced shoulder surgeons of two participating hospitals (Medical Center Haaglanden, The Hague, The Netherlands; Leiden University Medical Center, Leiden, The Netherlands) were contacted for inclusion in the current study. Inclusion criteria were as follows: full-thickness supraspinatus tear proven with magnetic resonance imaging (MRI-arthrogram) and one or more of the following criteria present, aside from a positive Neer impingement test, a positive Hawkins test and diffuse unilateral anterosuperior shoulder pain for >3 months: pain with arm abduction, retroflexion and/or internal rotation (e.g., closing the door, putting on jacket); pain with overhead activities; pain at night or incapable of lying on the shoulder; classic painful arc; positive Yocum test; positive full or empty can test. Patients were included for post-operative evaluation unless any other causes for shoulder symptoms than RC tears were identified during surgery. Additionally, RC status was evaluated 1 year after surgery using ultrasound. Inclusion criteria for healthy subjects (controls) were: between 20 and 50 years old (in order to limit the chance of including subjects with asymptomatic RC tears), no present shoulder complaints, and no history of medically treated shoulder complaints.
Exclusion criteria for all subjects were: insufficient Dutch language skills or no informed consent, presence of physical problems influencing muscle activation and arm mobility (other than RC tear in the patient group), any form of inflammatory arthritis of the shoulder, glenohumeral (GH) or symptomatic acromioclavicular osteoarthritis, a history of surgical interventions of the shoulder, clinical signs of cervical radiculopathy, GH instability, or frozen shoulder syndrome (<90° of passive abduction and external rotation). After standard radiographs and MRI-arthrogram evaluation, patients were excluded in case of subscapularis or teres minor tendon pathologies, calcific tendonitis, intra-articular or bony lesions (Hill Sachs, (old) fractures, tumors), labrum abnormalities, capsular or ligamentous tears/avulsions, superior labral tear from anterior to posterior (SLAP lesion), pulley lesion, biceps tendinitis or tear, os acromiale, or cartilage lesions.
The patient group was clinically evaluated before surgery and 1 year after surgery, using the Western Ontario Rotator Cuff index (WORC) [5, 12, 29] and the Constant Score (CS) [2]. RC status (re-tear yes/no) 1 year after surgery was assessed with ultrasound.
All stages of this study are in compliance with the declaration of Helsinki, written informed consent was obtained from all participants, and the local medical ethics review board (METC, Leiden University Medical Center) approved the study.
2.2 Surgical procedure
RC repair surgery was performed by either one of two participating experienced orthopedic shoulder surgeons using an all-arthroscopic (AA) or mini-open (MO) technique according to the surgeon’s preference. There is no difference in clinical outcome and complication rate between the AA and MO procedures [28]. All patients were operated under general anesthesia in lateral decubitus position with the arm held in a three-point shoulder distraction device. In both procedures, the edges of the tear are debrided, and the insertion site for the suture anchors on the major tubercle is prepared using a shaver. A suture bridge repair construct is applied, using 2–4 anchors depending on the size of the tear, to secure the tendons with a 5.5-mm CorkScrew (Arthrex, Naples, Florida) in the medial row and a knotless 3.5-mm Bio-PushLock anchor (Arthrex, Naples, Florida) in the lateral row. In case of a longitudinal extension of the tear, the margin convergence technique was applied first. After wound closure, a standard dressing is applied, and the arm is placed in a sling for 6 weeks.
There was a standard postoperative rehabilitation protocol for all patients, under supervision of a local physical therapist. Active exercises of the elbow, wrist, and hand were encouraged from the first day after surgery. The rehabilitation protocol consisted of active assisted abduction in the scapular plane limited to 70° and 0° of external rotation in the first 4–6 weeks, as tolerated. After this, active range of motion exercises were started. When the patient was pain free, isotonic strengthening exercises were initiated.
2.3 Experimental setup
In order to compare EMG over muscles, subjects, and time, normalization with maximal activation increases the reliability of the measurement [11]. However, assessing maximum voluntary contraction in pre- and post-intervention patients may not be reliable. An alternative is to normalize EMG over two isometric but antagonist tasks, resulting in an activation ratio (AR) [26]. This concept, applied for normalizing EMG of the deltoid muscle under two contrasting arm loading conditions, stratified for force magnitude and force direction but at different locations at the humerus (i.e., different moment loading conditions), previously resulted in a deltoid moment loading response which was shown to be sensitive for patients with RC lesions: patients with a proven RC lesion had a larger increase in deltoid activation in response to increased arm abduction moment loading compared to healthy subjects [27]. We applied the same method to qualify the contribution of supraspinatus during abduction for each subject, based on changes in the activation of the deltoid (DE) as a response to increasing the external force moment arm of an abduction task force of constant magnitude. The applied setup has also been applied and validated in various other shoulder EMG studies [3, 4, 16, 23, 26]. Controls were evaluated once and RC patients were evaluated in two sessions: in the month before a planned RC repair procedure and in the second year after RC repair.
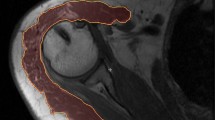
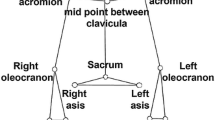
Subjects were seated with the affected (patients) or dominant (controls) arm fully suspended in a splint that was attached to a force sensor (AMTI-300, Advanced Mechanical Technology Inc., Wavertown, MA, USA). The two translational degrees of freedom perpendicular to the humerus were fixed, and the longitudinal translation and three rotational degrees of freedom were released (Fig. 1). The splint allowed for variation in point of force application (force sensor) alongside the humerus. In this way, external moment loading can be varied, without changing task force magnitude. Subjects were instructed to maintain the arm in a standardized position during the experiment: arm elevation of 60°, 30° of horizontal abduction with the humerus 45° internally rotated, as applied in previous studies with this setup [3, 4, 16, 23, 26, 27]. Arm position was visually controlled for by markings on the experimental setup. The arm was fully supported for gravity in this specific condition, so subjects were able to maintain the arm this way without any effort.
Setup for isometric tasks with a small or large moment arm of an external task force. In the current study, we applied abduction tasks. For these tasks, subjects had to move a cursor (red dot) to a target (blue dot) randomly representing each of seven, respectively, applied equidistant abduction directions, 15° apart, ranging from pressing arm straight up (0°, a) to pushing the arm sideward (90°, b). The point of force application, i.e., where the force sensor is attached to the splint, can be varied in order to realize large moments (a) or small moments tasks (b), while keeping the exerted task force constant (color figure online)
Subjects performed isometric abduction tasks perpendicular to the longitudinal axis of the humerus. By applying forces onto the force sensor, subjects could control a visually displayed cursor (red dot) that had to be moved to randomly appearing targets on a computer screen. Each target represented a force vector of constant magnitude in one of seven equidistant abduction directions (15° apart), away from the midline or sagittal plane of the body and in the scapular plane, ranging from 0° (push arm straight up) to 90° (push arm sideward; Fig. 1). Subjects held the cursor within each target area for 2 s. Force magnitude was determined individually during each session and set at 10 N below the maximum level at which subjects could perform the 2-s tasks, as recommended previously, with a minimum of 10 N to secure sufficient signal over noise ratio [25]. After practice rounds, two task trials were performed: one trial with the point of force application at about 10 cm distally from the GH joint, i.e., the ‘small moment arm’ condition, and one trial with the point of force application approximately 25 cm distally from the GH joint, i.e., the ‘large moment arm’ condition. Note that within each session, the force magnitude was constant for the two trials. In order to prevent fatigue and other carry over effects, there was a minimal 15-s rest period between the tasks and a period of 5 min between the two trials.
Activity of the main deltoid muscle parts (anterior: DA; medial: DM; posterior: DP) were recorded with a bi-polar surface EMG system (DelSys Bagnoli-16, Boston, MA, USA; DE-2.1 single differential electrodes, inter-electrode distance 10 mm, bandwidth 20–450 Hz). EMG electrodes were applied after palpation of the muscle bellies, while the subjects were positioned in the experimental setup. The skin was shaved where needed, scrubbed with skin preparation gel (skinPure, Nihon Kohden, Tokyo, Japan), and cleansed using alcohol pads.
2.4 Data processing
The simultaneously recorded 2-s force and EMG signals for each force task were analog-to-digitally converted (2,000 Hz). After subtracting EMG rest activity, the EMG recordings were rectified and averaged for each force task resulting in seven aEMG observations for each muscle during each trial. From these seven observations, we obtained a single activation measure for each muscle part by averaging aEMGs, but because the different deltoid muscle(part)s are not equally responsive for all seven force directions, we averaged the aEMGs over only a selection of the force directions, depending on the involved deltoid muscle part. In order to determine the most prominent activation directions of the muscle parts, we applied the previously reported principal action (PA) method [3, 16, 23]. This PA is the experimentally determined task direction in which the (EMG of the) muscle is most active. We selected the force task directions within ±45° around the PA of each individual muscle part and averaged the related aEMGs accordingly. The resultant rEMGs were normalized for each subject and muscle using a Muscle Ratio (R Muscle, based on the Activation Ratio [27]), where muscle activation changes between the small and large moment trials (rEMGLarge − rEMGSmall) are divided by the sum of rEMGs of both trials (rEMGLarge + rEMGSmall) (Eq. 1):
This R Muscle enables easy interpretation and inter- and intra-subject comparisons of EMG recordings: R Muscle values greater than 0 indicate a relative increase in the activation of the assessed muscle with larger abduction moment loading. Additionally, by assessing normalized relative deltoid EMG in response to increased moment loading instead of, e.g., raw EMG recordings or rEMG, inter individual variability from volume conductor effects, EMG equipment settings, subcutaneous fat tissue, and skin preparation are prevented. For the statistical analysis, it should be noted that the statistical distribution of R Muscle around 0 [representing the zero-hypothesis (H0): no difference between rEMGLarge and rEMGSmall] is symmetrically distributed [−1, 1], but conservatively biased toward 0. This is in contrast to more general normalizations relative to either rEMGLarge or rEMGSmall, which are asymmetrically distributed around H0 = 0: [0, inf.], respectively, and biased toward greater values than 0, which is more prone finding false-positive differences between rEMGLarge and rEMGSmall.
2.5 Statistical analysis
Mean Muscle Ratios (R Muscle), corresponding standard deviations (SD), and 95 % confidence intervals (95 % CI) for R DA, R DM, and R DP were calculated. Additionally, R DELT was calculated for each subject and trial, by averaging the R Muscle’s of all three deltoid muscle parts. Muscle Ratios greater than zero (R Muscle > 0) indicate an increase in muscle activation with large moment arm loading. R Muscle’s with 95 % CIs excluding 0 can be regarded as significant changes in muscle activation in response to the changes in arm moment loading.
The average R Muscle outcomes were compared between (a) controls and pre-operative RC tear patients using unpaired t tests, (b) paired t test for pre- and post-operative RC tear patients without a re-tear, and (c) unpaired t tests comparing post-operative RC tear patients and controls. Additionally, mean patients’ pre-operative and post-operative WORC and CS were assessed and compared using paired t tests.
In order to take into account interactions between Muscle Ratios and to assess all recorded data in a single analysis, we performed a mixed model analysis with Muscle Ratio as dependent variable and as independent variables: disease status, pre-/post-surgery, muscle (DA, DP, DM), and the interaction term between muscle and disease status. A random effect per subject was included to take into account repeated measures in the patients.
IBM SPSS Statistics 20.0 for windows (IBM, Armonk, NY, USA) was used for all statistical analyses.
3 Results
3.1 Patients
Twenty-one controls and 33 patients with symptomatic RC tears were included in the study. Average age of the controls was 26 years (range 20–43) and 10 (45.5 %) were male. All were able to fulfill the experimental tasks without any shoulder symptoms. For patients, mean age was 61 years (range 46–75) and 18 (54.5 %) were male. Mean pre-op WORC was 51.9 points (SD = 21.8), and mean pre-op CS was 56.8 (SD = 15.5).
With regard to the pre-operative measurements in patients, five were unable to perform the experimental tasks due to pain and/or coordinative problems, and in three patients, there were technical problems. For the post-operative measurements, four patients had a re-tear, three patients did not want to participate, two could not be contacted anymore, two patients ultimately did not undergo surgery because of decreased symptoms, and one patient could not perform the experimental tasks due to pain.
Of the 25 patients completing all tasks before surgery, 18 completed all tasks after successful surgery (no re-tear) with an average follow-up of 1.2 years (range 1.0–1.6) and were available for paired pre-operative versus post-operative analyses. In these patients, mean post-operative WORC improved with 25.5 points (95 % CI 15.6–35.3) to 76.1 and mean CS with 29.2 points (95 % CI 18.9–39.5) to 83.1.
3.2 rEMG during small and large abduction moment tasks in controls and cuff tear patients
The deltoid muscle(part)s are not equally responsive for all seven force directions, and we averaged the aEMGs of each muscle part over only a selection of the force directions, depending on the muscle involved, based on the principal action (PA) of the deltoid muscle(part)s. The average PA directions were PADA = −10° (SEM = 1.6), PADM: 44° (SEM = 2.6), and PADP: 83° (SEM = 3.2). There were no significant differences between patient and control PAs (data not shown). Consequently, the selection of force directions for DA ranged between −55° and 35° [i.e., 0°, 15°, and 30° force tasks (three force tasks/force directions)], for DM between −1° and 88° [i.e., 0°, 15, 30°, 45°, 60°, and 75° force tasks (six tasks)], and for DP between 38° and 128° [i.e., 45°, 60°, 75°, and 90° force tasks (four tasks)]. Resulting weighting factors for the average DELT calculation were three for DA, six for DM, and four for DP.
In controls, there was an average relative increase in deltoid muscle activation for large abduction moment loading, depicted in R Muscle > 0 for all separate muscle parts resulting in an average deltoids (DELT) increase of R DELT = 0.11 (95 % CI 0.06–0.16). This increase was significant for DA, DM, and DELT, with corresponding 95 % CIs excluding 0 (Table 1). In pre-operative patients, there was a significant increase for DA, DM and DP with an average DELT increase of R DELT = 0.17 (95 % CI 0.10–0.23) for DELT. On average, patient deltoid Ratios were larger than the deltoid Ratios in the control group for all individual muscle parts in our data, where larger Ratios indicate a larger (compensatory) increase in deltoid activation in a response to the increase in abduction moment loading (Table 1; Fig. 2). When comparing data of controls and patients with both successful pre- and post-operative measurements available (n = 18), pre-operative DA, DP and DELT Ratios were significantly larger in patients compared to controls (Fig. 2).
Relative increase in each of the deltoid muscle parts with increased arm abduction moment loading, displayed in mean R Muscle’s with 95 % CIs, for controls and RC tear patients before and 1 year after surgical RC repair. Before surgery, RC tear patients have on average a larger increase in deltoid activation with increased arm abduction loading compared to controls (statistically significant for DA, DP, and DELT). One year after RC repair, relative DA and DM activations in response to increased arm abduction were lower and no longer statistically significantly higher than control values. This could be due to a decrease in the need for DA and DM to compensate for lost RC function during abduction tasks as performed in a setup with an abduction-anteflexion arm position
After surgery, the average deltoid Ratios in patients decreased for DA, DM and DELT, but paired analyses indicated no statistically significant differences with pre-operative measurements (Table 2; Fig. 2). Comparing the deltoid Ratios of the post-operative group to controls now resulted in smaller mean differences between these two groups for DA, DM and DELT: 0.027 for DA (p = 0.64), −0.03 for DM (p = 0.55) and 0.04 (p = 0.23) for DELT (Fig. 2). For DP, a significant difference between the two groups remained: 0.128 (p = 0.04).
In mixed model analyses, effect size of disease status was −0.10 (95 % CI 0.00–0.20, p = 0.06). Estimated effect size of surgery on Muscle Ratio was negative (average decrease of R to healthy values) but not significant: −0.03 (95 % CI −0.08 to 0.03, p = 0.29). Effects of muscle [DA, DM, DP] and interaction terms were statistically not significant, although the effect of surgery on specifically the Muscle Ratio of the medial deltoid appeared relevant: −0.09 (95 % CI −0.21 to 0.03, p = 0.13).
4 Discussion and conclusions
With the increasing debate on RC tears and its (surgical) treatment, we need objective outcome measures and more insight in the (biomechanical) principles of RC disease. In this study we aimed at discriminating pre- and postoperative RC tear patients from controls and illustrate the potential biomechanical effect and functional restoration of RC repair by quantifying the compensating activation of the deltoids in response to a changing arm abduction loading moments.
The results show firstly, that an increase in arm abduction moment loading, with a constant task force magnitude, is accompanied by a significant increase in deltoid muscle activation in both controls and RC tear patients. With respect to our first hypothesis, we may conclude that the deltoids are responsive for the experimental design of glenohumeral moment increase, as has been shown previously. Secondly, the increase in deltoid activation was largest in pre-operative RC tear patients in our data, as depicted in significantly larger average Muscle Ratios compared to controls (Fig. 2). In mixed model analysis, there was a large and relevant effect of disease status on Muscle Ratio. This suggests that the deltoid muscle compensates for lost RC function in RC tear patients with shoulder symptoms, as has been previously reported [9, 10, 15, 18, 20, 24, 27]. Thirdly, the main question of our study was whether RC repair surgery would indeed result in a partly or full normalization of cuff function, which would be observed in a normalization of the deltoid moment response. For this question our experiment was not conclusive. One year after RC repair surgery, average Muscle Ratios of the deltoid muscle parts in patients appeared to decrease toward the controls’ values, which would suggest that RC repair surgery restores (at least part of) the function of the RC. However, the average decreases in deltoid activation were relatively small and not statistically significant compared to pre-operative measurements. On the other hand, the post-operative Muscle Ratios of the deltoids did not significantly differ from the control group, where pre-operative Muscle Ratios did significantly differ from the control group (Fig. 2). This could indicate that surgery did result in a normalization in some patients, at least for the anterior and medial deltoid parts. Lastly, with regards to clinical results, the patient group significantly improved 1 year post-surgery on both the WORC and Constant Score.
Symptoms of RC tears, most often supraspinatus tears, are generally most apparent with active arm abduction. Nevertheless, specifically the deltoid is regarded as an abduction moment generator [1, 8, 13]. Hence, increasing arm abduction moment loading (while keeping exerted force magnitude constant) predominantly leads to an increase in deltoid activity [27]. This is supported by the results of our study. In case of RC tears, lost supraspinatus function can be partially compensated by the deltoid, specifically with regards to its function in generating arm abduction moments [7, 9, 10, 15, 18, 20, 24, 27]. Confirmatory to the latter is that previous studies have shown that knockout of the supraspinatus, e.g., by a tear or nerve block, coincided with increased deltoid activation [7, 9, 15, 18, 24, 27]. In support of this, we found larger deltoid Muscle Ratios in RC tear patients compared to controls (Fig. 2).
The posterior deltoid differed most between patients and controls and did not seem to respond to surgery. The posterior deltoid may potentially reflect the infraspinatus abduction portion more than the supraspinatus muscle. The quality of repair, differentiated over the supraspinatus and the infraspinatus may differ in advance on the supraspinatus, and may thus reflect in our results. Furthermore, it is plausible that the stabilizator function of the RC is sub-optimal in pre-operative and post-operative patients, requiring more activity of other muscles (including DP) for glenohumeral stabilization.
Hence, we found a significant increase in deltoid activation for controls and pre-operative patients with increased abduction moment loading, significantly more deltoid activation in pre-operative patients versus controls, large effects of disease status and surgery on R Muscle, and an average increase in deltoid activation with large moments that was substantially larger for all muscle parts in pre-operative patients and lower for post-operative patients. However, we were unable to find significant differences with most t tests. The interpretation of these tests should take into account the relatively high value of R Muscle for DP in patients (see above) and the large measurement SDs. Patient SDs could have been larger due to, e.g., variations in the severity of symptoms and cuff tear size. Furthermore, two patients showed low pre-operative R Muscle’s and high post-operative R Muscle’s, contrary to the other subjects. There were no clinical or recording abnormalities for these patients, but when removing these outliers from the analyses, there was a significant decrease in DA activation after surgery (data not shown).
There are some limitations that need to be taken into account when interpreting our results. Firstly, deltoid activation might be simply more increased in pre-operative patients due to pain. Pain was less 1 year after surgery and this could explain the decrease of the post-operative deltoid compensatory activation. However, suprascapular knockout studies in healthy subjects and model simulation studies have also found increased deltoid compensatory activation as a response to decreased RC functioning (e.g., nerve blocks), i.e., without pain playing a role [7, 15, 18, 24]. Secondly, there was a significant age difference between the controls and the patients, as we wanted to include controls with a low chance of asymptomatic cuff tears. Although age can influence EMG recordings, it is plausible that age has no influence on the relative increase in deltoid activation with larger moment arms, such as expressed in Muscle Ratios. In linear regression analyses (data not shown) for pre-operative and control R Muscle of each muscle and the combined DELT as dependent variables and with disease status and age as independent variables, we found no statistically significant or relevant age effects for DA, DM, DP, and DELT. However, it is recommendable to further assess age effects in a single group (either with or without pathology) with a broader age range. Lastly, as stated in the introduction, RC tear patients form a heterogeneous population. We used strict eligibility inclusion criteria and extensive investigations, including MRI-arthrograms, and patients were selected by two experienced orthopedic surgeons specialized in shoulders in order to include a homogeneous patient group in whom it is highly likely the shoulder symptoms are caused by the observed RC tear. Currently, there are no better methods to select these patients or organize them in potential subgroups. Biomechanical testing of repair in these groups seems to be even more difficult.
Concluding, where the deltoid seems to compensate for lost RC function in cuff tear patients, this increased deltoid activation appears partially reduced 1 year after surgical RC cuff repair, which would suggest restoration of RC function. However, where we had sufficient power to discriminate pre-operative patients and controls and with the on average smaller and statistically insignificant differences between post-operative patients and controls, pre- versus post-operative differences were relatively small and associated statistics were not conclusive. This might be due to, e.g., limited accuracy or precision of the applied experimental setup, variability in subjects, or it is the result of actually only limited or variable restoration of RC function after surgical repair. Further research is needed to investigate whether applying an alternative experimental setup, e.g., with the arm alongside the body and abduction tasks in a single direction, leads to more accuracy, better responsiveness, and similar results.
References
Ackland DC, Pak P, Richardson M, Pandy MG (2008) Moment arms of the muscles crossing the anatomical shoulder. J Anat 213:383–390. doi:10.1111/j.1469-7580.2008.00965.x
Constant CR, Gerber C, Emery RJ, Sojbjerg JO, Gohlke F, Boileau P (2008) A review of the constant score: modifications and guidelines for its use. J Should Elbow Surg 17:355–361. doi:10.1016/j.jse.2007.06.022
de Groot JH, Rozendaal LA, Meskers CG, Arwert HJ (2004) Isometric shoulder muscle activation patterns for 3-D planar forces: a methodology for musculo-skeletal model validation. Clin Biomech (Bristol, Avon) 19:790–800. doi:10.1016/j.clinbiomech.2004.05.013
de Groot JH, van de Sande MA, Meskers CG, Rozing PM (2006) Pathological Teres major activation in patients with massive rotator cuff tears alters with pain relief and/or salvage surgery transfer. Clin Biomech (Bristol, Avon) 21(Suppl 1):S27–S32. doi:10.1016/j.clinbiomech.2005.09.011
de Witte PB, Henseler JF, Nagels J, Vlieland TPV, Nelissen RG (2012) The Western Ontario rotator cuff index in rotator cuff disease patients: a comprehensive reliability and responsiveness validation study. Am J Sports Med 40:1611–1619. doi:10.1177/0363546512446591
Fokter SK, Cicak N, Skorja J (2003) Functional and electromyographic results after open rotator cuff repair. Clin Orthop Relat Res:121–130. doi:10.1097/01.000093903.12372.3f
Gerber C, Blumenthal S, Curt A, Werner CM (2007) Effect of selective experimental suprascapular nerve block on abduction and external rotation strength of the shoulder. J Should Elbow Surg 16:815–820. doi:10.1016/j.jse.2007.02.120
Gorelick ML, Brown JM (2007) Mechanomyographic assessment of contractile properties within seven segments of the human deltoid muscle. Eur J Appl Physiol 100:35–44. doi:10.1007/s00421-007-0397-8
Hansen ML, Otis JC, Johnson JS, Cordasco FA, Craig EV, Warren RF (2008) Biomechanics of massive rotator cuff tears: implications for treatment. J Bone Joint Surg Am 90:316–325. doi:10.2106/JBJS.F.00880
Hawkes DH, Alizadehkhaiyat O, Kemp GJ, Fisher AC, Roebuck MM, Frostick SP (2012) Shoulder muscle activation and coordination in patients with a massive rotator cuff tear: an electromyographic study. J Orthop Res 30:1140–1146. doi:10.1002/jor.22051
Keenan KG, Farina D, Maluf KS, Merletti R, Enoka RM (2005) Influence of amplitude cancellation on the simulated surface electromyogram. J Appl Physiol 98:120–131. doi:10.1152/japplphysiol.00894
Kirkley A, Alvarez C, Griffin S (2003) The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med 13:84–92. doi:10.1097/00042752-200303000-00004
Kuechle DK, Newman SR, Itoi E, Morrey BF, An KN (1997) Shoulder muscle moment arms during horizontal flexion and elevation. J Should Elbow Surg 6:429–439. doi:10.1016/S1058-2746(97)70049-1
Mall NA, Kim HM, Keener JD, Steger-May K, Teefey SA, Middleton WD, Stobbs G, Yamaguchi K (2010) Symptomatic progression of asymptomatic rotator cuff tears: a prospective study of clinical and sonographic variables. J Bone Joint Surg Am 92:2623–2633. doi:10.2106/JBJS.I.00506
McCully SP, Suprak DN, Kosek P, Karduna AR (2007) Suprascapular nerve block results in a compensatory increase in deltoid muscle activity. J Biomech 40:1839–1846. doi:10.1016/j.jbiomech.2006.07.010
Meskers CG, de Groot JH, Arwert HJ, Rozendaal LA, Rozing PM (2004) Reliability of force direction dependent EMG parameters of shoulder muscles for clinical measurements. Clin Biomech (Bristol, Avon) 19:913–920. doi:10.1016/j.clinbiomech.2004.05.012
Reilly P, Macleod I, Macfarlane R, Windley J, Emery RJ (2006) Dead men and radiologists don’t lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl 88:116–121. doi:10.1308/003588406X94968
San Juan JG, Kosek P, Karduna AR (2012) Humeral head translation after a suprascapular nerve block. J Appl Biomech [Epub ahead of print]
Seida JC, LeBlanc C, Schouten JR, Mousavi SS, Hartling L, Vandermeer B, Tjosvold L, Sheps DM (2010) Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med 153:246–255
Sharkey NA, Marder RA, Hanson PB (1994) The entire rotator cuff contributes to elevation of the arm. J Orthop Res 12:699–708
Sher JS, Uribe JW, Posada A, Murphy BJ, Zlatkin MB (1995) Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg Am 77:10–15
Sobel JS, Winters JC (1996) Shoulder complaints in general practice. Diagnosis and treatment. PhD Thesis, University of Groningen, Groningen, The Netherlands
Steenbrink F, de Groot JH, Veeger HE, Meskers CG, van de Sande MA, Rozing PM (2006) Pathological muscle activation patterns in patients with massive rotator cuff tears, with and without subacromial anaesthetics. Man Ther 11:231–237. doi:10.1016/j.math.2006.07.004
Steenbrink F, de Groot JH, Veeger HE, van der Helm FC, Rozing PM (2009) Glenohumeral stability in simulated rotator cuff tears. J Biomech 42:1740–1745. doi:10.1016/j.jbiomech.2009.04.011
Steenbrink F, Meskers CG, van Vliet B, Slaman J, Veeger HE, de Groot JH (2009) Arm load magnitude affects selective shoulder muscle activation. Med Biol Eng Comput 47:565–572. doi:10.1007/s11517-009-0482-8
Steenbrink F, Nelissen RG, Meskers CG, van de Sande MA, Rozing PM, de Groot JH (2009) Teres major muscle activation relates to clinical outcome in tendon transfer surgery. Clin Biomech (Bristol, Avon) 25:187–193. doi:10.1016/j.clinbiomech.2009.11.001
Steenbrink F, Meskers CG, Nelissen RG, de Groot JH (2010) The relation between increased deltoid activation and adductor muscle activation due to glenohumeral cuff tears. J Biomech 43:2049–2054. doi:10.1016/j.jbiomech.2010.04.012
van der Zwaal P, Thomassen BJW, Nieuwenhuijse MJ, Lindenburg R, Swen JWA, van Arkel ERA (2013) Clinical outcome in all-arthroscopic versus mini-open rotator cuff repair in small- to medium-sized tears: a randomized controlled trial in 100 patients with one year follow-up. Arthroscopy 29:266–273. doi:10.1016/j.arthro.2012.08.022
Wiertsema SH, Rietberg MB, Hekman KM, Schothorst M, Steultjens MP, Dekker J (2013) Reproducibility of the Dutch version of the Western Ontario Rotator Cuff Index. J Should Elbow Surg 22:165–170. doi:10.1016/j.jse.2012.03.014
Yamaguchi K, Tetro AM, Blam O, Evanoff BA, Teefey SA, Middleton WD (2001) Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Should Elbow Surg 10:199–203. doi:10.1067/mse.2001.113086
Acknowledgments
The authors would like to acknowledge J. van der Ploeg and P. Bakkenes (Technical Dept., Leiden University Medical Center, The Netherlands) for their input in developing the experimental setup, J.W.A. Swen for performing some of the surgeries, and L. ter Braak and S. Werner (Faculty of Movement Sciences, VU University, Amsterdam) for performing measurements on the healthy controls. This study is part of a larger project funded by ZonMw, The Netherlands Organization for health research and development (NOW) (grant number 40-00703-98-8564), and the Dutch Arthritis Association (grant number 09-1-303).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Witte, P.B., van der Zwaal, P., van Arkel, E.R.A. et al. Pathologic deltoid activation in rotator cuff tear patients: normalization after cuff repair?. Med Biol Eng Comput 52, 241–249 (2014). https://doi.org/10.1007/s11517-013-1095-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-013-1095-9