Abstract
Background
Total hip arthroplasty (THA) is one of the most successful surgical interventions devised in modern times. Attempts to change the current THA procedure with unproven innovations bring the risk of increased failure rates while trying to improve the benefit of the surgery.
Questions/Purposes
This manuscript examines the evolution of THA at the Rothman Institute illustrating the key elements that lead the success of this procedure at this institution. These key elements include femoral stem design, use of highly crossed-linked polyethylene and use of pain and rehabilitation protocols. We attempted to describe the long-term results regarding safety, effectiveness, and durability of specific THA implant designs used at this institution drawing on reported evidence in the literature.
Methods
The authors performed a review of peer-reviewed articles related to the Rothman Institute’s experience with THA.
Results
Total hip arthroplasty is an efficient, safe, and durable procedure. It is a highly successful operation to restore function and improve pain. The survivorship of THA procedures at the Rothman Institute is higher than 99% at 10 years based on mechanical failure. The use of collarless, tapered wedge femoral stem, highly crossed-linked polyethylene, and improved pain rehabilitation protocols have contributed to this success.
Conclusions
There is a well-documented long-term survivorship after THA. Future innovation in THA should address new challenges with younger and more demanding patients, rather than change current methods that have a proven good survivorship. This innovation depends mainly upon improvements in the bearing surfaces and advances in pain control and rehabilitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty (THA) is a highly successful operation that is the gold standard for surgical treatment of end-stage degenerative joint disease of the hip [20]. The procedure will be performed 572,000 times in the USA alone by the year 2030 according to Kurtz et al. [16]. Studies from the Rothman Institute have demonstrated survivorship of >99% at long-term follow-up [24, 33, 34]. There are three main areas where significant elements have contributed to the long-term survivorship and good clinical outcomes of this procedure including: specific femoral stem implants (collarless, tapered wedge), advancements in the bearing surfaces (highly crossed-linked polyethylene) and improvements of perioperative pain management and rehabilitation protocols.
This manuscript describes the evolution of total hip arthroplasty at the Rothman Institute and aims to illustrate the main characteristics of implants, bearing surfaces, and changes on pain and rehabilitation protocols that lead to successful long-term results. Additionally, the long-term results regarding safety, effectiveness, and durability of specific designs used at this institution are reported. Given the good long-term results after THA, attempts to change the current procedure with no proven or long-term followed innovations may backfire risking higher failure rates while trying to increase the benefit of the surgery.
Search Strategy and Criteria
The PubMed database was used to search relevant articles from the Rothman Institute related to THA outcomes. The searching criteria included [Rothman] and [hip arthroplasty]. This initial search showed 154 manuscripts. From those, only THA cohort studies describing outcomes and survivorship of the different implants that have been used at this institution were included. Additionally, papers related to pain management and rehabilitation protocols were included as well. A total of 27 manuscripts were included in the final review.
Results
Nine series of THA using cementless tapered femoral stems were identified [4, 10, 13–15, 18, 24, 33, 34]. Overall, the results of cementless fixation with tapered stems for THA have been outstanding. The senior author (RHR) has been utilizing one basic design for all hips from 1983 to the present, with over 13,000 THA performed. The stem design consists of a collarless, tapered wedge. The proximal portion of the titanium alloy stem is plasma sprayed for bone ongrowth (Fig. 1). The senior author transitioned from a cemented Charnley design, used from 1970 to 1983, to this design secondary to its reproducible, simple, and efficient technique. Several series, including data from the Rothman Institute, have demonstrated 0% aseptic loosening at long-term follow-up for this femoral implant [27, 28, 33, 34].
Proximal portion of the titanium alloy stem is plasma sprayed for bone ongrowth. ©Stryker 2011. Images courtesy of Stryker. “Howmedica Osteonics Corp. (‘Stryker Orthopaedics’) grants permission for a limited one-time use of this image of its product as shown and retains all copyrights and all other intellectual property for this product. Stryker Orthopaedics also must approve, in advance, any copy that is associated with the use of this image”
While the architecture of the femoral implant has remained largely unchanged, the design has undergone some minor evolutionary improvements in regard to neck geometry. The metallurgy of stem alloys has improved allowing the neck to be reduced to a trapezoidal shape, without increasing the risk of metal fatigue failure, therefore reducing the chance of component-to-component impingement (Fig. 2). Additionally, in order to facilitate recreation of the patient's femoral anatomy, the necks were made proportional to the femoral stem size and two offset options (132° and 127°) were designed.
Stem neck trapezoidal. ©Stryker 2011. Images courtesy of Stryker. “Howmedica Osteonics Corp. (‘Stryker Orthopaedics’) grants permission for a limited one-time use of this image of its product as shown and retains all copyrights and all other intellectual property for this product. Stryker Orthopaedics also must approve, in advance, any copy that is associated with the use of this image”
The criteria for the use of any surgical implant should be focused on safety, effectiveness, and durability. The effectiveness of THA is measured by pain and functional outcome. Two studies comparing the effectiveness of different stems performed at our institution were found [9, 11]. A matched pair analysis comparing the tapered, wedged design to the Charnley design at 2–5-year follow-up demonstrated no significant difference in pain or functional outcome scores [29]. In a study of 36 staged bilateral hip arthroplasty using the Charnley design in one side and tapered, wedge design in the other side, patient preference was evaluated [9]. Seventy-eight percent of patients either preferred the cementless design or had no preference. Twenty-two percent of patients preferred the cemented design.
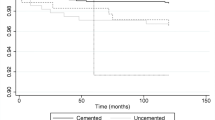
In terms of implant safety and durability, more than 300,000 total hip arthroplasties of contemporary design have been performed worldwide without a documented fracture of the femoral stem. The outcome of a cohort of 121 patients (129 hips), with a minimum 10-year follow-up, revealed an average Harris Hip Score of 92.1 with a 3.6% incidence of thigh pain. One patient in the cohort was revised [24]. The revision rate of second- and third-generation tapered stems was compared to the experience with the cemented Charnley design. At 10-year follow-up, the revision rate of third-generation tapered stems was 0.6% [4], second-generation tapered stems 0.83% [24] and Charnley stem was 1.8% [12]. A report of the senior author's first 200 third-generation stems at 9-year minimum follow-up resulted in survivorship of 99.5% [4]. An overview of revision rates of tapered stem cohorts at the Rothman Institute over 15 years of follow-up suggests that over 98% of uncemented designs remain well fixed without the need for revision (Table 1). It is important to note that several other centers have reproduced these excellent results. Controlled, non-designer data at mid-term to long-term follow-up have revealed 0–1% revision rates [8, 19, 28]. Further data from the 2009 British Hip Registry have demonstrated unsurpassed mid-term results [21].
The bearing surface options available for modern THA include metal-on-highly crossed-linked polyethylene, ceramic-on-highly cross-linked polyethylene, ceramic-on-ceramic, and metal-on-metal. The bearing surface has traditionally been the rate limiting step in longevity of the modern THA construct. While cementless implants have achieved long-term fixation, cementless components with conventional polyethylene have had survivorship limited by wear and osteolysis [22, 36]. This challenges the survivorship of THA, especially when the average lifespan of the general population has increased over the last century by 30 years. One third of 50-year-old females will live to be 100 years old [17]. Therefore, the durability of THA must meet the demands of a population that is more active and living longer.
The introduction of highly cross-linked polyethylene (HXLP) was a major advance in THA. The chemical bond formed by ionizing radiation followed by secondary annealing has led to a measurable decrease in wear [6]. Concerns exist, however, with reduction in the mechanical properties of the polyethylene and oxidation by free radicals. In a study by Rothman et al. [32], a lightly cross-linked polyethylene (ArCom (Biomet, Warsaw, IN)) was compared to a highly cross-linked polyethylene (Crossfire (Stryker Orthopaedics, Mahwah, NJ)). The volumetric wear was significantly reduced from 79.9 mm3/year in ArCom to 41.1 mm3/year in Crossfire (p = 0.0002) [32]. These results have been duplicated in other studies [1, 3]. Calvert, et al. reported more than 100% volumetric wear reduction of HXLP vs. conventional polyethylene in a randomized prospective study [3]. Long-term data reported by Engh et al. showed the wear rate of conventional polyethylene to be 0.23 mm3/year as opposed to 0.04 mm3/year in HXLP [7]. The mechanical strength of a third-generation highly cross-linked polyethylene (X3, Stryker Orthopaedics, Mahwah, NJ) as measured by yield and ultimate fatigue has also been reported to be not significantly different from conventional polyethylene [6]. Electronic spin resonance evaluation of X3 has demonstrated the virtual elimination of free radicals [35]. Given the recently published short-comings of hard-on-hard bearing surfaces, the senior author utilizes a delta ceramic head on X3 polyethylene for patients under 70 years old and a metal head on X3 polyethylene for patients 70 years and older.
Pain control and accelerated rehabilitation are not isolated from the above discussion. A multifaceted approach to accelerated rehabilitation is employed at the Rothman Institute [31]. Accelerated rehabilitation begins with patient selection. Patients deemed appropriate candidates for accelerated rehabilitation are those who are physiologically young, of ideal body weight, and are not on preoperative narcotic medications. The patients undergo a preoperative educational program starting with the preoperative surgical evaluation, continuing with an educational class (for patients and family), and so-called “prehabilitation” as necessary. Stable initial fixation of the hip arthroplasty components allows patients to weight-bear as tolerated immediately after surgery [5]. Accelerated rehabilitation is also facilitated by eliminating the so-called hip precautions [30]. Proper perioperative analgesia enables the patient to comfortably rehabilitate immediately after surgery. An extended release epidural morphine sulfate injection (DepoDur; EKR Therapeutics Inc., Bedminster, NJ), given preoperatively, provides perioperative analgesia. Furthermore, perioperative injection of marcaine, epinephrine, and ketorolac has been shown to reduce pain without significant increase in complications [2]. The use of intravenous narcotics has been greatly reduced. A multimodal regimen of nonsteroidal anti-inflammatory medications and anti-emetics, with limited oral narcotic medications has reduced the incidence of nausea [25]. Nasal oxygen and intravenous and bladder catheters are removed early to facilitate patient movement.
The above perioperative protocol has shown that it is possible to create a matrix of a 24-h stay after THA but the long-term safety has not been established. The impact of length of stay on mortality is unknown. Ottenbacher, et al. [23] demonstrated that there was a small, but consistent, increase in mortality from 1994 to 2001 as length of stay at rehabilitation centers decreased. The main concern is that serious complications such as venous thromboembolic events, myocardial infarction, and symptomatic anemia may occur in a suboptimal setting.
Discussion
Total hip arthroplasty is one of the most successful interventions of modern medicine. The outcome of THA as measured by pain relief and function has been nearly optimized. The evolution of THA in recent years has focused on prolonging the durability of THA, especially as the population of patients expected to require THA expands. Perioperative pain management protocols and accelerated rehabilitation have improved the ability of patients to recover after the operation.
The ceiling effect for THA may be such that any improvements may be in the field of bioengineering. The future of total hip arthroplasty may be so-called smart implants. Smart implants may be able to reduce the incidence of infection by attaching antibiotics to the prosthesis and osteoinductive materials may improve osseointegration [26].
As with the evolution of any process, care must be taken to undergo vigorous scientific evaluation of any changes. This is especially true, given the near perfect pain relief and function experienced with THA. This paper has described the evolution of THA at the Rothman Institute. Each step in the evolution must be carefully evaluated in controlled trials.
The main limitation of this review is that it focuses on one institution's experience with THA. The rationale for choice of implant design, bearing surface option and rehabilitation protocol is dictated by a multitude of factors that may differ from institution to institution. This review was designed as a summary of the Rothman Institute's experience, but excellent results have been reported with other approaches and techniques as well.
In conclusion, total hip arthroplasty is perhaps the most rewarding operation in the history of medicine. Future innovation in THA should address new challenges with younger and more demanding patients, rather than change current methods that have good survivorship records. We, as surgeons, are entrusted with keeping it safe, effective, and durable for our patients.
References
Bitsch RG, Loidolt T, Heisel C, Ball S, Schmalzried TP (2008) Reduction of osteolysis with use of Marathon cross-linked polyethylene. A concise follow-up, at a minimum of five years, of a previous report. The Journal of Bone and Joint Surgery. American Volume 90:1487–1491.
Busch CA, Whitehouse MR, Shore BJ, MacDonald SJ, McCalden RW, Bourne RB. The efficacy of periarticular multimodal drug infiltration in total hip arthroplasty. Clinical Orthopaedics and Related Research. 2010;468:2152–2159.
Calvert GT, Devane PA, Fielden J, Adams K, Horne JG. A double-blind, prospective, randomized controlled trial comparing highly cross-linked and conventional polyethylene in primary total hip arthroplasty. The Journal of Arthroplasty. 2009;24:505–510.
Casper DS, Kim GK, Restrepo C, Parvizi J, Rothman RH. Primary total hip arthroplasty with an uncemented femoral component five- to nine-year results. The Journal of Arthroplasty. 2011;26:838–841.
Ciccotti MG, Rothman RH, Hozack WJ, Moriarty L. Clinical and roentgenographic evaluation of hydroxyapatite-augmented and nonaugmented porous total hip arthroplasty. The Journal of Arthroplasty. 1994;9:631–639.
Dumbleton JH, D'Antonio JA, Manley MT, Capello WN, Wang A. The basis for a second-generation highly cross-linked UHMWPE. Clinical Orthopaedics and Related Research. 2006;453:265–271.
Engh CA, Powers CC, Ho H, Beykirch-Padgett SE, Hopper RH, Jr., Engh CA, Jr. The effect of poly sterilization on wear, osteolysis and survivorship of a press-fit cup at 10-year followup. Clinical Orthopaedics and Related Research. 2011.
Froimson MI, Garino J, Machenaud A, Vidalain JP. Minimum 10-year results of a tapered, titanium, hydroxyapatite-coated hip stem: an independent review. The Journal of Arthroplasty. 2007;22:1–7.
Hearn SL, Bicalho PS, Eng K, Booth RE, Jr., Hozack WJ, Rothman RH. Comparison of cemented and cementless total hip arthroplasty in patients with bilateral hip arthroplasties. The Journal of Arthroplasty. 1995;10:603–608.
Hozack W, Gardiner R, Hearn S, Eng K, Rothman R. Taperloc femoral component. A 2–6-year study of the first 100 consecutive cases. The Journal of Arthroplasty. 1994;9:489–493.
Hozack WJ, Rothman RH, Booth RE, Jr., Balderston RA. Cemented versus cementless total hip arthroplasty. A comparative study of equivalent patient populations. Clinical Orthopaedics and Related Research. 1993:161–165.
Hozack WJ, Rothman RH, Booth RE, Jr., Balderston RA, Cohn JC, Pickens GT. Survivorship analysis of 1,041 Charnley total hip arthroplasties. The Journal of Arthroplasty. 1990;5:41–47.
Hozack WJ, Rothman RH, Eng K, Mesa J. Primary cementless hip arthroplasty with a titanium plasma sprayed prosthesis. Clinical Orthopaedics and Related Research. 1996:217–225.
Keisu KS, Orozco F, McCallum JD, 3 rd, Bissett G, Hozack WJ, Sharkey PF, Rothman RH. Cementless femoral fixation in the rheumatoid patient undergoing total hip arthroplasty: minimum 5-year results. The Journal of Arthroplasty. 2001;16:415–421.
Keisu KS, Orozco F, Sharkey PF, Hozack WJ, Rothman RH, McGuigan FX. Primary cementless total hip arthroplasty in octogenarians. Two to eleven-year follow-up. The Journal of Bone and Joint Surgery. American Volume. 2001;83-A:359–363.
Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. The Journal of Bone and Joint Surgery. American Volume. 2007;89:780–785.
Lenfant C. Shattuck lecture—clinical research to clinical practice—lost in translation? The New England Journal of Medicine. 2003;349:868–874.
Lettich T, Tierney MG, Parvizi J, Sharkey PF, Rothman RH. Primary total hip arthroplasty with an uncemented femoral component: two- to seven-year results. The Journal of Arthroplasty. 2007;22:43–46.
McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component. The Journal of Bone and Joint Surgery. American Volume. 2008;90:1290–1296.
National Institute of Health. Consensus Statement Total Hip Replacement. 1994;12(5). http://consensus.nih.gov/cons/098/098_intro.htm. Accessed 8th August 2011.
National Joint Registry for England and Wales. 6th Annual Report. 2009. http://www.njrcentre.org.uk/NjrCentre/Portals/0/Sixth%20annual%20NJR%20report.pdf. Accessed 8th August 2011
Orishimo KF, Claus AM, Sychterz CJ, Engh CA. Relationship between polyethylene wear and osteolysis in hips with a second-generation porous-coated cementless cup after seven years of follow-up. The Journal of Bone and Joint Surgery. American Volume. 2003;85-A:1095–1099.
Ottenbacher KJ, Smith PM, Illig SB, Linn RT, Ostir GV, Granger CV. Trends in length of stay, living setting, functional outcome, and mortality following medical rehabilitation. JAMA : the Journal of the American Medical Association. 2004;292:1687–1695.
Parvizi J, Keisu KS, Hozack WJ, Sharkey PF, Rothman RH. Primary total hip arthroplasty with an uncemented femoral component: a long-term study of the Taperloc stem. The Journal of Arthroplasty. 2004;19:151–156.
Parvizi J, Miller AG, Gandhi K. Multimodal pain management after total joint arthroplasty. The Journal of Bone and Joint Surgery. American Volume. 2011;93:1075–1084.
Parvizi J, Wickstrom E, Zeiger AR, Adams CS, Shapiro IM, Purtill JJ, Sharkey PF, Hozack WJ, Rothman RH, Hickok NJ. Frank Stinchfield Award. Titanium surface with biologic activity against infection. Clinical Orthopaedics and Related Research. 2004:33–38.
Pieringer H, Auersperg V, Griessler W, Bohler N. Long-term results with the cementless Alloclassic brand hip arthroplasty system. The Journal of Arthroplasty. 2003;18:321–328.
Pospischill M, Knahr K. Cementless total hip arthroplasty using a threaded cup and a rectangular tapered stem. Follow-up for ten to 17 years. The Journal of Bone and Joint Surgery. British Volume. 2005;87:1210–1215.
Purtill JJ, Eng K, Rothman RH, Hozack WJ. Heterotopic ossification. Incidence in cemented versus cementless total hip arthroplasty. The Journal of Arthroplasty. 1996;11:58–63.
Restrepo C, Mortazavi SM, Brothers J, Parvizi J, Rothman RH. Hip dislocation: are hip precautions necessary in anterior approaches? Clinical Orthopaedics and Related Research. 2011;469:417–422.
Rothman RH. Accelerated Rehabilitation for Total Hip Arthroplasty. In: The Hip Society. Washington, D.C.: 2005.
Rothman RHS, P.F.; Hozack, W.J.; Martell, J. Wear performance of conventional (Arcom) and highly cross-linked acetabular liners in bilateral total hip arthroplasty. The Journal of Arthroplasty. 2004;19:261.
Sakalkale DP, Eng K, Hozack WJ, Rothman RH. Minimum 10-year results of a tapered cementless hip replacement. Clinical Orthopaedics and Related Research. 1999:138–144.
Teloken MA, Bissett G, Hozack WJ, Sharkey PF, Rothman RH. Ten to fifteen-year follow-up after total hip arthroplasty with a tapered cobalt-chromium femoral component (tri-lock) inserted without cement. The Journal of Bone and Joint Surgery. American Volume. 2002;84-A:2140–2144.
Wang A, Yau SS, Essner A, Herrera L, Manley M, Dumbleton J. A highly crosslinked UHMWPE for CR and PS total knee arthroplasties. The Journal of Arthroplasty. 2008;23:559–566.
Zicat B, Engh CA, Gokcen E. Patterns of osteolysis around total hip components inserted with and without cement. The Journal of Bone and Joint Surgery. American Volume. 1995;77:432–439.
Disclosures
(MSA) certifies that he has or may receive payments or benefits from a commercial entity (Zimmer) related to this work. (RHR) certifies that he has or may receive payments or benefits from a commercial entity (Stryker, Riverside) related to this work. One or more of the authors (MSA) has received research funding (DePuy). CAH certifies that he has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Level of Evidence: Level IV: Theraputic Study. Systematic Review of Level IV Studies
Rights and permissions
About this article
Cite this article
Austin, M.S., Higuera, C.A. & Rothman, R.H. Total Hip Arthroplasty at the Rothman Institute. HSS Jrnl 8, 146–150 (2012). https://doi.org/10.1007/s11420-012-9268-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-012-9268-x