Abstract
The sinus node is an inhomogeneous structure. In the embryonic heart all myocytes have sinus node type pacemaker channels (I f) in their sarcolemma. Shortly before birth, these channels disappear from the ventricular myocytes. The response of the adult sinus node to changes in the interstitium, in particular to (neuro)transmitters, results from the interplay between the responses of all of its constituent cells. The response of the whole sinus node cannot be simply deduced from these cellular responses, because all cells have different responses to specific agonists. A biological pacemaker will be more homogeneous. Therefore it can be anticipated that tuning of cycle length may be problematic. It is discussed that efforts to create a biological pacemaker responsive to vagal stimulation, may be counterproductive, because it may have the potential risk of ‘standstill’ of the biological pacemaker. A normal sinus node remains spontaneously active at high concentrations of acetylcholine, because it has areas that are unresponsive to acetylcholine. The same is pertinent to other substances with a negative chronotropic effect. Such functional inhomogeneity is lacking in biological pacemakers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Whether or not there will be a place for biological pacemakers in addition to or as a substitute for technically very effective pacemakers, is discussed in another paper in this issue [53]. The biological material for biological pacemakers is derived from embryonic stem cells or from other types of cells with an undifferentiated status, or, alternatively, stems from genetic-engineering techniques. Therefore, it is relevant to consider the pacemaker characteristics of embryonic hearts and myocytes.
2 The embryonic heart
2.1 The initiation of the heart rhythm: early sinus node control
The embryonic heart develops by the fusion of two primordia into one single tube [60]. This tube bends and septates, eventually leading to the four-chambered heart [8]. Fano and Badano [21] were the first in 1890 to show that there is a pacemaker hierarchy within the embryonic heart. They observed the propagation of contraction waves in longitudinal strips cut from the chicken heart, but they also noticed the higher contraction rate of the atrium compared with the ventricle after transection between these two segments. However, at an earlier stage of development Sabin [54] had shown in 1917 that the onset of contraction is in the ventricle not in the atrium:
“It is interesting to note that there is no movement whatever in the vein, the entire twitching being confined to the ventricle proper.”
The onset of cardiac contraction in the chicken embryo is at 29–30 h of development, whereas the circulation of the blood starts at 38–40 h [46]. Patten and Kramer [46] noted in 1933 about the ventricular onset of contraction:
“The first contractions were not rhythmic in their recurrence. They appeared more as sporadic flutters of restlessness in the developing myocardium, manifested first in one area and then in another, but always limited to the ventricle. (...) If one watches a heart at this stage for an hour or more, making repeated counts of the beats and recording the rest periods, it becomes apparent that the series of beats are tending to become longer and the rest intervals shorter. In other words a definite rhythmicity is gradually becoming established.”
The latter sentence from this famous paper of Patten and Kramer [46] confuses contractility with automaticity. Sabin [54] and Patten and Kramer [46] optically observed the onset of excitation-contraction coupling rather than the onset of automaticity. It was thought that there was a gradual development of pacemaker hierarchy from ventricle towards the atrium, ultimately ending in pacemaker dominance in the sinus venosus [3]. Van Mierop [59] has shown that this point of view is wrong. Early electrophysiological measurements were made by Meda and Ferroni [34] in 1959, showing the presence of diastolic depolarization in the sinus venosus and its absence in the ventricle in embryonic chicken hearts of 42 h of development. Van Mierop [59] explicitly made clear that there is electrical activation in hearts before they start to contract. Thus, he impaled hearts from 28 h of incubation and observed that there was electrical propagation of action potentials, originating from the sinus venosus, towards the ventricle even in completely non-contracting embryonic hearts. At a slightly later stage of development he noted:
“In 31-h embryos (...) the bulboventricular part of the heart was always seen to beat, the sinoatrial part never. Here again, however, sinoatrial action potentials could be recorded which were followed after an interval of about 100 ms by a ventricular action potential and a peristaltoid ventricular contraction.”
Obviously, the early observations on contractility have obscured the electrical pacemaker behaviour of the early embryonic heart for decades. The fact that the sinus node controls heart rate in very early embryonic stages, does not mean that the embryonic ventricle would not display automaticity if it were not paced. This auxiliary characteristic relies on the fact that embryonic ventricle, at least in the mouse, has a sinus node type of pacemaker current based on HCN4 channels, which disappear a couple of days before birth [66] (see below).
Although it is clear that pacemaker dominance resides within the posterior side of the tubular heart (i.e. at the venous input side), it remains enigmatic how the sinus node develops towards its morphological recognizable structure, to quote Moorman and colleagues [37]. Recent advances in molecular biology have made clear that the transcription factor Tbx3 is unique for the central part of the cardiac conduction system, which comprises the sinus node, the atrioventricular node, the atrioventricular bundle and the proximal part of the bundle branches [25]. Where Tbx3 is expressed, chamber type molecular markers as connexin40 or natriuretic precursor peptide A are absent [25].
2.2 Embryonic cardiac development after the initiation of a regular heart rhythm
Until 6 days of development, that is after the establishment of regular sinus node function, the embryonic heart functions (1) without an AV node, (2) without a specific conduction system and (3) without valves. The origin of the AV node and of the ventricular conduction system has long been a matter of controversy (for older literature, see [7]). The AV node develops from the lower part of the interatrial septum and not from the AV canal, i.e. the zone between the atrium and the ventricle in the tubular heart, which becomes the annulus fibrosis in the adult heart [2]. Even after the development of the AV node (at about 6 days of development) there is no electrical communication between the atrium and the ventricle by this pathway, simply because the AV node and the ventricular septum are not yet connected [2]. The ventricular conduction system develops in situ, from the ventricular trabeculae [60]. In the embryonic heart at 1.5 days of development there is already some electrophysiological differentiation. The action potentials in (part of) the atrium and the ventricle are different [34, 59]. At this stage there is coexpression of adult atrial and ventricular isomyosins in the entire tubular heart except in a part of the sinoatrial region [14]. Until 2 days of development there is no zone in the heart in which the conduction velocity exceeds 2 cm/s [1]. Thus, there is slow conduction in the whole tubular heart. The conduction is also slow compared with the central zone of the adult sinoatrial node of several mammalian species [42]. During further development (stages older than 14 according to Hamburger and Hamilton [23]) there is a gradual loss of the coexpression of both isomyosins in the atrium and the ventricle [55]. This correlates with further electrophysiological differentiation within the heart [1]. Thus, areas with synchronous contraction (faster conduction) tend to show single isomyosin expression, whereas areas with peristaltoid contraction (slow conduction) maintain the coexpression of both types of isomyosins [14]. The outflow tract of a developing embryonic heart at day 4 shows remarkably slow conduction. Figure 1 (from [15]) shows a unique feature of the embryonic heart. Traces 1 and 2 are unipolar electrograms recorded from the ventricle and the outflow tract respectively. This embryonic heart was paced from the left atrium (open triangle in trace 1). The ventricular depolarization is indicated with the open circle and the ventricular repolarization with the filled square. The arrow in trace 2 indicates the activation of the outflow tract. Finally, trace 3 shows a transmembrane potential from the outflow tract. The upstroke of the (slow) action potential coincides with the activation of the outflow tract in trace 2. Also, the stimulation artefact of the next cycle in the left atrium occurs in the middle of the plateau phase of the action potential in the outflow tract (indicated with the large filled triangle in trace 3). The role of this very late activating (and contracting) area is probably to provide the embryonic heart with a physiological substitute for valves that have not been developed at this stage. In the adult heart this area becomes the right ventricular outflow tract. It is remarkable that this area maintains the feature of final latest activation as has been described in many species under several circumstances, but recently also in the human heart under complete physiological conditions [51]. Apart from the fact that the outflow tract constitutes an interesting feature of cardiac development, it is emphasized (although completely speculative), that abnormal remnants of such embryological zones may play a role in syndromes and diseases as right ventricular dysplasia or Brugada syndrome, which are thought to have primarily a molecular background during recent years. The debate of the underlying mechanism behind Brugada syndrome has recently focused on the significance of conduction slowing [10] versus repolarization disorders [35] with or without a prominent role for so-called channelopathies, in this case a mutation in the gene encoding the fast inward sodium channel. It is quite remarkable that the large majority of patients in a syndrome with supposed genetic background do in fact not carry the mutation [11]. It might be that a genetic disorder is not the cause of the syndrome, but rather a modulating factor. The reason for elaborating on this issue is that it might indicate that introducing tissue with inherent slow conduction, derived from embryonic tissue or mimicking characteristics of embryonic tissue, like a biological pacemaker, may come with the price of proarrhythmia.
Electrical recordings from embryonic chicken heart of 4 days old. Traces 1 and 2 unipolar electrograms from ventricle and outflow tract. Trace 1 unipolar electrogram from ventricle. Open triangle stimulus artefact from pacing at left atrium. Open circle activation of ventricle. Filled square repolarization of ventricle. Trace 2 unipolar electrogram from outflow tract. Arrow repolarization of outflow tract. Trace 3 transmembrane potential from outflow tract. The stimulation artefact of the next cycle in the left atrium (trace 1) occurs in the mid of the plateau phase of the action potential in the outflow tract (indicated with the large filled triangle in trace 3). Reproduced with permission from [15]
2.3 Sequential (ontogenetic) appearance of membrane currents
Recent progress in genetic engineering has renewed the interest in the early development of the mouse heart. The order by which membrane currents appear in the embryonic heart has thus far been restricted to studies in mice embryos [12] and in cell cultures derived from mouse embryonic stem cells (for review see [24]). The slow inward calcium current (I Ca–L) has been demonstrated at 9.5 days post coitum (dpc) [30] and increases steadily until birth at 19 dpc, [12, 30], whereas the fast inward sodium current (I Na) becomes prominent at later stage [12]. With respect to the repolarizing currents the transient outward current (I to1) develops first [12, 24, 67] with higher atrial than ventricular density [12]. Other outward potassium currents develop later with different regional densities [12]. Thus, cells at 11–13 dpc depend on I Ca–L for the upstroke and on I to1 for repolarization of their action potentials in line with the observation that these currents develop also first in cells derived from mouse embryonic stem cells [24, 67]. Figure 2 (from [67]) shows a putative scheme with sequential development of membrane currents in the embryonic murine ventricle. The horizontal arrow at the top of Fig. 2 shows supposed development, whereas the arrow at the bottom of Fig. 2 indicates the order by which membrane currents might (re)appear when the view is taken that under certain pathological conditions a foetal gene program is recapitulated. It goes without saying that the latter is highly speculative. The pacemaker current I f plays a prominent role in pacemaking in the adult sinus node, also in man. Figure 2 shows that this current disappears around birth from the embryonic murine ventricle. Reintroducing it in ventricle therefore introduces a current that is normally absent in ventricle.
Order by which membrane currents develop in the murine embryonic ventricle (arrow at top). During remodeling in pathophysiological processes these currents might reappear in reverse order (arrow at bottom). Reproduced with permission from [67]
2.4 Role of pacemaker currents with focus on I f
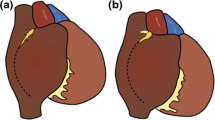
The embryonic mouse heart starts to beat at 8.5 dpc. The full gestation period takes 21 days. Figure 3a (taken from [66]) shows that ventricular myocytes from hearts at 9.5 dpc exhibit spontaneous activity and Fig. 3c shows the presence of inward current activating upon hyperpolarization, which is a feature of the pacemaker current I f. At 18 dpc, that is 3 days before birth, the action potential configuration has changed substantially, spontaneous activity has slowed down and has lost regularity (Fig. 3b). The I f current has disappeared almost completely shortly before birth (Fig. 3d). The fact that these ventricular myocytes display automaticity at early development does not exclude that the sinus node drives the embryonic heart from the very onset of electrical activity as in the chicken heart [59], but experimental proof for this is lacking. The right panel of Fig. 3 shows that the principal ion channel subunit at 9.5 dpc is based on expression of HCN4, which is a member of the hyperpolarization-activated cyclic nucleotide-gated (HCN) family of genes [4] and which is underlying the I f current of the adult sinus node. During the second half of embryonic development the expression of HCN4 mRNA disappears almost completely (Fig. 3, right panel). HCN2, which is virtually the only expressed HCN gene in adult working atrial and ventricular myocytes, displays low expression during the full period of embryonic development. The role of the HCN2 based I f current in adult atrium and ventricle is unclear, given the negative potential range where this current activates [45]. It thus seems as if immature ventricular myocytes are more or less sinus node type cells and that during the process of maturation the loss of sinus node type I f current and the gain of inward rectifier current (I K1) [12, 67] results in the loss of intrinsic automaticity.
Pacemaker current I f in embryonic murine ventricle. Panel a action potentials at stage 9.5 days post coitum (dpc). Panel b action potentials at stage 18 dpc. Panel c activation of I f upon hyperpolarizing pulses at 9.5 dpc. Panel d activation of I f upon hyperpolarizing pulses at 18 dpc. Right panel Expression of HCN1 mRNA, HCN2 mRNA and HCN4 mRNA at 9.5 and 18 dpc. Compiled from [66]
2.5 ß-Adrenergic modulation of currents in embryonic myocytes
As early as at 9.5 dpc I f current is responsive to ß-adrenergic modulation [66], as is the case with the L-type Ca2+ current [30]. The fact that I f is more responsive to forskolin than to isoproterenol [66] suggests that the intracellular second messenger cascade develops earlier than (coupling to) the ß-adrenoceptor in the sarcolemma. Directly after birth the responsiveness to ß-adrenergic stimulation continues to increase as has been demonstrated in chicken [56].
Interestingly, in cardiomyocytes differentiated from human embryonic stem cells, positive chronotropic effects have been reported in response to phenylephrine (10−4 M), an α-adrenergic agonist, and to isoprenaline (10−6 M), a ß-adrenergic agonist. Also, negative effects of exposure to carbachol (10−4 M) were reported, which suggests effective vagal responsiveness [38]. However, the concentrations of all these substances were very high.
3 Pacemaking in the adult sinus node
3.1 Regularity and basic cycle length
Soon after the development of the technique to isolate individual myocytes from a whole heart [49], it was refined to the sinus node [33]. It came much as a surprise that single sinus node cells, despite the fact that they have been isolated from an intact adult sinus node, no longer possess the feature of beat-to-beat regularity (Fig. 4, taken from [43]). Also, an isolated sinus node, detached from the right atrium beats faster than when attached to the right atrium [27] and nodal areas close to the crista terminalis have a higher intrinsic frequency than the pacemaker area, which appears ‘leading’ in an intact sinus node [28]. The latter results from a steeper diastolic depolarization in combination with shorter action potential duration [43]. These intrinsic characteristics change when the nodal cells are interconnected with each other and with the surrounding, hyperpolarizing, atrium. The function of the intact sinus node has been regarded as a process of synchronization rather than as process of conduction with a leading, dominant pacemaker delivering current to its surroundings [36]. Obviously, knowledge of the behaviour of single sinus nodal cells is insufficient to understand the behaviour of the whole sinus node. This issue will reappear when chronotropic effects and autonomic modulation are discussed (see below).
Action potentials of a single sinus node cell isolated from a rabbit sinus node. There is no beat-to-beat regularity. Horizontal bar 100 ms. Vertical bar 50 mV. Reproduced with permission from [43]
3.2 Mechanism of pacemaking
The main distinction between sinus node cells and working myocardial cells, irrespective whether it concerns atrial or ventricular cells, is that the former do not possess physiologically relevant I K1 current. This feature is also seen in embryological cells at early stages [12, 24, 67]. This explains why sinus node cells do not have a resting membrane potential, do not have a threshold potential for excitation and exert automaticity. In fact, automaticity results from the discrepancy between the kinetics of early inward and outward currents when these are not cancelled by the overwhelming conductance of the inward rectifier current (I K1). The lack of relevant I K1 current also explains the theoretical resting potential of −38 mV, where a sinus nodal cell would become quiescent, which is more a compromise between the Nernst potentials for K+ (about −90 mV) and Na+ (+70 mV) than in any other part of the heart. The fact that the maximum diastolic potential is much more negative (at about −65 mV) follows from the fact that the oscillations of the three important pacemaker mechanisms are more or less out of phase. The (outward) delayed rectifier current, probably primarily its rapid component (I Kr), at least in man [61], drives the maximum negative potential of sinus node cell to an area where the other two currents (the pacemaker current I f and the L-type Ca2+ current) can become operational. Which of these currents is the most critical for automaticity is not a very relevant physiological question, although it has given rise to ample debate [16, 26, 44]. It should be noted, however, that full blockade of either I Kr [62] or the L-type Ca2+ current [64] is incompatible with pacemaking. Full blockade of the ‘pacemaker current’ (I f) decreases heart rate, but does not prevent automaticity. The background, however, is that blockade of I Kr prevents the generation of a sufficiently negative membrane potential, which prevents the L-type Ca2+ current or I f to become activated and that blockade of L-type Ca2+ current prevents the upstroke of action potentials in sinus node cells. Blockade of the I f current, either by Cs+ or by alinidine or comparable agents, affects peripheral nodal cells more than the primary pacemaker area and thus does not disturb the standard nodal activation pattern [41].
4 Autonomic modulation of the adult sinus node
The pacemaker current involved in pacemaking are all more or less sensitive to environmental changes, amongst which autonomic modulation. Figure 5 (taken from [6]) shows a scheme of the rabbit sinus node with the dominant, leading (or primary) pacemaker area at the asterisk. Numerous changes in either concentrations of ions, or in autonomic tone or in circulating neurohumoural factors or blockers of specific membrane currents all may give rise to different local responses and therefore change the activation pattern of the nodal area. Because of the different responsiveness of those areas the chronotropic response of the intact sinus node cannot easily be predicted from the chronotropic responses of its constituent cells. The sinus node comprises several morphological cell types [63]. In addition there are also functional differences between more central (typical) nodal cells and peripheral (latent) pacemaker cells [5], which nevertheless have a higher intrinsic pacemaker potency [43]. Figure 6 (taken from [39]) shows the result of a computer analysis of cell types in the rabbit sinus node by discriminant analysis. Based on a combination of morphological and electrophysiological characteristics a specific type was assigned to each sinus node cell of which the location was unknown to the computer. Figure 6 shows that typical nodal cells are surrounded towards the crista terminalis (CT) by transitional cells with normal excitability and towards the interatrial septum by transitional cells with low excitability.
Pacemaker shifts in response to several interventions. CT crista terminalis, SEP interatrial septum, SVC vena cava superior, IVC vena cava inferior, E-4031 blocker of rapid component of delayed rectifier current, 4-AP 4-amino pyridine (blocker transient outward current). Adr adrenaline, Ach acetylcholine, Nif nifedipine (blocker L-type Ca2+ current) Reproduced with permission from [6]
Computer analysis of different sinus node cell types based on morphological and electrophysiological characteristics. Filled squares typical nodal cells. Filled triangles transitional cells with normal excitability. Open triangles transitional cells with low excitability. Open square atrial cell. The computer assigned the cell type by discriminant analysis, but was not aware of the location of the cells. Reproduced with permission from [39]
This is called functional inhomogeneity and we will explain this concept in more detail in the next section, because it is highly relevant for the requirements of autonomic modulation of a biological pacemaker.
4.1 Functional inhomogeneity
Figure 7 (taken from [32]) shows the background of functional inhomogeneity and its consequences for nodal chronotropic effects. Intact rabbit sinus nodes were sequentially impaled and activation patterns were determined during standard conditions (no adrenaline, no acetylcholine) and during the presence of either adrenaline (Adr) or acetylcholine (Ach). This gave rise to three different pacemaker centres (see also Fig. 5), one located in the superior sinus node (S, neither Adr nor Ach present), one located in the inferior sinus node (I, in the presence of Adr) and one located in the transitional zone (Tr), closer to the crista terminalis (CT, in the presence of Ach). These three centres were separated from each other. This will deliver three preparations (‘S’, ‘I’ and ‘Tr’) from each individual sinus node. Next the chronotropic responses to adrenaline and acetylcholine were determined for each of these centres. The responses of the primary centre (S) were intermediate both to acetylcholine and to adrenaline. The Adr centre (I) had large responses to both (neuro)humoural factors. The chronotropic responses to acetylcholine are depicted by dashed lines at the top of the histogram. There were individual preparations that turned quiescent in response to acetylcholine. In contrast, the Ach centre (Tr) hardly changed its cycle length after administration of either substance. The functional significance of these data is important. It indicates that there is huge intranodal variability with respect to receptor density and probably also innervation. Figure 8 (taken from [22]) shows recent data on the effect of vagal stimulation of the rabbit sinus node on the nodal activation pattern simultaneously assessed by optical methods. At the top left the field of view is shown with the orifices of the superior (SVC) and inferior vena cava (IVC) and the crista terminalis (CT) and the interatrial septum (IAS). The black dotted line indicates a line of block which is present under normal conditions [5]. EG indicates the site of the atrial electrogram. The black square indicates the area of optical recordings shown in the bottom panels a, b and c. Panel A is the last activation just prior to postganglionic vagal nerve stimulation. This occurs at a frequency which leads to neural firing with no direct influence on cardiac cells. Panel B is taken just after vagal stimulation and panel C indicates the fourth activation after stimulation. The normal activation pattern starts at ‘A’ in the top left panel and at ‘B’ after vagal stimulation. The shift is immediate and leads to a changed activation pattern for four consecutive cycles (see also the atrial electrogram in the upper right panel). The white zones in panels B and C show that there are areas that turn electrically quiescent. In addition, the upper right panel shows a hyperpolarization by 16% in the centre, which is dominant in the absence of vagal stimulation (trace 1). This hyperpolarization increases towards the block zone (33%; trace 4). The importance of this recent study of Fedorov et al. [22] is that it definitely shows that vagal stimulation can turn areas of the sinus node inexcitable without complete depression of pacemaker function of the complete sinus node. The lesson to be learned here is that a biological pacemaker with strong homogeneous response to vagal stimulation or to comparable stimuli may not constitute a sound goal.
Intact sinus nodes were mapped in normal Tyrode and in the presence of adrenaline (Adr; 0.6 μM) or acetylcholine (Ach; 5.5 μM). Subsequently these three centres (S: superior (primary) centre (Prim); I: inferior centre leading in the presence of Adr; Tr: transitional centre leading in the presence of Ach) were separated from each other and their chronotropic responses to Adr and Ach were measured. Such responses of subgroups are masked in the intact sinus node by pacemaker shifts. This phenomenon is known as functional inhomogeneity. Note that the inferior centre shows large responses to both Adr and Ach. The response to the latter may result in quiescence (indicated by dashed lines at the top of the bar). Reproduced with permission from [32]
Rabbit sinus node. Top left outline of preparation. Black square phrame of optical recordings as in bottom panels (a), (b) and (c). ‘A’ and ‘B’ indicate sites of pacemaker dominance during control and postganglionic vagal stimulation. EG site of electrogram in top right panel. CT crista terminalis; IAS interatrial septum. SVC superior vena cava; IVC inferior vena cava. Bottom panels activation patterns during control conditions (a), during the first cycle after postganglionic vagal stimulation (b) and during the fourth cycle after postganglionic vagal stimulation (c). Optical recordings of action potentials at the sites 1, 2, 3 and 4 in the bottom panels appear in the top right panel together with the amount of hyperpolarization of the maximum diastolic potential given as a percentage. See text for further details. Reproduced with permission from [22]
It should be noted that agents and/or neurohumoural factors with a positive chronotropic effect select for intranodal sites with a high intrinsic responsiveness. Agents with a negative chronotropic effect, however, select for intranodal sites with a low intrinsic responsiveness. As a consequence, an intact sinus node will always display composite chronotropic responses because pacemaker shifts will obscure the responses of specific intranodal sites. The Ach (Tr) centre shows an important feature: it hardly responds to acetylcholine and, thereby, prevents standstill of a normal sinus node. If a biological pacemaker were innervated in combination with a homogeneous distribution of muscarinic (M2) receptors, the risk of complete standstill is evident. This does not seem an attractive property of a biological pacemaker.
4.2 The case of accentuated antagonism
The same amount of (nor)epinephrine produces more acceleration, if the acetylcholine concentration or vagal tone is higher [29, 31, 40]. This phenomenon has been named ‘accentuated antagonism’ and has been explained by interaction between the two limbs of the autonomic nervous system at the pre- and postjunctional sites [29, 69]. Although this explanation may seem valid, it should be noted that functional inhomogeneity provides an alternative and more simple explanation. A high vagal tone shifts pacemaker dominance to areas with low responsiveness to both transmitters, whereas a high sympathetic tone shifts pacemaker dominance to areas with high responsiveness to both transmitters (Figs. 5, 7).
In addition, it should be realized that autonomic modulation affects the steepness of diastolic depolarization. A doubling of the slope of diastolic depolarization has a much more prominent effect at low heart rate than at high heart rate. Therefore it is logical that vagal and sympathetic effects are cycle length dependent [40]. At the level of single sinus node cells Rocchetti et al. [52] have unequivocally demonstrated that time-domain measurements of cycle length variability (changes in heart rate variability) cannot be translated into changes in neural input: “any condition depressing diastolic depolarization rate (DDR) may enhance cycle length (CL) variability, independent of changes in the pattern of neural activity” [52]; see also [68].
4.3 Differences between neural and humoural effects
It has been observed in dogs that bilateral vagal stimulation results in a lower heart rate in combination with stellate ganglion stimulation than in combination with norepinephrine infusion [57]. Although an intricate prejunctional interaction may explain this observation, functional inhomogeneity may provide a more simple explanation for this remarkable difference. High vagal tone will shift the pacemaker to the area with lowest innervation. Such an area may still accelerate in response to circulating catecholamines, but not or much less to sympathetic stimulation, simply because the nerves do not impinge on that particular area.
5 The transplanted heart
The transplanted heart is a rich source of information for the relation between the autonomic nervous system and the heart [9]. Blood pressure results from the product between cardiac output and peripheral resistance. Cardiac output is—in its turn—composed of the product between heart rate and stroke volume. The basic physiological concept that only cardiac output is directly, i.e. on a ‘per cycle’ basis is affected by vagal influences, whereas peripheral resistance is only affected by sympathetic influences with its concomitant 0.1 Hz dominant frequency seems untenable, given the fact that recipients of a donor heart are able to stand up at all. However, this reasoning applies in fact also to a normal heart.
The pivotal loss of information after heart transplantation is not the loss of information from the receptors in the sinus caroticus and in the arch of the aorta (baroreflex), but from the intracardiac receptors. Indeed, the main problems of these patients are blunted responses to volume expansion and to natriuremia. Thus these patients function in a permanent state of a large circulating volume and hypertension [9].
It has been reported that—at least—sympathetic reinnervation may occur after cardiac transplantation [65]. The evidence is based on the fact that the donor heart is able to produce noradrenaline after an injection with tyramine in the left anterior descending or circumflex coronary arteries. Although very interesting and probably functionally relevant, such experiments prove that the nerves in the donor heart still have or have regained metabolic activity. In my opinion it does not unequivocally prove that the central nervous system of the recipient has sympathetic neural control over the donor heart. In dogs with autotransplantation it has been reported that the maximal heart rate during exercise increases much more slowly and to a substantially lower maximum heart rate [17]. Nevertheless, in patients with a transplanted heart the maximum exercise tolerance can be large [9].
By and large, the most severe problems in patients with a transplanted heart, besides the problems with rejection, reside in the relation between heart and kidneys and focus on regulation of the total blood volume and blood pressure and to a lesser extent on exercise tolerance and postural changes. Probably this results from the fact that the intrinsic response to preload changes of donor hearts (Starling law) remains—at least partially—effective. I think, therefore, that innervation of a biological pacemaker is less important than the capacity to respond to circulating catecholamines (see below).
6 Biological pacemakers
6.1 State of the art
Thus far moderate success has been achieved with biological pacemakers either along the lines of a genetic or a cellular approach (Rosen et al., this issue [53]). Successful introduction of human ß2-adrenoceptor constructs has been reported in the murine heart [19] and in the porcine heart [20]. As far as the in vivo parts of these studies are involved, I wish to underscore that demonstrating that heart rate can be increased after the introduction of components of the adrenergic system is not the same as demonstrating that the heart is able to respond to catecholamines. Secondly, the response to injection of these constructs persisted for 2–3 days in the mice [19]) and for less than 2 days in the pigs [20]. Obviously, these responses are transient. In the case of cellular approaches it is important to know what happens to the implanted or injected biomaterials in case of loss of function. The biological function is simply lost, when the implant disappears (is ‘eaten’), but when it is still sitting in the myocardium and has lost pacemaker potency, a proarrhythmic risk may ensue.
In the dog substantial success has been achieved thus far (Rosen et al., this issue [53]) both by a gene therapy approach [47, 50] and by a cellular approach based on adult human mesenchymal stem cells [48]. In the former approach injection of adenoviral contructs with mouse HCN2 constructs into the left canine atrium [47] yielded spontaneous rhythms during vagal stimulation (in order to silence the native sinus node). This occurred 3–4 days after injection. Left atrial myocytes isolated from these hearts showed prominent I f current. In a comparable study HCN2 adenovirus contructs were injected in the posterior limb of the left bundle branch of canine hearts [50]. Again, during vagal stimulation ventricular escape rhythms were demonstrated at least 7 days after the injection. There was a brief period of arrhythmias after the injection, but this appears to be related to the injection not to the construct, because the arrhythmias were also prominent in the control group and ceased after days. Although these results are encouraging, it is emphasized that positive chronotropy in response to catecholamines was not demonstrated. Along the cellular approach human mesenchymal stem cells transfected with the murine HCN2 gene were injected in the epicardium of the left canine ventricle [48]. Again, during sinus arrest pacemaker activity was observed. In the in vitro part of this study [48], acetylcholine did not affect I f current, although it could mitigate the response to isoproterenol. Although it had been reported that human mesenchymal stem cells can form functional gap junctions with freshly isolated canine ventricular myocytes [58], this was also demonstrated in vivo at the actual site of injection of the engineered mesenchymal stem cells [48].
An experimental proof for the putative scheme as shown in Fig. 7 of Rosen et al. [53] (this issue), in which a genetically engineered stem cell is able to deliver pacemaker current to a myocyte is provided in another paper in this issue [13]. Thus, the spontaneous beating rate of neonatal rat cardiomyocytes can be tuned by co-culturing them with HEK−293 cells which stably express murine inward rectifier channels (Fig. 3 in [13], this issue). Although the beating rate of the neonatal rat cardiomyocytes rapidly decreases with a small proportion (only 5%) of engineered HEK-293 cells, spontaneous beating did not cease even when the large majority of cells (75%) were HEK-293 cells. With full blockade of I K1 current, more subtle tuning of the remaining ensemble spontaneous beating rate resulted. Although the authors did not emphasize this themselves, it is of particular interest that even with full blockade of I K1 current, the percentage of HEK-293 cells remains important for the final beating rate. This resembles the natural situation in which an intact, but isolated sinus node has a higher frequency than a complete right atrium, where the sinus node is connected to the surrounding atrial muscle [27].
6.2 Requirements of a biological pacemaker
I cite here a phrase from the paper by Rosen et al. [53] elsewhere in this issue: “...we have taken a lesson from our engineering colleagues who designed the electronic pacemaker; that is we are working to fine-tune a structure that mimics the sinus node functionally without recapitulating it morphologically.” Creating a homogeneous biological sinus node with functional responses to neurotransmitters with a prospect to real innervation, or at least with adrenergic- and muscarinic-type responses to humoural factors seems at first glance a desirable goal, but might probably not be such a good idea. The reason is simple. Such a biological pacemaker would also have the capacity of quiescence. This is exactly what we do not want. The ideal biological pacemaker would be one that is able to cope with postural changes and exercise. The former goal may seem far-fetched. It requires innervation, because adaptations are needed within a single cardiac cycle. For a response to exercise it is sufficient that a biological pacemaker can increase its rate. The biological pacemaker in statu nascendi as proposed by Rosen et al. [53] in this issue fulfils this more moderate goal and has a limitation that may constitute two advantages that can become important in future competition with the electronic pacemaker. The biological pacemaker is based on the pacemaker current (I f) only, not on a combination of multiple membrane currents, e.g. the acetylcholine sensitive K+ current (I K-Ach) is lacking. Therefore it cannot easily turn quiescent. It can only accelerate, which is exactly what an electronic pacemaker cannot. The debate on the mechanism of vagal modulation of sinus rhythm has never been definitely settled. Either acetylcholine inhibits I f current or it increases I K-Ach current or it does both (see for details Boyett et al. 2000). Figure 9 (taken from [18]) focuses on this issue. The left panel shows the effect of postganglionic vagal nerve stimulation (same technique as applied by Fedorov et al. [22]; see Fig. 8 in this paper), coupled to the cardiac cycle in the isolated right atrium of the rabbit. The top left panel shows the effect 10 stimuli per cycle leading to a prolongation of cycle length from 456 to 531 ms. The bottom left panel shows the same experiment in the presence of 3 μM atropine, blocking the vagally mediated response. During this procedure a hyperpolarizing pulse was given during diastole (right panel). This leads to an electrotonic disturbance of the membrane potential during diastole, which can be followed at a distance from the site of current injection. When the membrane conductance is high, much current ‘escapes’ over the sarcolemma and little current is transported along the axial pathway, the conductance of which is determined by cytoplasm and gap junctions. The right panel shows that during vagal stimulation the electrotonic potential decreases, which by simple Ohm’s law means that the resistance of the sarcolemma has decreased by opening of a membrane channel, not by closing. This provides a strong argument for opening of I K-Ach, not closing of I f in response to physiologically relevant vagal stimulation. This supports my view that it is fortunate that the biological pacemaker of Rosen et al. [53] (this issue) is solely based on I f current.
Postganglionic vagal stimulation in the rabbit sinus node. The chrontropic effect of ten stimuli locked to the spontaneous cycle is shown in the top panel left. The bottom panel left shows the same response in the presence of 3 μM atropine. The right panel shows the electrotonic potential during diastole. There is a 15–20% decrease of this potential during vagal stimulation, which can only be explained when membrane resistance has decreased. This implies that vagal stimulation increases the overal membrane conductance. This is more compatible with an increase of I K-Ach than with a decrease of I f in response to vagal stimulation. Compiled from [18]
A relatively high intrinsic heart rate based on a biological pacemaker, without the possibility of deceleration (e.g. during rest or sleep) may also be useful from the point of view that cardiac muscle with suboptimal contractile performance has impaired capacitance to compensate low heart rate by a high stroke volume. For this reason the management of recipients of a transplanted heart aims at maintaining a relatively high resting heart rate, if possible above 100 beats/min [9].
7 Conclusion
Biological pacemakers have a long way to go before they will ever be superior to electronic pacemakers. There is, however, important progress. It seems sufficient when biological pacemakers aim at responsiveness to humoural factors not neural factors in order to be able to cope with exercise.
References
Argüello C, Alanis J, Pantoja O, Valenzuela B (1986) Electrophysiological and ultrastructural study of the atrioventricular canal during the development of the chick embryo. J Mol Cell Cardiol 18:499–510
Argüello C, Alanis J, Valenzuela B (1988) The early development of the atrioventricular node and bundle of His in the embryonic chick heart. An electrophysiological and morphological study. Development 102:623–637
Barry A (1942) The intrinsic pulsation rates of fragments of the embryonic chick heart. J Exp Zool 91:119–130
Biel M, Schneider A, Wahl C (2002) Cardiac HCN channels: structure, function, and modulation. Trends Cardiovasc Med 12:206–213
Bleeker WK, Mackaay AJC, Masson-Pévet M, Bouman LN, Becker AE (1980) Functional and morphological organization of the rabbit sinus node. Circ Res 46:11–22
Boyett MR, Honjo H, Kodama I (2000) The sinoatrial node, a heterogeneous pacemaker structure. Cardiovasc Res 47:658–687
Canale ED, Campbell GR, Smolich JJ, Campbell JH (1986) Cardiac muscle. Springer, Berlin
Christoffels VM, Burch JB, Moorman AFM (2004) Architectural plan for the heart: early patterning and delineation of the chambers and the nodes. Trends Cardiovasc Med 14:301–307
Cirklin JK, Young JB, McGiffin DC (2002) Physiology of the transplanted heart. In: Cirklin JK, Young JB, McGiffin DC (eds) Heart transplantation. Churchill Livingstone, New York, pp 353–372
Coronel R, Casini S, Koopmann TT, Wilms-Schopman FJG, Verkerk AO, de Groot JR, Bhuiyan Z, Bezzina CR, Veldkamp MW, Linnenbank AC, van der Wal AC, Tan HL, Brugada P, Wilde AAM, de Bakker JMT (2005) Right ventricular fibrosis and conduction delay in a patient with clinical signs of Brugada syndrome: a combined electrophysiological, genetic, histopathologic, and computational study. Circulation 112:2769–2777
Coronel R, Berecki G, Opthof T (2006) Why the Brugada syndrome is not yet a disease: syndromes, diseases and genetical causality. Cardiovasc Res 72:361–363
Davies MP, An RH, Doevendans P, Kubalak S, Chien KR, Kass RS (1996) Developmental changes in ionic channel activity in the embryonic murine heart. Circ Res 78:15–25
De Boer TP, van Veen TAB, Houtman AJ, Jansen JA, van Amersfoorth SC, Doevendans PA, Vos MA, van der Heyden MAG (2007) Inhibition of cardiomyocyte automaticity by electrotonic application of inward rectifier current from Kir2.1 expressing cells. Med Biol Eng Comput (this issue). DOI 10.1007/s11517-006-0059-8
De Jong F, Geerts WJC, Lamers WH, Los JA, Moorman AFM (1987) Isomyosin expression patterns in tubular stages of chicken heart development: a 3-D immunohistochemical analysis. Anat Embryol 177:81–90
De Jong F, Opthof T, Wilde AAM, Janse MJ, Charles R, Lamers WH, Moorman AFM (1992) Persisting zones of slow impulse conduction in developing chicken hearts. Circ Res 71:240–250
DiFrancesco D (1993) Pacemaker mechanisms in cardiac tissue. Annu Rev Physiol 55:451–467
Donald DE, Shephard JT (1963) Response to exercise in dogs with cardiac denervation. Am J Physiol 205:494–500
Duivenvoorden JJ, Bouman LN, Opthof T, Bukauskas FF, Jongsma HJ (1992) Effect of transmural vagal stimulation on electrotonic current spread in the rabbit sinoatrial node. Cardiovasc Res 26:678–686
Edelberg JM, Aird WC, Rosenberg RD (1998) Enhancement of murine cardiac chronotropy by the molecular transfer of the human ß2 adrenergic receptor cDNA. J Clin Invest 101:337–343
Edelberg JM, Huang DT, Josephson ME, Rosenberg RD (2001) Molecular enhancement of procine cardiac chronotropy. Heart 86:559–562
Fano G, Badano F (1890) Etude physiologique des premiers stades dedévelopement du coeur embryonaire du poulet. Arch Ital Biol 13:387–422
Fedorov VV, Hucker WJ, Dobrzynski H, Rosenshtraukh LV, Efimov IR (2006) Postganglionic nerve stimulation induces temporal inhibition of excitability in the rabbit sinoatrial node. Am J Physiol Heart Circ Physiol 291:H612–H623
Hamburger V, Hamilton HL (1951) A series of normal stages in the development of the chick embryo. J Morphol 88:49–92
Hescheler J, Fleischman BK, Lentini S, Maltsev VA, Rohwedel J, Wobus AM, Addicks K (1997) Embryonic stem cells: a model to study structural and functional properties in cardiomyogenesis. Cardiovasc Res 36:149–162
Hoogaars WMH, Tessari A, Moorman AFM, De Boer PAJ, Hagoort J, Soufan AT, Campione M, Christoffels VM (2004) The transcriptional repressor Tbx3 delineates the developing central conduction system of the heart. Cardiovasc Res 62:489–499
Irisawa H, Brown HF, Giles W (1993) Cardiac pacemaking in the sinoatrial node. Physiol Rev 73:197–227
Kirchhof CJHJ, Bonke FIM, Allessie MA, Lammers WJ (1987) The influence of the atrial myocardium on impulse formation in the rabbit sinus node. Pflügers Arch 410:198–203
Kodama I, Boyett MR (1985) Regional differences in the electrical activity of the rabbit sinus node. Pflügers Arch 404:214–226
Levy MN (1971) Sympathetic–parasympathetic interactions in the heart. Circ Res 29:437–445
Liu W, Yasui K, Arai A, Kamiya K, Cheng J, Kodama I, Toyama J (1999) ß-Adrenergic modulation of L-type Ca2+ channel currents in early-stage embryonic mouse heart. Am J Physiol 276:H608–H613
Mackaay AJC, Opthof T, Bleeker WK, Jongsma HJ, Bouman LN (1980) Interaction of adrenaline and acetylcholine on cardiac pacemaker function. J Pharmacol Exp Ther 214:417–422
Mackaay AJC, Opthof T, Bleeker WK, Jongsma HJ, Bouman LN (1982) Interaction of adrenaline and acetylcholine on sinus node function. In: Bouman LN, Jongsma HJ (eds) Cardiac rate and rhythm. Martinus Nijhoff, The Hague, pp 507–523
Masson-Pévet M, Jongsma HJ, Bleeker WK, Tsjernina L, van Ginneken ACG, Treijtel BW, Bouman LN (1982) Intact isolated sinus node cells from the adult rabbit heart. J Mol Cell Cardiol 14:295–299
Meda E, Ferroni A (1959) Early functional differentiation of heart muscle cells. Experientia 15:427–428
Meregalli PG, Wilde AAM, Tan HL (2005) Pathophysiological mechanisms of Brugada syndrome: depolarization disorder, repolarization disorder, or more? Cardiovasc Res 67:367–378
Michaels DC, Matyas EP, Jalife J (1987) Mechanisms of sinoatrial pacemaker synchronization: a new hypothesis. Circ Res 61:704–714
Moorman AFM, De Jong F, Denyn MMFJ, Lamers WH (1998) Development of the cardiac conduction system. Circ Res 82:629–644
Mummery C, Ward-Van Oostwaard D, Doevendans P, Spijker R, Van Den Brink S, Hassink R, Van Der Heyden M, Opthof T, Pera M, Brutel De La Riviere A, Passier R, Tertoolen L (2003) Differentiation of human embryonic stem cells to cardiomyocytes. Role of coculture with visceral endoderm-like cells. Circulation 107:2733–2740
Opthof T, Bleeker WK, Masson-Pevet M, Jongsma HJ, Bouman LN (1983a) Little-excitable transitional cells in the rabbit sinoatrial node: a statistical, morphological and electrophysiological study. Experientia 39:1099–1101
Opthof T, Mackaay AJC, Bleeker WK, Jongsma HJ, Bouman LN (1983b) Cycle length dependence of the chronotropic effects of adrenaline and acetylcholine in the rabbit sinoatrial node. J Autonom Nerv Syst 8:193–204
Opthof T, Duivenvoorden JJ, VanGinneken ACG, Jongsma HJ, Bouman LN (1986) Electrophysiological effects of alinidine (St 567) on sinoatrial node fibers in the rabbit heart. Cardiovasc Res 20:727–739
Opthof T, De Jonge B, Jongsma HJ, Bouman LN (1987a) Functional morphology of the mammalian sinuatrial node. Eur Heart J 8:1249–1259
Opthof T, Van Ginneken ACG, Bouman LN, Jongsma HJ (1987b) The intrinsic cycle length in small pieces isolated from the rabbit sinoatrial node. J Mol Cell Cardiol 19:923–934
Opthof T (1988) The mammalian sinoatrial node. Cardiovasc Drugs Ther 1:573–597
Opthof T (1998) The membrane current (I f) in human atrial cells. Implications for atrial arrhythmias. Cardiovasc Res 38:537–540
Patten BM, Kramer TC (1933) The initiation of contraction in the embryonic chick heart. Am J Anat 53:349–375
Plotnikov AN, Sosunov EA, Qu J, Shalpakova IN, Anyukhovsky EP, Liu L, Janse MJ, Brink PR, Cohen IS, Robinson RB, Danilo P, Rosen MR (2004) Biological pacemaker implanted in canine left bundle branch provides ventricular escape rhythms that have physiologically acceptable rates. Circulation 109:506–512
Potapova I, Plotnikov A, Lu Z, Danilo P, Valiunas V, Qu J, Doronin S, Zuckerman J, Shalapakova IN, Gao J, Pan Z, Herron AJ, Robinson RB, Brink PR, Rosen MR, Cohen IS (2004) Human mesenchymal stem cells as a gene delivery system to create cardiac pacemakers. Circ Res 94:952–959
Powell T, Twist VW (1976) A rapid technique for the isolation and purification of adult cardiac muscle cells having respiratory control and a tolerance to calcium. Biochem Biophys Res Comm 72:327–333
Qu J, Plotnikov AN, Danilo P, Shlapakova I, Cohen IS, Robinson RB, Rosen MR (2003) Expression and function of a biological pacemaker in canine heart. Circulation 107:1106–1109
Ramanathan C, Jia P, Ghanem R, Ryu K, Rudy Y (2006) Activation and repolarization of the normal human heart under complete physiological conditions. Proc Natl Acad Sci USA 103:6309–6314
Rocchetti M, Malfatto G, Lombardi F, Zaza A (2000). Role of the input/output relation of sinoatrial myocytes in cholinergic modulation of heart rate variability. J Cardiovasc Electrophysiol 11:522–530
Rosen MR, Brink PR, Cohen IS, Robinson RB (2007) Biological pacemakers based on I f. Med Biol Eng Comput (this issue)
Sabin FR (1917) Origin and development of the primitive vessels of the chick and the pig. Carnegie Cont Embryol 6:61–124
Sanders E, De Groot IJM, Geerts WJC, De Jong F, Van Horssen AA, Los JA, Moorman AFM (1986) The local expression of adult chicken heart myosins during development. Anat Embryol 174:187–193
Satoh H, Sperelakis N (1993) Hyperpolarization-activated inward current in embryonic chick cardiac myocytes: developmental changes and modulation by isoproterenol and carbachol. Eur J Pharmacol 240:283–290
Takahashi N, Zipes DP (1983) Vagal modulation of adrenergic effects of canine sinus and atrioventricular nodes. Am J Physiol 244:H775–H781
Valiunas V, Doronin S, Valiuniene L, Potapova I, Zuckerman J, Walcott B, Robinson RB, Rosen MR, Brink PR, Cohen IS (2004) Human mesenchymal stem cells make cardiac connexins and form functional gap junctions. J Physiol 555:617–626
Van Mierop LHS (1967) Location of pacemaker in chick embryo heart at the time of initiation of heartbeat. Am J Physiol 212:H407–H415
Van Mierop LHS (1979) Morphological development of the heart. In: Berne RM, Sperelakis N, Geiger SR (eds) Handbook of physiology, Sect. 2, vol 1. The heart. Williams and Wilkins Co., Baltimore, pp 1–28
Veldkamp MW, Van Ginneken ACG, Opthof T, Bouman LN (1995) Human delayed rectifier. Circulation 92:3497–3504
Verheijck EE, van Ginneken ACG, Bourier J, Bouman LN (1995) Effects of delayed rectifier current blockade by E-4031 on impulse generation in single sinoatrial nodal myocytes of the rabbit. Circ Res 76:607–615
Verheijck EE, Wessels A, Van Ginneken ACG, Bourier J, Markman MWM, Vermeulen LJM, De Bakker JMT, Lamers WH, Opthof T, Bouman LN (1998) Distribution of atrial and nodal cells within the rabbit sinoatrial node. Models of sinoatrial transition. Circulation 97:1623–1631
Verheijck EE, van Ginneken ACG, Wilders R, Bouman LN (1999) Contribution of L-type Ca2+ current to electrical activity in sinoatrial nodal myocytes of rabbits. Am J Physiol 276:H1064–H1077
Wilson RF, Laxson DD, Christensen BV, McGinn AL, Kubo SH (1993) Regional differences in sympathetic reinnervation after human orthotopic cardiac transplantation. Circulation 88:165–171
Yasui K, Liu W, Opthof T, Kada K, Lee J-K, Kamiya K, Kodama I (2001) The I f current and spontaneous activity in mouse embryonic ventricular myocytes. Circ Res 88:536–542
Yasui K, Niwa N, Takemura H, Opthof T, Muto T, Horiba M, Shimizu A, Lee JK, Honjo H, Kamiya K, Kodama I (2005) Pathophysiological significance of T-type calcium channels: expression of T-type Ca(2+) channels in fetal and diseased heart. J Pharmacol Sci 99:205–210
Zaza A, Lombardi F (2001) Autonomic indexes based on the analysis of heart rate variability: a view from the sinus node. Cardiovasc Res 50:434–442
Zipes DP, Miyazaki T (1990) The autonomic nervous system and the heart: basis for understanding interactions and effects on arrhythmia development. In: Zipes DP, Jalife J (eds) Cardiac electrophysiology. From cell to bedside. W.B. Saunders, Philadelphia, pp 312–330
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Opthof, T. Embryological development of pacemaker hierarchy and membrane currents related to the function of the adult sinus node: implications for autonomic modulation of biopacemakers. Med Bio Eng Comput 45, 119–132 (2007). https://doi.org/10.1007/s11517-006-0138-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-006-0138-x