Abstract
Background
Return to play after anterior cruciate ligament (ACL) reconstruction can increase risk for both ipsilateral graft rupture and contralateral ACL rupture. The risk for injury of the contralateral knee after ACL reconstruction could be nearly double that of ipsilateral graft rupture.
Questions/Purposes
We sought to identify independent, patient-related risk factors for contralateral ACL rupture following primary ACL reconstruction.
Methods
A national database was queried for patients who underwent primary ACL reconstruction from 2007 to 2015 with a minimum of 2 years of post-operative follow-up (n = 12,044). Patients who underwent subsequent primary ACL reconstruction on the contralateral extremity were then identified. A multivariate binomial logistic regression analysis was utilized to evaluate patient-related risk factors for contralateral ACL rupture, including demographic and comorbidity variables. Adjusted odds ratios and 95% confidence intervals were calculated for each risk factor.
Results
Of the 3707 patients who had a minimum of 2 years of database activity and comprised the study group, 204 (5.5%) experienced a contralateral ACL rupture requiring reconstruction. Independent risk factors for contralateral ACL rupture included age less than 20 years, female gender, tobacco use, and depression. Obesity, morbid obesity, type 1 diabetes, type 2 diabetes, and a history of anxiety were not significant predictors of contralateral injury.
Conclusion
We were able to adequately power an analysis to identify several significant patient-related risk factors for contralateral ACL rupture after primary ACL reconstruction, including younger age, female gender, tobacco use, and depression. This information can be used to counsel patients on the risk of injury to the contralateral knee.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anterior cruciate ligament (ACL) is the most commonly reconstructed ligament of the knee. Modern reconstructive techniques produce reliable outcomes, with a high rate of return to pre-injury sporting activity [5, 7, 13]. While return to play is a key outcome for both patients and surgeons after ACL reconstruction (ACLR), it also places patients at increased risk for both ipsilateral graft rupture and contralateral ACL rupture. A contralateral ACL tear is a devastating event for the patient, and recent long-term follow-up studies suggest that the risk for injury of the contralateral knee could be nearly double that of ipsilateral graft rupture [12, 22]. While numerous studies have reported on risk factors for ipsilateral graft rupture following ACLR, studies evaluating risk factors for contralateral ACL rupture within 2 years have been limited to institutional reviews and international registries [1, 10,11,12,13,14, 16, 18, 20,21,22]. One review of 17,346 ACLRs found risk factors associated with ipsilateral ACLR revision to include allografts, hamstring autografts, male sex, younger age, and lower body mass index (BMI); risk factors associated with an increased risk of contralateral ACLR included younger age, female sex, and lower BMI [13]. Another study of 2965 patients who underwent ACLR found that younger age, participation in a high-energy sport, and high-school level of participation were all associated with a significantly higher ACLR revision rate [17]. Studies on contralateral ACLR after primary surgery are limited due to small sample sizes from specialty centers or focus on a regional demographic, and thus are not truly representative of a general orthopedic practice. Understanding the risk of contralateral ACLR following primary ACLR is important to surgeons, patients, and therapists in counseling patients and designing post-operative rehabilitation and return-to-sport guidelines. Therefore, we sought to identify independent, patient-related risk factors for contralateral ACL rupture and reconstruction within 2 years of primary ACLR by searching a national administrative US insurance database.
Methods
The PearlDiver patient records database (www.pearldiverinc.com, Colorado Springs, CO, USA), a national administrative insurance dataset, was used for the current study. This database contains patient records from both Medicare and private payer insurers such as UnitedHealthcare and Humana. The PearlDiver Humana database contains procedural volumes, prescription drug information, basic patient demographics, and numerous other data for patients with International Classification of Disease, 9th Revision (ICD-9), diagnoses and procedures or Current Procedural Terminology (CPT) codes. The Humana database was chosen for the present study. The database covers patients insured from 2007 to the first quarter of 2016, and tracks patients across all locations (inpatient and outpatient) throughout the database years. In total, the database contains the de-identified and anonymous data of approximately 20 million patients with orthopedic diagnoses, and is thus exempt from institutional review board approval.
Patients included in this study were those who underwent arthroscopic-assisted ACLR and were queried in the database using CPT code 29888. To ensure a homogenous cohort and reduce the effect that additional procedures might have on contralateral ACL rupture, patients with the following concomitant procedures were excluded: CPT codes 27405 (open primary repair of knee collateral ligament), 27407 (open primary repair of knee cruciate ligament), 27409 (open primary repair of knee collateral and cruciate ligament), 27412 (open autologous chondrocyte implantation, knee), 27415 (osteochondral allograft, knee, open), 27416 (osteochondral autograft, knee, open), 27420 (open reconstruction of dislocating patella), 27422 (open reconstruction of dislocating patella with extensor realignment), 27425 (open lateral retinacular release), 27427 (open extra-articular ligamentous reconstruction, knee), 27428 (open intra-articular ligamentous reconstruction, knee), 27429 (open intra- and extra-articular ligamentous reconstruction, knee), 29866 (arthroscopic knee osteochondral autograft implantation), 29867 (arthroscopic knee osteochondral allograft implantation), and 29889 (arthroscopically aided posterior cruciate ligament repair/augmentation or reconstruction). In addition, patients without a coded laterality, those undergoing revision ACLR, and those without a minimum of 2-year post-operative database follow-up were excluded. This study group was then queried for patients who underwent contralateral ACLR by using the CPT code 29888 with the appropriate laterality modifier.
A multivariable binomial logistic regression analysis was performed to examine the independent effect of various patient demographics and comorbidities on the incidence of contralateral ACLR. Demographics in the regression included female sex, age younger than 20 years, obesity (BMI, 30 to 39.9 kg/m2), morbid obesity (BMI, 40 to 49.9 kg/m2), and tobacco use. Comorbidities included in the regression were type 1 diabetes, type 2 diabetes, depression, and anxiety. Unfortunately, the PearlDiver database does not index data on graft type, level of sports participation, or other descriptors of activity level. For all statistical comparisons, p < 0.05 was considered significant. SPSS version 23 for Macintosh (IBM, Armonk, NY, USA) was used for all statistical calculations.
Results
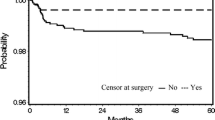
A total of 3707 unique patients met inclusion criteria and had a minimum of 2 years of database activity. This included 204 (5.5%) patients who underwent a contralateral ACLR during the study period. Independent risk factors for contralateral ACL rupture are provided in Table 1 and included age less than 20 years (OR 3.71, p < 0.0001), female gender (OR 1.48, p < 0.0001), tobacco use, (OR 1.55, p = 0.0005), and depression (OR 1.54, p < 0.0001). Obesity, morbid obesity, type 1 diabetes, type 2 diabetes, and a history of anxiety were not significant predictors of contralateral injury (p > 0.05).
Discussion
We found that the incidence of contralateral ACLR following primary reconstruction was 5.5%. In addition, we were able to isolate several patient-specific variables associated with contralateral ACLR after primary reconstruction, including age under 20 years, female gender, tobacco use, and depression. While several of these factors have been associated with subsequent contralateral ACL injury, others such as depression and tobacco use had not been adequately studied until this point. The identification of risk factors for contralateral ACLR following primary reconstruction is of high importance in counseling patients and in designing and implementing injury prevention programs for at-risk patients.
There are several limitations to our study, many of which are inherent to studies making use of administrative claims databases [24]. First, while we were able to identify several statistically significant demographic risk factors for contralateral ACLR not previously identified, many of these may lack clinical relevance. Numerous other factors have been shown to affect the risk of contralateral ACLR after primary ACLR that we were unable to identify in the PearlDiver database and therefore left uncontrolled for and unstudied. This represents a major limitation to using the PearlDiver database for researchers interested in variables including time to return to sport, type of sport, and primary reconstruction graft type [13, 16, 20]—established risk factors that may be more relevant than some of the demographic variables identified in our study. Still, our study contributes to a growing, important body of literature on risks following primary ACLR. Second, our findings rely on the quality and accuracy of the coded data within the dataset. Thus, miscoding and non-coding represent possible sources of error. Third, we defined contralateral ACL rupture by patients undergoing contralateral reconstruction, and there are likely some patients who experience contralateral rupture and opt not to undergo reconstruction. Such ACL ruptures would not have been captured. Finally, while we attempt to study a large, representative population of patients who underwent primary ACLR, our data includes patients only from a single insurer, and these findings may not hold true in other populations, such as Medicaid or Medicare beneficiaries.
While recent studies have reported that patients who sustain ACL injuries may report higher rates of symptoms of depression and that such disorders may be associated with worse post-operative outcome scores and lower rates of return to play, no studies to date have examined if depression increases the risk of contralateral ACLR. Our study found that a history of depression nearly doubles the odds of contralateral ACLR after primary reconstruction [23]. The mechanism behind such a relationship is likely multifactorial and complex. Adhering to post-operative rehabilitation protocols after ACLR has been shown to correlate with reported outcomes and recurrent injury [2, 23]. Thus, depressed patients may have a more difficult time adhering to or completing ACL rehabilitation and might therefore be at increased risk for contralateral injury when returning to sport.
Studies examining the influence of tobacco on subsequent ACL injury in either knee after ACLR have produced conflicting results [4, 8, 15]. Kaeding et al. analyzed 2488 patients from the Multicenter Orthopedic Outcomes Network (MOON) cohort and did not find an association between smoking status and ACL graft retear or contralateral tear [8]. However, Cancienne et al. examined the PearlDiver database and reported a significant association between tobacco use and ipsilateral and/or contralateral ACL rupture within 5 years post-operatively [4]. However, those authors were unable to differentiate between ipsilateral revision reconstructions and contralateral injuries. Our study demonstrated a significant association in only patients who underwent contralateral ACLR following ipsilateral reconstruction. There are multiple mechanisms by which tobacco use could increase the risk of contralateral injury. Patients who smoke have been shown to demonstrate significantly worse clinical outcome scores and increased anterior translation following primary ACLR [9, 15]. Poor functional outcomes and residual laxity following surgery might place the contralateral extremity at increased risk for injury and ACL rupture.
The other risk factors for contralateral and ipsilateral injury following primary ACLR have been previously documented and show similarities. Kaeding et al. reviewed 2683 patients from the Multicenter Orthopaedic Outcomes Network (MOON) cohort and reported that younger age, higher activity level, and allograft type were predictors of increased odds of ipsilateral graft failure [8]. Similarly, Salmon et al. studied 760 primary ACLRs and reported increased odds of ACL graft rupture in those with a contact mechanism of initial injury and those who returned to International Knee Documentation Committee level 1 or 2 sports [18]. Webster et al. reviewed 561 patients at a mean follow-up of approximately 5 years and reported odds for sustaining a contralateral ACL rupture increased threefold for patients younger than 20 years [21]. Similarly, Andernord et al. utilized the Swedish National Knee Ligament Registry and reported age younger than 20 years significantly increased the risk of contralateral ACLR in females, with a relative risk of 2.9 [1]. Our study found that patients younger than 20 years experienced a 3.71 increased odds of undergoing contralateral ACLR, which is consistent with other registry studies [1, 13]. We found that female gender was associated with significantly increased risk of contralateral ACLR, a similar finding to that reported by both Maletis et al. and Shelbourne et al. [13, 19]. Shelbourne et al. hypothesized that the reason females experience an increased incidence of contralateral injury (as compared to graft rupture) is because of smaller native ligament size in the native knee [19]. Thus, the reconstructed ACL in females results in a graft that is larger than the native ACL in the contralateral knee, protecting the reconstructed knee from reinjury and possibly predisposing the contralateral knee to ACL rupture [19]. In summary, documented risk factors for ipsilateral graft failure and contralateral ACLR are largely similar.
Finally, the remaining demographics and comorbidities failed to show any association with contralateral ACLR, including obesity or morbid obesity, type 1 or type 2 diabetes, and a history of anxiety. This is in agreement with other studies that have also shown no significant association between these factors and graft failure or contralateral ACLR [3, 6]. Some authors have suggested that patients with an elevated BMI and diabetes may be less active after ACLR and therefore at reduced risk of contralateral injury [6]. Conversely, others have hypothesized that previously unconditioned high-risk patients who undergo ACLR may experience increases in muscle control and proprioception during post-operative rehabilitation that are protective of the contralateral ACL [6].
In conclusion, we were able to adequately power an analysis to identify several significant patient risk factors for contralateral ACL rupture, including younger age, female gender, tobacco use, and depression, all of which should be used to counsel patients on their risk for future injury to the contralateral knee.
References
Andernord D, Desai N, Björnsson H, Gillén S, Karlsson J, Samuelsson K. Predictors of contralateral anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43:295–302.
Arundale AJH, Capin JJ, Zarzycki R, Smith AH, Snyder-Mackler L. Two year ACL reinjury rate of 2.5%: outcomes report of the men in a secondary ACL injury prevention program (ACL-sports). Int J Sports Phys Ther.. 2018;13:422–431.
Brophy RH, Huston LJ, Wright RW, et al. Outcomes of ACL reconstruction in patients with diabetes. Med Sci Sports Exerc. 2016;48:969–973.
Cancienne JM, Brockmeier SF, Werner BC. Tobacco use is associated with increased rates of infection and revision surgery after primary superior labrum anterior and posterior repair. J Shoulder Elb Surg. 2016;25(11):1764–1768.
Colombet P, Saffarini M, Bouguennec N. Clinical and functional outcomes of anterior cruciate ligament reconstruction at a minimum of 2 years using adjustable suspensory fixation in both the femur and tibia: a prospective study. Orthop J Sport Med. 2018;6(10):2325967118804128.
DiSilvestro KJ, Jauregui JJ, Glazier E, et al. Outcomes of anterior cruciate ligament reconstruction in obese and overweight patients. Clin J Sport Med. 2017. https://doi.org/10.1097/JSM.0000000000000521.
Edwards PK, Ebert JR, Joss B, et al. Patient characteristics and predictors of return to sport at 12 months after anterior cruciate ligament reconstruction: the importance of patient age and postoperative rehabilitation. Orthop J Sport Med. 2018;6:232596711879757.
Kaeding CC, Pedroza AD, Reinke EK, et al. Risk factors and predictors of subsequent acl injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015;43:1583–1590.
Kvist J, Kartus J, Karlsson J, Forssblad M. Results from the Swedish national anterior cruciate ligament register. Arthrosc J Arthrosc Relat Surg. 2014;30:803–810.
Lai CCH, Feller JA, Webster KE. Fifteen-year audit of anterior cruciate ligament reconstructions in the Australian Football League from 1999 to 2013: return to play and subsequent ACL injury. Am J Sports Med. 2018;46(14):3353–3360.
Mae T, Shino K, Matsumoto N, Yoneda K, Yoshikawa H, Nakata K. Risk factors for ipsilateral graft rupture or contralateral anterior cruciate ligament tear after anatomic double-bundle reconstruction. Asia-Pacific J Spor Med Arthrosc Rehabi Technol. 2014;1:90–95.
Magnussen RA, Meschbach NT, Kaeding CC, Wright RW, Spindler KP. ACL graft and contralateral ACL tear risk within ten years following reconstruction. JBJS Rev. 2015;3(1).
Maletis GB, Inacio MCS, Funahashi TT. Risk factors associated with revision and contralateral anterior cruciate ligament reconstructions in the Kaiser Permanente ACLR Registry. Am J Sports Med. 2015;43:641–647.
Nakase J, Tsuchiya H, Kitaoka K. Contralateral anterior cruciate ligament injury after anterior cruciate ligament reconstruction: a case controlled study. Sports Med Arthrosc Rehabil Ther Technol. 2012;4:46.
Novikov DA, Swensen SJ, Buza JA, Gidumal RH, Strauss EJ. The effect of smoking on ACL reconstruction: a systematic review. Phys Sportsmed. 2016;44:335–341.
Pierce T, Issa K, Cassidy K, Festa A, McInerney V, Scillia A. Risk factors for contralateral ACL injury: a single institution case–control study. J Knee Surg. 2018;31:846–850.
Ponce B, Cain E, Pflugner R, et al. Risk factors for revision anterior cruciate ligament reconstruction. J Knee Surg. 2015;29:329–336.
Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg. 2005;21:948–957.
Shelbourne KD, Gray T, Haro M. Incidence of subsequent injury to either knee within 5 years after anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2009;37:246–251.
Swärd P, Kostogiannis I, Roos H. Risk factors for a contralateral anterior cruciate ligament injury. Knee Surgery Sport Traumatol Arthrosc. 2010;18:277–291.
Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42:641–647.
Wright RW, Magnussen RA, Dunn WR, Spindler KP Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: a systematic review. J Bone Joint Surg Am. 2011;93:1159–1165.
Wu H-H, Liu M, Dines JS, Kelly JD, Garcia GH. Depression and psychiatric disease associated with outcomes after anterior cruciate ligament reconstruction. World J Orthop. 2016;7:709–717.
Zhang AL, Montgomery SR, Ngo SS, Hame SL, Wang JC, Gamradt SC. Analysis of rotator cuff repair trends in a large private insurance population. Arthroscopy. 2013;29:623–629.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jourdan M. Cancienne, MD, and Robert Browning, MD, declare that they have no conflicts of interest. Brian C. Werner, MD, reports grants and personal fees as board or committee member from American Orthopedic Society for Sports Medicine and American Shoulder and Elbow Surgeons, as well as research support from Arthrex, Inc., Biomet, and Integra LifeScience, outside the submitted work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
Informed Consent
Informed consent was waived from all patients for being included in this study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Additional information
Level of Evidence: Level IV, case series
Rights and permissions
About this article
Cite this article
Cancienne, J.M., Browning, R. & Werner, B.C. Patient-Related Risk Factors for Contralateral Anterior Cruciate Ligament (ACL) Tear After ACL Reconstruction: An Analysis of 3707 Primary ACL Reconstructions. HSS Jrnl 16 (Suppl 2), 226–229 (2020). https://doi.org/10.1007/s11420-019-09687-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-019-09687-x