Abstract
Smoking is a risk factor for death and dying for individuals who smoke and for those who inhale second hand smoke. Smokers struggle to quit smoking because of the negative affect associated with nicotine withdrawal. We assessed the efficacy of a mindfulness-based intervention for smoking cessation in individuals with mild intellectual disabilities. In addition to the basic concentration meditation, the mindfulness-based smoking cessation program included daily intention, mindful observation of thoughts, and Meditation on the Soles of the Feet. In a two-group randomized controlled trial, 51 protocol-eligible participants were randomly assigned to either the experimental group (mindfulness-based intervention) or the control group (treatment as usual). Results showed a statistically significant reduction in smoking commensurate with mindfulness-based training when compared to the treatment as usual condition. This finding was evident regardless of whether the analysis included only those who completed the study or the total sample in an intent-to-treat analysis. Furthermore, those receiving the mindfulness-based intervention were significantly more successful in abstaining from smoking during a 1-year follow-up than the treatment as usual group. These results suggest mindfulness-based interventions may be effective treatments for smoking cessation in individuals with mild intellectual disabilities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Smoking is a risk factor for death and dying. Approximately one in five deaths can be attributed directly to the effects of smoking and about 10 % of these deaths are a result of secondhand smoke exposure (Centers for Disease Control and Prevention 2008). On average, the life span of smokers is shortened by 10 years when compared to non-smokers (Jha et al. 2013). Smoking is responsible for 87 % of lung cancer deaths, as well as for many non-cancerous lung diseases, such as chronic bronchitis, emphysema, and chronic obstructive pulmonary disease (Centers for Disease Control and Prevention 2008). Smoking may also cause heart disease, aneurysms, bronchitis, emphysema and stroke, and it may worsen pneumonia and asthma, negatively impact the immune system, and increase the risk of sexual impotence in male smokers (U.S. Department of Health and Human Services 2010). Furthermore, cigarette smoking costs the United States $97 billion in lost productivity and $96 billion in health care expenditures, with another $10 billion in costs from inhaling second hand smoke (Behan et al. 2005; Centers for Disease Control and Prevention 2008).
In the United States, 19 % of adults are current smokers—those who smoke every day or on some days (Centers for Disease Control and Prevention 2012). Estimates of the prevalence of cigarette smoking by individuals with intellectual disabilities vary widely, ranging from about 2 % to 36 %, depending on the independent variables reported in the surveys (e.g., nature and size of the study sample, living arrangements, age range, gender, degree of intellectual disabilities, and comorbid mental illness) (Emerson and Turnbull 2005; Kalyva 2007; Robertson et al. 2000; Tracy and Hosken 1997). This variability suggests that some individuals with intellectual disabilities choose to smoke cigarettes as much as their peers in the general population.
The research on interventions designed to help individuals with intellectual disabilities to stop smoking is limited to just three published studies. In the first study, Peine et al. (1998) reported a study in which two individuals had been reinforced with cigarettes for not engaging in maladaptive behaviors. Peine et al. helped these two individuals reduce their smoking by 50 % over a 3-year period by thinning the reinforcement schedule through the introduction of alternative reinforcers, such as coffee, tea, diet soda pop, diet candy, fruit juices and magazines.
In the other two studies, Singh et al. (2011a, 2013a) evaluated the effectiveness of a mindfulness-based smoking cessation program with individuals diagnosed with mild intellectual disabilities. This program included the following components: basic concentration meditation, daily intention, mindful observation of thoughts, and Meditation on the Soles of the Feet. Singh et al. (2011a) used a changing-criterion analysis to show that a 37-year-old man who had smoked for 17 years was able to fade his cigarette smoking from 12 per day at baseline to 0 within 3 months, and maintain this for a year. Follow-up data showed he was able to abstain from smoking for a further 3 years. Singh et al. (2013a) replicated this study and reported similar outcomes with three additional individuals with mild intellectual disabilities.
Other studies have used mindfulness-based procedures for smoking cessation, but with participants who did not have intellectual disabilities. For example, Davis et al. (2007) used a modified version of the Mindfulness Based Stress Reduction (MBSR; Kabat-Zinn 1990) protocol with 18 individuals who had an average smoking history of 19.9 cigarettes per day for 26.4 years. Results showed that 10 of the 18 participants quit smoking during week seven of the 8-week MBSR course and were still abstinent at a 6-week post-quit follow-up.
Although this was not strictly a smoking cessation study, Bowen and Marlatt (2009) reported the effects of a brief mindfulness-based intervention on negative affect, smoking-related urges and smoking behavior among 123 nicotine-deprived college student smokers. The mindfulness-based intervention included accepting one’s feelings, sensations, or thoughts in a mindful, nonjudgmental manner, and “urge surfing” as described by Marlatt and Gordon (1985). While the mindfulness-based intervention did not reduce the urge to smoke, it reduced the students’ response to those urges.
Rogojanski et al. (2011) extended the Bowen and Marlatt (2009) study by comparing the effects of the same mindfulness-based intervention to a thought suppression strategy on cigarette craving in 61 participants in a randomized controlled trial. Results showed no significant difference in smoking behavior between the mindfulness-based intervention and the thought suppression groups, with participants in both groups smoking an average of 3.41 fewer cigarettes at post-treatment when compared to pre-treatment. However, when compared to the thought suppression group, the participants in the mindfulness-based condition showed statistically significant reductions in negative affect and depressive symptoms, and marginal reductions in the level of nicotine dependence.
Brewer et al. (2011) compared the effectiveness of mindfulness training and a standard smoking cessation treatment in a randomized controlled trial, with 88 participants. The mindfulness training was adapted from mindfulness-based manuals used in drug relapse prevention (Bowen et al. 2009; Brewer et al. 2009). Results at the end of the trial, as well as at a 17-week follow-up, showed significantly greater reductions in cigarettes smoked and point prevalence of abstinence under mindfulness training than under the standard treatment.
These mindfulness-based studies have shown either a reduction in smoking urges or smoking cessation. The two proof of concept studies by Singh et al. (2011a, 2013a) provide preliminary evidence that mindfulness-based interventions may be effective for smoking cessation in individuals with mild intellectual disabilities. The objective of the present study was to extend the current literature on the use of mindfulness-based interventions for smoking cessation in this population. Thus, we report a randomized controlled trial of a three-component mindfulness-based program for smoking cessation in individuals with mild intellectual disabilities. We hypothesized that the efficacy of the mindfulness-based intervention would be at least similar to or significantly better than that of the control condition, treatment as usual.
Method
Participants
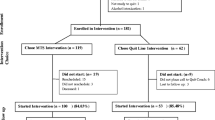
Figure 1 presents the participant flow through the study. The participants were recruited over a 3-year period from the community, by referrals from families, supported living and group home supervisors, and primary care physicians. They had to meet the following criteria to be included in the study: (1) adult with mild intellectual disability; (2) ability to give own informed consent; (3) willingness to enter a smoking cessation study; (4) approval by their primary care physician to engage in this smoking cessation program; (5) willingness to engage in mindfulness training or continue with their current treatment(s); (6) willingness to work with their Support Coordinator to collect smoking data; and (7) an absence of Axis I psychiatric diagnosis.
A total of 137 individuals with intellectual disabilities were referred to the study. Their level of intellectual disability was determined by their IQ and adaptive behavior in their school or medical records prior to the age of 18 years. Of these, 86 did not meet the requirements of the study protocol: 39 did not meet the criterion for level of intellectual functioning; following a discussion of the study protocol, 13 refused to participate in the study; prior to randomization, 10 wanted a guarantee of being included in the experimental group; another 10 did not receive clearance from their primary care physician for participation; and 14 had an Axis I psychiatric diagnosis. All 86 individuals who did not meet inclusion criteria were offered alternative treatments outside of the study protocol.
The 51 participants with mild intellectual disabilities who met the inclusion criteria were randomly assigned to either the experimental group (i.e., mindfulness-based training) or the control group (i.e., treatment as usual). Randomization was via alternate placement in the experimental and control groups. All 51 individuals had a regular day job for varying number of hours each weekday (range = 7 h to 25 h). Nine worked in garden nurseries, 5 in landscaping, 13 in local supermarkets, 2 at gas stations, 3 at pharmacies, 11 in fast food restaurants, and 8 in parks and recreation. The individuals did not have to pay to be included in the study protocol and all had consented to participate in the study.
Table 1 presents demographic and baseline smoking data by treatment condition. The experimental group consisted of 25 participants, of which 20 were males. Their mean age was 32.56 years (SD = 10.29) and they had been smoking for a mean of 15.08 years (SD = 9.70). They had participated in a number of smoking cessation programs (mean = 2.80) and had been on their current smoking cessation program for a mean of 9.44 weeks (SD = 7.17). Of the 25 who were enrolled in the experimental group, 21 completed the treatment, while four dropped out of the study at a mean of 19.75 weeks (SD = 9.74). The control group consisted of 26 participants, of which 21 were males. Their mean age was 34.40 years (SD = 10.46) and they had been smoking for a mean of 17.24 years (SD = 10.48). They had participated in a number of smoking cessation programs (mean = 2.81) and had been on their current smoking cessation program for a mean of 10.20 weeks (SD = 6.41). Of the 26 who were enrolled in the control group, 19 completed the treatment, while seven dropped out of the study at a mean of 20.42 weeks (SD = 5.40).
Trainer
The trainer had a 35-year history of service provision to people with intellectual and developmental disabilities. In addition, the trainer had a long-standing personal meditation practice, clinical expertise, and experience in mindful service delivery to individuals at all levels of intellectual functioning. The trainer provided the training individually, in small groups, or via Skype, depending on the logistics of the participants entering into the study and the training location.
Procedure
Experimental Design
This was a randomized controlled trial, with two arms: experimental (mindfulness-based intervention) and control (treatment as usual).
Assessment
Prior to entry into the study, the participants did not track how many cigarettes they smoked each day, although they had a general idea when they needed to purchase additional packets of cigarettes. Each participant was given a hand tally counter to track the number of cigarettes smoked daily and a smoking log for recording (at bedtime) the number of cigarettes smoked each day.
Reliability
Periodically, two sets of data were collected. Each participant counted the exact number of cigarettes smoked daily by pressing the mechanical tally counter button each time he or she lighted a new cigarette. Thus, relighting a partially smoked cigarette was not counted. In addition, each person’s Support Coordinator also recorded the number of cigarettes smoked by the participant during the period when both were present. This provided a real-time reliability check on the self-recording of the participant. The average overall reliability across the individuals and their Support Coordinators was 96 % (range 92–100 %).
Mindfulness Procedures
We replicated the three mindfulness-based procedures used by Singh et al. (2011a; 2013a) as follows:
Intention
Having a firm intention is one of the foundations of mindfulness practice because it sets the context for the changes that follow (Shapiro and Carlson 2009). The participants in the experimental group were taught to verbally self-affirm their intention to quit smoking and to give directionality to their conscious decision to stop smoking (Michael et al. 2012). This affirmation was to assist them to overcome inertia to give up smoking, to motivate them to continue working daily on their intention to gradually stop smoking, and to remind themselves that they wanted to do this. They used the statement, “I will not smoke today. I will not smoke anymore” as their affirmation.
Mindful Observation of Thoughts
The participants in the experimental condition were taught a standard mindfulness procedure for observing their thoughts, individualized in terms of language, idiom and explanation of practice to match their ability to understand and engage in the meditation practice. They were taught that they were not their thoughts and that desire to smoke was merely a thought, so they could observe their “desire” thoughts and let them go. This procedure was adapted to deal with each participant’s urge to smoke. In general, they were taught an inter-related series of mindfulness practices that would enable them to emotionally disengage from their thoughts. The mindfulness practices required them to (1) focus on successive thoughts, (2) observe the beginning, middle, and end of each thought, (3) observe their thoughts as clouds (“thought clouds”) passing through their awareness, without (a) pushing the thoughts away, (b) engaging with the thoughts, or (c) becoming emotionally attached to the thoughts, and (4) observe the urges to smoke as thought clouds. The procedure for these practices is presented in Table 2.
Meditation on the Soles of the Feet (SoF)
If the urge to smoke was too strong, and they could not let it go, the participants were taught the SoF procedure to rapidly move the focus of their attention from the craving to smoke to a neutral point on their body, the soles of their feet (Singh et al. 2011b). The procedure is presented in Table 3.
Fidelity of Mindfulness Training
To ensure fidelity of training, a second experienced trainer observed randomly selected audiotapes of the primary trainer’s instruction sessions. The fidelity of the training sessions was rated at 100 % by the second trainer.
Treatment as Usual
The participants in the control group continued to receive their current treatments as usual (TAU), including motivational therapies (n = 9), behavior therapies (n = 7), nicotine replacement therapy (n = 4), non-nicotine medicines (n = 4), behavior therapy and nicotine replacement therapy (n = 1), and behavior therapy and motivational therapy (n = 1). No changes were made to either the therapists or the delivery of the therapies. The fidelity of the different treatments provided to the participants in the control group was not assessed out of professional courtesy to the community therapists.
Experimental Condition (Mindfulness-Based Intervention)
Pre-baseline
One month prior to the baseline, the mindfulness trainer met with each participant in the experimental group for an hour and explained the nature of mindfulness, the daily meditation practice, the customized mindfulness practices, and the data collection requirements. The trainer taught the participants a basic concentration (Samatha) meditation that they could practice each day (McDonald 2005). They were asked to practice for just a few minutes to begin with and then to gradually increase it until they reached 20 min per day, either in one sitting or two sittings of 10 min each. They practiced this meditation for 1 month before the mindfulness-based interventions for smoking cessation were initiated.
Baseline
Given that the individuals did not have a good count of their baseline smoking rate, they entered a 4-week baseline phase during which they learned to track and record the number of cigarettes they smoked each day. During these 4 weeks, they were instructed to continue smoking as they had done prior to entry into the study, but were required to keep a log of the number of cigarettes smoked each day. In addition, they were weaned off their current smoking cessation treatments. They were taught the first three parts of the Mindful Observation of Thoughts procedure (see Table 2): Part 1 on the first day of baseline, Part II 2 days later, and Part III 3 days after that. Daily training sessions lasted 5 to 7 min on Part I, about 10 min with the addition of Part II, and about 15 min with the addition of Part III. On the last day of baseline, they were also taught the Intention procedure (see above) through discussion and practice during a 45-min training session.
Intervention
From the first day of intervention, all participants used the affirmation (i.e., Intention) every morning before getting out of bed and whenever they had a desire to smoke. During the first week, the affirmation was practiced and discussed with the trainer but, after that, it was used and practiced independently. The participants were also trained on Part IV of the Mindful Observation of Thoughts procedure (see Table 2) on the first day of intervention and, from then on, they were required to practice all four parts of this meditation for 20 min each morning. In addition, they had training on Meditation on the Soles of the Feet during 30-min supervised role-play and practice sessions with the trainer, twice a day for 5 days. During the following 10 days they were given practice assignments, after which they were instructed to use the procedure to control any desire to smoke. The participants were required to practice and use this procedure throughout the rest of the intervention period, which lasted up to 36 weeks.
Criterion Changes
During the intervention phase, criterion changes were arranged when each participant met with the trainer. The trainer was in contact with the participants once a week to review progress and to collaboratively set their next criterion change in the coming week. In between these contacts, the trainer kept in touch with each participant via telephone and adjusted the criterion changes as necessary. Criterion changes could be made after the participant maintained smoking at a set criterion for at least three consecutive days (Singh and Leung 1988). However, 3 days was a minimum requirement and the participants were free to maintain their smoking longer, at any criterion level, until they were ready to decrease to a lower level. Criterion changes continued until each participant reached zero cigarettes over three consecutive days. The phase ended when each participant did not smoke for four consecutive weeks, or reached week 40 of the study, whichever came first.
Follow-Up
During a 1-year follow-up phase, participants were contacted once every 3 months to track their abstinence, lapse, or rate of smoking for a continuous period of 1 week. There was no requirement to engage in mindfulness practices during the 1-year follow-up period, but the participants had to collect data on their smoking if they were still smoking or had lapsed during the follow-up period.
Control Condition (TAU)
Pre-baseline
One month prior to the baseline, the mindfulness trainer met with the participants in the control group for an hour, and explained the nature of the study, their role in it, and the data collection requirements. The trainer answered all their questions regarding the study and their current treatments, encouraged them to adhere to their current treatment requirements, and discussed the health and wellness benefits that might accrue from quitting smoking.
Baseline
Similar to the experimental group participants, individuals in the control group did not have a good count of their baseline smoking rate. Thus, they were taught how to track and record the number of cigarettes they smoked each day. They were instructed to continue with their treatment as they had done prior to entry into the study, but were required to keep a log of the number of cigarettes smoked each day.
Intervention
The trainer met with the participants, discussed the status of their current treatment for smoking cessation, and encouraged them to continue with their efforts to quit smoking. They were encouraged and reinforced to keep a log of the number of cigarettes each day.
Follow-Up
As with the experimental group participants, during a 1-year follow-up phase, control group participants were contacted once every 3 months to track their abstinence, lapse, or rate of smoking for a continuous period of 1 week. The participants continued to collect data on their smoking if they were still smoking or had lapsed during the follow-up period.
Data Analysis
A series of Chi-square and independent samples t-tests were used to compare the experimental and control conditions on demographic variables and baseline assessments of smoking frequency. A Chi-square test was also used to compare the frequency of drop-out occurrences across conditions, and independent samples t-tests were used to compare drop-out times (i.e., number of weeks into treatment) and characteristics of drop-outs (i.e., baseline smoking among drop-outs) across conditions.
Two sets of analyses were used to examine treatment efficacy. The first analysis included only participants who completed treatment. Descriptive statistics were used to report frequencies of complete smoking cessation across groups, and mean number of cigarettes being smoked at the end of the study (defined as either smoking zero cigarettes for 4 weeks or the number of cigarettes being smoked at week 40). An independent samples t-test was used to compare groups on mean number of cigarettes smoked at the end of the study. Finally, an independent samples t-test was used to compare groups on the mean number of cigarettes smoked during the 4-week period of 1-year follow-up. With the criterion change design adopted in this study, complete data across all 36 weeks of intervention were not available for most participants (i.e., no data were collected once the ‘0’ criterion was reached), so no repeated measures analyses were computed.
A second set of analyses adopted an “intent-to-treat” approach (West et al. 2005). All participants were retained for analyses, regardless of whether or not they dropped out. It is important to note that there are various recommended approaches for handling the missing data that occurs in ‘intent-to-treat’ analyses (e.g., Mazumdar et al. 1999). In the present study, the last observation carried forward approach was used because the amount of missing data was small, and it offers a relatively conservative test of treatment efficacy by assuming progress toward smoking cessation did not continue following drop-out (e.g., The Cochrane Collaboration 2002). Independent samples t-tests were used to compare the experimental and control groups at the end of the study and during the 4-week period of 1-year follow-up. Adopting an intent-to-treat approach enables computation of repeated measures analyses (repeated measures ANOVA) because data were available for all participants across all weeks within all phases of the study.
Results
The treatment and control conditions did not differ significantly on any demographic characteristics or baseline smoking measures (see Table 1). A total of 7 and 4 participants dropped out of the control and experimental conditions, respectively. The difference in dropout rates across groups was not statistically significant, χ 2(1) = 1.05, p = ns. The number of weeks that drop-outs remained in treatment also did not differ significantly between the control (M = 20.42, SD = 5.41) and experimental (M = 19.75, SD = 9.74) conditions, t(9) = 0.15, p = ns.
Analysis of Treatment Completers
Based on treatment completer analysis, Fig. 2 provides a visual comparison of the experimental versus control group on mean number of cigarettes smoked per week throughout all study phases. Among the participants who remained in the study until smoking cessation was successful or for the full 40 weeks, 100 % of the treatment completers in the experimental condition reached full smoking cessation (smoked zero cigarettes by the end of the study), whereas only 38.89 % of treatment completers in the control condition reached full smoking cessation. In terms of mean number of cigarettes smoked at the conclusion of the treatment phase among treatment completers, the difference between the experimental condition (M = 0, SD = 0) and control condition (M = 17.48, SD = 23.40) was statistically significant, t(36) = 3.44, p < .01 (Cohen’s d = 1.15). In terms of relapse (assessed for 1 week, every 3 months, during the year following the treatment phase), the difference in mean number of cigarettes smoked per week in the experimental condition (M = 2.31, SD = 0.27) versus the control condition (M = 39.77, SD = 0.54) remained statistically significant, t(36) = 278.39 (Cohen’s d = 87.75).
Intent-to-Treat Analyses
Due to the potential bias of including only participants who remained in the study at completion, all analyses were also conducted using an intent-to-treat approach. That is, all participants were retained in the analyses, regardless of whether or not they dropped out of the study. Based on intent-to-treat analysis, Fig. 3 provides a visual comparison of the experimental versus control group on mean number of cigarettes smoked per week throughout all study phases. Using this approach, the difference between numbers of cigarettes smoked at the conclusion of the treatment phase between the experimental condition (M = 12.40, SD = 34.50) and control condition (M = 38.27, SD = 35.58) was statistically significant, t(49) = 2.63, p < .05 (Cohen’s d = 0.74). During the follow-up phase, the mean number of cigarettes smoked per week in the experimental condition (M = 14.34, SD = 34.14) was significantly less than that of the control condition (M = 40.62, SD = 40.27), t(49) = 2.51, p < .05 (Cohen’s d = 0.70).
For the repeated measures analysis, there was a significant time by condition interaction, F(2, 47) = 10.41, p < .001 (partial η2 = 0.31), accounting for 31 % of total variability in the mean number of cigarettes smoked. As can be seen in Fig. 4, there was no significant difference between conditions during baseline, but significant differences emerged during the treatment and follow-up phases (d treatment phase = 0.55, d follow-up phase = 0.70). Pairwise comparisons with a Bonferroni correction showed that the mean number of cigarettes smoked per week during mindfulness intervention was significantly lower than the mean number of cigarettes smoked during baseline (p < .01; effect size representing improvement from baseline to intervention: d experimental = 2.15). A similar trend occurred, though with a lower effect size, for the control condition (p < .05; d control = 1.55).
Discussion
Cigarette smoking is a lethal indulgence and a preventable cause of death and disability. While education and legislation has had some impact in reducing its prevalence, almost one in five people still smoke, including those with intellectual disabilities. Quitting smoking is difficult because negative affect increases during nicotine withdrawal, and smokers often return to smoking to escape from the negative emotions produced by smoking cessation (Adams et al. 2014). We suspect that this may also be the case with people with intellectual disabilities who attempt to quit smoking, but there is scant research attesting to proven methods of smoking cessation in this population.
In this study, there were no differences between the experimental (mindfulness-based intervention) and control (treatment as usual) groups in terms of age, smoking history, number of cigarettes smoked per week during baseline, and weeks on treatment as usual prior to entry into the study. Furthermore, there were no differences across the two groups in terms of dropout rates during the study or the number of weeks the dropouts remained in the study. When considering only those who completed the study (i.e., those who remained in the study until smoking cessation was successful or for the full 40 weeks), a statistically significant number of participants stopped smoking in the experimental group when compared to those in the control group. Similarly, statistically significant findings were evident when considering all participants who entered the study, regardless of whether or not they completed the study. During the 1-yr follow-up, the mean number of cigarettes smoked by participants in the experimental group was significantly smaller than those in the control group. This finding held regardless of whether the analysis involved only those who completed the study or all who entered the study protocol. These data suggest that the mindfulness-based interventions used in this study were effective in assisting individuals with mild intellectual disabilities to stop smoking and maintain their smoking cessation for up to a year.
Two previous smoking cessation studies had indicated that customized mindfulness-based procedures might be effective with people with intellectual disabilities (Singh et al. 2011a, 2013a). The present study provides empirical data from a randomized controlled trial to support these findings. That individuals with mild intellectual disabilities can benefit from mindfulness-based procedures is beyond question given current experimental data (Harper et al. 2013; Hwang and Kearney 2013; Myers et al. 2014). For example, in another randomized controlled trial, individuals with mild intellectual disabilities showed a significant reduction in their physical and verbal aggression during and following the mindfulness-based training condition when compared to a waiting list control condition (Singh et al. 2013b).
Many smokers have reported that although they tried to quit smoking, they had to resume smoking to overcome the negative affect they experienced during nicotine withdrawal (Katz and Singh 1986). In the present study, we suspect that the use of a changing criterion design for self-determining, not only when but also how many cigarettes the individual could smoke per criterion, enabled each participant to pace his or her smoking cessation. Even though the design requires the experimenter(s) to set the criterion for change (e.g., a minimum of three consecutive days at the preset criterion for number of cigarettes smoked), the participants could maintain their smoking longer, at any criterion level, until they were ready to decrease to a lower level (Barlow et al. 2009). This enabled them to move at the pace of physiological adjustment of their body to the nicotine withdrawal, thus minimizing negative affect during successive step-wise progression to smoking cessation.
In addition to the foundational Samatha meditation, the mindfulness-based intervention included three procedures that synergistically assisted the participants to exercise self-control and manage negative affect. The first procedure, intention, precedes and provides the setting event for action. It gives directionality to the movement of the mind, thus enabling the person to actualize the intended action (Tsering 2005, 2006). In the present study, the participants invoked a daily intention to quit smoking to overcome the inertia required to adhere to the smoking cessation protocol. The second procedure, mindful observation of thoughts, enabled the participants to simply observe the urge to smoke but not identify with the desire. This helped them not to get emotionally attached with the desire to smoke, to see the desire as mere thoughts, and to let go of these thoughts. In essence, this meditation assisted them with emotion regulation. The third procedure, Meditation on the Soles of the Feet, which is derived from the basic Samatha meditation, provided a back-up process for regulating emotional arousal by shifting one’s attention from an emotionally arousing thought, event, or situation to a neutral part of the body. This process results in the fading of the emotion arousal because the mind cannot focus on two nonhabitual processes simultaneously (Foerde et al. 2006). For smoking cessation, the participants learned to shift the focus of their attention from the smoking urges to the soles of their feet. This procedure has been used effectively to curb highly emotionally charged behaviors such as anger and deviant sexual arousal (Singh et al. 2011c, 2013b).
When the data from the present study are considered in concert with those from previous studies, there appears to be a small but growing evidence-base to support the efficacy of mindfulness-based interventions for smoking cessation (Carim-Todd et al. 2013). Exactly how and why mindfulness-based interventions assist in smoking cessation is unclear. Although our study was not designed to answer these questions, understanding the nuances of emotion regulation might aid the development or refinement of mindfulness-based procedures for smoking cessation. For example, research suggests that failure to quit smoking may be better explained in terms of a smoker’s (in)ability to manage negative affect produced by nicotine withdrawal, rather than by the intensity or severity of the negative affect (Abrantes et al. 2008; Brown et al. 2005; Gonzalez et al. 2008). Thus, future research might focus on the differential abilities for effectively regulating emotions of those smokers who are successful quitters, and those that either cannot quit smoking or who lapse early after quitting. Similarly, it behooves us to investigate specific facets of mindfulness, perhaps as measured by the Five Facet Mindfulness Questionnaire (Baer et al. 2006), which may be more strongly correlated with emotion regulation deficits of quitters. Such data are needed to customize and refine mindfulness-based strategies that hone in on specific emotion regulation deficits of quitters.
This study is not without its limitations. We reported observational data on the number of cigarettes smoked by the individuals during and following mindfulness training. While we reported the reliability of the observational data, we could have also verified the participant’s smoking abstinence with carbon monoxide breath tests, plasma nicotine levels, or other physiological indices (Davis et al. 2007; Schnoll et al. 2009). Another limitation is the relatively modest sample size in both the experimental and control groups. This precluded further analyses of the treatment effects in terms of demographic and other variables, such as the types and nature of previous treatments used by the participants. Furthermore, we did not provide a measure of the participants’ mindfulness prior to and following mindfulness-based training. Although such a measure may have provided an indication of change in their mindfulness status due to the training, the absence of a mindfulness rating scale that has been psychometrically validated with this population precluded us from doing so.
In sum, this study demonstrated that a customized mindfulness-based procedure was significantly superior in producing smoking cessation by individuals with mild intellectual disabilities when compared to a treatment as usual control condition. Following the mindfulness-based training, almost all study participants continued to abstain from smoking during the 1-year follow-up. This study adds to the small emerging research literature of the use of mindfulness-based procedures by individuals with developmental disabilities (Myers et al. 2014).
References
Abrantes, A. M., Strong, D. R., Lejuez, C. W., Kahler, C. W., Carpenter, L. L., Price, L. H., Niaura, R., & Brown, R. A. (2008). The role of negative affect in risk for early lapse among low distress tolerance smokers. Addictive Behaviors, 33, 1394–1401.
Adams, C. E., Heppner, W. L., Houchins, S., Stewart, D. W., Vidrine, J. I., & Wetter, D. W. (2014). Mindfulness meditation and addictive behaviors. In N. N. Singh (Ed.), Psychology of meditation (pp. 311–343). New York: Nova Science.
Baer, R. A., Smith, G., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45.
Barlow, D. H., Nock, M. K., & Hersen, M. (2009). Single case experimental designs: strategies for studying behavior change (3rd ed.). Boston, MA: Allyn & Bacon.
Behan, D. F., Eriksen, M. P., & Lin, Y. (2005). Economic effects of environmental tobacco smoke report. Schaumburg, IL: Society of Actuaries.
Bowen, S., & Marlatt, A. (2009). Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors, 23, 666–671.
Bowen, S., Chawla, N., Collins, S. E., Witkiewitz, K., Hsu, S., Grow, J., Clifasefi, S., Garner, M., Douglass, A., Larimer, M. E., & Marlatt, A. (2009). Mindfulness-based relapse prevention for substance use disorders: a pilot efficacy trial. Substance Abuse, 30, 295–305.
Brewer, J. A., Sinha, R., Chen, J. A., Michalsen, R. N., Babuscio, T. A., Nich, C., Grier, A., Bergquist, K. L., Reis, D. L., Potenza, M. N., Carroll, K. M., & Rounsaville, B. J. (2009). Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Substance Abuse, 30, 306–317.
Brewer, J. A., Mallik, S., Babuscio, T. A., Nich, C., Johnson, H. E., Deleone, C. M., Minnix-Cotton, C. A., Byrne, S. A., Kober, H., Weinstein, A. J., Carroll, K. M., & Rounsaville, B. J. (2011). Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug and Alcohol Dependence, 119, 72–80.
Brown, R. A., Lejuez, C. W., Kahler, C. W., Strong, D. R., & Zvolensky, M. J. (2005). Distress tolerance and early smoking lapse. Clinical Psychology Review, 25, 713–733.
Carim-Todd, L., Mitchell, S. H., & Oken, B. S. (2013). Mind-body practices: an alternative, drug-free treatment for smoking cessation? A systematic review of the literature. Drug and Alcohol Dependence, 132, 399–410.
Centers for Disease Control and Prevention. (2008). Smoking attributable mortality, years of potential life lost, and productivity losses—United States, 2000-2004. Morbidity and Mortality Weekly Report, 57, 1226–1228.
Centers for Disease Control and Prevention. (2012). Current cigarette smoking among adults—United States, 2011. Morbidity and Mortality Weekly Report, 61, 889–894.
Davis, J. M., Fleming, M. F., Bonus, K. A., & Baker, T. B. (2007). A pilot study on mindfulness based stress reduction for smokers. BMC Complementary and Alternative Medicine, 7, 2. doi:10.1186/1472-6882-7-2.
Emerson, E., & Turnbull, L. (2005). Self-reported smoking and alcohol use among adolescents with intellectual disabilities. Journal of Intellectual Disabilities, 9, 58–69.
Foerde, K., Knowlton, B. J., & Poldrack, R. A. (2006). Modulation of competing memory systems by distraction. Proceedings of the National Academy of Sciences, 103, 11778–11783.
Gonzalez, A., Zvolensky, M. J., Vujanovic, A., Leyro, T. M., & Marshall, E. C. (2008). An evaluation of anxiety sensitivity, emotional dysregulation, and negative affectivity among daily cigarette smokers: relation to smoking motives and barriers to quitting. Journal of Psychiatric Research, 43, 138–147.
Harper, S. K., Webb, T. L., & Rayner, K. (2013). The effectiveness of mindfulness-based interventions for supporting people with intellectual disabilities: a narrative review. Behavior Modification, 37, 431–453.
Hwang, Y.-S., & Kearney, P. (2013). A systematic review of mindfulness intervention for individuals with developmental disabilities: long-term practice and long lasting effects. Research in Developmental Disabilities, 34, 314–326.
Jha, P., Ramasundarahettige, C., Landsman, V., Rostron, B., Thun, M., Anderson, R. N., McAfee, T., & Peto, R. (2013). 21st century hazards of smoking and benefits of cessation in the United States. New England Journal of Medicine, 36, 341–350.
Kabat-Zinn, J. (1990). Full catastrophe living: how to cope with stress, pain and illness using mindfulness meditation. New York: Dell.
Kalyva, E. (2007). Prevalence and influences on self-reported smoking among adolescents with mild learning disabilities, attention deficit hyperactivity disorder, and their typically developing peers. Journal of Intellectual Disabilities, 11, 267–279.
Katz, R. C., & Singh, N. N. (1986). Reflections on the ex-smoker: some findings on successful quitters. Journal of Behavioral Medicine, 9, 191–202.
Marlatt, G. A., & Gordon, J. R. (1985). Relapse prevention: maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press.
Mazumdar, S., Liu, K. S., Houck, P. R., & Reynolds, C. F. (1999). Intent-to-treat analysis for longitudinal clinical trials: coping with the challenge of missing values. Journal of Psychiatric Research, 33, 87–96.
McDonald, K. (2005). How to meditate. Boston, MA: Wisdom Publications.
Michael, R. B., Garry, M., & Kirsch, I. (2012). Suggestion, cognition, and behavior. Current Directions in Psychological Science, 21, 151–156.
Myers, R. E., Winton, A. S. W., Lancioni, G. E., & Singh, N. N. (2014). Mindfulness in developmental disabilities. In N. N. Singh (Ed.), Psychology of meditation (pp. 209–240). New York: Nova Science.
Peine, H. A., Darvish, R., Blakelock, H., Osborne, J. G., & Jenson, W. R. (1998). Non-aversive reduction of cigarette smoking in two adult men in a residential setting. Journal of Behavior Therapy and Experimental Psychiatry, 29, 55–65.
Robertson, J., Emerson, E., Gregory, N., Hatton, C., Turner, S., Kessissoglou, S., & Hallam, A. (2000). Lifestyle related risk factors for poor health in residential settings for people with intellectual disabilities. Research in Developmental Disabilities, 21, 469–486.
Rogojanski, J., Vettese, L. C., & Antony, M. M. (2011). Coping with cigarette cravings: comparison of suppression versus mindfulness-based strategies. Mindfulness, 2, 14–26.
Schnoll, R. A., Patterson, F., Wileyto, E. P., Tyndale, R. F., Benowitz, N., & Lerman, C. (2009). Nicotine metabolic rate predicts successful smoking cessation with transdermal nicotine: a validation study. Pharmacology, Biochemistry and Behavior, 92, 6–11.
Shapiro, S. L., & Carlson, L. E. (2009). The art and science of mindfulness: integrating mindfulness into psychology and the helping professions. Washington: American Psychological Association.
Singh, N. N., & Leung, J. P. (1988). Smoking cessation through cigarette-fading, self-recording, and contracting: treatment, maintenance and long-term follow-up. Addictive Behaviors, 13, 101–105.
Singh, N. N., Lancioni, G. E., Winton, A. S. W., Singh, A. N. A., Singh, J., & Singh, A. D. A. (2011a). Effects of a mindfulness-based smoking cessation program for an adult with mild intellectual disability. Research in Developmental Disabilities, 32, 1180–1185.
Singh, N. N., Singh, J., Adkins, A. D., Singh, A. N., & Winton, A. S. W. (2011b). Meditation on the soles of the feet: a trainer’s manual. Raleigh: Fernleaf (www.fernleafpub.com).
Singh, N. N., Lancioni, G. E., Winton, A. S. W., Singh, A. N., Adkins, A. D., & Singh, J. (2011c). Can adult offenders with intellectual disabilities use mindfulness-based procedures to control their deviant sexual arousal? Psychology, Crime and Law, 17, 165–179.
Singh, N. N., Lancioni, G. E., Winton, A. S. W., Karazsia, B. T., Singh, A. D. A., Singh, J., Singh, A. N. A., & Singh, J. (2013a). A mindfulness-based smoking cessation program for individuals with mild intellectual disability. Mindfulness, 4, 148–157.
Singh, N. N., Lancioni, G. E., Karazsia, B. T., Winton, A. S. W., Myers, R. E., Singh, A. N. A., Singh, A. D. A., & Singh, J. (2013b). Mindfulness-based treatment of aggression in individuals with intellectual disabilities: a waiting-list control study. Mindfulness, 4, 158–167.
The Cochrane Collaboration (2002). Intent to treat issues. Retrieved from: http://www.cochrane-net.org/openlearning/html/mod14–4.htm.
Tracy, J., & Hosken, R. (1997). The importance of smoking education and preventive health strategies for people with intellectual disability. Journal of Intellectual Disability Research, 41, 416–421.
Tsering, T. G. (2005). The four noble truths. Boston, MA: Wisdom.
Tsering, T. G. (2006). Buddhist psychology. Boston, MA: Wisdom.
U.S. Department of Health and Human Services. (2010). How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
West, R., Hajek, P., Stead, L., & Stapleton, J. (2005). Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction, 100, 299–303.
Acknowledgments
Portions of the data in this paper were presented at the First International Conference on Mindfulness, Sapienza University of Rome, Rome, Italy, May 8–12, 2013. We thank the individuals and Support Coordinators who participated in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Singh, N.N., Lancioni, G.E., Myers, R.E. et al. A Randomized Controlled Trial of a Mindfulness-Based Smoking Cessation Program for Individuals with Mild Intellectual Disability. Int J Ment Health Addiction 12, 153–168 (2014). https://doi.org/10.1007/s11469-013-9471-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-013-9471-0