Abstract
Expression and function of the immunoregulatory molecule HLA-E was investigated in patients with relapsing-remitting (RR) multiple sclerosis (MS). Serum and cerebrospinal fluid (CSF) soluble (s)HLA-E and -G levels were measured by ELISA in 80 RRMS patients. Controls were patients with other inflammatory neurological disorders (OIND, n = 81) and noninflammatory neurological disorders (NIND, n = 86). Serum sHLA-E concentrations were higher in RRMS than in NIND patients only. CSF sHLA-E concentrations were higher in RRMS than controls. Increased CSF sHLA-E levels were detected in MRI inactive and clinically stable RRMS patients. sHLA-E intrathecal synthesis (ITS) was higher in RRMS than controls, and the number of patients with sHLA-E ITS above cut-off was higher i) in MS than controls, and ii) in clinically stable than clinically active MS patients. sHLA-E CSF levels and ITS correlated with i) the same sHLA-G parameters, and ii) disease duration. HLA-E expression and co-expression with CD markers were investigated in MS plaques from three different cases by immunohistochemistry and confocal microscopy, respectively. Infiltrating T lymphocytes and macrophages, as well as resident microglial cells and astrocytes expressed HLA-E. CSF samples from MS patients were finally tested for inhibitory activity of in vitro CTL and NK cell mediated cytotoxicity. sHLA-E+ were more effective than sHLA-E− CSF samples in such inhibition. Maximum inhibition was achieved with sHLA-E+/sHLA–G+ CSF samples In conclusion, increased sHLA-E CSF levels may play an immunomodulatory role in MS, contributing to the inhibition of intrathecal inflammatory response. The potential of sHLA-E as biomarker of MS activity warrants further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HLA-E belongs to “non-classical” HLA-class Ib molecules, that also include HLA-G, -F and -H (Le Bouteiller and Lenfant 1996). In contrast with highly polymorphic HLA-class Ia molecules (HLA-A, -B and -C) HLA-Ib molecules display a low degree of polymorphism, and different immunoregulatory properties (O’Callaghan and Bell 1998). HLA-G has been extensively characterized in the last years (Pistoia et al. 2007), whereas limited information are so far available on HLA-E, -F and -H.
HLA-E mRNA expression has been detected in different cell types. However, HLA-E expression on the cell surface, that requires the presence of nonapeptides derived from the HLA-I molecules leader peptide and of β2 microglobulin, is extremely restricted, and may be related to cell activation (Braud et al. 1998a). HLA-E exerts immunosuppressive functions, inhibiting NK cell and CD8+ T cell mediated lysis upon interaction with the NKG2A/CD94 inhibitory receptor (Braud et al. 1998b). However, in some physiological conditions, HLA-E interacts also with NKG2C/CD94 activating receptor, especially when HLA-E binds HLA-G derived peptides (Llano et al. 1998). Moreover, HLA-E can bind peptides derived from self or foreign proteins and present them to classical CD8+ T cells (Garcia et al. 2002; Pietra et al. 2003). Finally, a sub-population of HLA-E restricted regulatory CD8+ T cells has been characterized in mice (Lu et al. 2008).
In the last years, the expression and function of soluble (s)HLA-E, that is generated by shedding of the membrane-bound molecule operated by metalloproteases, have been characterized in different pathological conditions, such as melanoma (Allard et al. 2011) and juvenile idiopathic arthritis (Prigione et al. 2011). Moreover, it has been demonstrated that sHLA-E is released by endothelial cells upon activation (Coupel et al. 2007).
A strong correlation between HLA-E and HLA-G has been demonstrated in physiological and pathological conditions (Rabot et al. 2005; Kren et al. 2011). HLA-G expression and function have been characterized in the last years in patients with multiple sclerosis (MS), a chronic inflammatory disease of the central nervous system (CNS) of autoimmune pathogenesis (Goverman 2009). HLA-G has an important role in MS, since i) cerebrospinal fluid (CSF) levels and intrathecal synthesis (ITS) of sHLA-G are increased in MS with respect to controls and associated with clinical and radiological evidence of disease remission (Fainardi et al. 2003, 2006), ii) elevated sHLA-G in CSF correlates with the presence of an anti-inflammatory and pro-apoptotic intrathecal microenvironment (Fainardi et al. 2003, 2008) and is predominantly composed of HLA-G5 isoform (Fainardi et al. 2007), iii) HLA-G expression is high within and around MS lesions and on monocytes in CSF of MS patients (Wiendl et al. 2005), and iv) HLA-G+ regulatory T cells are recruited in CNS and highly represented in CSF and inflammatory brain lesions of MS patients (Huang et al. 2009).
With this background, we have here investigated i) the presence of sHLA-E in serum and CSF from MS patients and controls, ii) correlations between sHLA-E and sHLA-G concentration in CSF, and iii) correlations between serum and CSF levels of sHLA-E, clinical/radiological disease activity and clinical features in RRMS patients.
Materials and methods
Patients
The approvals of the Committee for Medical Ethics in Research of the University of Ferrara and of the Ethical Committee of the G. Gaslini Institute have been obtained for experiments involving human subjects. Written informed consent was obtained from all subjects participating in the study.
MS patients’ characteristics are summarized in Table 1. CSF and serum samples were collected from 80 patients satisfying the criteria for definite MS according to McDonald classification (McDonald et al. 2001), and admitted to the MS Centre of the Section of Neurology, University of Ferrara. All patients suffered from relapsing remitting (RR) MS, diagnosed according to the Lublin criteria (Lublin and Reingold 1996). Clinically active disease was defined as the occurrence of a relapse at admission (Lublin and Reingold 1996), and patients were classified as clinically active (CA, n = 60) or clinically stable (CS, n = 20). Disease severity was scored at the time of sample collection using Kurtzke’s Expanded Disability Status Score (EDSS) (Kurtzke 1983). At the time of sample collection, patients with i) symptoms of acute infection or ii) who had received potential disease-modifying therapies during the 6 months before the investigation, were excluded from the study.
CSF and serum samples from patients with other inflammatory neurological disorders (OIND, n = 81) and non-inflammatory neurological disorders (NIND, n = 86), free of immunosuppressant drugs at the time of sample collection, were tested as neurological controls. NIND and OIND patients’ characteristics are summarized in Table 2.
CSF specimens were obtained by non-traumatic lumbar puncture performed for diagnostic purposes. Serum samples were prepared by centrifugation of blood specimens withdrawn by puncture of an anterocubital vein at the same time of CSF extraction. Paired CSF and serum samples from MS patients and controls were collected after informed consent (according to the Declaration of Helsinki) under sterile conditions, and stored at −70 °C until tested. All samples were analyzed blind, without knowledge of clinical and radiological findings.
Magnetic resonance imaging technique
Brain magnetic resonance imaging (MRI) scans were performed within 48 h after sampling as previously described (Fainardi et al. 2006). Accordingly, 27 MS patients (24 CA and 3 CS) showing Gadolinium (Gd) enhancement were classified as MRI active (Gd+), and 53 (36 CA and 17 CS) were considered as MRI inactive (Gd−). All brain MRI scans were evaluated blind by one investigator (E.F.).
sHLA-E and sHLA-G specific ELISA
Enzyme-Linked Immunosorbent Assay (ELISA) for sHLA-E was performed as previously described (Prigione et al. 2011). Briefly, MaxiSorp Nunc-Immuno 96 microwell plates (Nunc A/S, Roskilde, Denmark) were coated overnight at 4 °C with 3D12 mAb, specific for HLA-E HC (eBioscience, Science Center Drive, San Diego, CA, USA). After three washes with PBS 0.05 % Tween 20 (washing buffer), plates were saturated with 200 μl/w of PBS 2 % BSA (Sigma, St. Louis, MO, USA) for 30 min at RT. 100 μl of test samples (CSF or sera) or standard (serial dilutions of total extract from normal peripheral blood mononuclear cells) were added to each well and incubated at RT for 2 h. After three washes, 100 μl of detection reagent (HRP-conjugated anti-β2 microglobulin mAb, Exbio, Vestec, CZ) was added, and plates were incubated for 2 h at RT. After three washes, 100 μl of TMB (substrate for HRP), was added, and reaction was stopped after approximately 30′ by adding H2SO4 5N. Absorbance at 450 nm was measured using Infinite® 200 PRO spectrometer (Tecan Group Ltd., Seestrasse, Männedorf, Switzerland). Results are expressed as arbitrary units/ml (1 unit = quantity of sHLA-E in 1 μg of total extract).
sHLA-G ELISA was carried out in undiluted CSF and serum samples as described elsewhere (Fainardi et al. 2003) using as capture antibody the mAb MEM-G9 (Exbio, Praha, Czech Republic), which recognizes the HLA-G molecule in β2-microglobulin associated form, at a concentration of 20 ng/ml. As detecting antibody an anti-β2-microglobulin MoAb conjugated with HRP was used (DakoCytomation, Rødovre, Denmark). The intra-assay coefficient of variation (CV) was 1.4 % and the inter-assay CV was 4.0 %. The limit of sensitivity was 1.0 ng/ml.
According to the IgG Index, intrathecal production of both sHLA-E and sHLA-G was calculated by the following formula: sHLA Index = CSF/serum sHLA: CSF/serum albumin, where the ratio between CSF and serum albumin concentrations represents the status of blood-CSF-barrier. Intrathecal synthesis was assumed for values greater than 3 SD above the mean of NIND.
Human tissue histology
HLA-E expression in human MS and non MS tissues was investigated using 6 μm thick sections of OCT embedded human tissues from 3 post-mortem MS and one non-MS brains provided by the Italian Multiple Sclerosis Brain Bank, Genoa and stored at −80 °C until tested. Tissue sections were layered onto glass slides, frozen, air-dried and fixed in methanol at 4 °C for 20 min. For immunohistochemical analysis, sections were stained with anti-CD45 (Thermo Scientific, 1:50 dilution) or anti-HLA-E (LifeSpan Biosciences, 1:100 dilution) monoclonal antibodies (Abs), using a biotinylated anti-mouse IgG Ab as secondary reagent (UltraVision Plus Detection System, Thermo Scientific). The latter was detected by horseradish peroxidase (HRP) (Sigma Aldrich) and stained tissue sections were examined with an Olympus Provis AX70 optical microscope.
For double immunofluorescent analysis, CD3, CD68, IBA1 and GFAP were detected using specific rabbit polyclonal Abs and Alexa Fluor 594 conjugated anti-rabbit secondary Ab (Molecular Probes, 1:200 dilution). HLA-E was detected using a specific mouse monoclonal Ab and Alexa Fluor 488 conjugated anti-mouse secondary Ab (Molecular Probes, dilution 1:200). Nuclei were counterstained with DAPI (Sigma), followed by fluorescent mounting (DakoCytomation). Negative controls were prepared by omitting either the primary or the secondary antibodies in the double immunofluorescence analysis.
Fluorescence image acquisition was performed by a multi-channel Leica TCS SP5 laser-scanning confocal microscope, equipped with 458, 476, 488, 514, 543 and 633 nm excitation lines. Images (512 × 512 pixels, 12 bit) were taken through a plan-apochromatic oil immersion objective 63×/NA 1.4. Light collection configuration was optimized according to the combination of chosen fluorochromes and sequential channel acquisition was performed to avoid cross-talk phenomena. Leica LasAF software package was used for acquisition, storage and visualization. Each slide was analyzed by counting at least three different fields.
Generation of CTL, NK and dendritic cells from normal donors
The study was approved by the Ethical Committee of the G. Gaslini Institute, Genoa, Italy. Peripheral blood (PB) samples from two normal donors were obtained following written informed consent. Mononuclear cells (MNC) were isolated by Ficoll-Hypaque (Sigma) density gradient.
Monocyte enriched cell populations were then isolated by Percoll (Pharmacia, Uppsala, Sweden) 50.6 % density gradient centrifugation, resuspended in X-VIVO 15® medium (Cambrex) and plated onto 6 well plates (Corning Incorporated, NY, USA) at 2 × 106/well. After 2 h incubation, non adherent cells were removed and adherent cells were cultured in X-VIVO 15® medium with 400 U/ml rGM-CSF (PeproTech EC, London, UK) and 25 ng/ml rIL-4 (ImmunoTools, Friesoythe, Germany) for 5 days to generate immature dendritic cells (iDC). In some experiments, iDC were pulsed with EBNA-1 antigen (Prospec, Rehovot, Israel, 1 μg/ml) for 18 h and then treated with rIL-6 (125 U/ml), rTNF-α (5 ng/ml), rIL-1β (5 ng/ml, Strathmann Biotech AG, Hamburg, Germany) and PGE2 (1 μg/ml) (Sigma-Aldrich, Saint Louis, MO, USA) for 24 h to generate EBNA-1 pulsed mature dendritic cells (mDC).
CD8+ T cell populations were purified from PBMC by immunomagnetic enrichment with CD8 MicroBeads (Miltenyi Biotec GmbH, Bergisch Gladbach, Germany). CD8+ T cells were cultured in 96 well plates (Corning) at 10:1 cell ratio with autologous EBNA-1 pulsed mDC in RPMI 1640 supplemented with 10 % heat inactivated human AB serum and 5 ng/ml rIL-7 (Peprotech). Lymphocytes underwent 3 rounds of weekly stimulation with autologous EBNA-1 pulsed mDC and, starting from the second round of stimulation, 10 ng/ml rIL-15 (Immunotools) were added to the culture medium.
Total NK cells were isolated from PB samples using NK isolation kit (Myltenyi Biotec), following manufacturer’s protocol. NK cells were cultured in RPMI 10 % FBS at 37 ° C and 5 % CO2 with 10 ng/ml IL-15 (Immunotools) for 24 h before being used as effector cells.
Cytotoxicity assay
Epstein–Barr Virus nuclear antigen (EBNA)-1 specific CTL and activated NK cells were pre-treated for 30′ at 37 °C as follows: i) medium alone, ii) HLA-E+/HLA-G− CSF samples from three MS patients, ii) HLA-E−/HLA-G+ CSF samples from three MS patients, iii) HLA-E−/HLA-G− CSF samples from three MS patients, and iv) HLA-E+/HLA-G+ CSF samples from three MS patients. Cells were then used as effector cells in a standard 4 h 51Cr release assay. EBNA-1 specific CTL were tested against autologous EBNA-1 pulsed mDC and activated NK cells were tested against autologous iDC. Effector to target (E:T) cell ratio was 50:1 and 25:1, respectively. Blocking experiments were performed adding to target cells (EBNA-1 pulsed mDC) anti-HLA class I mAb TP25.99 mAb (10 μg/ml) 30 min before culture with EBNA-1 specific CTL. Specific lysis was determined according to the formula: % specific lysis = cpm (sample-spontaneous)/cpm (total-spontaneous) × 100.
Statistical analysis
The normality of each variable was checked by using the Kolmogorov–Smirnov test. When normality of data distribution was found in all variables, statistical analysis was performed by a parametric approach. Conversely, when normality of data distribution was rejected in several variables, a non-parametric analysis was applied. Accordingly, t test or Mann–Whitney test was used to compare CSF and serum mean levels of sHLA-E among the various groups, whereas Chi-square test was used to compare percentages of i) MS, NIND and OIND patients or ii) CA, CS, Gd+ and Gd− MS patients for sHLA-E index analysis. In cases of multiple comparisons, a Bonferroni posthoc correction was applied. As normality of data distribution was not detected in several MS variables, the Spearman rank correlation coefficient test was used to identify possible relationships among different variables. The significance range as follows: *p < 0.05 (significant), **p < 0.005, and ***p < 0.0005.
Results
sHLA-G and sHLA-E concentration in biological samples from MS, NIND and OIND patients
First, concentrations of sHLA-G and -E were tested in serum and CSF samples from MS, OIND and NIND patients. CSF and serum sHLA-G levels were detectable in 56/80 (70 %) and 51/80 (63.75 %) MS, in 32/81 (39.51 %) and 26/81 (32.1 %) OIND and in 15/86 (17.44 %) and 25/86 (29.07 %) NIND patients, respectively, whereas CSF and serum sHLA-E concentrations were measurable in 71/80 (88.75 %) and 77/80 (96.25 %) MS, in 48/81 (59.26 %) and 77/81 (95.06 %) OIND and in 51/86 (59.3 %) and 72/86 (83.72 %) NIND patients, respectively.
sHLA-G concentration has been previously analyzed in biological samples from MS patients (Fainardi et al. 2006, 2007, 2008). Consistently with published data, we found that serum sHLA-G levels were significantly higher in MS patients than in NIND (ng/ml, mean ± SD; MS 6.41 ± 8.25; NIND 2.56 ± 6.01; p < 0.0001) and OIND patients (ng/ml, mean ± SD; OIND 3.23 ± 6.7, p = 0.0006; Fig. 1a). CSF levels of sHLA-G were also significantly higher in MS patients than in NIND (ng/ml, mean ± SD; MS 18.08 ± 19.16; NIND 1.2 ± 7.21; p < 0.0001) and in OIND (ng/ml, mean ± SD; OIND 6.02 ± 12.65; p < 0.0001) patients (Fig. 1b).
sHLA-G and -E concentration in biological samples. sHLA-G and -E concentrations were evaluated by ELISA in serum (a and c, respectively) and CSF (b and d, respectively) samples from 80 MS, 81 OIND and 86 NIND patients. Results are expressed as ng/ml (sHLA-G) or arbitrary units/ml (sHLA-E). Each point represents a single observation. Horizontal bars indicate medians. p values are indicated where difference is statistically significant
In contrast, serum sHLA-E levels were significantly higher in MS patients than in NIND (units/ml, mean ± SD; MS 25.1 ± 27.3; NIND 16.6 ± 24.4; p = 0.0085) but not OIND patients (units/ml, mean ± SD; OIND 21.4 ± 25.7; Fig. 1c). Conversely, as shown in Fig. 1d, CSF levels of sHLA-E were significantly increased in MS patients as compared to either NIND (units/ml, mean ± SD; MS 19.3 ± 21.1; NIND 7.1 ± 8; p = 0.0009) or OIND (units/ml, mean ± SD; OIND 9.5 ± 14.1; p = 0.0022) patients.
Of note, no significant differences were found in demographic, clinical and radiological data between CSF and serum sHLA-G positive and negative MS, OIND and NIND patients (data not shown).
sHLA-E levels are increased in CSF from MS patients and correlate with disease activity
Next, we compared serum and CSF sHLA-E levels between MS patients with i) clinically active (CA) vs clinically stable disease (CS) and ii) MRI active (Gd+) vs MRI inactive (Gd−) disease.
As shown in Fig. 2a, serum levels of sHLA-E were similar in CA MS and CS MS patients (units/ml, mean ± SD; CA 25.5 ± 27.8; CS 23.7 ± 26.5), whereas CSF sHLA-E levels were significantly higher in CS than in CA MS patients (units/ml, mean ± SD; CA 14.7 ± 19.5; CS 30.7 ± 20.9; p = 0.0042). Accordingly, as shown in Fig. 2b, serum levels of sHLA-E were similar in Gd+ and Gd− MS patients (units/ml, mean ± SD; Gd+ 19.5 ± 20.1; Gd− 28 ± 30.2), whereas CSF sHLA-E levels were significantly higher in Gd− than in Gd+ MS patients (units/ml, mean ± SD; Gd+ 10.7 ± 16.1; Gd− 23.8 ± 22.2; p = 0.0081).
Correlations between CSF sHLA-E concentration and disease activity. sHLA-E concentrations were evaluated by ELISA in serum and CSF samples from 60 clinically active (CA) and 20 clinically stable (CS) (a), as well as from 27 Gd+ and 53 Gd− (b) MS patients. Results are expressed as arbitrary units/ml. Each point represents single observations. Horizontal bars indicate medians. p values are indicated where difference is statistically significant
ITS of sHLA-E is increased in MS patients and correlates with disease activity
Next, we analyzed the intrathecal synthesis (ITS) of sHLA-G and sHLA-E. sHLA-G and -E index values were calculated in 47 MS, 52 OIND and 46 NIND patients.
sHLA-G index was significantly higher in MS patients (mean ± SD; 0.53 ± 0.94) than in OIND (mean ± SD; 0.15 ± 0.43, p = 0.0002) and NIND (mean ± SD; 0.01 ± 0.04, p < 0.0001) patients (Fig. 3a), as previously reported (Fainardi et al. 2006). Similarly, sHLA-E index was significantly higher in MS patients (mean ± SD; 0.54 ± 0.74) than in OIND (mean ± SD; 0.16 ± 0.52, p < 0.0001) and NIND (mean ± SD; 0.08 ± 0.15, p < 0.0001) patients (Fig. 3b).
Intrathecal synthesis of sHLA-G and -E. Intrathecal synthesis (ITS), as expressed by sHLA-G (a) and sHLA-E (b) index was calculated in 47 MS (black circles), 52 OIND (white circles) and 46 NIND (white squares) patients. Each point represents single observations. Horizontal bars indicate medians. p values are indicated where difference is statistically significant. c Bars indicate the percentage of MS (black bars), OIND (grey bars), NIND (white bars), CA or Gd+ MS (dark grey), CS or Gd− MS (light grey) patients with a sHLA-E index greater than the calculated cut-off value of 0.54 (3 SD above the mean of NIND). p values are indicated where difference is statistically significant
The cut-off level for sHLA-E index, calculated in NIND patients (as described above), was 0.54. As shown in Fig. 3c, the number of patients with sHLA-E index values above cut-off level was significantly higher in MS patients (15/47, 31.9 %) than in NIND (1/46, 2.17 %, p = 0.0002) and in OIND (3/52, 5.76 %, p = 0.0012) patients.
Next, we analyzed patients with sHLA-E index above cut-off value in i) CA vs CS and ii) Gd+ vs Gd− MS patients. As shown in Fig. 3c, the number of patients with sHLA-E index values above cut-off was significantly higher in CS (8/14, 57.14 %) than in CA MS patients (7/33, 21.21 %, p = 0.03), whereas no significant differences were detected between Gd− (8/30, 26.66 %) and Gd+ (7/17, 41.17 %) MS patients.
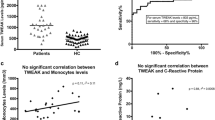
Correlations between sHLA-E, sHLA-G and MS clinical features
We next performed a statistical analysis to correlate serum/CSF levels of sHLA-E and sHLA-E ITS with other parameters, such as disease duration, expanded disability status scale (EDSS) and sHLA-G. sHLA-E levels in CSF positively correlated with disease duration (Fig. 4a, R = 0.32, p = 0.01) and CSF sHLA-G concentrations (Fig. 4b, R = 0.32, p = 0.01). Moreover, sHLA-E index values correlated with disease duration (Fig. 4c, R = 0.44, p = 0.0022) and sHLA-G index values (Fig. 4d, R = 0.26, p = 0.05). No correlations were found between serum sHLA-E levels and any clinical parameter. In particular, no associations emerged between sHLA-G and sHLA-E levels and age, demonstrating that ageing did not influence the associations we observed between sHLA-G and sHLA-E and disease duration (not shown).
Correlations between sHLA-E and other parameters. Correlations between CSF sHLA-E levels (U/ml) and disease duration (a) or CSF sHLA-G levels (b), and between sHLA-E index values and disease duration (c) or sHLA-G index values (d). Each point represents single observations. Lines represent linear regressions
HLA-E positive cells are highly enriched in active MS plaques
In order to assess whether HLA-E is expressed by immune cells infiltrating MS tissues, we stained active MS plaques from three autoptic tissues. Immunohistochemical analyses revealed that HLA-E was highly expressed in active MS plaques (Fig. 5e, f and g) containing an abundant CD45+ cell infiltrate (Fig. 5a, b and c ). In contrast, no expression was detected in white matter specimen from non-MS tissues (Fig. 5d and h).
Immunohistochemical analysis of HLA-E expression in MS plaques HLA-E is expressed in MS plaques (e, f, g) characterized by a rich CD45+ infiltrate (a, b, c). HLA-E and CD45+ are not expressed in the white matter from non-MS tissues (d, h). Analysis was performed with an optical microscope Olympus Provis AX 70, with a 40× Olympus objective; the bar corresponds to 20 μm
Next, we investigated by confocal microscopy the immunophenotype of HLA-E expressing cells within the plaques. Most CD3-positive T cells were found to express HLA-E (Fig. 6a, b, c). A very high number of CD68+ macrophages (Fig. 6d, e, f) and IBA1+ microglia (Fig. 6g, h, i) co-localized with HLA-E. Interestingly, also the majority, but not the totality, of GFAP-positive astrocytes expressed HLA-E. Altogether these results demonstrate that, within active MS plaques, both infiltrating immune cells and resident neural elements express HLA-E.
HLA-E is expressed by immune cells and astrocytes in active MS plaques Immunofluorescence was carried out on samples from frozen MS tissues as it follows: a, d, g, j HLA-E (green channel), b CD3 (red channel), e CD68 (red channel), h IBA-1 (red channel), k GFAP (red channel). Colocalization (merge) of HLA-E with CD3 (c), CD68 (f), IBA-1 (i) and GFAP (l) is depicted. Fluorescence image acquisition was performed by a multi-channel Leica TCS SP5 laser-scanning confocal microscope
Soluble HLA-G and -E in CSF samples synergistically inhibit CTL and NK cell function
Finally, in order to evaluate a possible immunoregulatory function of sHLA-G and -E in CSF samples, we treated EBNA-1 specific CTL and activated NK cells from normal donors with CSF samples from different MS patients, containing or not sHLA-E and/or -G. Next, we tested the cytotoxic activity of these cells against autologous i) EBNA-1 pulsed mDC or ii) iDC, respectively.
NK cells efficiently lysed autologous iDC (% specific lysis: mean ± SD: 61.22 ± 1.88). Such lysis was significantly inhibited when NK cells were pre-treated with i) HLA-G−/HLA-E+ (46.38 ± 3.99, p < 0.0001), ii) HLA-G+/HLA-E− (47.67 ± 1.48, p < 0.0001), iii) HLA-G+/HLA-E+ (43.77 ± 3.87, p < 0.0001) and HLA-G−/HLA-E− (53.92 ± 1.66, p < 0.0001) CSF samples. Moreover, such inhibition was significantly higher using HLA-G+/HLA-E+ CSF samples than HLA-G+/HLA-E− (p = 0.03) or HLA-G−/HLA-E− (p = 0.001) CSF samples (Fig. 7a).
Inhibition of CTL and NK cell mediated cytotoxicity by CSF samples. Cytotoxicity of NK cells vs autologous iDC (a) and EBNA-1 specific CTL vs autologous EBNA-1 pulsed mDC (b). Effector cells were pre-treated with medium alone or CSF samples from MS patients (HLA-E+/HLA-G−, HLA-E−/HLA-G+, HLA-E−/HLA-G−and HLA-E+/HLA-G+). Mean of six different experiments ± SD is shown. p values are indicated where the difference is statistically significant
EBNA-1 specific CTL efficiently lysed autologous EBNA-1 pulsed mDC (% specific lysis: mean ± SD: 32.25 ± 1.04). HLA-restriction was witnessed by a significant reduction of lysis (13.55 ± 3.22, p < 0.0001) achieved by a pre-incubation of target cells with a blocking anti-HLA class I mAb (data not shown).
CTL mediated lysis was significantly inhibited when cells were pre-treated with i) HLA-G−/HLA-E+ (14.3 ± 3.56, p < 0.0001), ii) HLA-G+/HLA-E− (7.46 ± 3.94, p < 0.0001), iii) HLA-G+/HLA-E+ (2.96 ± 3.4, p < 0.0001) and HLA-G−/HLA-E− (25.45 ± 5.8, p < 0.0001) CSF samples. Again, CTL lysis inhibition was significantly higher using HLA-G+/HLA-E+ CSF samples than HLA-G+/HLA-E− (p = 0.01) or HLA-G−/HLA-E− (p = 0.0002) CSF samples (Fig. 7b)
Taken together, these results indicated that, although additional CSF factors beside sHLA-G and -E suppress CTL and NK cell mediated cytotoxicity, sHLA-E in CSF from MS patients has an important immunoregulatory role and synergizes with sHLA-G.
Discussion
We report here for the first time the presence of sHLA-E in serum and CSF samples from MS patients and neurological controls.
We demonstrated that sHLA-E levels were higher in serum from MS patients than in NIND but not OIND patients, thus suggesting that the increased serum sHLA-E concentrations may be related to inflammation rather than reflect a peculiar feature of MS. Accordingly, no correlation was found between serum sHLA-E levels and duration or severity of the disease.
Conversely, the concentrations of sHLA-E in CSF were higher in MS patients than in NIND and OIND patients. Moreover, we showed that increased concentrations of sHLA-E in CSF were present in MS patients with MRI and clinically stable rather than patients with MRI and clinically active disease. Furthermore, we found that ITS of sHLA-E was higher in MS patients than in OIND and NIND patients. The number of patients with a sHLA-E index above the cut-off level was significantly higher in MS than in NIND/OIND patients, and among MS patients, was higher in clinically stable than in clinically active patients.
Taken together, these data suggest that sHLA-E may have a protective role in MS patients, similarly to that observed for sHLA-G (Fainardi et al. 2003, 2006, 2007, 2008). In addition, these findings were in accordance with the recent demonstration that RNA and protein HLA-E expression were increased in active MS white matter lesions (Durrenberger et al. 2012). sHLA-E may cooperate with sHLA-G in the resolution of intrathecal inflammatory response, inhibiting NK cell and CTL function. In this line, we have demonstrated that CSF samples containing both sHLA-G and -E are more effective in vitro in the inhibition of CTL and NK cell mediated lysis than i) CSF samples containing sHLA-G alone or ii) CSF samples negative for both sHLA-G and -E.
Moreover, a good correlation between CSF levels and ITS of sHLA-E and those of sHLA-G was detected, thus further supporting the hypothesis that these two molecules act synergistically in the control of intrathecal inflammation during MS, as previously demonstrated in other physiological and pathological conditions (Rabot et al. 2005; Kren et al. 2011). In addition, we demonstrated that CSF levels of sHLA-E and ITS of sHLA-E correlated with disease duration, thus indicating that the increased concentration of this molecule in CSF may have an important role in the control of the disease.
The role of HLA-G in MS has been unraveled, for the first time, by our group (Fainardi et al. 2003). We showed that CSF levels of sHLA-G were higher in MS patients than in controls and in MS patients with clinically inactive than clinically active disease (Fainardi et al. 2003). The implication of HLA-G in MS was then confirmed by various subsequent studies over the last years (Wiendl et al. 2005; Fainardi et al. 2006, 2007, 2008; Huang et al. 2009). It has been suggested that sHLA-G in CSF may be secreted by infiltrating monocytes and microglial cells, and in addition, generated by shedding of the membrane-bound molecule expressed on HLA-G+ regulatory CD4+ and CD8+ T cells (Fainardi et al. 2011). Limited information is available as to the cellular sources of sHLA-E. In this line, we have recently demonstrated that HLA-E is up-regulated on the surface of infiltrating T and B cells from synovial fluid in juvenile idiopathic arthritis patients, as compared to paired peripheral blood, suggesting that the expression of this molecule may be increased in activated auto-reactive cells (Prigione et al. 2011). Moreover, HLA-E expression on normal glial cells has been recently documented (van Velzen et al. 2009). Accordingly, we have here demonstrated that both infiltrating immune cells (T lymphocytes and macrophages) and resident cells (microglial cells and astrocytes) expressed HLA-E within active MS plaques.
In conclusion, we have described here for the first time the expression and function of the immunoregulatory molecule HLA-E in MS. Our data suggest a potential role for sHLA-E, synergistic with sHLA-G, in the termination of neuroinflammation in MS patients, that is related to remission of the disease. In this respect, sHLA-E in the CSF may represent a novel, promising biomarker of disease activity in MS to be validated in future studies.
References
Allard M, Oger R, Vignard V, Percier JM, Fregni G, Perier A, Caignard A, Charreau B, Bernardeau K, Khammari A, Dreno B, Gervois N (2011) Serum soluble HLA-E in melanoma: a new potential immune-related marker in cancer. PLoS One 6:e21118
Braud VM, Allan DS, Wilson D, McMichael AJ (1998a) TAP- and tapasin-dependent HLA-E surface expression correlates with the binding of an MHC class I leader peptide. Curr Biol 8:1–10
Braud VM, Allan DS, O’Callaghan CA, Soderstrom K, D’Andrea A, Ogg GS, Lazetic S, Young NT, Bell JI, Phillips JH, Lanier LL, McMichael AJ (1998b) HLA-E binds to natural killer cell receptors CD94/NKG2A, B and C. Nature 391:795–799
Coupel S, Moreau A, Hamidou M, Horejsi V, Soulillou JP, Charreau B (2007) Expression and release of soluble HLA-E is an immunoregulatory feature of endothelial cell activation. Blood 109:2806–2814
Durrenberger PF, Webb LV, Sim MJ, Nicholas RS, Altmann DM, Boyton RJ (2012) Increased HLA-E expression in white matter lesions in multiple sclerosis. Immunology 137:317–325
Fainardi E, Rizzo R, Melchiorri L, Vaghi L, Castellazzi M, Marzola A, Govoni V, Paolino E, Tola MR, Granieri E, Baricordi OR (2003) Presence of detectable levels of soluble HLA-G molecules in CSF of relapsing-remitting multiple sclerosis: relationship with CSF soluble HLA-I and IL-10 concentrations and MRI findings. J Neuroimmunol 142:149–158
Fainardi E, Rizzo R, Melchiorri L, Castellazzi M, Paolino E, Tola MR, Granieri E, Baricordi OR (2006) Intrathecal synthesis of soluble HLA-G and HLA-I molecules are reciprocally associated to clinical and MRI activity in patients with multiple sclerosis. Mult Scler 12:2–12
Fainardi E, Rizzo R, Melchiorri L, Stignani M, Castellazzi M, Caniatti ML, Baldi E, Tola MR, Granieri E, Baricordi OR (2007) Soluble HLA-G molecules are released as HLA-G5 and not as soluble HLA-G1 isoforms in CSF of patients with relapsing-remitting multiple sclerosis. J Neuroimmunol 192:219–225
Fainardi E, Rizzo R, Melchiorri L, Stignani M, Castellazzi M, Tamborino C, Paolino E, Tola MR, Granieri E, Baricordi OR (2008) CSF levels of soluble HLA-G and Fas molecules are inversely associated to MRI evidence of disease activity in patients with relapsing-remitting multiple sclerosis. Mult Scler 14:446–454
Fainardi E, Castellazzi M, Stignani M, Morandi F, Sana G, Gonzalez R, Pistoia V, Baricordi OR, Sokal E, Pena J (2011) Emerging topics and new perspectives on HLA-G. Cell Mol Life Sci 68:433–451
Garcia P, Llano M, de Heredia AB, Willberg CB, Caparros E, Aparicio P, Braud VM, Lopez-Botet M (2002) Human T cell receptor-mediated recognition of HLA-E. Eur J Immunol 32:936–944
Goverman J (2009) Autoimmune T cell responses in the central nervous system. Nat Rev Immunol 9:393–407
Huang YH, Zozulya AL, Weidenfeller C, Metz I, Buck D, Toyka KV, Bruck W, Wiendl H (2009) Specific central nervous system recruitment of HLA-G(+) regulatory T cells in multiple sclerosis. Ann Neurol 66:171–183
Kren L, Slaby O, Muckova K, Lzicarova E, Sova M, Vybihal V, Svoboda T, Fadrus P, Lakomy R, Vanhara P, Krenova Z, Sterba J, Smrcka M, Michalek J (2011) Expression of immune-modulatory molecules HLA-G and HLA-E by tumor cells in glioblastomas: an unexpected prognostic significance? Neuropathology 31:129–134
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1444–1452
Le Bouteiller P, Lenfant F (1996) Antigen-presenting function(s) of the non-classical HLA-E, -F and -G class I molecules: the beginning of a story. Res Immunol 147:301–313
Llano M, Lee N, Navarro F, Garcia P, Albar JP, Geraghty DE, Lopez-Botet M (1998) HLA-E-bound peptides influence recognition by inhibitory and triggering CD94/NKG2 receptors: preferential response to an HLA-G-derived nonamer. Eur J Immunol 28:2854–2863
Lu L, Kim HJ, Werneck MB, Cantor H (2008) Regulation of CD8+ regulatory T cells: interruption of the NKG2A-Qa-1 interaction allows robust suppressive activity and resolution of autoimmune disease. Proc Natl Acad Sci U S A 105:19420–19425
Lublin FD, Reingold SC (1996) Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis. Neurology 46:907–911
McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP, Lublin FD, McFarland HF, Paty DW, Polman CH, Reingold SC, Sandberg-Wollheim M, Sibley W, Thompson A, van den Noort S, Weinshenker BY, Wolinsky JS (2001) Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol 50:121–127
O’Callaghan CA, Bell JI (1998) Structure and function of the human MHC class Ib molecules HLA-E, HLA-F and HLA-G. Immunol Rev 163:129–138
Pietra G, Romagnani C, Mazzarino P, Falco M, Millo E, Moretta A, Moretta L, Mingari MC (2003) HLA-E-restricted recognition of cytomegalovirus-derived peptides by human CD8+ cytolytic T lymphocytes. Proc Natl Acad Sci U S A 100:10896–10901
Pistoia V, Morandi F, Wang X, Ferrone S (2007) Soluble HLA-G: are they clinically relevant? Semin Cancer Biol 17:469–479
Prigione I, Penco F, Martini A, Gattorno M, Pistoia V, Morandi F (2011) HLA-G and HLA-E in patients with juvenile idiopathic arthritis. Rheumatology (Oxford) 50:966–972
Rabot M, Tabiasco J, Polgar B, Aguerre-Girr M, Berrebi A, Bensussan A, Strbo N, Rukavina D, Le Bouteiller P (2005) HLA class I/NK cell receptor interaction in early human decidua basalis: possible functional consequences. Chem Immunol Allergy 89:72–83
van Velzen M, Laman JD, Kleinjan A, Poot A, Osterhaus AD, Verjans GM (2009) Neuron-interacting satellite glial cells in human trigeminal ganglia have an APC phenotype. J Immunol 183:2456–2461
Wiendl H, Feger U, Mittelbronn M, Jack C, Schreiner B, Stadelmann C, Antel J, Brueck W, Meyermann R, Bar-Or A, Kieseier BC, Weller M (2005) Expression of the immune-tolerogenic major histocompatibility molecule HLA-G in multiple sclerosis: implications for CNS immunity. Brain 128:2689–2704
Acknowledgments
We thank Mrs. Camilla Valentino for excellent secretarial assistance. This work have been supported by Ministero del Lavoro, della Salute e delle Politiche Sociali (Progetti di Ricerca Corrente) and by Research Program Regione Emilia Romagna - University 2007–2009, (Innovative Research) - code PRUa1a-2007–008. The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morandi, F., Venturi, C., Rizzo, R. et al. Intrathecal Soluble HLA-E Correlates with Disease Activity in Patients with Multiple Sclerosis and may Cooperate with Soluble HLA-G in the Resolution of Neuroinflammation. J Neuroimmune Pharmacol 8, 944–955 (2013). https://doi.org/10.1007/s11481-013-9459-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11481-013-9459-3