Abstract
This study aimed to compare glenohumeral stability during functional tasks in subjects with previous dislocation injury against non-injured controls. Six subjects with previous injury and six controls were asked to complete hand-positioning tasks against external forces applied in six directions. Arm kinematics, muscle activations and hand forces were measured and used as input to an inverse-dynamic model of the shoulder that optimised muscle forces to solve the load-sharing problem. Glenohumeral stability was calculated using the direction of the joint reaction force vector in the glenoid. The simulations showed that GH stability was significantly lower in the previously injured group compared to the controls, and that the direction of exerted forces had a significant effect on GH stability, with the hand pushing away from the body and medially producing significantly lower stability. GH stability was significantly lower in the previously injured group for all six force directions, even though all participants were back to normal activities and reported no symptoms from their injuries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The human shoulder has been described as the perfect compromise between mobility and stability [15]. However, due to the shallow glenoid, passive stability of the joint is limited and stability must be maintained by coordinated activation of the muscles around the joint. This active stability is required for successful completion of a number of activities of daily living, but stability of the joint can be compromised in a number of conditions such as nerve injury, rotator cuff tears, spinal cord injury and stroke.
The incidence of shoulder dislocation is thought to be about 17 per 100,000 [6], with the majority of these being anterior dislocations as a result of trauma [3]. Traumatic dislocation of the glenohumeral joint is a common occurrence which carries a significant risk of morbidity in the form of recurrent instability [8].
Physical examinations used to diagnose shoulder instability include the anterior drawer test, the posterior drawer test and the apprehension test [2]; however, there is little evidence regarding the reliability and validity of these types of physical examinations [7]. While these tests may indicate whether a shoulder is unstable, they are limited in their ability to quantify the instability. Other methods of assessing shoulder instability are questionnaires [1]; however, the accuracy of these is dependent on the individual’s ability to answer accurately.
A better understanding of muscle function and individual muscle forces in the shoulder may enable a better understanding of instability and its causes. However, measuring muscle forces and joint reaction forces in vivo is not possible with non-invasive methods. Biomechanical models allow for the estimation of these forces based on external measurements.
One biomechanical model of the shoulder is the Delft shoulder and elbow model (DSEM) [14]. The DSEM is a 3D inverse-dynamic model of the shoulder complex that calculates muscle and joint forces from an input of external loads and recorded motions of the body. It has been validated qualitatively over a wide range of flexion and abduction postures using EMG recordings from a number of shoulder and arm muscles [14], and more quantitatively by comparing joint forces measured using an instrumented prosthesis with those predicted by the model during forward flexion and abduction tasks [11].
The calculation of joint contact forces includes the magnitude and direction of the glenohumeral joint reaction force (GH-JRF) vector, which should point into the glenoid in a stable shoulder. The orientation of this vector, which is influenced both by the forces in the muscles crossing the glenohumeral joint and the orientation of the scapula, provides an estimate of the stability of the joint during normal activity.
This estimate can be further improved using EMG recorded from the subject to constrain the muscle activation patterns predicted by the model, as implemented in previous research [11]. It was found that this EMG-driven model predicted GH-JRF up to 45 % more accurately than the model with no EMG input in patients with instrumented total shoulder prostheses. It was suggested this improvement was due to the ability of the model to take the existence of possibly abnormal muscle co-contractions of patients into account. Therefore, this EMG-driven model could be used to more accurately predict GH-JRF in other clinical populations with altered muscle activations.
The aim of this study was to quantify the differences in active stability of the glenohumeral joint in people with previous dislocation injuries, who may show altered neuromuscular control, compared to a non-injured control population. It was hypothesised that the previously injured shoulders would be less stable than the non-injured shoulders, and that the DSEM-based method for estimating GH stability would be sensitive enough to detect the change. Additional aims of the study were to identify the conditions under which joint stability is most compromised, and to identify the changes in muscle forces and scapular kinematics associated with this instability.
2 Methods
2.1 Subjects
Six previously injured subjects (mean age = 27 ± 7) and six non-injured controls (mean age = 25 ± 6) were recruited; all participants were male. Subjects were eligible for inclusion if they had had a previous injury that had been identified as a shoulder dislocation, but were not currently undergoing medical treatment or rehabilitation. Time since dislocation was not controlled, but the previously injured subjects were not under the care of a physician, had all returned to normal activities of daily living, had no known symptoms of shoulder instability and had no known rotator cuff tears.
2.2 Upper limb stability task
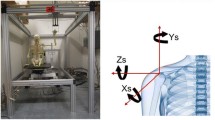
A robot arm (Haptic Master, Moog FCS, Nieuw Vennep, NL) was used to apply forces to the hand of the participant during upper limb postural stability tasks. A virtual reality environment (written in GameStudio) was used to present the task to the subject. An image of the subject’s arm was presented on a computer screen, and a target appeared at a predetermined (but randomised) position. The participant was asked to move the handle to the target position and resist the force applied through the handle, attempting to keep the hand as close to the target as possible. The experimental setup is shown in Fig. 1.
Forces were applied at nine positions (the centre and corners of a 20 cm virtual cube) in two directions along three axes (push/pull, left/right and up/down) and at two levels (5 and 10 N). The participant sat on a stool of height 70 cm, and the centre of the virtual cube was 30 cm above this, such that the arm was in a comfortable position in front of the participant and the hand height did not exceed that of the shoulder. This gave a total of 108 conditions, for which the order was randomised so the subject could not predict which force would come next. The duration of force application was 5 s for each condition, with a 5-s rest before the next condition to allow for movement to the new position. The session was split into two minute trials, with two minutes of rest between each trial. The interaction force between the robot arm and the participant’s hand was recorded throughout the trial at a frequency of 50 Hz.
2.3 Measurement of upper limb kinematics
Marker clusters were placed over the sternum, upper arm and forearm. Virtual markers were created using a probe with 4 active markers and used to define the thorax, humerus and forearm coordinate systems (Table 1). The local coordinate systems were constructed following the ISB standardisation protocol definitions [16]. Three-dimensional upper limb kinematics were recorded at 50 Hz using a CODA motion analysis system (Codamotion, Charnwood Dynamics, UK) throughout the upper limb stability test.
2.4 Electromyography data
Surface electromyograms (EMG) of biceps brachii, triceps lateral head, anterior, middle and posterior deltoids, infraspinatus and pectoralis major were recorded (Biometrics Ltd., Newport, Wales, UK). Sensor placement was carried out according to SENIAM guidelines as far as possible. All EMG data were normalised to MVCs taken for each muscle prior to the recording of the trials. EMG data were recorded at 1000 Hz using pre-amplifiers with 15–450 Hz band-pass filters. EMG envelopes were subsequently calculated by rectifying and low pass filtering the data at 10 Hz.
2.5 Scapular regression
Three-dimensional scapular kinematics were estimated during movement using a regression method, where scapular positions measured at a series of static locations were used to reconstruct the positions during dynamic movements. The static measurements were made during elevation of the arm in 4 planes of motion, using a scapular locator [5]. The locator had three adjustable legs which were positioned over the Angulus Inferior, Angulus Acromialis and Trigonum Spinae of the scapula. The same researcher palpated the skin, adjusted the locator and manually positioned it on the specific landmarks throughout the arm raises for all subjects. Regression analysis was then used to estimate scapular position based on positioning of the humerus and thorax for each subject. Estimated scapular positions were used to describe the shoulder kinematics and as input kinematic data for the inverse-dynamic simulations.
2.6 Inverse-dynamic simulations
Inverse-dynamic simulations were carried out using a large-scale model of the shoulder and elbow (DSEM) [11, 14]. Force, kinematic and EMG data were used as model inputs to estimate the muscle and joint forces at the shoulder during the positioning tasks. The model comprises 3-DOF sternoclavicular, acromioclavicular and glenohumeral joints, 2-DOF at the elbow, and a scapulothoracic gliding plane describing the motion of the scapula over the thorax. The muscles of the upper limb are divided into 139 elements and wrapping objects such as spheres and cylinders are defined to model their lines of action. Solution of the load-sharing problem is achieved by the minimisation of a cost-function representing energy consumption in the muscles [13].
An EMG-driven version of the model was used [11] for previously injured and non-injured subjects. In this model, at each time step, the calculated optimal muscle forces in the load-sharing optimisation were constrained by maximum and minimum muscle forces estimated using measured EMG data, for those muscles where EMG was measured (biceps brachii, triceps lateral head, anterior, middle and posterior deltoids, infraspinatus and pectoralis major). This constraint was set at ± 5 %, meaning the model-predicted muscle activation (estimated force divided by maximum isometric force at that length) was required to lie within ± 5 % of the measured EMG.
Muscle forces and the direction and magnitude of the reaction force in the glenohumeral joint were calculated by the model.
2.7 Model-based estimate of stability
Functional stability of the joint was estimated using the force vector in the glenoid during the upper limb stability task. Good-quality data on the passive structures such as ligaments and capsule around the glenohumeral joint are not available for this model, so the joint is modelled as a three degree-of-freedom joint, where translation is precluded. The stability of the joint is therefore represented by the orientation of the joint reaction force vector away from the normal, where this tendency of the force to cause dislocation is used as a proxy for joint stability.
The stability value was calculated as the mean value over 5s, using the angle of the vector away from the centre of the glenoid (Fig. 2; Eq. 1). A stability value of −1 results when the force is in the centre of the glenoid. As the vector moves towards the outside of the glenoid, the stability value increases towards 0, which is the maximum value that can be reached before dislocation of the joint.
where θ r and ϕ r are the angles of the vector away from the normal to the glenoid along the major and minor axes of the ellipse, and θ a and ϕ a are the maximum angles of that vector as it reaches the rim of the glenoid.
The effect of subject group, position and force direction on stability values was analysed for significance using a three-way ANOVA. Multiple comparisons (with Bonferroni correction) were performed for significant factors in the ANOVA. Muscle force predictions were reported for the most unstable condition. A Wilcoxon rank sum test was used to test for significant differences in muscle forces between the control and previously injured groups.
3 Results
A three-way ANOVA to assess the effects of previous injury, upper limb position and force direction found significant differences (p < 0.05) in stability values for previous injury and force direction. No significant difference was found for upper limb position.
Table 2 shows the influence of force direction on GH stability value. The previously injured group was found to have significantly lower stability than the control group for all force directions. Force direction was also found to be a significant factor for the glenohumeral stability value. ‘Push’ and ‘left’ forces produced significantly lower stability than ‘pull’, ‘right’ and ‘up’ forces (p < 0.05).
Figure 3 shows forces in the main shoulder muscles. Forces are shown for the condition where the subject is pushing to the left, as this condition produced the lowest values of stability. Subscapularis, teres minor, middle deltoid, posterior deltoid, serratus anterior and trapezius were all found to be significantly higher and supraspinatus, infraspinatus, anterior deltoid significantly lower in the previously injured group.
Table 3 shows the differences in scapular kinematics throughout all conditions. Scapular elevation was found to be significantly greater and posterior tilt significantly lower in the previously injured group. There was no significant difference in protraction between groups.
4 Discussion
This study has used a model-based approach to quantify glenohumeral stability in a range of arm positions, using the DSEM to estimate joint reaction force in both non-injured and previously injured shoulders. Upper limb postures tested during the current study were within the range of those used to validate the model [11, 14]. It was found that the previously injured shoulders had a lower stability value than the control group, as hypothesised, supporting this as a suitable method of calculating stability during a functional task. The sensitivity of this method is demonstrated by the fact that the previously injured subjects had no symptoms of instability and had returned to normal activity. It was found that the differences between groups were significant for all six force conditions.
No significant effects of arm position were seen for stability. Physical examinations used to diagnose instability often involve moving the upper limb into positions where the participant feels the shoulder is going to dislocate [2], suggesting that position of the arm does affect stability. The reason it was not seen in the current study is possibly due to the relatively small range of motion between the positions tested, compared to the more extreme positions, such as 90° abduction and maximal external rotation, used in previous physical examinations [4]. Furthermore, to simplify the experimental setup, the height of the workspace was not scaled to subject height in the current study, thereby introducing a small amount of additional variability into each arm posture tested.
Using the force condition with the lowest stability values for the previously injured group, we compared individual model-estimated muscle forces between the two groups for muscles around the shoulder.
Forces produced by the supraspinatus and infraspinatus muscles were significantly lower in the previously injured group, while forces in the teres minor and subscapularis muscles were significantly greater in the previously injured group. Forces in the posterior deltoid and middle deltoid were significantly higher in the previously injured group, and forces in the anterior deltoid were found to be significantly lower.
The single stability value provides a useful summary of multi-directional changes in the joint reaction force vector that easily allows us to test for differences between groups. In addition, by plotting the intersection of the vector with the glenoid, we can quickly see the direction of any instability. In this case, the stability plot shows joint reaction force vectors close to the posterior rim of the glenoid.
It is likely that increased posterior deltoid forces along with decreased anterior deltoid forces in the previously injured group led to this shift in the joint reaction force vector. The control group showed more balanced forces between the anterior and posterior deltoids with similar force values for both muscles. This is in agreement with previous research that has found subjects with multi-directional instability show increased EMG activity of posterior deltoid during abduction of the arm compared to control subjects [10].
Significant differences in scapular kinematics were also seen between groups for elevation and posterior tilt. Previous research, using healthy subjects, found scapular posterior tilt to increase as humerus elevation increased [9]. That study found posterior tilt was approximately 6° at 40° of humerus elevation and 10° at 90° of humerus elevation. These are similar to the control group in the current study, as would be expected comparing two groups of healthy subjects. The previously injured group showed significantly higher posterior tilt, comparable to values at 120° of humerus elevation in previous research [9]; however, humeral elevation did not go above 90° during the stability task in the current study.
Previous literature has reported increased posterior tilt in shoulders with multi-directional instability, compared with healthy shoulders, while performing abduction of the humerus in the scapular plane [12]. It is difficult to generalise these results to the results of the current study, due to the difference in movements and direction of instability of subjects tested. However, both suggest that there may be a relationship between increased posterior tilt and shoulder instability.
The addition of the EMG constraint to the muscle force optimisation allows the model to account for co-contraction and may increase the accuracy of muscle force prediction in clinical populations with abnormal muscle activation patterns [11]. One of the limitations in this method is the difficulty in isolating individual muscles, particularly the infraspinatus muscle, with surface electrodes. It is possible there is some crosstalk between muscles recorded, and further research is needed to quantify this error. However, any limitation in recording the infraspinatus EMG is common to both previously injured subjects and controls, so should not account for the differences seen between the groups.
Another limitation lies in the way the EMG signal is normalised. In this study, EMG was normalised to MVC trials where the participant was asked to exert a maximal effort against resistance provided by the experimenter. If subjects failed to elicit a true MVC, activation of the muscles during the stability task would be overestimated. Obtaining a true MVC may be particularly difficult in previously injured subjects with shoulder instabilities due to the fear of re-injury. Further research is needed to establish the reliability of MVC trials for muscles around the shoulder, particularly in subjects with glenohumeral instability.
A ±5 % constraint was used for the EMG constraint as suggested in previous research [11], which analysed different tolerances on a single subject to quantify the effect of EMG constraints on model-predicted GH-JRF. It was found that different tolerances did influence GH-JRF; however, these changes were not considerable in the range of 1–10 % tolerance. It is suggested that asymmetric bounds would be most appropriate, for example +5 −25 %, as an inadequate MVC effort will lead to overestimation rather than underestimation of muscle activity.
In conclusion, this study has demonstrated a method of quantifying glenohumeral stability with enough sensitivity to detect significant differences between previously dislocated and non-injured shoulders. Further research is needed to validate and assess the reliability of these methods, particularly the EMG recordings used to constrain the load-sharing optimisation. Differences were found in scapular kinematics and muscle forces around the shoulder, providing some possible explanations for the differences in stability between the two groups. It is believed that this method of calculating stability and assessing muscle activation can be used to develop and assess rehabilitation interventions in future research.
References
Dawson J, Fitzpatrick R, Carr A (1999) The assessment of shoulder instability. J Bone Joint Surg 81:420–426
Gerber C, Ganz R (1984) Clinical assessment of instability of the shoulder with special reference to anterior and posterior drawer tests. J Bone Joint Surg 66:551–555
Groh G, Wirth M, Rockwood C Jr (2010) Results of treatment of luxiato erecta (inferior shoulder dislocation). J Shoulder Elbow Surg 19:423–426
Jobe F, Kvitne R, Giangarra C (1989) Shoulder instability in the overhand or throwing athlete. Orthop Rev 18:1214–1238
Johnson G, Stuart P, Mitchell S (1992) A method for the measurement of three-dimensional scapula movement. Clin Biomech 8:269–273
Kroner K, Lind T, Jensen J (1998) The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg 108:288–290
Marx R, Bombardier C, Wright J (1999) What do we know about the reliability and validity of physical examination tests used to examine the upper extremity? J Hand Surg 24:185–193
McBride T, Kalogrianitis S (2011) Dislocations of the shoulder joint. Trauma 14:47–56
McClure P, Michener L, Sennett B, Karduna A (2001) Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg 10:269–277
Morris A, Kemp G, Frostick S (2004) Shoulder electromyography in multidirectional instability. J Shoulder Elbow Surg 13:24–29
Nikooyan A, Veeger H, Westerhoff P, Bolsterlee B, Graichen F, Bergmann G, van der Helm F (2012) An emg-driven musculo-skeletalmodel of the shoulder. Hum Mov Sci 31:429–447
Ogston J, Ludewig, P (2007) Differences in 3-dimensional shoulder kinematics between persons with multidirectional instability and asymptomatic controls. Am J Sports Med 35:1361–1370
Praagman M, Chadwick E, van der Helm F, Veeger H (2006) The relationship between two different mechanical cost functions and muscle oxygen consumption. J Biomech 39:758–765
van der Helm F (1994) A finite element musculoskeletal model of the shoulder mechanism. J Biomech 27:511–553
Veeger H, van der Helm F (2007) Shoulder function: the perfect compromise between mobility and stability. J Biomech 40:2119–2129
Wu G, van der Helm F, Veeger H, Makhsous M, Roy P, Anglin C, Nagels J, Karduna A, McQuade K, Wang X, Werner F, Buchholz B (2005) ISB recommendation on denitions of joint coordinate systems of various joints for the reporting of human joint motionpart II: shoulder, elbow, wrist and hand. J Biomech 38:981–992
Acknowledgments
The authors would like to thank Joris Lambrecht (Case Western Reserve University) for the GameStudio visualisation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marchi, J., Blana, D. & Chadwick, E.K. Glenohumeral stability during a hand-positioning task in previously injured shoulders. Med Biol Eng Comput 52, 251–256 (2014). https://doi.org/10.1007/s11517-013-1087-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-013-1087-9