Abstract
Background
Effective antiretroviral therapy (ART) has reduced the incidence of HIV-associated neurocognitive impairment (HNCI) but its prevalence remains high. Clinical trials have yet to identify a consistently effective treatment for HNCI, other than ART, but in vitro data support that some drugs approved by the Food and Drug Administration (FDA) for other indications might benefit individuals with HNCI. Some of these drugs, such as serotonin reuptake inhibitors (SRIs) and HMG-CoA reductase inhibitors (statins), may do so by reducing HIV replication in the CNS and are already widely used by HIV-infected individuals.
Methods
Six-hundred fifty-eight HIV-infected participants of the CHARTER cohort had a baseline assessment, which included comprehensive neuropsychological (NP) testing and HIV RNA measurements in plasma and cerebrospinal fluid (CSF). Four-hundred sixty-seven (71%) subjects used ART, 195 (30%) used SRIs, and 63 (10%) used statins.
Results
SRI users were less likely to have HIV RNA levels in CSF above 50 copies (c)/mL (29 vs. 37% in non-SRI users, OR 0.69, p = 0.05). This association was most evident for three of the seven SRIs (citalopram, sertraline, and trazodone, or “antiviral” SRIs, combined 25 vs. 38% in non-SRI users, OR 0.56, p = 0.01) and was strongest in those not taking concomitant ART (61 vs. 83%, OR 0.31, p = 0.01). “Antiviral” SRI users also performed better on NP tests (median global deficit score 0.37 vs. 0.47, p = 0.04). Statin users were also less likely to have HIV RNA levels in CSF above 50 c/mL (16 vs. 37%, p < 0.001) but, in contrast to SRIs, the association was strongest in those taking ART (2 vs. 18%, p < 0.001). Statin use was not associated with better NP performance. Multivariate analyses indicated that the use of “antiviral” SRIs—but not statins—was associated with undetectable HIV RNA levels in CSF and better NP performance.
Conclusions
SRIs may reduce HIV replication in CSF and improve NP performance. This was particularly true for three SRIs—supporting differences in antiviral efficacy between drugs—in individuals who were not taking ART. In contrast, statins were not associated with lower HIV replication in CSF in multivariate analyses and were not associated with better NP performance. These analyses support the value of large observational cohort studies in identifying FDA-approved drugs that may be worth further investigation.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Background
Effective antiretroviral therapy (ART) has reduced the incidence of HIV-associated neurocognitive impairment (HNCI) but its prevalence remains high (Sacktor 2002; McArthur et al. 2003; Cysique et al. 2004; Tozzi et al. 2005). This high prevalence reflects the limited CNS effectiveness of ART and the lack of a consistently effective treatment for HNCI that augments ART (Heseltine et al. 1998; No Authors Listed 1998; Schifitto et al. 1999; Sacktor et al. 2000; Clifford et al. 2002). In vitro data support that some drugs approved by the Food and Drug Administration (FDA) for other indications may benefit individuals with HNCI.
Interest has recently focused on minocycline (Zink et al. 2005) and inhibitors of glycogen synthase kinase-3 beta, such as lithium (Gallicchio et al. 1993; Harvey et al. 2002; Dou et al. 2005; Letendre et al. 2006) and valproic acid (Ances et al. 2006; Schifitto et al. 2006). However, these drugs are not commonly prescribed to HIV-infected individuals, limiting preliminary assessment of their impact on outcomes in cohort studies. In contrast, two other classes of approved drugs, serotonin reuptake inhibitors (SRIs) and 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors (statins), are often prescribed to HIV patients. This is important because both classes of drugs may inhibit HIV replication in vitro but their effects have not been evaluated in humans.
Kristiansen and Hansen (2000), for example, demonstrated that the selective SRIs, paroxetine and femoxetine, reduced p24 levels in an in vitro HIV inhibition cell culture system although the mechanism of action was not identified. Several studies have supported the antiviral activity of statins (Giguere and Tremblay 2004; Mukhtar et al. 2005) although others have not (Moncunill et al. 2005; Negredo et al. 2006). If statins do inhibit HIV replication, they may do so via multiple mechanisms, including reduction of chemokine receptor-containing membrane lipid rafts (Popik et al. 2002; Goebel et al. 2005; Hillyard et al. 2006), adhesion molecule expression (Gilbert et al. 2005), and Rho guanosine triphosphatase activity (del Real et al. 2004). Because both classes of drugs may affect the CNS (Anderson 2004; Schmeer et al. 2006), we hypothesized that they would reduce HIV RNA levels in CSF and be associated with better neuropsychological (NP) performance compared with individuals who took neither class of drug. To test these hypotheses, we analyzed data from individuals enrolled in CHARTER (CNS AntiRetroviral Therapy Effects Research), an NIH-funded, North American cohort designed to assess the impact of HIV and ART on the central nervous system.
Methods
Study description
CHARTER is a multicenter, prospective, observational study designed to recruit a cohort that is similar to the U.S. population of HIV-infected individuals and to determine the effects of ARV therapy on the nervous system. The research was conducted at six North American locations: Johns Hopkins University, Baltimore, MD; Mt. Sinai, New York, NY; University of California, San Diego, CA; University of Texas, Galveston, TX; University of Washington, Seattle, WA; and Washington University, St. Louis, MO. The Institutional Review Boards at each site approved the study. The study procedures included comprehensive NP and neuromedical assessments, phlebotomy, lumbar puncture, and other assessments. Subjects (n = 658) were included in this analysis if they completed baseline evaluations, had successful lumbar punctures, and had HIV RNA levels measured in both plasma and CSF.
SRI and statin use
Subjects completed a series of questionnaires capturing detailed information about current and past use of SRIs and statins. To increase the reliability of the data collected, subjects were presented with a complete list of available SRIs and statins and asked to indicate whether they had ever used or were currently using each medication.
Neuromedical and laboratory assessments
All subjects underwent standardized neuromedical assessments. AIDS was diagnosed according to 1993 Centers for Disease Control guidelines. Blood was collected by venipuncture and CSF by lumbar puncture. HIV RNA levels were quantified in plasma and CSF by reverse transcriptase-polymerase chain reaction (Amplicor®, Roche Diagnostics, Pleasanton, CA, USA) using the ultrasensitive assay (nominal limit of quantitation 50 copies (c)/mL). HIV RNA values were truncated at the lower limit of quantitation for the purpose of analysis (“undetectable”). CD4+ cell counts were measured by flow cytometry.
Neuropsychological assessment
All subjects received a comprehensive NP evaluation, which was constructed to provide a relatively focused, but nonetheless robust, assessment of the cognitive domains known to be impaired in HIV. Specifically, the test battery was comprised of the following measures: (1) Hopkins Verbal Learning Test—Revised (Benedict et al. 1998), (2) Brief Visuospatial Memory Test—Revised (Benedict 1997), (3) Controlled Oral Word Association Test (Gladsjo et al. 1999) (COWAT-FAS), (4) semantic verbal fluency (Gladsjo et al. 1999), (5) Trail Making Test, Parts A and B (Heaton et al. 2004a, b), (6) Wisconsin Card Sorting Test—64 Card Version (WCST-64) (Kongs et al. 2000), (7) Paced Auditory Serial Addition Test (Diehr et al. 1998), (8) Grooved Pegboard Test (Heaton et al. 1991), (9) the Digit Symbol, Symbol Search, and Letter-Number Sequencing Tests from the Wechsler Adult Intelligence Scale—Third Edition (Heaton et al. 2002), and (10) Heaton Story and Figure Memory Tests (Heaton et al. 2004a, b). All NP tests were administered and scored by certified psychometrists in accordance with published procedures.
Raw scores were converted to demographically adjusted T-scores (m = 50, SD = 10) based on published normative data to account for the influence of age, education, sex, and ethnicity when possible (Carey et al. 2004). T-scores were then converted into deficit scores according to the following criteria: >40T = 0, 39T–35T = 1, 34T–30T = 2, 29T–25T = 3, 24T–20T = 4, and ≤19T = 5. The deficit scores from each of the NP test variables were then averaged to derive a Global Deficit Score (GDS; range = 0–5.00) for each participant, whereby higher scores reflect greater levels of impairment. Global impairment was determined by GDS of at least 0.5.
All participants also completed the Beck Depression Inventory=II (BDI) (Beck et al. 1996). The BDI is a 21-item self-report measure that rates severity of depressive symptoms during the past two weeks. Depressive symptoms assessed with the BDI include both somatic (e.g., weight loss, fatigue) and nonsomatic (e.g., suicidal ideation, feelings of guilt) items.
Statistical analysis
Plasma and CSF HIV RNA values were log10-transformed before analysis to improve their distribution. Univariate analyses were performed using Fisher’s exact tests for categorical variables (e.g., gender), t tests for normally distributed continuous variables (e.g., age), or Wilcoxon rank sum tests for skewed continuous variables (e.g., HIV RNA). Given the limited number of analyses, no adjustment for multiple comparisons was imposed. Logistic regression was used for multivariate analyses predicting HIV RNA detection in CSF. Linear regression was used for multivariate analyses predicting NP performance. All analyses were performed using JMP (version 6.0, SAS Institute Inc., Cary, NC, USA).
Results
Participant characteristics
Of 658 subjects, 467 (71%) reported ARV use, 195 (30%) reported SRI use, and 63 (10%) reported statin use at the time of their study visit. HIV RNA levels were detectable in plasma for 383 (58%) subjects and in CSF for 230 (35%) subjects. The median CD4 count was 402 cells/μL, and 64% of subjects had a diagnosis of AIDS.
Table 1 lists the seven SRIs reported by participants. SRI users endorsed more severe symptoms of depression on the BDI than nonusers (median BDI score [interquartile range (IQR)]: 16 [9–26] vs. 11 [5–20], p < 0.001). They were also more likely to be Caucasians (53 vs. 38%, p < 0.01) and female (26 vs. 18%, p = 0.03) but had similar levels of age and education. SRI users were more likely to be prescribed with ARVs (77 vs. 70%, p = 0.06), have higher CD4 counts (median [IQR] in cells per microliter: 433 [267–635] vs. 389 [229–565], p = 0.07), and have lower HIV RNA levels in plasma (median [IQR] in log10 copies per milliliter: 1.9 [1.7–3.5] vs. 2.4 [1.7–4.8], p = 0.07). SRI use was not associated with nadir CD4 count or AIDS diagnosis.
Table 1 also lists the five statins reported by participants. Compared to nonusers, statin users had higher CD4 counts (median [IQR] in cells per microliter: 499 [342–726] vs. 392 [237–576], p < 0.01) and lower HIV RNA levels in plasma (median [IQR] in log10 copies per milliliter: 1.7 [1.7–2.5] vs. 2.4 [1.7–4.1], p < 0.001). Statin users were also older (mean age in years [SD]: 49 (7) vs. 43 (8), p < 0.001), better educated (mean years of education [SD]: 14 (3) vs. 12 (2), p < 0.001), and more likely to be Caucasians (59 vs. 41%, p < 0.01) compared to nonstatin users. Additional demographic and clinical details are provided in Table 1.
SRI or statin use and HIV RNA in CSF
SRI users were less likely to have detectable HIV RNA in CSF compared to nonusers (29 vs. 37%, OR = 0.69, p = 0.05) although this relationship only trended toward significance when HIV RNA levels were expressed as a continuous variable (median [IQR] in log10 copies per milliliter: 1.7 [1.7–2.0] vs. 1.7 [1.7–2.5], p = 0.06). When individual drugs were analyzed for their relationship to HIV RNA levels in CSF, three drugs trended toward associations with lower HIV RNA levels in CSF [citalopram (n = 24, p = 0.10), trazodone (n = 64, p = 0.09), and sertraline (n = 37, p = 0.11)]. Combining users of these three drugs into an “antiviral” SRI category (n = 125) strengthened the association with HIV RNA in CSF (median [IQR] in log10 copies per milliliter: 1.7 [1.7–1.7] vs. 1.7 [1.7–2.5], p = 0.05; 25% detectable vs. 37% in non-SRI users, OR = 0.56, p = 0.02). Statin users also had lower HIV RNA levels in CSF (median [IQR] in log10 copies per milliliter: 1.7 [1.7–1.7] vs. 1.7 [1.7–2.5], p < 0.01) and had less than half the odds of having detectable HIV RNA levels in CSF as nonstatin users (16 vs. 37%, OR = .32, p < 0.001). Subjects who reported use of more than one SRI (n = 33) or more than one statin (n = 7) did not have significantly lower HIV RNA levels in CSF than those who reported use of only one drug in each class.
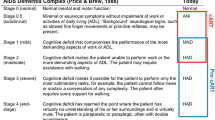
Four groups were defined by combining use of “antiviral” SRIs and statins (Neither, SRI Only, Statin Only, and SRI + Statin). HIV RNA levels in CSF differed among the four groups (mean in log10 copies per milliliter: 2.2 Neither vs. 2.1 SRI Only vs. 2.0 Statin Only vs. 1.8 SRI + Statin, ANOVA p = 0.03; proportion greater than 50 c/mL: see Fig. 1). Pairwise comparisons indicated that only the “SRI+ Statin” group had lower HIV RNA levels in CSF than the “Neither” group (OR = 0.21, p = 0.02).
To determine whether ART accounted for the observed relationships between SRI or statin use and HIV RNA levels in CSF, analyses were stratified by ART use (Fig. 2). Among subjects using ARVs, statin users were much less likely to have detectable HIV RNA in CSF than nonstatin users (2% detectable vs. 18%, OR = 0.09, p < 0.001). In contrast, “antiviral” SRIs were more strongly associated with lower HIV RNA levels in CSF among subjects not using ARVs. In this group, “antiviral” SRI users had less than half the odds of having detectable HIV RNA in CSF as non-SRI users (61% detectable vs. 83%, OR = 0.31, p = 0.01).
“Antiviral” SRI users (denoted “SRI” in this graph for simplicity) who did not use ART had less than half the odds of having detectable HIV RNA levels in CSF as non-SRI users (OR = 0.31), and statin users who used ART had less than a tenth the odds of having detectable HIV RNA levels in CSF as nonstatin users (OR = 0.09).
To determine whether other factors might account for the observed relationships, a series of logistic regressions was performed evaluating the variance in HIV RNA levels in CSF explained by AIDS diagnosis, ART use, CD4 count, HIV RNA levels in plasma, BDI, education, age, gender, and ethnicity. In the best-fit model, undetectable HIV RNA levels in CSF were associated with the use of “antiviral” SRIs (OR = 0.72, p < 0.05), ART use (p < 0.001), lower CD4 counts (p < 0.01), undetectable HIV RNA levels in plasma (p < 0.001), and Caucasian ethnicity (p = 0.02) but not the use of statins (p = 0.09) (model R 2 = 0.46, p < 0.001).
SRI or statin use and NP impairment
Users of “antiviral” SRIs performed better on NP testing, whether measured as better global deficit scores (median [IQR]: 0.37 [0.16–0.94] vs. 0.47 [0.26–1.00], p = 0.04) or a lower proportion of impairment (55 vs. 64%, p = 0.05). Statin use was not associated with NP performance or impairment status. In a linear regression model predicting global deficit scores and adjusting for AIDS diagnosis, ART use, CD4 count, plasma and CSF HIV RNA, education, age, gender, ethnicity, and BDI, only the use of “antiviral” SRIs was significantly associated with normal NP performance (p = 0.03).
Discussion
The current analysis supports further evaluation of three SRIs (citalopram, sertraline, and trazodone) and perhaps statins (predominantly atorvastatin and pravastatin in this cohort) for their antiviral and central nervous system effects. This is important because effective treatments for HIV-associated neurocognitive disorders remain an important unmet medical need based on the high prevalence in untreated and treated populations in both developed and resource-limited settings. Drug development efforts for HNCI have slowed for a number of reasons, including shifting patterns of disease and antiretroviral prescribing practices, challenges in assessment and diagnosis, and the limited success of prior trials. Observational cohort studies can support drug development by confirming—or refuting—the effectiveness of drugs that are used in a sufficiently large proportion of the cohort.
Our analysis demonstrated that individuals who took SRIs were more likely to have undetectable HIV RNA levels in CSF and better global NP performance. A plausible explanation for these effects is that SRI use resulted in better mood, resulting in better antiretroviral adherence or better effort on NP testing. Several facts argue against this hypothesis. First, better mood was not associated with undetectable HIV RNA levels in CSF or better NP performance (data not shown), arguing that this was not the mediator between these measures and SRI use. Second, SRI use was associated with lower HIV RNA levels in CSF predominantly among individuals who were not using ART, arguing strongly against the adherence theory. Third, only three SRIs were associated with undetectable HIV RNA levels in CSF and better NP performance, drug-specific effects that argue against attribution to the improvements in mood that all SRI drugs are designed to yield. Fourth, SRI use remained independently associated with undetectable HIV RNA levels in CSF even after adjusting for mood, antiretroviral use, and other disease-related measures. Together, these facts refute the hypothesis that better mood explained the findings but instead support a more direct link between SRI use, reduction in HIV RNA in CSF, and NP performance.
Statins were not expected to affect mood or ART adherence, so the observed associations with undetectable HIV RNA levels in CSF are less likely to be confounded. This association, however, only trended toward statistical significance after adjusting for antiretroviral use, SRI use, HIV RNA levels in plasma, and other measures. The effects of statins did not differ for individual drugs although these analyses were limited by the relatively low prevalence of statin use in the cohort. In contrast to SRIs, statins were associated with undetectable HIV RNA levels in CSF in ART-treated individuals, suggesting that their effects may be mediated by modifying antiretroviral metabolism or distribution. Several explanations are possible for the observed lack of NP benefit of statins. First, the association between statin use and undetectable HIV RNA levels in CSF could be an artifact due to type-I statistical error or confounding conditions, such as access-to-care. Subjects who used statins, for example, who used more prescription medications (as indexed by SRIs and statins), were more likely to be Caucasians and had more years of education and higher CD4 counts, all of which have been associated with better medical care in the U.S. (Currier and Fliesler 1995; Palacio et al. 2002; Cargill and Stone 2005). Balancing these factors, however, is the fact that statin users and nonusers were followed by the same providers in the same clinics and had similar rates of AIDS and ART use. Second, the benefits conferred by reduced HIV RNA levels might be mitigated by other conditions. In HIV-infected individuals, ART—particularly with certain protease inhibitors like ritonavir—can be complicated by several metabolic disorders, sometimes collectively termed lipodystrophy. When statins are used to treat protease inhibitor-induced lipodystrophy, the NP benefit could be negated by several factors, including the protease inhibitor, the statin, or the lipodystrophy disorder itself. Protease inhibitors, for example, are among the least CNS-penetrating antiretrovirals and, as such, individuals treated with them may have higher HIV RNA levels in CSF and may be at greater risk for HIV-associated neurocognitive disease compared to those taking non-PI combination regimens. Statins have been associated with evidence of brain injury such as memory loss although conflicting data exist (Wagstaff et al. 2003). If statins do injure the brain, this would paradoxically limit the antiviral benefit they confer in HIV-infected individuals. Hyperlipidemia and metabolic disorders have also been linked to higher risk for neurocognitive disease (Evans et al. 2004; Valcour et al. 2005). Because some metabolic disorders, such as lipoatrophy, are associated with mitochondrial injury, this might be a common mechanism linking them with brain injury. While these explanations are plausible, their analysis in this manuscript is limited by the sample size (63 individuals using five different statins). CHARTER aims to address these issues as part of an ongoing metabolic substudy.
The study has important limitations. First, its cross-sectional, observational design may not adequately account for potentially confounding factors, such as pretreatment differences between comparison groups. Second, although the overall sample size is large, only a subset of individuals used the drugs of interest. This was particularly true for statins, which were used in only 10% of the cohort. While this limited the power of the study to detect associations with study outcomes, the adjusted associations still trended toward statistical significance and therefore, if they are confirmed in independent analyses, the effect sizes could be substantial. Third, the current analyses do not include dosing or concentration data for SRIs or statins or adherence data for ART. Such data could modify the relationships with study outcomes. For example, an association between higher concentrations of citalopram and better outcomes would improve confidence in the study’s findings. Another notable issue is ART adherence, especially in light of the substantial proportion of non-SRI-using subjects who had symptoms of at least mild depression (median BDI 11). Non-SRI-using subjects who had untreated depression might also have reduced ART adherence, which could lead to ART failure, which, in turn, would tend to confound our analyses. Fourth, possible mechanisms of anti-HIV activity have been postulated for statins but, as yet, none has been identified for SRIs. Until a mechanism of action is identified, our findings must be considered with caution.
Despite these limitations, the findings support further evaluation of the antiviral and neurocognitive benefits of SRIs and possibly statins in HIV-infected individuals. They also reinforce that well-designed cohort studies can provide evidence suggesting additional effects of FDA-approved drugs. This evidence can then be used to focus further investigation. In an environment of rising drug development costs and constrained research budgets, such analyses may leverage pharmaceutical investment, reduce development time and risk, and extend drug indications, ultimately leading to more effective and less expensive treatments for HIV-infected individuals.
References
Ances B, Letendre S, Buzzell M, Marquie-Beck J, Lazaretto D, Marcotte TD, Grant I, Ellis RJ (2006) Valproic acid does not affect markers of HIV disease progression. J Neurovirol 12:403–406
Anderson GM (2004) Peripheral and central neurochemical effects of the selective serotonin reuptake inhibitors (SSRIs) in humans and nonhuman primates: assessing bioeffect and mechanisms of action. Int J Dev Neurosci 22:397–404
Beck AT, Steer RA, Brown GK (1996) Manual for the Beck Depression Inventory-II. Psychological Corporation, San Antonio, TX
Benedict RH (1997) Brief visuospatial memory test—revised. Psychological Assessment Resources, Inc., Odessa, Florida
Benedict RH, Schretlen D, Groninger L, Brandt J (1998) Hopkins verbal learning test—revised: normative data and analysis of inter-form and test–retest reliability. Clin Neuropsychol 12:43–55
Carey CL, Woods SP, Gonzalez R, Conover E, Marcotte TD, Grant I, Heaton RK (2004) Predictive validity of global deficit scores in detecting neuropsychological impairment in HIV infection. J Clin Exp Neuropsychol 26:307–319
Cargill VA, Stone VE (2005) HIV/AIDS: a minority health issue. Med Clin North Am 89:895–912
Clifford DB, McArthur JC, Schifitto G, Kieburtz K, McDermott MP, Letendre S, Cohen BA, Marder K, Ellis RJ, Marra CM (2002) A randomized clinical trial of CPI-1189 for HIV-associated cognitive-motor impairment. Neurology 59:1568–1573
Currier J, Fliesler N (1995) Demographics of HIV survival revisited. AIDS Clin Care 7:94
Cysique LA, Maruff P, Brew BJ (2004) Prevalence and pattern of neuropsychological impairment in human immunodeficiency virus-infected/acquired immunodeficiency syndrome (HIV/AIDS) patients across pre- and post-highly active antiretroviral therapy eras: a combined study of two cohorts. J Neurovirol 10:350–357
del Real G, Jimenez-Baranda S, Mira E, Lacalle RA, Lucas P, Gomez-Mouton C, Alegret M, Pena JM, Rodriguez-Zapata M, Alvarez-Mon M, Martinez AC, Manes S (2004) Statins inhibit HIV-1 infection by down-regulating Rho activity. J Exp Med 200:541–547
Diehr MC, Heaton RK, Miller W, Grant I (1998) The Paced Auditory Serial Addition Task (PASAT): norms for age, education, and ethnicity. Assessment 5:375–387
Dou H, Ellison B, Bradley J, Kasiyanov A, Poluektova LY, Xiong H, Maggirwar S, Dewhurst S, Gelbard HA, Gendelman HE (2005) Neuroprotective mechanisms of lithium in murine human immunodeficiency virus-1 encephalitis. J Neurosci 25:8375–8385
Evans RM, Hui S, Perkins A, Lahiri DK, Poirier J, Farlow MR (2004) Cholesterol and APOE genotype interact to influence Alzheimer disease progression. Neurology 62:1869–1871
Gallicchio VS, Cibull ML, Hughes NK, Tse KF (1993) Effect of lithium in murine immunodeficiency virus infected animals. Pathobiology 61:216–221
Giguere JF, Tremblay MJ (2004) Statin compounds reduce human immunodeficiency virus type 1 replication by preventing the interaction between virion-associated host intercellular adhesion molecule 1 and its natural cell surface ligand LFA-1. J Virol 78:12062–12065
Gilbert C, Bergeron M, Methot S, Giguere JF, Tremblay MJ (2005) Statins could be used to control replication of some viruses, including HIV-1. Viral Immunol 18:474–489
Gladsjo JA, Schuman CC, Evans JD, Peavy GM, Miller SW, Heaton RK (1999) Norms for letter and category fluency: demographic corrections for age, education, and ethnicity. Assessment 6:147–178
Goebel J, Logan B, Forrest K, Mieczkowski A, Roszman TL, Wills-Karp M (2005) Atorvastatin affects interleukin-2 signaling by altering the lipid raft enrichment of the interleukin-2 receptor beta chain. J Investig Med 53:322–328
Golden JC (1978) Stroop color and word test. Stoelting Co., Chicago, IL
Harvey BH, Meyer CL, Gallichio VS, Manji HK (2002) Lithium salts in AIDS and AIDS-related dementia. Psychopharmacol Bull 36:5–26
Heaton RK, Grant I, Matthews CG (1991) Comprehensive norms for an expanded Halstead–Reitan battery: demographic corrections, research findings, and clinical applications. Psychological Assessment Resources, Odessa, FL
Heaton RK, Taylor MJ, Manly JJ (2002) Demographic effects and use of demographically corrected norms with the WAIS-III and WMS-III. In: Tulsky D, Saklofske D, Heaton RK, Chelune G, Ivnik R, Bornstein RA, Prifitera A, Ledbetter M (eds) Clinical Interpretation of the WAIS-III and WMS-III. Academic Press, San Diego, CA
Heaton RK, Miller SW, Taylor MJ, Grant I (2004a) Revised comprehensive norms for an expanded Halstead–Reitan battery: demographically adjusted neuropsychological norms for African American and Caucasian adults. Psychological Assessment Resources, Lutz, FL
Heaton RK, Marcotte TD, Mindt MR, Sadek J, Moore DJ, Bentley H, McCutchan JA, Reicks C, Grant I (2004b) The impact of HIV-associated neuropsychological impairment on everyday functioning. J Int Neuropsychol Soc 10:317–331
Heseltine PN, Goodkin K, Atkinson JH, Vitiello B, Rochon J, Heaton RK, Eaton EM, Wilkie FL, Sobel E, Brown SJ, Feaster D, Schneider L, Goldschmidts WL, Stover ES (1998) Randomized double-blind placebo-controlled trial of peptide T for HIV-associated cognitive impairment. Arch Neurol 55:41–51
Hillyard DZ, Nutt CD, Thomson J, McDonald KJ, Wan RK, Cameron AJ, Mark PB, Jardine AG (2006) Statins inhibit NK cell cytotoxicity by membrane raft depletion rather than inhibition of isoprenylation. Atherosclerosis Jun 27; (Epub ahead of print)
Kongs SK, Thompson LL, Iverson GL, Heaton RK (2000) Wisconsin card sorting test-64 card computerized version. Psychological Assessment Resources, Odessa, FL
Kristiansen JE, Hansen JB (2000) Inhibition of HIV replication by neuroleptic agents and their potential use in HIV infected patients with AIDS related dementia. Int J Antimicrob Agents 14:209–213
Letendre SL, Woods SP, Ellis RJ, Atkinson JH, Masliah E, van den Brande G, Durelle J, Grant I, Everall I (2006) Lithium improves HIV-associated neurocognitive impairment. Aids 20:1885–1888
McArthur JC, Haughey N, Gartner S, Conant K, Pardo C, Nath A, Sacktor N (2003) Human immunodeficiency virus-associated dementia: an evolving disease. J Neurovirol 9:205–221
Moncunill G, Negredo E, Bosch L, Vilarrasa J, Witvrouw M, Llano A, Clotet B, Este JA (2005) Evaluation of the anti-HIV activity of statins. Aids 19:1697–1700
Mukhtar M, Mengistu A, Acheampong E, Sullivan J, Nunnari G, Argyris E, Kalayeh M, Williams K, Pomerantz R (2005) Statins block enhanced transvascular migration of HIV-1-infected cells: a novel therapeutic approach for HIV-1 neuroinvasion (Abstract 391). In: 12th Conference on Retroviruses and Opportunistic Infections, Boston, MA
Negredo E, Clotet B, Puig J, Perez-Alvarez N, Ruiz L, Romeu J, Molto J, Rey-Joly C, Blanco J (2006) The effect of atorvastatin treatment on HIV-1-infected patients interrupting antiretroviral therapy. Aids 20:619–621
No Authors Listed (1998) A randomized, double-blind, placebo-controlled trial of deprenyl and thioctic acid in human immunodeficiency virus-associated cognitive impairment. Dana consortium on the therapy of HIV dementia and related cognitive disorders. Neurology 50:645–651
Palacio H, Kahn JG, Richards TA, Morin SF (2002) Effect of race and/or ethnicity in use of antiretrovirals and prophylaxis for opportunistic infection: a review of the literature. Public Health Rep 117:233–251; discussion 231–232
Popik W, Alce TM, Au WC (2002) Human immunodeficiency virus type 1 uses lipid raft-colocalized CD4 and chemokine receptors for productive entry into CD4(+) T cells. J Virol 76:4709–4722
Sacktor N (2002) The epidemiology of human immunodeficiency virus-associated neurological disease in the era of highly active antiretroviral therapy. J Neurovirol 8(Suppl 2):115–121
Sacktor N, Schifitto G, McDermott MP, Marder K, McArthur JC, Kieburtz K (2000) Transdermal selegiline in HIV-associated cognitive impairment: pilot, placebo-controlled study. Neurology 54:233–235
Schifitto G, Sacktor N, Marder K, McDermott MP, McArthur JC, Kieburtz K, Small S, Epstein LG (1999) Randomized trial of the platelet-activating factor antagonist lexipafant in HIV-associated cognitive impairment. Neurological AIDS Research Consortium. Neurology 53:391–396
Schifitto G, Peterson DR, Zhong J, Ni H, Cruttenden K, Gaugh M, Gendelman HE, Boska M, Gelbard H (2006) Valproic acid adjunctive therapy for HIV-associated cognitive impairment: a first report. Neurology 66:919–921
Schmeer C, Kretz A, Isenmann S (2006) Statin-mediated protective effects in the central nervous system: general mechanisms and putative role of stress proteins. Restor Neurol Neurosci 24:79–95
Tozzi V, Balestra P, Lorenzini P, Bellagamba R, Galgani S, Corpolongo A, Vlassi C, Larussa D, Zaccarelli M, Noto P, Visco-Comandini U, Giulianelli M, Ippolito G, Antinori A, Narciso P (2005) Prevalence and risk factors for human immunodeficiency virus-associated neurocognitive impairment, 1996 to 2002: results from an urban observational cohort. J Neurovirol 11:265–273
Valcour VG, Shikuma CM, Shiramizu BT, Williams AE, Watters MR, Poff PW, Grove JS, Selnes OA, Sacktor NC (2005) Diabetes, insulin resistance, and dementia among HIV-1-infected patients. J Acquir Immune Defic Syndr 38:31–36
Wagstaff LR, Mitton MW, Arvik BM, Doraiswamy PM (2003) Statin-associated memory loss: analysis of 60 case reports and review of the literature. Pharmacotherapy 23:871–880
Zink MC, Uhrlaub J, DeWitt J, Voelker T, Bullock B, Mankowski J, Tarwater P, Clements J, Barber S (2005) Neuroprotective and anti-human immunodeficiency virus activity of minocycline. JAMA 293:2003–2011
Acknowledgments
The CNS HIV Anti-Retroviral Therapy Effects Research (CHARTER) is supported by award N01 MH22005 from the National Institutes of Health.
The CHARTER Group is affiliated with the Johns Hopkins University; Mount Sinai School of Medicine; University of California, San Diego; University of Texas, Galveston; University of Washington, Seattle; and Washington University, St. Louis, and is headquartered at the University of California, San Diego, and includes: Director: Igor Grant, M.D.; Codirectors: J. Allen McCutchan, M.D., Ronald J. Ellis, M.D., Ph.D., Thomas D. Marcotte, Ph.D.; Center Manager: Shondra Neumayer, R.N., F.N.P.; Neuromedical Component: Ronald J. Ellis, M.D., Ph.D. (P.I.), J. Allen McCutchan, M.D., Terry Alexander, R.N.; Laboratory, Pharmacology and Immunology Component: Scott Letendre, M.D. (P.I.), Edmund Capparelli, Pharm.D., Janis Durelle; Neurobehavioral Component: Robert K. Heaton, Ph.D. (P.I.), J. Hampton Atkinson, M.D., Steven Paul Woods, Psy.D., Donald Franklin; Virology Component: Joseph K. Wong, M.D. (P.I.), Caroline Ignacio; Imaging Component: Terry Jernigan, Ph.D. (P.I.), Michael J. Taylor, Ph.D., Rebecca Theilmann, Ph.D.; Data Management Unit: Anthony C. Gamst, Ph.D. (P.I.), Clint Cushman, Michelle Frybarger; Statistics Unit: Ian Abramson, Ph.D. (P.I.), Deborah Lazzaretto, M.S.; Protocol Coordinating Component: Thomas D. Marcotte, Ph.D. (P.I.), Rodney von Jaeger, M.P.H.; Johns Hopkins University Site: Justin McArthur (P.I.); Mount Sinai School of Medicine Site: Susan Morgello, M.D. (Co-P.I.), David Simpson, M.D. (Co-P.I.); University of California, San Diego Site: J. Allen McCutchan, M.D. (P.I.); University of Washington, Seattle Site: Ann Collier, M.D. (Co-P.I.), Christina Marra, M.D. (Co-P.I.); University of Texas, Galveston Site: Benjamin Gelman, M.D., Ph.D. (P.I.); and Washington University, St. Louis Site: David Clifford, M.D. (P.I.), Muhammad Al-Lozi, M.D.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the United States Government.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Letendre, S.L., Marquie-Beck, J., Ellis, R.J. et al. The Role of Cohort Studies in Drug Development: Clinical Evidence of Antiviral Activity of Serotonin Reuptake Inhibitors and HMG-CoA Reductase Inhibitors in the Central Nervous System. Jrnl Neuroimmune Pharm 2, 120–127 (2007). https://doi.org/10.1007/s11481-006-9054-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11481-006-9054-y