Abstract
Background
Controversies still exist regarding the optimal diagnostic and therapeutic strategies in patients with prosthetic joint infections (PJI).
Questions/Purposes
How effective are preoperative and intraoperative cultures in isolating organisms and how do these culture results compare to one another? What are the results of surgical treatment of PJI in the hip and knee in an international, tertiary referral center cohort?
Patients and Methods
One hundred sixteen patients (N = 59 hip PJI, N = 57 knee PJI) were recruited prospectively to registries at three international, tertiary referral centers between December 2008 to November 2011. Retrospective review of prospective registry data including demographics, microbiology results, and operative reports was performed.
Results
Preoperative synovial fluid aspiration yielded an organism in only 45.2% and 44.4% of cases, respectively, for knee and hip PJI. False-negative rates of preoperative aspiration relative to intraoperative culture were 56% and 46% in hip and knee PJI, respectively, with discordance rates of 25% and 21.4%, respectively. Rates of negative intraoperative cultures were 15% in hip PJI and 20.7% in knee PJI. Open debridement with prosthetic retention was the most common initial revision procedure performed (48.3% of hip PJI and 63.8% of knee PJI). This method of revision was successful in 41.3% of hip PJI and 59.4% of knee PJI. Initial failure rates for prosthetic revision was lower than debridement with prosthetic retention but remained substantial in both hip PJI (initial success of one-stage exchange 60% and two-stage exchange 70%) and knee PJI (initial success of one-stage exchange 80% and two-stage exchange 75%).
Conclusion
Diagnosis and treatment of PJI remains challenging with difficulty in isolating the offending organism and with high rates of prosthetic revision and initial treatment failures. Future advances in organism isolation and international standardization of treatment protocols may improve patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prosthetic joint infection (PJI) remains one of the most common causes of revision arthroplasty. It can result in multiple revision surgeries and significant patient morbidity. Periprosthetic infection rates remain around 1–2% after primary total hip and knee arthroplasty and comprise approximately 7–12% of revision cases [4, 5, 16, 23, 39, 47]. The number of primary and revision arthroplasties being performed continues to increase every year, and as a result, the burden of periprosthetic infections will rise over time. The diagnosis and treatment of periprosthetic infections remains challenging, and significant controversy still exists as to the optimal approach for these patients.
Many diagnostic modalities have been investigated in an attempt to accurately identify patients with PJI. Hematologic testing including ESR and CRP levels, imaging studies, and synovial fluid aspiration are the most common components of the diagnostic algorithm used in suspected periprosthetic infection [2, 10, 12, 15, 17, 26–32, 38–46]. Once the diagnosis is established, current treatment protocols include irrigation and debridement with polyethylene exchange, one- and two-stage exchange arthroplasties, arthrodesis, and chronic suppression [1, 7, 8, 11, 14, 19–21, 23, 25, 30, 33, 37, 45, 48]. Factors such as patient co-morbidities, time course, soft tissue integrity, and infecting organism characteristics may all influence the surgical approach chosen [1, 7, 8, 11, 14, 19–21, 23, 25, 30, 45, 48].
The purpose of the present study was twofold: (1) to compare the rate of isolation and type of isolated organisms in pre- and intra-operative synovial fluid and tissue cultures in hip and knee PJI in an international, tertiary referral center patient cohort and (2) to compare surgical treatment algorithms for both hip and knee PJI including failure rates and need for prosthetic revision in this same patient cohort.
Patients and Methods
Study Design
This is a multicenter study performed as part of the Traveling Fellowship of the International Society of Orthopedic Centers. Participating institutions were the Hospital for Special Surgery (HSS), New York; Schulthess Klinik, Zurich; and the Royal National Orthopaedic Hospital (RNOH), London. These specialist hospitals are known to have an infection rate as low as 0.2% for primary hip and knee arthroplasty.
Patient Demographics
All patients that presented with a periprosthetic hip or knee infection at one of the three institutions from December 2008 to November 2011 were recruited prospectively into registries at the respective institutions. A retrospective review of these databases yielded patient demographic information including hospital of presentation, comorbidities, age, sex, laterality, previous revision surgery, time from implantation, and length of follow-up.
Inclusion criteria include all adult patients who had undergone primary total hip or knee arthroplasty and presented during the study period with PJI. Exclusion criteria included primary arthroplasty for malignancy, unicondylar knee arthroplasty or trochlear arthroplasty, hip resurfacing, hemiarthroplasty of the hip, infected endoprosthetic replacements, total hips or knees performed for failed fracture fixation, history of native joint septic arthritis, infected periprosthetic fractures, superficial wound infections, coexistent metabolic bone disease other than osteoporosis or inflammatory arthritis, and incomplete hospital records.
The diagnosis of periprosthetic infection was determined based on clinical presentation (sinus tract, pain, erythema), intraoperative findings (purulence), two or more positive intra-operative cultures, and histopathologic results (>10 neutrophils per high power field) consistent with infection. Diagnosis of PJI was determined by the operating surgeon based on the above characteristics and documented in the registries. Serum laboratory studies, preoperative aspiration results, and intraoperative culture results were recorded. The results between pre-operative and intra-operative cultures were compared, and subsequent organism growth from both was recorded. Data for both early (<4 weeks) and late (>4 weeks) infections from primary surgery were included.
Detailed records of treatment protocols for all cases of periprosthetic infection were obtained and classified as follows: (1) debridement with or without polyethylene exchange, (2) one-stage revision arthroplasty, (3) two-stage revision arthroplasty, (4) resection arthroplasty with or without fusion, and (5) antibiotic suppression. Initial treatment protocols were considered to have failed if a separate treatment protocol was subsequently performed. Failure rates between different treatment protocols were compared in both total hip and total knee arthroplasty with early and late infections analyzed separately from one another.
Statistical analysis
SPSS 16 statistical software package was used for analysis. Students’ t test was used for comparisons of continuous data, and chi-square test was used for comparison of categorical data with crosstabs used as required. P value of <0.05 was considered significant.
Results
PJI Hip
Demographics
There were 60 infected total hips in 59 patients (see Table 1). Patients were recruited from the following institutions: HSS—23 (39%), Schulthess Klinik—22 (35.6%), and RNOH—15 (25.4%). There were 30 male (50.8%) and 29 female (49.2%) patients. The left side was involved in 58.3% (35 patients), and the right side was involved in 41.7% (25 patients). The mean age of the patients at primary surgery was 61 years old (SD, 12 years) with a range from 31 to 86 years old (see Table 1).
Mean time period from primary surgery to infection was 3 years and 2 months (range, 4 days to 20 years) (see Table 1). There were 19 (31.7%) early infections (<4 weeks) and 41 (68.3%) late infections (>4 weeks) (see Table 1). Final follow-up ranged from 78 days to 21 years and 11 months (median, 2 years and 10 months) from the primary procedure and 47 days to 5 years and 9 months (median, 1 year and 8 months) from the revision procedure.
Sixteen patients (26.7%) had undergone previous revision for diagnoses other than infection (instability, aseptic loosening).
Culture Results
The most common organisms associated with periprosthetic hip infection were coagulase-negative staph (CONS) and methicillin-sensitive Staphylococcus aureus (MSSA) (see Table 2). Methicillin-resistant S. aureus (MRSA) was the most common isolate from patients with early infection that failed the initial surgical procedure (see Table 2). In late infections, MSSA and Staphylococcus epidermidis were the most common isolates from patients that failed initial surgical procedures (see Table 2). Preoperative diagnostic aspiration of the hip was performed in 27 hips (45%) and grew an organism in only 12 hips (44.4%) (see Table 1). Intraoperative synovial cultures grew an organism in 51 hips (85%). The remaining nine hips (15%) did not grow an organism despite clinical and intra-operative findings in the diagnostic of the infection.
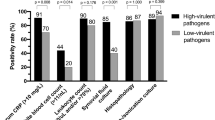
False-negative preoperative aspiration occurred in 56% of cases relative to operating room cultures. Discordance of organisms was present in 25% of preoperative aspirations relative to OR cultures. Microbial virulence did not appear to influence organism isolation from preoperative aspiration versus intraoperative culture (see Table 3). Urine cultures were positive in 3 (5%) of the 59 patients. However, none of these patients grew the same organism in urine culture and intra-operative tissue cultures from the hip.
Revision Procedures
Initial revision procedures were debridement with or without polyethylene exchange in 29 (48.3%), one-stage revision in 10 (16.7%), first stage of two-stage revision in 20 (33.3%), and girdlestone arthroplasty in 1 (1.7%) hips (see Fig. 1). The total number of revision surgeries necessary ranged from 1 to 6 (mean, 2.42; SD, 1.34). Based on center, early infection was treated by debridement with or without polyexchange (HSS—9, RNOH —2, SK—4), one-stage revision (HSS—2), and two-stage revisions (HSS—1, SK—1). For late infection, initial treatment was debridement with or without polyexchange (HSS—5, RNOH—4, SK—5), one-stage revision (HSS—2, RNOH—2, SK—4), two-stage revision (HSS—1, RNOH—6, SK—8), and one girdlestone (RNOH—1).
Flowchart depicting the initial treatment protocols followed in prosthetic joint infection of the hip and their failure rates in acute versus chronic infection. Subsequent procedures performed, overall rates of prosthetic retention, and ultimate infection status at final follow up of the patient are included.
In cases of early infection, initial debridement with or without polyethylene exchange was successful in 7/15 or 47% of the cases (see Fig. 1). In contrast, one- and two-stage revisions were both successful in 2/2 or 100% of cases (see Fig. 1). In cases of late infection, initial debridement with or without polyethylene exchange was successful in 5/14 or 36% of the cases. In contrast, one-stage revision was successful in 4/8 or 50% of cases and two-stage revision was successful in 12/18 or 67% of cases (see Fig. 1). There was a failure of initial treatment protocol in 27 (45%) of the hips. Ultimate prosthesis retention rates in patients undergoing debridement as an initial surgical procedure was 56% in early infections and 38% of cases in late infection (see Fig. 1). Patients who failed initial surgical protocols required many subsequent procedures including two girdlestone resections (3%) and four proximal femoral replacements for chronic osteomyelitis (6.7%) (see Fig. 1). Total hip arthroplasties with late infection were more prone for revision of prosthesis than those with early infection (p = 0.001). There was no association between the onset of infection (early or late) with the number of revision procedures performed (p = 0.283). There was no statistical significance in initial failure rates between individual treatments (p = 0.140).
PJI Knee
Demographics
There were 58 infected total knee arthroplasties in 57 patients, with 24 (42.1%) males and 33 (57.9%) females (see Table 4). Institution of presentation was as follows: HSS—27 (47.3%), Schulthess Klinik—14 (24.6%), and RNOH—16 (28.1%). Age of the patients at primary surgery ranged from 36 years to 81 years (mean, 63 years; SD, 10 years) (see Table 4).
Infection presented 5 days to 23 years, 9 months following the primary procedure (mean, 3 years and 2 months) (see Table 4). There were 16 (27.6%) early infections (<4 weeks) and 42 (72.4%) late infections (>4 weeks) (see Table 4). Left side was involved in 32 knees (55.2%) versus right side in 26 knees (44.8%) (see Table 4). Final follow-up ranged from 163 days to 24 years and 3 months (median, 2 years and 8 months) from the primary surgery and 108 days to 3 years and 5 months (median, 1 year and 9 months) from the first revision for infection.
Ten knees (17.2%) had undergone previous revision prior to periprosthetic joint infection for diagnoses other than infection (instability, aseptic loosening, hematoma evacuation, tibial tuberosity avulsion).
Culture Results
Preoperative diagnostic aspiration was performed in 31 knees (53.4%), of which 14 (45.2%) grew an organism (see Table 4). Intra-operative cultures grew an organism in 46 cases (79.3%), while 12 (20.7%) had negative cultures (see Table 4). False-negative rates in the preoperative aspiration were 46% relative to intraoperative cultures. Discordance between preoperative aspiration and intraoperative culture was 21.4%. S. epidermidis was the most common organism isolated from early knee PJI, while CONS and MSSA were more common in chronic infection (see Table 5). In acute infection, both successful and unsuccessful initial surgical procedures had similar organism distributions (see Table 5). In late infection, CONS was more likely to be present in failed initial procedures relative to other organisms (see Table 5). Organism distributions between preoperative aspiration cultures and intraoperative cultures were similar (see Table 6). Five patients (8.8%) had positive urine cultures. However, none of them grew the same organism in urine culture as in the tissue sample from the knee.
Revision Procedures
Total number of revision surgeries ranged from 1 to 7 (mean, 2.1; SD, 1.4). The initial surgical procedure was debridement with or without polyethylene exchange in 37 (63.8%), one-stage revision in 5 (8.6%), and first stage of two-stage revision in 16 (27.6%) knees (Fig. 2). Based on center, early infection was treated by debridement with or without polyexchange (HSS—11, SK—2) and two-stage revisions (HSS—1). For late infection, initial treatment was debridement with or without polyexchange (HSS—10, RNOH—5, SK—8), one-stage revision (HSS—1, RNOH—3, SK—1), two-stage revision (HSS—3, RNOH—8, SK—3).
Flowchart depicting the initial treatment protocols followed in prosthetic joint infection of the knee and their failure rates in acute versus chronic infection. Subsequent procedures performed, overall rates of prosthetic retention, and ultimate infection status at final follow up of the patient are included.
Surgical debridement as the first revision procedure was successful in 10/14 or 71% of early infection versus 12/23 or 52% of late infection. Ultimate prosthetic retention was 10/14 or 71% and 14/23 or 61% in these patients due to subsequent revision procedures or failure of repeat debridements (see Fig. 2). One-stage revision had initial success in 4/5 or 80% of late infections (see Fig. 2). Two-stage revision had initial treatment success in 1/2 or 50% of early infections and 11/14 or 79% of late infections (see Fig. 2). Antibiotic spacers were used in 22 (81.5%) of the 27 knees that underwent two-stage revision. Patients who failed initial treatment required many subsequent procedures including two cases of arthrodesis (see Fig. 2). At final follow-up, seven knees (12.1%) were being treated for persistent infection. The different treatments were not statistically significant from one another in initial success rates (p = 0.44). Knees with late infection had higher chance of revision of prosthesis than those with early infection (p = 0.028). However, the onset of infection did not influence the total number of revision procedures performed (p = 0.283).
Comparison of Infected Total Hip and Total Knee Arthroplasties
There existed no differences between infected hip and knee arthroplasties in the incidence of prosthetic revisions, one- versus two-stage revisions, positive bacterial growth in tissue culture, preoperative aspiration–postoperative culture discrepancy, or failure of initial treatment protocol (p > 0.05). Late infection (>4 weeks) led to higher rates of prosthetic revisions in both PJI of hip and knee (p < 0.05).
Discussion
Although the rates of infection following total hip and knee arthroplasty have decreased considerably from 9% in 1964 to 1–2%, the increase in the number of arthroplasties performed each year has increased the overall burden of PJI [4, 5, 16, 23, 25, 35, 39, 47]. Cost burden to the healthcare system has reached $500 million in the USA and £200 million in the UK with associated loss of quality of life due to treatment-related morbidity and compromised outcomes even after revision arthroplasty [23, 35, 39]. In order to reduce the burden on the health-care system and to optimize patient outcomes, it has become important to devise and refine strategies to diagnose and treat PJI [23]. In this study, we present the experience in diagnosis and treatment of PJI in three international, tertiary referral centers for PJI. The purpose of the present study was twofold: (1) to compare rate and type of organism isolation from pre- and intra-operative synovial fluid and tissue cultures in hip and knee PJI and (2) to compare surgical treatments for both hip and knee PJI including failure rates and need for prosthetic revision in our cohort.
This current study has several limitations. The average follow-up was adequate to screen for the presence of infection. It is possible that patients with shorter-term follow-up could present with failure of treatment at a later date that was not captured within our study interval. This could underestimate the failure rates associated with different treatment protocols. In addition, our follow-up may not be long enough to judge the outcomes of these treatment protocols over longer time periods. Differences in hospital protocols with the preoperative use of ESR, CRP, and intraoperative use of frozen sections precluded the assessment of these parameters in the diagnosis of periprosthetic infection. Synovial WBC was not available in the retrospective records at all institutions so they could not be compared. Antibiotic therapy used for each patient both intravenous and in the spacers was not available at all centers so could not be included in the study. Preoperative aspirations were performed at the discretion of the treating surgeon with no standardized institutional protocols. The study was a retrospective one based completely on hospital records at three separate international institutions. This requires accurate record keeping and introduces potential inter-institutional and inter-surgeon variability in defining the diagnosis and treatment of periprosthetic infection.
Synovial fluid aspiration and intraoperative tissue culture have been advocated as critical to the diagnosis of PJI and organism isolation [10, 22, 24, 25, 34, 36, 39, 41]. Similar to our study, however, previous studies have identified significant limitations in our ability to isolate organisms and diagnose infection from these modalities [6, 18, 27, 40].
In our study, preoperative synovial fluid aspiration had poor diagnostic accuracy regarding organism isolation. Preoperative synovial fluid aspiration yielded an organism in only 45.2% and 44.4% of cases, respectively, for knee and hip PJI. While the isolated organism from preoperative aspiration was accurate if positive, the high false-negative rates of synovial fluid aspiration relative to intraoperative culture make early organism isolation a challenge. Organism virulence did not appear to affect its ability to be isolated by preoperative aspiration as both high virulence organisms like MRSA and lower virulence organisms like CONS had difficulty being isolated by aspiration cultures alone. Previous studies have shown high false negative rates of synovial fluid aspiration [6, 18, 27, 40]. Contamination of aspiration results has contributed to high rates of false positivity in previous studies [27, 40]. False-negative aspiration results have been attributed to low concentrations of organisms, delay in transport or inoculating the sample, inability to aspirate fluid, and preferential adherence of microorganisms to the implant or in the bone–cement interface rather than the synovium [6, 18, 27]. These factors could account for poor organism isolation from preoperative aspirations.
In our study, intraoperative cultures had improved diagnostic results relative to preoperative aspiration; however, significant rates of negative intraoperative cultures (15% in hip PJI and 20.7% in knee PJI) made organism isolation challenging. Previous studies have found limitations to intraoperative cultures in organism isolation with a false-positive rate from 3% to 31.5% and a false-negative rate of 2% to 18% [3, 11, 13, 27–29, 31, 32, 39, 42, 46]. Potential causes of false-negative intraoperative cultures include inadequate incubation time, inappropriate choice of culture media, and prior antimicrobial therapy [27]. Methods to improve the diagnostic accuracy of both preoperative aspiration cultures and intraoperative tissue cultures are critical to early identification of affecting organisms and providing targeted antimicrobial therapy.
The second purpose of our study was to compare surgical treatments for both hip and knee PJI including failure rates and need for prosthetic revision in our cohort. Open debridement with prosthetic retention was the most common initial revision procedure performed in our cohort (48.3% of hip PJI and 63.8% of knee PJI). This method of revision failed in 58.6% of hip PJI and 40.5% of knee PJI. This was performed in the cases of acute (<4 weeks) infection and in some cases of late infection. Inter-institutional and inter-surgeon variability existed in selecting candidates for this initial treatment across centers. In certain cases, debridement with prosthetic retention was attempted prior to prosthetic exchange to avoid patient morbidity and health-care costs associated with prosthetic replacement especially in cases where symptoms may have been present for less than a couple of weeks. Early infection and knee PJI were more likely to be treated successfully with debridement and prosthetic retention relative to hip PJI and late infections. Ultimately, 23.3% of hip PJI and 41.3% of knee PJI were able to retain their implant and avoid costly and morbid revision procedures. The use of irrigation and open debridement as an initial treatment protocol in PJI remains controversial. Early (< 2 weeks) hematogenous infection with low-virulence organisms demonstrates the best results with this treatment modality, while longer infectious periods and high-virulence organisms such as MRSA have higher failure rates [7, 9, 21, 23].
Initial failure rates for prosthetic revision was lower than debridement with prosthetic retention but remained substantial in both hip PJI (initial failure of one stage exchange 40% and two stage exchange 30%) and knee PJI (initial failure of one stage exchange 20% and two stage exchange 25%). For patients with initial failure, a significant number of subsequent revision procedures are necessary to achieve infection eradication. Two-stage exchange is generally considered to be the gold standard treatment for infected total hip and knee arthroplasty and is generally more effective than the one-stage exchange in most patients [8, 14, 20, 30, 48]. Cuckler et al. report no recurrence of infection with an average follow-up of 5.4 years for 44 infected total knee arthroplasties treated with two-stage revision using articulating spacers [8]. Toulson et al. found that, at a minimum of 2-year follow-up, 94% of patients had been reimplanted and 95% remained infection free with two-stage exchange [44]. A one-stage cementless revision may be effective in carefully selected patients with a low-virulence organism [48]. The high failure rates of initial prosthetic exchange in our study highlight the need for multiple exchange procedures and the significant morbidity involved in treating patients with PJI even in cases that ultimately successfully eradicate the infection.
In conclusion, preoperative aspiration has low diagnostic yield in identifying organisms responsible for PJI with a high false-negative rate relative to intraoperative cultures. Additionally, false-negative intraoperative cultures remain problematic in organism identification. In regard to treatment of PJI in this international cohort, significant failure rates of initial procedures exist with or without prosthetic exchange across all the major centers. Inter-institutional standardized protocols to identify the most cost-effective strategies for managing these patients are necessary to optimize patient outcomes.
References
Azzam KA, Seeley M, Ghanem E, Austin MS, Purtill JJ, Parvizi J. Irrigation and debridement in the management of prosthetic joint infection: traditional indications revisited. J Arthroplasty. 2010; 25(7): 1022-1027.
Barrack RL, Harris WH. The value of aspiration of the hip joint before revision total hip arthroplasty. J Bone and Joint Surg. 1993; 75-A: 66-76.
Berbari EF, Marculescu C, Sia I, et al. Culture-negative prosthetic joint infection. Clin Infect Dis. 2007; 45(9): 1113-1119.
Charnley J. A clean-air operating enclosure. British J Surg. 1964; 51: 202-205.
Clohisy JC, Calvert G, Tull F, McDonald D, Maloney WJ. Reasons for revision hip surgery: a retrospective review. Clin Orthop Relat Res. 2004; 429: 188-192.
Costerton JW, Stewart PS, Greenberg EP. Bacterial biofilms: a common cause of persistent infections. Science, NY. 1999; 284(5418): 1318-1322.
Crockarell JR, Hanssen AD, Osmon DR, Morrey BF. Treatment of infection with débridement and retention of the components following hip arthroplasty. J Bone Joint Surg Am. 1998; 80(9): 1306-1313.
Cuckler JM. The infected total knee: management options. J Arthroplasty. 2005; 20(4 suppl 2): 33-36.
Deirmengian C, Greenbaum J, Stern J, et al. Open debridement of acute gram-positive infections after total knee arthroplasty. Clin Orthop Relat Res. 2003; 416: 129-134.
Della Valle CJ, Sporer SM, Jacobs JJ, Berger RA, Rosenberg AG, Paprosky WG. Preoperative testing for sepsis before revision total knee arthroplasty. J Arthroplasty. 2007; 22: 90-93.
Della Valle CJ, Zuckerman JD, Di Cesare PE. Periprosthetic sepsis. Clin Orthop Relat Res. 2004; 420: 26-31.
Eftekhar NS. Postoperative wound infection. In Total Hip Arthroplasty. Vol. 2, pp. 1457–1504. St. Louis, C. V. Mosby, 1993.
Fitzgerald RH, Peterson LFA, Washington JA, Van Scoy RE, Coventry MB. Bacterial colonization of wounds and sepsis in total hip arthroplasty. J Bone and Joint Surg. 1973; 55-A: 1242-1250.
Haddad FS, Muirhead-Allwood SK, Manktelow AR, Bacarese-Hamilton I. Two-stage uncemented revision hip arthroplasty for infection. J Bone Joint Surg Br. 2000; 82(5): 689-694.
Hanssen AD, Rand JA. Evaluation and treatment of infection at the site of a total hip or knee arthroplasty. Instr Course Lect. 1999; 48: 111-122.
Hernigou P, Flouzat-Lachianette CH, Jalil R, Batista SU, Guissou I, Poignard A. Treatment of infected hip arthroplasty. The Open Orthopaedics Journal. 2010; 4: 126-131.
Hughes SP, Dash CH, Benson MK, Field CA. Infection following total hip replacement and the possible prophylactic role of cephaloridine. Journal of the Royal College of Surgeons of Edinburgh. 1978; 23(1): 9-12.
Ince A, Rupp J, Frommelt L, Katzer A, Gille J, Lohr JF. Is "aseptic" loosening of the prosthetic cup after total hip replacement due to nonculturable bacterial pathogens in patients with low-grade infection? Clin Infect Dis. 2004; 39(11): 1599-1603.
Kalore NV, Gioe TJ, Singh JA. Diagnosis and management of infected total knee arthroplasty. Open Orthop J. 2011; 5: 86-91.
Kotelnicki J, Mitts K. Surgical treatments for patients with an infected total knee arthroplasty. JAAPA. 2009; 22(11): 40-46.
Koyonos L, Zmistowski B, Della Valle CJ, Parvizi J. Infection control rate of irrigation and debridement for periprosthetic joint infection. Clin Orthop Relat Res. 2011; 469(11): 3043-3048.
Lachiewicz PF, Rogers GD, Thomason HC. Aspiration of the hip joint before revision total hip arthroplasty. Clinical and laboratory factors influencing attainment of a positive culture. J Bone Joint Surg Am. 1996; 78(5): 749-754.
Leone JM, Hanssen AD. Management of infection at the site of a total knee arthroplasty. J Bone Joint Surg Am. 2005; 87(10): 2335-2348.
Marculescu CE, Berbari EF, Hanssen AD, Steckelberg JM, Osmon DR. Prosthetic joint infection diagnosed postoperatively by intraoperative culture. Clin Orthop Relat Res. 2005; 439: 38-42.
Moyad TF, Thornhill T, Estok D. Evaluation and management of the infected total hip and knee. Orthopedics. 2008; 31(6): 581-588.
Mulcahy DM, Fenelon GC, McInerney DP. Aspiration arthrography of the hip joint. Its uses and limitations in revision hip surgery. J Arthroplasty. 1996; 11: 64-68.
Müller M, Morawietz L, Hasart O, Strube P, Perka C, Tohtz S. Diagnosis of periprosthetic infection following total hip arthroplasty – Evaluation of the diagnostic values of pre- and intraoperative parameters and the associated strategy to preoperatively select patients with a high probability of joint infection. Journal of Orthopaedic Surgery and Research. 2008; 3: 31.
Pandey R, Berendt AR, Athanasou NA. Histological and microbiological findings in non-infected and infected revision arthroplasty tissues. The OSIRIS Collaborative Study Group. Oxford Skeletal Infection Research and Intervention Service. Arch Orthop Trauma Surg. 2000; 120(10): 570-574.
Pandey R, Drakoulakis E, Athanasou NA. An assessment of the histological criteria used to diagnose infection in hip revision arthroplasty tissues. Journal of Clinical Pathology. 1999; 52(2): 118-123.
Parvizi J, Adeli B, Zmistowski B, Restrepo, Greenwald AS. Management of Periprosthetic Joint Infection: The Current Knowledge: AAOS Exhibit Selection. J Bone Joint Surg Am 2012;94(14):e104 1–9.
Parvizi J, Ghanem E, Sharkey P, Aggarwal A, Burnett RS, Barrack RL. Diagnosis of infected total knee: findings of a multicenter database. Clin Orthop Relat Res. 2008; 466(11): 2628-2633.
Peersman G, Laskin R, Davis J, Peterson M. Infection in total knee replacement: a retrospective review of 6489 total knee replacements. Clin Orthop Relat Res 2001;15–23.
Rao N, Crossett LS, Sinha RK, Le Frock JL. Long-term suppression of infection in total joint arthroplasty. Clin Orthop Relat Res. 2003; 414: 55-60.
Roberts P, Walters AJ, McMinn DJ. Diagnosing infection in hip replacements. The use of fine-needle aspiration and radiometric culture. J Bone Joint Surg Br. 1992; 74: 265-271.
Sculco TP. The economic impact of infected joint arthroplasty. Orthopedics. 1995; 18: 871-873.
Mf S, Della Valle CJ, Sporer SM, Paprosky WG. Perioperative testing for joint infection in patients undergoing revision total hip arthroplasty. J Bone Joint Surg Am. 2008; 90(9): 1869-1875.
Segreti J, Nelson JA, Trenholme GM. Prolonged suppressive antibiotic therapy for infected orthopedic prostheses. Clin Infect Dis. 1998; 27(4): 711-713.
Shih LY, Wu JJ, Yang DJ. Erythrocyte sedimentation rate and C-reactive protein values in patients with total hip arthroplasty. Clin Orthop. 1987; 225: 238-246.
Spangehl MJ, Masri BA, O’Connell JX, Duncan CP. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg Am. 1999; 81(5): 672-683.
Spangehl MJ, Younger ASE, Masri BA, Duncan CP. Diagnosis of infection following total hip arthroplasty. J Bone Joint Surg Am. 1997; 79: 1578-1588.
Squire MW, Della Valle CJ, Parvizi J. Preoperative diagnosis of periprosthetic joint infection: role of aspiration. AJR Am J Roentgenol. 2011; 196(4): 875-879.
Tietjen R, Stinchfield FE, Michelsen CB. The significance of intracapsular cultures in total hip operations. Surg, GynecAnd Obstet. 1977; 144: 699-702.
Tigges S, Stiles RG, Meli RJ, Roberson JR. Hip aspiration: a cost-effective and accurate method of evaluating the potentially infected hip prosthesis. Radiology. 1993; 189: 485-488.
Toulson C, Walcott-Sapp S, Hur J, et al. Treatment of infected total hip arthroplasty with a 2-stage reimplantation protocol: update on "our institution’s" experience from 1989 to 2003. J Arthroplasty. 2009 Oct; 24(7): 1051-1060.
Tsukayama DT, Goldberg VM, Kyle R. Diagnosis and management of infection after total knee arthroplasty. J Bone Joint Surg Am. 2003; 85(Suppl 1): S75-80.
Tunney MM, Patrick S, Gorman SP, et al. Improved detection of infection in hip replacements. A currently underestimated problem. J Bone Joint Surg Br. 1998; 80(4): 568-572.
Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ. Long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res. 2006; 452: 28-34.
Yoo JJ, Kwon YS, Koo KH, Yoon KS, Kim YM, Kim HJ. One-stage cementless revision arthroplasty for infected hip replacements. Int Orthop. 2009; 33(5): 1195-1201.
Acknowledgments
The authors wish to thank the International Society of Orthopedic Centers (ISOC) for providing funding through the Traveling Fellowship for Dr. Shanmugasundaram.
Disclosures
Conflict of Interest: Saseendar Shanmugasundaram, MD, Benjamin F. Ricciardi, MD and Timothy WR. Briggs, MD have declared that they no conflict of interest. Patrick S. Sussmann, MD, receives speaker fees from Depuy and Johnson and Johnson, outside the work. Mathias P. Bostrom, MD, is a paid consultant to Smith and Nephew and serves as a board member of the Orthopedic Research Society and HSS Journal, outside the work.
Human/Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent: Informed consent was obtained from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Level of Evidence: Level IV (retrospective study). See the Guidelines for Authors for a complete description of levels of evidence.
Rights and permissions
About this article
Cite this article
Shanmugasundaram, S., Ricciardi, B.F., Briggs, T.W.R. et al. Evaluation and Management of Periprosthetic Joint Infection–an International, Multicenter Study. HSS Jrnl 10, 36–44 (2014). https://doi.org/10.1007/s11420-013-9366-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-013-9366-4