Abstract
The present study sought to examine optimism and hope as predictors of suicidal behaviors (viz., suicide ideation and suicide attempt) in a sample of 179 adult primary care patients. Furthermore, we aimed to determine if the combination of hope and optimism would account for additional variance in the prediction model for suicidal behaviors among this population. In this cross-sectional study, participants completed measures of hope (viz., agency and pathways), optimism, and suicidal behaviors, as well as a series of demographics questions. Hierarchical regression analyses were conducted to test the aforementioned hypotheses. Results indicated that hope and optimism were both significant and unique predictors of suicidal behaviors among adult primary care patients. However, the hope-by-optimism interaction terms were not found to be significant. Some implications of the present findings are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Suicide represents a serious health concern in the USA, where rates are as high as 13.7/100,000 people, surpassing suicide rates of several other developed nations (e.g., UK of Great Britain; Canada; World Health Organization (WHO) 2016). In fact, suicidal behaviors (e.g., suicide ideation and suicide attempt) are of particular concern, given that in 2013 alone, an estimated 9.3 million American adults exhibited suicide ideation and 1.3 million adults attempted suicide (Substance Abuse and Mental Health Services Administration (SAMHSA) 2014). Due to these alarming rates of suicidal behaviors, it is not surprising that researchers have become increasingly interested in understanding the factors that influence suicidal behaviors among adult populations.
One population particularly vulnerable to suicide in which suicidal behaviors may be important to examine is adult primary care patients (Windfuhr et al. 2016). Although prevalence rates of suicide ideation have been found to be as high as 10.5% among primary care patients (Schulberg et al. 2004), much of the extant research has focused on other populations with comparatively lower rates of suicidal behaviors (e.g., 8.0% suicide ideation among college students; SAMHSA 2014). That said, over half of the 928.6 million annual visits to a physician’s office in the United States are made to primary care physicians (Hing et al. 2013). Additionally, approximately 45% of individuals who died by suicide visited their primary care physician within the month prior (Luoma et al. 2002), which emphasizes the crucial role primary healthcare professionals play in suicide risk assessment and treatment. Research findings have indicated that signs of suicide risk may frequently be overlooked in primary healthcare settings (Beautrais et al. 1998; Pirkis and Burgess 1998). Reasons for this may include the lack of suicide risk assessment by primary care physicians (Hepner et al. 2007) and the difficulty associated with accurately assessing suicide risk, as some patients may conceal suicide ideation or have suicidal thoughts without intention to die (Freedenthal 2008). Accordingly, it becomes important to further understand the specific factors that may be predictive of suicidal behaviors among adult primary care patients.
When considering suicide risk, it may be particularly valuable to examine the role of protective factors as past studies have indicated that positive psychological constructs may serve as protective factors against suicidal behaviors (e.g., Chang et al. 2017; Davidson and Wingate 2013; Luo et al. 2016). For instance, previous findings have indicated hope, defined as the ability to motivate oneself to achieve a self-determined goal (Snyder et al. 1991), to be a significant predictor of lower suicide ideation among adults (Chang et al. 2017; Davidson et al. 2010; O’Keefe and Wingate 2013; Tucker et al. 2013). Hope is composed of two subcomponents, namely, hope agency (i.e., goal-directed energy) and hope pathways (i.e., the planning in order to accomplish goals, Snyder et al. 1991). Snyder’s (2002) hope theory suggests that individuals with greater hope report more positive outcomes in a variety of areas, including psychological adjustment, as greater hope tends to elicit a greater number of positive emotions (Snyder et al. 1999; Snyder et al. 1991). Despite the emphasis that has been placed on expanding the research on protective factors of suicide risk (WHO 2014), few studies have examined the role of hope pathways and hope agency in predicting suicide risk among adult primary care patients. Notably, past studies have examined the relationship between hope and other maladjustment outcomes among primary care patients. For instance, a study by Chang et al. (2013a, b, c) found hope to be a significant predictor of depressive symptoms among adult primary care patients. However, little is currently known about hope in relation to suicidal behaviors within this population. Thus, given previous findings that have demonstrated the potential protective role hope may have on suicidal behaviors and the lack of research on hope and suicidal behaviors in primary care patients, it may be important to examine the relationship between hope and suicidal behaviors among this population.
Beyond hope, another positive psychological construct that has been consistently found to be associated with suicidal behaviors is optimism (e.g., Huffman et al. 2016), defined as the expectation that good things are to come in the future (Scheier and Carver 1985). Individuals with greater optimism have been shown to have a better capacity for positive psychological adjustment (e.g., emotional well-being, adaptive coping) than those with less optimism (Carver et al. 2010). Accordingly, it is not surprising that previous findings have indicated that optimism is a significant predictor of lower suicide ideation (Chang et al. 2017; Hirsch et al. 2007a, b; O’Keefe and Wingate 2013; Rasmussen and Wingate 2011; Tucker et al. 2013). Furthermore, optimism has been found to be a significant predictor of suicidal behaviors (Chang et al. 2013a, b, c) and other maladjustment outcomes (e.g., depressive symptoms; Chang et al. 2013a, b, c) among adult primary care patient populations. In other words, greater optimism among this population has been associated with a lesser risk for suicide. Indeed, as few researchers have examined the relationship between greater optimism and possible protection from suicidal behaviors among primary care patients, it may be valuable to expand upon the study by Chang et al. (2013a, b, c) that examined the relationship between optimism and depressive symptoms among this population. Thus, given the limited literature and the findings from previous studies, it may be valuable to examine the relationship between optimism and suicidal behaviors among primary care patients.
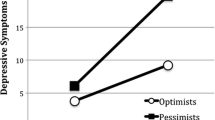
Importantly, it is worth noting that hope and optimism each represent unique constructs (Alarcon et al. 2013; Gallagher and Lopez 2009). For example, findings from a study by Bryant and Cvengros (2004) suggest that hope focuses more on attainment of specific personal goals, whereas optimism is broader and encompasses beliefs about general future outcomes. Given these conceptual differences, it would be important to examine the confluence of hope and optimism, as the combination of hope and optimism together may be more so predictive of suicidal behaviors among adult primary care patients than either construct alone. Specifically, given that hope focuses on personal agency and pathways necessary to achieve a certain future goal (Snyder 2002; Snyder et al. 1991) and optimism focuses on general future expectancies (Carver and Scheier 2002), the combination of hope and optimism may have a broader influence on psychological health than either construct alone (Alarcon et al. 2013). Thus, hope and optimism together may potentially provide additional protection from maladjustment outcomes (e.g., suicidal behaviors) among primary care patients. Indeed, results from previous studies (e.g., Chang et al. 2013a, b, c) have demonstrated a significant interaction of positive psychological constructs in relation to maladjustment. For example, Chang et al. (2013a, b, c) found evidence for a significant hope-by-optimism interaction that was additionally predictive of depressive symptoms in primary care patients. However, as no study to date has examined the utility of such an interaction in predicting suicidal behaviors among adult primary care patients, it may be of interest to examine for hope-by-optimism interaction effects to assess if the co-presence of hope and optimism offers any additional predictive value and possible protection against suicidal behaviors among primary care patients.
Purpose
Given these considerations, the present study was conducted to: (a) determine if optimism and hope (viz., hope agency, hope pathways) are unique predictors of suicidal behaviors in primary care patients and (b) determine if the hope-by-optimism interaction terms (viz., hope agency by optimism, hope pathways by optimism) would add further incremental validity to these predictions beyond the main effects of optimism, hope agency, and hope pathways.
For the purposes of the present study, suicidal behaviors were comprehensively characterized as participants’ lifetime suicide ideation and/or attempt, frequency of suicide ideation in the past 12 months, threat of suicide, and future likelihood of suicidal behaviors (Osman et al. 2001). Based on previous findings that provide support for hope and optimism as significant individual predictors of suicidal behaviors among adult populations (Chang et al. 2017; Davidson et al. 2010; Hirsch et al. 2007a; b; O’Keefe and Wingate 2013; Rasmussen and Wingate 2011; Tucker et al. 2013), we expected both hope and optimism to emerge as significant unique predictors of suicidal behaviors among adult primary care patients. Furthermore, given the contention that hope and optimism each have distinct beneficial effects on psychological well-being (Alarcon et al. 2013; Gallagher and Lopez 2009; Peterson 2000; Scheier and Carver 1985; Snyder et al. 1991), we examined for hope-by-optimism interactions in predicting suicidal behaviors. Consistent with the concept of “doubling up” on positive psychological constructs (Chang et al. 2013a, b, c), wherein the co-presence of both hope and optimism would provide additional possible protection from suicidal behaviors beyond either hope or optimism alone for primary care patients, we anticipated that primary care patients with greater hope coupled with greater optimism would report the least amount of suicidal behaviors.
Method
Participants
A total of 179 adults (112 females, 66 males, and 1 “other” gender identity) were recruited from a community-based primary care clinic located in the Southeast USA. Ages ranged from 19 to 79 (M = 45.16, SD = 12.11). Of all the participants, 85.5% (n = 153) identified as Caucasian, 7.8% (n = 14) identified as Black, 3.4% (n = 6) as Hispanic/Latino, 1.1% (n = 2) as American Indian/Alaskan Native, 0.6% (n = 1) as Asian, and 1.7% (n = 3) as “Other” race/ethnicity. At the time of data collection, 54.7% (n = 98) were unemployed, 17.3% (n = 31) were on disability, 13.4% (n = 24) of participants were employed full-time, 11.2% (n = 20) were employed on a part-time basis, and 2.8% (n = 5) were retired. Regarding participants’ level of education, 30.1% (n = 54) of the present sample had not completed a high school education, 29.1% (n = 52) had earned their high school diploma or GED, 22.9% (n = 41) had completed some college but did not graduate, and 17.9% (n = 32) earned an Associate’s degree of higher. Participants identified as 34.6% (n = 62) divorced, 29.1% (n = 52) single and never married, 22.3% (n = 40) married and living with their spouse, 8.9% (n = 16) married and not living with their spouse, and 5.0% (n = 9) widowed.
Measures
Optimism
Optimism was assessed by using the Revised Life Orientation Test (LOT-R; Scheier et al. 1994), a 10-item measure designed to assess both positive and negative outcome expectancies. Three of the items on the LOT-R are positively worded (e.g., “In uncertain times, I usually expect the best”), another three items (reverse scored) are negatively worded (e.g., “If something can go wrong for me, it will”), and four statements are filler items. Respondents rate each item on a 5-point Likert-type scale ranging from 0 (strongly disagree) to 4 (strongly agree). Higher scores on the LOT-R indicate higher levels of optimism, whereas lower scores indicate greater pessimism. In the present sample, the internal consistency of the LOT-R as measured by Cronbach’s alpha was .81.
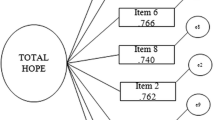
Hope
Hope was assessed by using the Hope Scale (HS; Snyder et al. 1991), a 12-item measure designed to assess for hope. The HS consists of two subscales: agency (i.e., goal-directed energy) and pathways (i.e., planning to accomplish goals). There are four items each for agency (e.g., “I energetically pursue my goals”) and pathways (e.g., “There are lots of ways around any problem”). The remaining four items on the scale are fillers. For each item, respondents rate how accurately each item describes them on an 8-point Likert-type scale, ranging from 1 (definitely false) to 8 (definitely true). Higher scores on the HS indicate greater hope. In the present sample, the internal consistency of the HS as measured by Cronbach’s alpha was .88.
Suicidal Behaviors
Suicidal behavior was assessed by using the Suicidal Behaviors Questionnaire-Revised (SBQ-R; Osman et al. 2001). The SBQ-R is a four-item measure designed to assess for (1) lifetime suicide ideation and attempts (“Have you ever thought about or attempted to kill yourself?”), (2) frequency of suicide ideation over the past 12 months (“How often have you thought about killing yourself in the past year?”), (3) threat of suicide (“Have you ever told someone that you were going to commit suicide or that you might do it?”), and (4) likelihood of engaging in suicidal behavior in the future (“How likely is it that you will attempt suicide someday?”). Respondents rate each item on a 5- to 7-point Likert-type scale to the extent that each item applies to them. Higher scores on the SBQ-R indicate greater suicidal behaviors (i.e., participant scores represent greater lifetime suicide ideation and/or attempt, greater frequency of suicide ideation in the previous 12 months, greater threat of suicide attempt, and/or greater likelihood of future suicidal behaviors). In the present sample, the internal consistency of the SBQ-R as measured by Cronbach’s alpha was .84.
Procedure
Approval for the study was obtained from the Institutional Review Board prior to data collection. Participants were recruited at a primary care clinic using advertisements displayed throughout the clinic, and subsequently completed a paper/pencil survey upon providing written, informed consent that indicated all data would be kept strictly confidential. After completing the survey, participants were compensated $15 for their participation. All participants were also provided with a comprehensive list of various community and national suicide prevention resources (e.g., National Suicide Prevention Lifeline).
Results
For all analyses, we controlled for demographics variables (viz., age, sex, race/ethnicity, education level, employment status, and marital status). We chose to control for demographic variables as primary care patients represent a diverse group of individuals who come from a variety of different backgrounds (e.g., different levels of education achievement, varying marital statuses). Moreover, based on previous research findings, we believed these differences could represent potential confounds and thus we chose to control for them (e.g., Abel and Kruger 2005; Ahmedani et al. 2015; Denney et al. 2009; Kõlves et al. 2010; Schneider et al. 2011).
Correlations, means, and standard deviations for all of the study measures are presented in Table 1. All correlations were significant and in the expected directions. For example, hope and optimism were positively correlated with each other, and both were also negatively correlated with suicidal behaviors. To examine for optimism and hope as predictors of suicidal behaviors in adult primary care patients, we conducted a set of hierarchical regression analyses with the demographic variables (viz., age, sex, race/ethnicity, employment status, education level, and marital status) as a control in Step 1. Hope and optimism were entered in Step 2. Finally, the hope agency by optimism and the hope pathways by optimism interaction terms were entered in Step 3. Notably, examinations of standardized residuals of the SBQ-R demonstrated violations of normality. Thus, we performed a log transformation on the SBQ-R scores in order to address the violated assumption of multiple regression, and subsequently used those scores for the regression analyses. To determine whether any of the predictors accounted for a small, medium, or large amount of variance in suicidal behaviors, we used Cohen’s (1977) convention for small (f2 = .02), medium (f2 = .14), and large effects (f2 = .35) as a general guide.
Results for predicting suicidal behaviors are presented in Table 2. In Step 1, demographic variables as a set did not account for a significant amount of variance in suicidal behaviors, F(6, 172) = 1.52, p > .05. When the hope subscales (viz., agency, pathways) and optimism were entered as a set in Step 2, it was found to account for a large (f2 = .47) 31.5% of additional variance in suicidal behaviors, F(3, 169) = 27.93.69, p < .001. Within the predictor set, hope agency (β = −.31, p ≤ .001) and optimism (β = −.25, p < .01) were each found to be significant predictors of suicidal behaviors. Notably, hope pathways (β = −.12, p > .05) was not found to be a significant predictor of suicidal behaviors. Finally, in Step 3, when the hope-by-optimism interaction terms were entered as a set, it was not found to be a significant predictor of suicidal behaviors, F(2, 167) = 0.061, p > .05. The total prediction model was found to account for a large (f2 = .58) 36.6% of the variance in suicidal behaviors, F(11, 167) = 8.75, p < .001.
Noteworthy, the present sample of adult primary care patients demonstrated a moderate level of suicide risk (M = 6.64, SD = 3.85). The average total score on the SBQ-R among the present sample is just slightly lower than the cutoff SBQ-R score for high risk of suicide among non-clinical adult populations (i.e., a total score of less than or equal to seven; Osman et al. 2001). Moreover, in accordance with scoring guidelines for the SBQ-R, 34.6% of the participants could be categorized as being at a risk for suicide based on their response to the first item (i.e., selecting a 3 or 4 on the Likert-type scale for this item designed to assess lifetime suicide ideation and/or attempts). Results also suggest that the majority of participants (55.9%) had not experienced suicide ideation within the previous 12 months, while a small subset (5.6%) had experienced suicide ideation five times or more in the same time period. Of the present sample, 33.5% indicated that they had at some point told someone they were going to commit suicide or that they might do it. Lastly, the majority of the sample (64.8%) indicated that they did not believe it was at all likely they would attempt suicide in the future (i.e., chose a response option of 0 or 1). However, 9.6% responded that future suicide attempts were likely (i.e., response option 4, 5, or 6).
Discussion
Given previous research that has examined the influence of positive psychological constructs on suicidal behaviors in adult populations, the purpose of the present study was to examine the unique value of hope and optimism as predictors of suicidal behaviors in a sample of adult primary care patients. The results of our study indicated at least two important findings regarding hope and optimism in relation to suicidal behaviors. First, consistent with previous research studies that have emphasized the positive influence of optimism and hope on suicidal behaviors among adult populations (e.g., Chang et al. 2017; Davidson et al. 2010; Hirsch et al. 2007a, b; O’Keefe and Wingate 2013; Rasmussen and Wingate 2011; Tucker et al. 2013), both optimism and hope were found to be unique and significant predictors of suicidal behaviors in our sample of primary care patients after controlling for demographic variables (viz., age, sex, race, employment status, education level, and marital status). Interestingly, hope agency, but not hope pathways, emerged as a significant predictor of suicidal behaviors within this population. This finding is related to previous works, which have suggested that hope agency, and not hope pathways, is significantly related to negative affective conditions (Chang 2003; Chang et al. 2017) and suicidal risk (Muyan and Chang 2016). For adult primary care patients, having goal-directed energy (i.e., hope agency) may be more important than planning related to goals (i.e., hope pathways) in the protection against suicidal behaviors, although more research is needed to further investigate this relationship. Thus, our findings add to the current literature regarding the relationship between positive psychological constructs and suicidal behaviors among adult populations by suggesting the value of hope, specifically hope agency, and optimism as potential protective factors of suicide within an adult primary care population. Indeed, these findings emphasize the possible value of assessing for known and potential protective factors of suicide among primary care patients, in addition to risk factors of suicide.
Second, given the notion that hope and optimism have individual benefits on psychological health (Alarcon et al. 2013), as well as previous support for a significant interaction effect between suicidal behaviors and hope and optimism among other populations (i.e., Hungarian college students; Chang et al. 2017), the present study also sought to examine if such an interaction would be predictive of suicidal behaviors among adult primary care patients. Interestingly, neither of the hope-by-optimism interaction terms were found to be significant in predicting suicidal behaviors among primary care patients, suggesting that it may not be necessary for hope and optimism to be simultaneously present for primary care patients to experience protection from suicidal behaviors. Several of the previous studies that have demonstrated a significant hope-by-optimism interaction effect have been among young adult populations (e.g., Chang et al. 2017; Chang et al. 2013a, b, c). As such, it may be that the non-significant interactions in the present study indicate an important developmental influence of a “doubling up” effect. Unlike college students in a convenience sample, it may be that primary care patients who are middle-aged are better able to manage the difficulties of life that may contribute to suicide risk, and thus make the combination of these two constructs less influential. Nonetheless, given the unique and significant predictive value of both hope and optimism, it remains important to facilitate both variables among primary care patients.
The findings of the present study have at least two important implications for the current understanding of suicidal behaviors among adult primary care patients. First, given that primary healthcare professionals play a crucial role in the identification and treatment of factors contributing to suicide risk (US Department of Health and Human Services 2012), our findings suggest that it may be important for primary healthcare professionals to assess for the presence or absence of proposed protective factors, namely hope and optimism, when examining for patients’ risk of suicide. Consistent with past research indicating that hope and optimism represent unique constructs that differentially influence psychological health (Alarcon et al. 2013; Bryant and Cvengros 2004), both variables emerged as unique predictors of suicidal behaviors among primary care patients. This suggests that the inclusion of both hope and optimism within suicide risk assessments may provide a more holistic understanding of the factors that serve to protect a primary care patient from suicidal behaviors. However, while past suicide risk assessments that have been developed for primary care settings have focused on a variety of social protective factors (e.g., family support; Voros et al. 2006), few have focused on positive psychological constructs, including hope and optimism. Thus, including hope and optimism alongside more standard measures during suicide risk assessments will not only inform providers of their patients’ belief that they are capable of achieving a self-determined goal (i.e., hope) and their outlook of the future (i.e., optimism) but also underscore the potential value of considering hope and optimism in treatments for patients presenting with suicidal behaviors.
Second, our findings underscore the importance of cultivating and fostering hope and optimism among primary care patients, so as to serve as a possible form of protection from suicidal behaviors. Indeed, given that primary care providers only have a limited amount of time to dedicate to each individual patient, there may be particular utility for brief interventions that foster hope and optimism among patients presenting with suicidal behaviors. Previous literature has emphasized the roles optimism and hope each play in the treatment process of suicidal behaviors (e.g., Hirsch et al. 2007a, b; Rudd and Brown 2011). For instance, hope-generating interventions that focus on goal orientation and solution development have previously been presented as an intervention method in instances of suicide risk (e.g., Sharry et al. 2002; Softas-Nall and Francis 1998). Indeed, a study by Rhee et al. (2005) found that suicidal callers to a suicide crisis hotline demonstrated significant improvements on all of the study’s measures (e.g., decreased depressive symptoms; increased life satisfaction) in response to a brief, hope-generating intervention. Moreover, one brief, hope-based intervention that is rooted in hope theory (e.g., Snyder 1994), has been found to result in increased hope agency, life meaning, self-esteem, and associated with decreases in negative affective symptoms (e.g., depressive and anxious symptoms; Cheavens et al. 2006). As this treatment was not designed to address any specific psychopathology (Cheavens et al. 2006), it may be particularly useful for primary care patients that are not experiencing suicidal behaviors at the time of assessment.
Relatedly, fostering optimism has also been indicated as a potential means of reducing the negative implications of suicidal behaviors within the treatment process (Wingate et al. 2006). Indeed, a study by Huffman et al. (2014) demonstrated the feasibility and usefulness of certain positive psychological interventions (viz., best possible self [BPS] exercise) in improving optimism among suicidal inpatients. Given that the BPS exercise can be successfully completed within a matter of minutes, as well as its effectiveness at increasing optimism, this may be an intervention that could be utilized by providers within a primary care setting and also taught to patients for continued usage and enhanced efficacy of the exercise (Loveday et al. 2018). Additionally, while more extensive interventions may not be feasible in a primary healthcare setting, a recent study by Celano et al. (2017) found that a 6-week cognition-focused therapy significantly improved optimism among individuals recently hospitalized for suicidal behaviors. Indeed, this could be a form of intervention that primary healthcare providers can refer patients to in a community or hospital setting.
Given that the findings of our study indicate hope and optimism to be significant and unique predictors of suicidal behaviors among adult primary care patients, the aforementioned interventions are promising for a primary healthcare setting in terms of feasibility and usefulness. Indeed, brief interventions that promote and foster hope and optimism (viz., hope-generating interventions and BPS) may allow providers to promptly and effectively thwart patients’ suicidal behaviors, as well as make the appropriate subsequent treatment decisions or referrals. In instances of referral, providers may be able to refer their patients to other available resources within a primary healthcare or hospital setting (e.g., cognition-focused interventions).
Limitations
Although the present study provides important empirical support for optimism and hope as unique predictors of suicidal behaviors among adult primary care patients, some limitations should be noted. First, given that this study utilized a community sample of adult primary care patients who were at low to moderate risk for suicide, it may be of interest for future studies to examine optimism and hope in relation to suicidal behaviors among those who are at higher risk for suicide. Second, we focused the present study on factors that may predict suicidal behaviors among primary care patients. It may be important to also determine if other positive psychological constructs are predictive of suicidal behaviors among this population (e.g., self-compassion; Shapira and Mongrain 2009). Third, as the majority of the present sample identified as Caucasian (85.5%), it would be important for future research to examine whether the present findings hold true among other ethnoracial groups (e.g., African American primary care patients). Finally, given the cross-sectional nature of the present study, it is not possible to determine cause and effect. Indeed, it would be beneficial for future research to examine optimism and hope across time, so as to determine if these two constructs predict changes in suicidal behaviors across time among this population.
Concluding Thoughts
The present study was conducted among a sample of adult primary care patients to examine the predictive value of optimism and hope on suicidal behaviors, and to test for hope-by-optimism interaction effects in which the co-presence of these two variables would further predict suicidal behaviors. Overall, our findings demonstrate the role of optimism and hope as significant and unique predictors of suicidal behaviors among primary care patients. As a majority of individuals who die by suicide visit their primary care provider within the month prior, the primary healthcare setting represents a key place for suicide assessment, prevention, and intervention. In particular, the present findings may serve to inform approaches to suicide risk assessment and treatment in the primary healthcare setting by underscoring the potential benefits of including hope and optimism within assessments and utilizing brief hope- and optimism-generating interventions with patients who exhibit suicidal behaviors. Thus, it would be valuable for future research to expand upon these findings to further advance the current understanding of factors that could possibly protect against suicide risk among primary care patients, so that the primary healthcare system can better support and treat patients.
References
Abel, E. L., & Kruger, M. L. (2005). Educational attainment and suicide rates in the United States. Psychological Reports, 97, 25–28.
Ahmedani, B. K., Stewart, C., Simon, G. E., Lynch, F., Lu, C. Y., Waitzfelder, B. E., et al. (2015). Racial/ethnic differences in health care visits made before suicide attempt across the United States. Medical Care, 53, 430–435.
Alarcon, G. M., Bowling, N. A., & Khazon, S. (2013). Great expectations: a meta-analytic examination of optimism and hope. Personality and Individual Differences, 54, 821–827.
Beautrais, A. L., Joyce, P. R., & Mulder, R. T. (1998). Psychiatric contacts among youths aged 13 through 24 years who have made serious suicide attempts. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 504–511.
Bryant, F. B., & Cvengros, J. A. (2004). Distinguishing hope and optimism: Two sides of a coin, or two separate coins? Journal of Social and Clinical Psychology, 23, 273–302.
Carver, C. S., & Scheier, M. F. (2002). The hopeful optimist. Psychological Inquiry, 13, 288–290.
Carver, C. D., Scheier, M. F., & Segerstrom, S. C. (2010). Optimism. Clinical Psychology Review, 30, 879–889.
Celano, C. M., Beale, E. E., Mastromauro, C. A., Stewart, J. G., Millstein, R. A., Auerbach, R. P., Bedoya, C. A., & Huffman, J. C. (2017). Psychological interventions to reduce suicidality in high-risk patients with major depression: A randomized controlled trial. Psychological Medicine, 47, 810–821.
Chang, E. C. (2003). A critical appraisal and extension of hope theory in middle-aged men and women: is it important to distinguish agency and pathways components? Journal of Social and Clinical Psychology, 22, 121–143.
Chang, E. C., Yu, E. A., & Hirsch, J. K. (2013a). On the confluence of optimism and hope on depressive symptoms in primary care patients: does doubling up on bonum futurum proffer any added benefits? The Journal of Positive Psychology, 8, 404–411.
Chang, E. C., Yu, E. A., Kahle, E. R., Jeglic, E. L., & Hirsch, J. K. (2013b). Is doubling up on positive future cognitions associated with lower suicide risk in Latinos?: a look at hope and positive problem orientation. Cognitive Therapy and Research, 37, 1285–1293.
Chang, E. C., Yu, E. A., Lee, J. Y., Hirsch, J. K., Kupfermann, Y., & Kahle, E. R. (2013c). An examination of optimism/pessimism and suicide risk in primary care patients: does belief in a changeable future make a difference? Cognitive Therapy and Research, 37, 796–804.
Chang, E. C., Martos, T., Sallay, V., Chang, O. D., Wright, K. M., Najarian, A. S.-M., & Lee, J. (2017). Examining optimism and hope as protective factors of suicide risk in Hungarian college students: is risk highest among those lacking positive psychological protection? Cognitive Therapy and Research., 41(2), 278–288.
Cheavens, J. S., Feldman, D. B., Gum, A., Michael, S. T., & Snyder, C. R. (2006). Hope therapy in a community sample: a pilot investigation. Social Indicators Research, 77, 61–78.
Cohen, J. (1977). Statistical power analysis for the behavioral sciences (rev. ed.). New York: Academic Press.
Davidson, C. L., & Wingate, L. R. (2013). The glass half-full or a hopeful outlook: which explains more variance in interpersonal suicide risk in a psychotherapy clinic sample? The Journal of Positive Psychology, 8, 263–272.
Davidson, C. L., Wingate, L. R., Slish, M. L., & Rasmus, K. A. (2010). The great black hope: hope and its relation to suicide risk among African Americans. Suicide and Life-threatening Behavior, 40, 170–180.
Denney, J. T., Rogers, R. G., Krueger, P. M., & Wadsworth, T. (2009). Adult suicide mortality in the United States: marital status, family size, socioeconomic status, and differences by sex. Social Science Quarterly, 90, 1167–1185.
Freedenthal, S. (2008). Assessing the wish to die: a 30-year review of the suicide intent scale. Archives of Suicide Research, 12, 277–298.
Gallagher, M. W., & Lopez, S. J. (2009). Positive expectancies and mental health: identifying the unique contributions of hope and optimism. The Journal of Positive Psychology, 4, 548–556.
Hepner, K. A., Rowe, M., Rost, K., Hickey, S. C., Sherbourne, C. D., Ford, D. E., et al. (2007). The effect of adherence to practice guidelines on depression outcomes. Annals of Internal Medicine, 147, 320–329.
Hing, E., Rui, P., & Palso, K. (2013). National ambulatory medical care survey: 2013 state and national summary tables. Hyattsville, MD: National Center for Health Statistics.
Hirsch, J. K., Conner, K. R., & Duberstein, P. R. (2007a). Optimism and suicide ideation among young adult college students. Archives of Suicide Research, 11, 177–185.
Hirsch, J. K., Wolford, K., LaLonde, S. M., Brunk, L., & Morris, A. P. (2007b). Dispositional optimism as a moderator of the relationship between negative life events and suicide ideation and attempts. Cognitive Therapy and Research, 31, 533–546.
Huffman, J. C., DuBois, C. M., Healy, B. C., Boehm, J. K., Kashdan, T. B., Celano, C. M., Denninger, J. W., & Lyubomirsky, S. (2014). Feasibility and utility of positive psychology exercises for suicidal inpatients. General Hospital Psychiatry, 36, 88–94.
Huffman, J. C., Boehm, J. K., Beach, S. R., Beale, E. E., DuBois, C. M., & Healy, B. C. (2016). Relationship of optimism and suicidal ideation in three groups of patients at varying levels of suicide risk. Journal of Psychiatric Research, 77, 76–84.
Kõlves, K., Ide, N., & De Leo, D. (2010). Suicidal ideation and behaviour in the aftermath of marital separation: gender differences. Journal of Affective Disorders, 120, 48–53.
Loveday, P. M., Lovell, G. P., & Jones, C. M. (2018). The best possible selves intervention: A review of the literature to evaluate efficacy and guide future research. Journal of Happiness Studies, 19, 607–628.
Luo, X., Wang, Q., Wang, X., & Cai, T. (2016). Reasons for living and hope as the protective factors against suicidality in Chinese patients with depression: a cross sectional study. BMC Psychiatry, 16, 252.
Luoma, J. B., Martin, C. E., & Pearson, J. L. (2002). Contact with mental health and primary care providers before suicide. A review of the evidence. American Journal of Psychiatry, 159, 909–916.
Muyan, M., & Chang, E. C. (2016). Hope as a mediator of the link between intimate partner violence and suicidal risk in Turkish women: further evidence for the role of hope agency. Journal of Interpersonal Violence. https://doi.org/10.1177/0886260516675465.
O’Keefe, V. M., & Wingate, L. R. (2013). The role of hope and optimism in suicide risk for American Indians/Alaska natives. Suicide and Life-threatening Behavior, 43, 621–633.
Osman, A., Bagge, C. L., Gutierrez, P. M., Konick, L. C., Kopper, B. A., & Barrios, F. X. (2001). The suicidal behaviors questionnaire-revised (SBQ-R): validation with clinical and nonclinical samples. Assessment, 8, 443–454.
Peterson, C. (2000). The future of optimism. American Psychologist, 55, 44–55.
Pirkis, J., & Burgess, P. (1998). Suicide and recency of health care contacts. British Journal of Psychiatry, 173, 462–474.
Rasmussen, K. A., & Wingate, L. R. (2011). The role of optimism in the interpersonal-psychological theory of suicidal behavior. Suicide and Life-threatening Behavior, 41, 137–148.
Rhee, W. K., Merbaum, M., Strube, M. J., & Self, S. M. (2005). Efficacy of brief telephone psychotherapy with callers to suicide hotline. Suicide and Life-threatening Behavior, 35, 317–328.
Rudd, D. M., & Brown, G. K. (2011). A cognitive theory of suicide: building hope in treatment and strengthening the therapeutic relationship. In K. Michel & D. A. Jobes (Eds.), Building a therapeutic alliance with the suicidal patient (pp. 169–181). Washington, DC: American Psychological Association.
Scheier, M. F., & Carver, C. S. (1985). Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychology, 4, 219–247.
Scheier, M. F., Carver, C. S., & Bridges, M. W. (1994). Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. Journal of Personality and Social Psychology, 67, 1063–1078.
Schneider, B., Grebner, K., Schnabel, A., Hampel, H., Georgi, K., & Seidler, A. (2011). Impact of employment status and work-related factors on risk of completed suicide: a case–control psychological autopsy study. Psychiatry Research, 190, 265–270.
Schulberg, H. C., Bruce, M. L., Lee, P. W., Williams, J. W., & Dietrich, A. J. (2004). Preventing suicide in primary care patients: the primary care physician’s role. General Hospital Psychiatry, 11, 337–345.
Shapira, L. B., & Mongrain, M. (2009). The benefits of self-compassion and optimism exercises for individuals vulnerable to depression. The Journal of Positive Psychology, 5, 377–389.
Sharry, J., Darmody, M., & Madden, B. (2002). A solution focused approach to working with clients who are suicidal. British Journal of Guidance and Counselling, 30, 383–399.
Snyder, C. R. (1994). The psychology of hope: You can get there from here. New York: Free Press.
Snyder, C. R. (2002). Hope theory: rainbows in the mind. Psychological Inquiry, 13, 249–275.
Snyder, C. R., Harris, C., Anderson, J. R., Holleran, S. A., Irving, L. M., Signom, S. T., et al. (1991). The will and the ways: development and validation of an individual-differences measure of hope. Journal of Personality and Social Psychology, 60, 570–585.
Snyder, C. R., Cheavens, J., & Michael, S. T. (1999). Hoping. In C. R. Snyder (Ed.), Coping: the psychology of what works (pp. 205–231). New York: Oxford University Press.
Softas-Nall, B. C., & Francis, P. C. (1998). A solution-focused approach to suicide assessment and intervention with families. The Family Journal, 6, 64–66.
Substance Abuse and Mental Health Services Administration (SAMHSA). (2014). Results from the 2013 national survey on drug use and health: mental health findings. In Rockville. SAMSHA: MD.
Tucker, R. P., Wingate, L. R., O’Keefe, V. M., Mills, A. C., Rasmussen, K., Davidson, C. L., & Grant, D. M. (2013). Rumination and suicidal ideation: the moderating roles of hope and optimism. Personality and Individual Differences, 55, 606–611.
US Department of Health and Human Services (HHS). (2012). 2012 National strategy for suicide prevention: goals and objectives for action. (DHHS publication no. 283-07-2301). Washington, DC: HHS Office of the Surgeon General and National Action Alliance for Suicide Prevention.
Voros, V., Osvath, P., Kovacs, L., Varga, J., Fekete, S., & Kovacs, A. (2006). Screening for suicidal behaviour and mental disorders with prime-MD questionnaire in general practice. Primary Care & Community Psychiatry, 11, 193–196.
Windfuhr, K., While, D., Kapur, N., Ashcroft, D. M., Kontopantelis, E., Carr, M. J., et al. (2016). Suicide risk liked with clinical consultation frequency, psychiatric diagnoses and psychotropic medication prescribing in a national study of primary-care patients. Psychological Medicine, 46, 3407–3417.
Wingate, L. R., Burns, A. B., Gordon, K. H., Perez, M., Walker, R. L., Williams, F. M., & Joiner, T. E. (2006). Suicide and positive cognitions: positive psychology applied to the understanding and treatment of suicidal behavior. In T. E. Ellis (Ed.), Cognition and suicide: theory, research, and therapy (pp. 261–283). Washington, DC: American Psychological Association.
World Health Organization (WHO). (2014). Preventing suicide: a global imperative. Geneva: WHO.
World Health Organization (WHO). (2016). Suicide rates (per 100,000), data by country, 2012. Retrieved from http://apps.who.int/gho/data/node.main.MHSUICIDE?lang=en
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5).
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Additional information
The present work was completed in partial fulfillment of the requirements for the Accelerated Master’s Degree Program in Psychology by the first author under the guidance of the second author. The authors would like to thank the members of the Perfectionism and Optimism-Pessimism (POP) Lab for their support and useful suggestions on earlier drafts of this article.
Rights and permissions
About this article
Cite this article
Lucas, A.G., Chang, E.C., Lee, J. et al. Positive Expectancies for the Future as Potential Protective Factors of Suicide Risk in Adults: Does Optimism and Hope Predict Suicidal Behaviors in Primary Care Patients?. Int J Ment Health Addiction 18, 41–53 (2020). https://doi.org/10.1007/s11469-018-9922-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-018-9922-8