Abstract
Methamphetamine (METH) addiction is prevalent among individuals with HIV infection. We hypothesize that HIV-positive individuals are more prone to METH use and to the development of METH dependence. To test this hypothesis, we examined the effects of METH (daily intraperitoneal injection 2.5 mg/kg for 6 days) on rearing and head movement in 12–13-week-old male HIV-1 transgenic (HIV-1Tg) rats compared to F344 control rats as an indicator of behavioral sensitization, also representing neural adaptation underlying drug dependence and addiction. Body and brain weights were also recorded. The involvement of the dopaminergic system was investigated by examining dopamine receptors 1 (D1R) and 2 (D2R) and dopamine transporter (DAT) expression in the striatum and prefrontal cortex. METH increased rearing number and duration in both F344 and HIV-1Tg rats. Rearing number was attenuated over time, whereas rearing duration remained constant. METH also induced a progressive increase in stereotypical head movement in both F344 and HIV-1Tg rats, but it was greater in the HIV-1Tg rats than in the F344 animals. The brain to body weight ratio was significantly lower in METH-treated HIV-1Tg rats compared to F344 controls. There was no significant difference in striatal D1R, D2R, or DAT messenger RNA in HIV-1Tg and F344 rats. However, D1R expression was greater in the prefrontal cortex of HIV-1Tg rats than F344 rats and was attenuated by METH. Our results indicate that METH-induced behavioral sensitization is greater in the presence of HIV infection and suggest that D1R expression in the prefrontal cortex may play a role in METH addiction in HIV-positive individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of methamphetamine (METH), a highly addictive stimulant drug, is prevalent in the USA, especially among homosexual men, where its use is reportedly 30 times greater than in the general US population (Rhodes et al. 2007). Male homosexuals are also at a higher risk for HIV infection, up to 19 times more likely to be infected than the general population globally (Baral et al. 2007). Conversely, HIV-positive individuals are more likely to use METH than HIV-negative individuals (Molitor et al. 1998). One possible motivation for METH use by HIV-positive individuals is that the drug might help them to cope with their diagnosis and make them feel better physically (Semple et al. 2002). HIV patients may self-medicate with METH to overcome their HIV-related depression, fatigue, and neuropathic pain (Robinson and Rempel 2006). Since METH use is associated with more risky sexual behavior, some researchers have even suggested that treatment for METH abuse should be an essential part of HIV prevention (Colfax and Shoptaw 2005). Thus, there appears to be a bidirectional link between METH use and HIV infection. The possibility that HIV infection may enhance an individual’s addictive behavior, including the use of addictive drugs such as METH, has not been explored.
METH is similar in chemical structure to dopamine. It can be taken up by the dopamine transporter (DAT), enter dopamine neurons, and cause massive release of dopamine into the synaptic cleft (Coutinho et al. 2008). The effects of dopamine are mediated by at least two receptor subtypes, D1 and D2, which are coupled to the activation and inhibition of adenylate cyclase (Stoof and Kebabian 1981; Pollack 2004), respectively. Both the D1 receptor (D1R) and D2 receptor (D2R) are involved in METH-induced behavioral sensitization (BS; Ujike et al. 1989; Hamamura et al. 1991; Kelly et al. 2008). An altered striatal dopaminergic tone, such as that induced by recurrent or chronic METH use, may change the “reward circuitry.” When these circuits are “overloaded,” the increase in synaptic dopamine reinforces reward-seeking behavior, leading to addiction. HIV-1 infection or exposure to HIV viral proteins leads to damages in the dopaminergic terminals and dopaminergic deficits (Gelman et al. 2006; Chang et al. 2008) with decreased dopamine release (Ferris et al. 2009), which may lead to abuse of psychostimulant drugs that would increase dopamine release. Thus, based on various clinical and preclinical reports that HIV infection may alter dopaminergic pathways, we hypothesize that HIV-positive individuals are more prone to METH use than HIV-negative persons and that alterations in the expression of the dopamine receptors and dopamine transporters in the brain may be involved in the mechanisms underlying such reward-seeking behavior.
In rodents, repeated exposure to METH causes increased locomotor activity (such as rearing) and stereotypic behavior (such as repeated head movements). These behavioral changes are termed BS, which is thought to reflect some aspects of neuronal adaptation underlying drug dependence and addiction (Robinson and Berridge 1993, 2008). To test our hypothesis, we treated HIV-1 transgenic (HIV-1Tg) rats and F344 background control rats with METH and then compared BS (including rearing and repetitive head movement). The HIV-1Tg rat is a useful model since it carries the gag-pol deleted HIV-1 provirus and expresses seven of the nine HIV-1 genes, which mimics the persistent low level of infection and exposure to HIV viral proteins in individuals stably treated with antiretroviral medications (Reid et al. 2001, 2004; Ray et al. 2003). Both the brain and body weights of the rats were recorded. In addition, we assayed D1R, D2R, and DAT messenger RNA (mRNA) expression in the striatum and prefrontal cortex of the HIV-1Tg and F344 control rats with and without METH treatment to investigate a possible mechanism underlying addictive behavior.
Materials and methods
Animals
HIV-1Tg rats, derived from the Fisher 344/NHsd Sprague-Dawley background, were generated using a construct derived from the infectious HIV-1 provirus, pNL4-3, after deletion of a 3.1-kb Sph1-Bal1 fragment that overlaps the gag and pol genes (pNL4-3:d1443; Reid et al. 2001). These rats are commercially available (Harlan, Indianapolis, IN, USA). Nontransgenic Fisher 344/NHsd Sprague-Dawley rats (F344) were used as controls. The animals were housed in a temperature-controlled environment (21–22°C) with standard rat diet and water available ad libitum in a 12-h light/dark cycle. The experimental procedures were approved by the Institutional Animal Care and Use Committee at Seton Hall University.
METH administration and behavioral observations
METH ([+]methamphetamine hydrochloride, catalog # M-8750, Sigma-Aldrich Co., St. Louis, MO, USA) was dissolved in saline (1.25 mg/mL) for intraperitoneal (i.p.) injection. Eight male HIV-1Tg rats and eight male F344 rats (12 weeks old) were double-caged and allowed to adapt to the environment for 5 days. After 2 days of habituation to the injection procedure (saline, 2 mL/kg per day, i.p.), each group of animals was randomly subdivided into two groups and treated for 6 days with either 2.5 mg/kg per day METH or 2 mL/kg per day saline. The four groups of animals (n = 4 ea) were designated as HIV-1Tg + METH, HIV-1Tg + saline, F344 + METH, and F344 + saline. Following each injection, locomotor activity (rearing) and stereotypic behavior (repeated head movement) were scored for 2 min at 45, 90, 135, and 180 min. The rearing event was defined as both front paws raised from the ground with the rat standing on its hind paws. The repeated head movements were operationalized as lateral or circular motion; strictly vertical head movements were excluded. This time frame was chosen because the blood level of METH in the METH-treated rats is reported to be the highest within this time interval (Cho et al. 2001).
Brain dissection
Approximately 24 h following the last METH administration, the rats were sacrificed by decapitation; the brain from each animal was collected and weighed using a top load balance (Mettler PM 600 Electronic Balance, Mettler Instrument Corp., Hightstown, NJ, USA), and the ratio of the brain weight to the whole body weight prior to sacrifice was calculated. The brain was dissected on wet ice into various areas, including the striatum and prefrontal cortex, frozen on dry ice, and stored at −80°C until RNA isolation for real-time reverse-transcriptase polymerase chain reaction (RT-PCR) analysis.
RNA isolation, reverse transcription of RNA, and SYBR-green-based real-time PCR
Total RNA from the striatum and prefrontal cortex was extracted using TRIzol reagent according to the manufacturer’s protocol (cat. # 15596-018, Invitrogen, Carlsbad, CA, USA). One microgram of total RNA was reverse-transcribed into complementary DNA (cDNA) in a GeneAmp PCR System 2400 (Perkin Elmer, Waltham, MA, USA) for 1 h at 37°C and then for 10 min at 67°C. Real-time PCR assays were performed to compare D1R, D2R, and DAT mRNA expression in the striatum and prefrontal cortex of the four groups of rats. The primer sequences of the forward and reverse primers used in this study are listed in Table 1. A 2-μL aliquot of the cDNA was amplified in a 25-μL reaction system, including 12.5 μL of 2× SYBR Green PCR Master Mix (cat. # 4364346, Applied Biosystems, UK) and 0.35 μL of each 20-μM primer (Integrated DNA Technologies, Coralville, IA, USA) using an ABI 7000. The glyceraldehyde-3-phosphate dehydrogenase gene was used as an internal standard to normalize the Ct value of each sample. The relative level of gene expression was recorded as the fold of F344 + saline control by using the 2−ΔΔCT method.
Statistical analysis
Behavioral data were analyzed using three-way analysis of variance (ANOVA) with repeated measures over time, followed by a Student’s t test for comparing METH-induced locomotor and stereotypic increments between the F344 and HIV-1Tg rats on each day. Group differences in relative brain weights and relative gene expression levels in the striatum and prefrontal cortex were compared using a one-way ANOVA. All data were analyzed by SPSS 15.0 software and expressed as the mean ± SEM. Differences were considered significant at P < 0.05.
Results
Behavioral observations
Rearing
Rearing behavior has been used previously as a measure of locomotor effects (Neubert et al. 2007). The number and duration of rearings were scored for 2 min at 45, 90, 135, and 180 min following treatment with either 2.5 mg/kg per day METH or 2 mL/kg per day saline for 6 days. Total number and cumulative duration of rearing events were then calculated in each group. Before METH treatment, HIV-1Tg rats showed a trend for lower rearing counts compared to F344 rats (F (1, 6) = 4.658, P = 0.074). The number of rearings was increased following METH treatment in both the F344 and HIV-1Tg rats compared to saline-treated animals (Fig. 1a, F (1, 13) = 64.095, P < 0.01). However, the METH-induced rearings became attenuated over time (Fig. 1a, F (5, 65) = 8.128, P < 0.01), especially in the F344 group but not in the HIV-1Tg group. The difference in the METH-induced attenuation led to a greater increase in the number of rearings in the HIV-1Tg rats than in the F344 animals on days 4 (P < 0.05), 5 (P < 0.05), and 6 (P < 0.01; Fig. 1b). There was also a significant increase in the cumulative duration of rearings following METH treatment in both the F344 and HIV-1Tg rats compared to saline-treated animals (Fig. 1c, F (1, 13) = 82.769, P < 0.01) but no significant change in the cumulative duration of rearings over time (Fig. 1c, F (5,65) = 0.954, P = 0.453) or in the cumulative duration of rearings between the HIV-1Tg rats and the F344 animals on those days (Fig. 1d, P > 0.05).
a Rearing counts in HIV-1Tg and F344 rats. The daily number of rearings in the four groups of rats (F344 + saline, HIV-1Tg + saline, F344 + METH, HIV-1Tg + METH) was determined for 6 days within 3 h following administration of 2.5 mg/kg per day METH or 2 mL/kg per day saline. b Comparison of METH-induced rearing in F344 and HIV-1Tg rats. *P < 0.05, **P < 0.01. c Rearing duration in HIV-1Tg and F344 rats. The daily rearing duration in the four groups of rats (F344 + saline, HIV-1Tg + saline, F344 + METH, HIV-1Tg + METH) was determined for 6 days within 3 h following administration of 2.5 mg/kg per day METH or 2 mL/kg per day saline. d Comparison of METH-induced rearing duration in F344 and HIV-1Tg rats
Head movement
The number of head movements was scored for 2 min at 45, 90, 135, and 180 min after treatment for 6 days with either 2.5 mg/kg per day METH or 2 mL/kg per day saline. With saline treatment, HIV-1Tg rats showed nonsignificantly fewer head movements than the F344 rats. With METH treatment, head movement counts were significantly higher in both the F344 and HIV-1Tg rats than in the saline-treated controls (Fig. 2a, F (1, 13) = 281.550, P < 0.01); however, the HIV-1Tg + METH rats had even greater head movements than the F344 control animals (Fig. 2a, F (1, 13) =5.529, P < 0.05). In addition, there was a significant progressive augmentation of head movement in both F344 and HIV-1Tg rats over time compared to saline-treated controls (Fig. 2a, F (5, 65) = 28.710, P < 0.01 and F (5, 65) = 29.632, P < 0.01, respectively), with the greater increase occurring in the HIV-1Tg rats on days 2, 3, 4, 5, and 6 (Fig. 2b).
a Head movement in HIV-1Tg and F344 rats. The daily head movement in the four groups of rats (F344 + saline, HIV-1Tg + saline, F344 + METH, HIV-1Tg + METH) was determined for 6 days within 3 h following administration of 2.5 mg/kg per day METH or 2 mL/kg per day saline. b Comparison of METH-induced head movement in F344 and HIV-1Tg rats. *P < 0.05, **P < 0.01
The above behavioral assessments were repeated three times (with four animals per group) and we found similar results with each experiment.
Relative brain weights
The relative brain weights were obtained by calculating the ratio of brain weight to body weight. There was no significant difference in the relative brain weight of F344 + saline rats and HIV-1Tg + saline rats; however, the relative brain weight was significantly lower in the HIV-1Tg + METH rats than in the F344 + METH rats (P < 0.05; Fig. 3). The above difference was due to a trend for increase in the mean relative brain weight in METH-treated F344 rats (the ratio of brain weight to body weight is from 0.00728 to 0.00762, P = 0.083) and a nonsignificant decrease in the mean relative brain weight in METH-treated HIV-1Tg rats (the ratio is from 0.00713 to 0.00705, P = 0.813).
Reverse transcription of RNA and SYBR-green-based real-time RT-PCR
Striatum
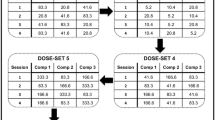
RNA from the striata of METH-treated HIV-1Tg rats and F344 rats was extracted and subjected to real-time RT-PCR analysis for D1R, D2R, and DAT expression. Striatal D1R, D2R, and DAT expressions were not different between the four groups of rats. As for the D1R to D2R ratio, there was no significant effect of either METH (F344 + METH rats) or HIV-1 infection alone (HIV-1Tg + saline rats), but there was a trend toward a higher D1R to D2R ratio in the HIV-1Tg + METH rats compared to the F344 + saline control animals (P = 0.066), which resulted from a slightly higher D1R, but no change in D2R (Fig. 4), which may be due to a synergistic effect of HIV-1 and METH.
Dopamine receptors 1 and 2 and dopamine transporter expression in the striatum of HIV-1Tg and F344 rats. Expression of dopamine receptor 1 (D1R), dopamine receptor 2 (D2R), and dopamine transporter (DAT), and the ratio of D1R to D2R in the striatum were determined in the four groups of rats (F344 + saline, HIV-1Tg + saline, F344 + METH, HIV-1Tg + METH) following administration of 2.5 mg/kg per day METH or 2 mL/kg per day saline. P = 0.066
Prefrontal cortex
The D1R expression level and the D1R to D2R ratio were greater in the prefrontal cortex of the HIV-1Tg rats than in the F344 rats, and the elevated D1R expression level was attenuated by METH. There was no significant difference in D2R and DAT expression in the prefrontal cortex between the four groups of rats (Fig. 5). Due to large individual variations in the HIV-1Tg + saline rats, the higher mean DAT expression did not reach significance in comparison with the other groups.
Dopamine receptors 1 and 2 and dopamine transporter expression in the prefrontal cortex of HIV-1Tg and F344 rats. The expression of dopamine receptor 1 (D1R), dopamine receptor 2 (D2R), and dopamine transporter (DAT), and the ratio of D1R/D2R in the prefrontal cortex were determined in the four groups of rats (F344 + saline, HIV-1Tg + saline, F344 + METH, HIV-1Tg + METH) following administration of 2.5 mg/kg per day METH or 2 mL/kg per day saline. *P < 0.05, **P < 0.01
Discussion
In rodents, a low-to-moderate dose of a psychostimulant such as METH produces an increase in locomotor activity (such as rearing). A higher dose results in the emergence of focused stereotypic behavior (such as repetitive head movements) and a resultant decrease in locomotion, including rearing. The gradual and incremental increase in drug-induced locomotion and stereotypic behavior is usually referred to as BS. BS induced by a psychostimulant in rodents has been considered as a model of drug addiction and is accompanied by adaptations in neural circuits that include those in the prefrontal cortex and striatal regions. Repetitive drug exposure induces incremental adaptive changes in the brain that may eventually lead to pathological craving and addictive behavior (compulsive drug seeking and drug taking; Schenk and Partridge 1997; Robinson and Kolb 2004; Brady et al. 2005; Jedynak et al. 2007; Robinson and Berridge 1993, 2008).
In our study, the HIV-1Tg + saline rats showed less rearing than the F344 + saline rats, which is consistent with possible damages to the dopaminergic terminals that were associated with psychomotor slowing in patients with HIV-1 infection (Wang et al. 2004; Chang et al. 2008). With METH treatment, rearing (locomotive) activity initially increased in both the HIV-1Tg and F344 control rats, but this increased rearing attenuated over time with continued METH administration in the F344 rats but not in the HIV-1Tg rats. These findings suggest the development of tolerance to the dose of METH administered in the F344 rats but not in the HIV-1Tg rats. At the same time, METH induced a progressive increase in stereotypical head movement in both F344 and HIV-1Tg rats. These results indicate that BS occurred in all animals as a result of chronic exposure to METH over time. However, the greater METH-induced locomotive activity and stereotypical head movement in the HIV-1Tg rats than in the F344 rats suggests that METH may induce greater BS in the presence of HIV infection.
Previous studies have shown that brain dopaminergic pathways play an important role in the development and expression of BS (Robinson and Berridge 1993, 2008). Repeated exposure to drugs such as to METH or cocaine causes dopaminergic systems to become hypersensitive, which is coupled to BS and the motivational incentive properties of drugs (Robinson and Berridge 1993, 2008). The effects of HIV infection and METH on the central nervous system are distinct, but they may converge on common pathways, particularly those involving the dopaminergic system (Ferris et al. 2008). Patients with HIV/AIDS often present with Parkinsonian symptoms, such as motor or psychomotor slowing, that reflect decreased dopaminergic synaptic transmission (Chang et al. 2008). Acutely, the HIV viral protein, TAT, has been shown to be toxic to the dopaminergic system by evoking an overflow of dopamine in the striatum of rats (Cass et al. 2003). However, with chronic exposure to HIV viral proteins, the damages to the dopaminergic neurons and their terminals would lead decrease dopamine release and possibly an upregulation of the postsynaptic dopaminergic receptors to compensate for the decreased dopaminergic transmission. This upregulation of the postsynaptic dopaminergic receptors, in turn, may lead to an enhanced responsiveness to METH, and produce greater sensitization in the HIV-infected individual, similar to our findings of greater BS in our HIV-1Tg rats.
METH is chemically similar to dopamine. Both dopamine receptors, D1R and D2R, are involved in METH-induced BS (Ujike et al. 1989; Hamamura et al. 1991; Kelly et al. 2008). In our study, dopamine receptor expression in the striatum was not affected by either METH (F344 + METH) or by HIV-1 effects alone (HIV-1Tg + saline rats), but there was a trend toward a higher D1R to D2R ratio in the HIV-1Tg + METH rats compared to the F344 + saline control animals, which resulted from the slightly higher (upregulated expression of) D1 receptors in the HIV-1Tg + METH group. Furthermore, both D1R expression and the D1R to D2R ratio were higher in the prefrontal cortex of the HIV-1Tg rats compared to F344 rats without exposure to METH, and these elevations were attenuated by METH. The differences in dopamine receptors between the striatum and prefrontal cortex may be one of the reasons that HIV-1Tg rats show greater BS and that attenuated D1R upregulation in the prefrontal cortex may be an adaptive response to repetitive METH stimulation. Drug abuse can alter mesolimbic dopamine reward pathways and result in uncontrolled cravings (“go” signals). Drug abuse can also alter the decision-making prefrontal cortex, which suppresses inappropriate reward responses (“stop” signals). Alterations in the signals in these two brain regions may lead to uncontrolled use despite severe consequences (Clay et al. 2008).
There have been some reports that the METH-induced changes in D1R, D2R, and DAT are not due to changes in the level of expression but, rather, changes in the function of these proteins. For example, in METH-sensitized animals, there is an increase in high-affinity states of D1R and D2R in the striatum but no change in density (Shuto et al. 2008), and, while there is no change in DAT protein level in the striatum, the kinetics of DAT are changed (Bjorklund et al. 2008; Ferris et al. 2008). Our results suggest that elevated D1R expression in the prefrontal cortex of HIV-positive individuals may play a role in the development of drug addiction. However, many more studies are needed to further clarify the involvement of the dopaminergic pathways in METH addiction in HIV-infected individuals.
BS induced by a psychostimulant is accompanied by neuroadaptation in the brain. In addition to changes in the dopamine system, we also showed that the relative brain weight was significantly lower in the HIV-1Tg + METH rats than in the F344 + METH rats. The higher mean relative brain weight in METH-treated F344 rats may reflect METH-mediated neuroinflammation, while the lower mean relative brain weight in METH-treated HIV-1Tg rats may reflect brain atrophy due to ongoing brain injury. These findings are also consistent with magnetic resonance imaging studies which found larger striatal and parietal brain volumes in METH users (Chang et al. 2005; Jernigan et al. 2005), whereas those with chronic HIV infection typically showed smaller brain volumes, primarily in striatal structures but also in cortical regions (Thompson et al. 2005; Ances et al. 2006).
METH can induce behavioral effects and neurotoxicity, depending on dosage and duration of METH administration. The neurotoxic dose is approximately 20 to 30 times higher than the dose that produces behavioral effects, such as locomotion and stereotypy (Seiden and Ricaurte 1987). Several studies have reported that various addictive drugs, especially METH, may synergize with HIV proteins such as TAT to cause dopaminergic neurotoxicity in the striatum (Gurwell et al. 2001; Theodore et al. 2006a, b). However, the treatment regimen in our study which resulted in behavioral effects was nonneurotoxic, and no obvious pathological changes were seen (data not shown). Possible explanations include: (1) a nonneurotoxic METH dosage regimen was used; (2) the transgenic rats can only express very low HIV-1 viral protein levels; and (3) these rats are still young, so the duration of exposure to the viral proteins may not be long enough to cause pathological changes. Nevertheless, the data from this study clearly demonstrate that the HIV-1Tg rat can be a useful model to study METH-induced BS, as well as to explore the mechanisms of drug addiction in HIV-positive individuals. Further studies on the expression levels of viral proteins, such as gp120 and TAT, in the brain, and any pathological changes that occur in the brain of the HIV-1Tg rat at different ages are being conducted.
References
Ances BM, Roc AC, Wang J, Korczykowski M, Okawa J, Stern J, Kim J, Wolf R, Lawler K, Kolson DL, Detre JA (2006) Caudate blood flow and volume are reduced in HIV+ neurocognitively impaired patients. Neurology 66:862–866. doi:10.1212/01.wnl.0000203524.57993.e2
Baral S, Sifakis F, Cleghorn F, Beyrer C (2007) Elevated risk for HIV infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. PLoS Med 4:e339. doi:10.1371/journal.pmed.0040339
Bjorklund NL, Sorg BA, Schenk JO (2008) Neuronal dopamine transporter activity, density and methamphetamine inhibition are differentially altered in the nucleus accumbens and striatum with no changes in glycosylation in rats behaviorally sensitized to methamphetamine. Synapse 62:736–745. doi:10.1002/syn.20528
Brady AM, Glick SD, O'Donnell P (2005) Selective disruption of nucleus accumbens gating mechanisms in rats behaviorally sensitized to methamphetamine. J Neurosci 25:6687–6695. doi:10.1523/JNEUROSCI.0643-05.2005
Cass WA, Harned ME, Peters LE, Nath A, Maragos WF (2003) HIV-1 protein Tat potentiation of methamphetamine-induced decreases in evoked overflow of dopamine in the striatum of the rat. Brain Res 984:133–142. doi:10.1016/S0006-8993(03)03122-6
Chang L, Cloak C, Patterson K, Grob C, Miller EN, Ernst T (2005) Enlarged striatum in abstinent methamphetamine abusers: a possible compensatory response. Biol Psychiatry 57:967–974. doi:10.1016/j.biopsych.2005.01.039
Chang L, Wang GJ, Volkow ND, Ernst T, Telang F, Logan J, Fowler JS (2008) Decreased brain dopamine transporters are related to cognitive deficits in HIV patients with or without cocaine abuse. Neuroimage 42:869–878. doi:10.1016/j.neuroimage.2008.05.011
Cho AK, Melega WP, Kuczenski R, Segal DS (2001) Relevance of pharmacokinetic parameters in animal models of methamphetamine abuse. Synapse 39:161–166. doi:10.1002/1098-2396(200102)39:2<161::AID-SYN7>3.0.CO;2-E
Clay SW, Allen J, Parran T (2008) A review of addiction. Postgrad Med 120:E01–E07
Colfax G, Shoptaw S (2005) The methamphetamine epidemic: implications for HIV prevention and treatment. Curr HIV/AIDS Rep 2:194–199. doi:10.1007/s11904-005-0016-4
Coutinho A, Flynn C, Burdo TH, Mervis RF, Fox HS (2008) Chronic methamphetamine induces structural changes in frontal cortex neurons and upregulates type I interferons. J Neuroimmune Pharmacol 3:241–245. doi:10.1007/s11481-008-9113-7
Ferris MJ, Mactutus CF, Booze RM (2008) Neurotoxic profiles of HIV, psychostimulant drugs of abuse, and their concerted effect on the brain: current status of dopamine system vulnerability in NeuroAIDS. Neurosci Biobehav Rev 32:883–909. doi:10.1016/j.neubiorev.2008.01.004
Ferris MJ, Frederick-Duus D, Fadel J, Mactutus CF, Booze RM (2009) In vivo microdialysis in awake, freely moving rats demonstrates HIV-1 Tat-induced alterations in dopamine transmission. Synapse 63:181–185. doi:10.1002/syn.20594
Gelman BB, Spencer JA, Holzer CE III, Soukup VM (2006) Abnormal striatal dopaminergic synapses in National NeuroAIDS Tissue Consortium subjects with HIV encephalitis. J Neuroimmune Pharmacol 1:410–420. doi:10.1007/s11481-006-9030-6
Gurwell JA, Nath A, Sun Q, Zhang J, Martin KM, Chen Y, Hauser KF (2001) Synergistic neurotoxicity of opioids and human immunodeficiency virus-1 Tat protein in striatal neurons in vitro. Neuroscience 102:555–563. doi:10.1016/S0306-4522(00)00461-9
Hamamura T, Akiyama K, Akimoto K, Kashihara K, Okumura K, Ujike H, Otsuki S (1991) Co-administration of either a selective D1 or D2 dopamine antagonist with methamphetamine prevents methamphetamine-induced behavioral sensitization and neurochemical change, studied by in vivo intracerebral dialysis. Brain Res 546:40–46. doi:10.1016/0006-8993(91)91156-U
Jedynak JP, Uslaner JM, Esteban JA, Robinson TE (2007) Methamphetamine-induced structural plasticity in the dorsal striatum. Eur J NeuroSci 25:847–853. doi:10.1111/j.1460-9568.2007.05316.x
Jernigan TL, Gamst AC, Archibald SL, Fennema-Notestine C, Mindt MR, Marcotte TD, Heaton RK, Ellis RJ, Grant I (2005) Effects of methamphetamine dependence and HIV infection on cerebral morphology. Am J Psychiatry 162:1461–1472. doi:10.1176/appi.ajp.162.8.1461
Kelly MA, Low MJ, Rubinstein M, Phillips TJ (2008) Role of dopamine D1-like receptors in methamphetamine locomotor responses of D2 receptor knockout mice. Genes Brain Behav 7:568–577. doi:10.1111/j.1601-183X.2008.00392.x
Molitor F, Truax SR, Ruiz JD, Sun RK (1998) Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West J Med 168:93–97
Neubert JK, Rossi HL, Pogar J, Jenkins AC, Caudle RM (2007) Effects of mu- and kappa-2 opioid receptor agonists on pain and rearing behaviors. Behav Brain Funct 3:49. doi:10.1186/1744-9081-3-49
Pollack A (2004) Coactivation of D1 and D2 dopamine receptors: in marriage, a case of his, hers, and theirs. Sci STKE 2004:pe50. doi:10.1126/stke.2552004pe50
Proudnikov D, Yuferov V, Zhou Y, LaForge KS, Ho A, Kreek MJ (2003) Optimizing primer—probe design for fluorescent PCR. J Neurosci Methods 123:31–45
Ray PE, Liu XH, Robinson LR, Reid W, Xu L, Owens JW, Jones OD, Denaro F, Davis HG, Bryant JL (2003) A novel HIV-1 transgenic rat model of childhood HIV-1-associated nephropathy. Kidney Int 63:2242–2253. doi:10.1046/j.1523-1755.2003.00028.x
Reid W, Sadowska M, Denaro F, Rao S, Foulke J Jr, Hayes N, Jones O, Doodnauth D, Davis H, Sill A, O’Driscoll P, Huso D, Fouts T, Lewis G, Hill M, Kamin-Lewis R, Wei C, Ray P, Gallo RC, Reitz M, Bryant J (2001) An HIV-1 transgenic rat that develops HIV-related pathology and immunologic dysfunction. Proc Natl Acad Sci USA 98:9271–9276. doi:10.1073/pnas.161290298
Reid W, Abdelwahab S, Sadowska M, Huso D, Neal A, Ahearn A, Bryant J, Gallo RC, Lewis GK, Reitz M (2004) HIV-1 transgenic rats develop T cell abnormalities. Virology 321:111–119. doi:10.1016/j.virol.2003.12.010
Rhodes SD, Hergenrather KC, Yee LJ, Knipper E, Wilkin AM, Omli MR (2007) Characteristics of a sample of men who have sex with men, recruited from gay bars and Internet chat rooms, who report methamphetamine use. AIDS Patient Care STDS 21:575–583. doi:10.1089/apc.2007.0002
Robinson TE, Berridge KC (1993) The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Brain Res Rev 18:247–291. doi:10.1016/0165-0173(93)90013-P
Robinson TE, Berridge KC (2008) Review: the incentive sensitization theory of addiction: some current issues. Philos Trans R Soc Lond B Biol Sci 363:3137–3146. doi:10.1098/rstb.2008.0093
Robinson TE, Kolb B (2004) Structural plasticity associated with exposure to drugs of abuse. Neuropharmacology 47(Suppl1):33–46. doi:10.1016/j.neuropharm.2004.06.025
Robinson L, Rempel H (2006) Methamphetamine use and HIV symptom self-management. J Assoc Nurses AIDS Care 17:7–14. doi:10.1016/j.jana.2006.07.003
Schenk S, Partridge B (1997) Sensitization and tolerance in psychostimulant self-administration. Pharmacol Biochem Behav 57:543–550. doi:10.1016/S0091-3057(96)00447-9
Seiden LS, Ricaurte GA (1987) Neurotoxicity of methamphetamine and related drugs. In: Meltzer HY (ed) Psychopharmacology: the third generation of progress. Raven, New York, pp 359–366
Semple SJ, Patterson TL, Grant I (2002) Motivations associated with methamphetamine use among HIV+ men who have sex with men. J Subst Abuse Treat 22:149–156. doi:10.1016/S0740-5472(02)00223-4
Shuto T, Seeman P, Kuroiwa M, Nishi A (2008) Repeated administration of a dopamine D1 receptor agonist reverses the increased proportions of striatal dopamine D1High and D2High receptors in methamphetamine-sensitized rats. Eur J NeuroSci 27:2551–2557. doi:10.1111/j.1460-9568.2008.06221.x
Spangler R, Goddard NL, Avena NM, Hoebel BG, Leibowitz SL (2003) Elevated D3 dopamine receptor mRNA in dopaminergic and dopaminoceptive regions of the rat brain in response to morphine. Brain Res Mol Brain Res 111:74–83
Stoof JC, Kebabian JW (1981) Opposing roles for D-1 and D-2 dopamine receptors in efflux of cyclic AMP from rat neostriatum. Nature 294:366–368. doi:10.1038/294366a0
Theodore S, Cass WA, Maragos WF (2006a) Involvement of cytokines in human immunodeficiency virus-1 protein Tat and methamphetamine interactions in the striatum. Exp Neurol 199:490–498. doi:10.1016/j.expneurol.2006.01.009
Theodore S, Cass WA, Maragos WF (2006b) Methamphetamine and human immunodeficiency virus protein Tat synergize to destroy dopaminergic terminals in the rat striatum. Neuroscience 137:925–935. doi:10.1016/j.neuroscience.2005.10.056
Thompson PM, Dutton RA, Hayashi KM, Toga AW, Lopez OL, Aizenstein HJ, Becker JT (2005) Thinning of the cerebral cortex visualized in HIV/AIDS reflects CD4 + T lymphocyte decline. Proc Natl Acad Sci USA 102:15647–15652. doi:10.1073/pnas.0502548102
Ujike H, Onoue T, Akiyama K, Hamamura T, Otsuki S (1989) Effects of selective D-1 and D-2 dopamine antagonists on development of methamphetamine-induced behavioral sensitization. Psychopharmacology (Berl) 98:89–92. doi:10.1007/BF00442011
Wang GJ, Chang L, Volkow ND, Telang F, Logan J, Ernst T, Fowler JS (2004) Decreased brain dopaminergic transporters in HIV-associated dementia patients. Brain 127:2452–2458. doi:10.1093/brain/awh269
Acknowledgement
This study was supported, in part, by National Institutes of Health (NIH) grants K02-DA016149 and R21-DA019836 (SLC) and K24-DA016170 (LC).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, X., Chang, L., Vigorito, M. et al. Methamphetamine-Induced Behavioral Sensitization Is Enhanced in the HIV-1 Transgenic Rat. J Neuroimmune Pharmacol 4, 309–316 (2009). https://doi.org/10.1007/s11481-009-9160-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11481-009-9160-8