Abstract
Background
Locking plates have been used increasingly for the management of distal humerus fractures. Studies that compare patient-centered outcomes between locking and non-locking fixation for distal humerus fractures are lacking.
Questions/Purposes
The purposes of this study were to (1) determine whether locking plates offered superior fixation compared with non-locking plates for distal humerus fractures, (2) determine whether the use of locking plates was associated with fewer complications, and (3) determine whether locking plate use resulted in superior radiographic outcome compared with non-locking plates. Lastly, another aim was to determine the average cost difference associated with locking plate use versus non-locking plate use for distal humerus fracture fixation.
Patients and Method
Demographic, clinical, and radiographic data including loss of fixation, range of motion, rate of infection, nonunion and reoperation, as well as measures of fixation were collected retrospectively and compared on 96 patients with surgically treated AO type 13C distal humerus fractures (65 locking, 31 non-locking) at 6-week and 6-month follow-up. Average costs of locking and non-locking constructs were calculated and compared.
Results
Three in 96 (3.1%) of all cases experienced loss of fixation, with no difference between the two groups. There was no difference between locking and non-locking groups with regard to the rate of nonunion, infection, and reoperation at 6 weeks and 6 months. On average, locking plate constructs were 348% more expensive than non-locking constructs.
Conclusion
While there are some significant differences in radiographic parameters and cost between locking and non-locking constructs for internal fixation of intra-articular distal humerus fractures, there were no statistically significant differences in clinical outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Intra-articular fractures of the distal humerus are among the most challenging problems that orthopedic surgeons encounter for several reasons, including the multifaceted articular anatomy of the distal humerus with three separate articulations: the proximity of neurovascular structures, the frequent occurrence of metaphyseal bone loss and significant comminution, and the unforgiving tendency of the elbow toward capsular stiffness and heterotopic ossification [7, 16]. Historically, these injuries were treated by means of closed reduction and slinging (“bag of bones” technique) because the results of open reduction and internal fixation were so poor [2]. Given advances in the techniques of open reduction and internal fixation with the goal of anatomic restoration and early mobilization, the standard of care shifted to open treatment of these injuries. These techniques utilized compression plating and screw fixation of both medial and lateral columns, with arguments made for both parallel and orthogonal plate orientations [1, 6, 8, 14]. The introduction of locking plate technology approximately a decade ago ushered in the latest advances for the management of intra-articular distal humerus fractures, offering enhanced biomechanical properties and more robust fixation.
Despite the possible advantages that locking plate fixation may provide, there are potential disadvantages and concerns regarding its use, including increased cost, factory-determined constraints of fixed-angle screws, malalignment, cross-threading of screws, and loss of diaphyseal fixation [4]. Data do exist regarding the use of locking plate technology in comparison to non-locking plates for distal humerus fractures, but only with attention to biomechanical parameters [10, 15]. No study to date exists that compares patient-centered outcomes between locking and non-locking fixation for distal humerus fractures. One might suggest that standard non-locking screws, well-placed to maximize subchondral buttressing, might perform as well or better than locking screws placed through the factory preset trajectories which are often distant from and not parallel to the articulation of the distal humerus. Ultimately, the clinical benefits of locking plate fixation for distal humerus fractures are not known.
The purpose of this study was to determine whether there was any appreciable difference between distal humerus fractures repaired with non-locking or locking plates with regard to clinical and radiographic outcomes. Specifically, we sought to (1) determine whether locking plates offered superior fixation compared with non-locking plates for distal humerus fractures, (2) determine whether the use of locking plates was associated with fewer complications, and (3) determine whether locking plate use resulted in superior radiographic outcome compared with non-locking plate use for distal humerus fractures. Lastly, this study sought to determine the average cost difference associated with locking plate use versus non-locking plate use for distal humerus fracture fixation.
Materials and Methods
This study was a retrospective comparison of intra-articular fractures of the distal humerus treated using either a locking or a non-locking plate fixation. After Institutional Review Board approval was obtained, patients eligible for inclusion were retrospectively identified at three academic level I trauma centers using billing records and trauma registries over a 6-year period (2002–2008). Patients were initially identified by current procedural terminology code for open reduction internal fixation of supracondylar or transcondylar humerus fracture with intercondylar extension (24546). From this list, patients were further selected based on the following inclusion criteria: (1) complete articular fracture (AO type 13C), as classified by the senior authors based on individual review of injury radiographs and/or computed tomography scan; (2) age >16 years; (3) ORIF within 4 weeks of initial injury; and (4) a minimum of 6 weeks of radiographic and clinical follow-up. The exclusion criteria were as follows: (1) follow-up <6 weeks; (2) distal humerus fracture that was not AO type 13C; (3) combined use of locking and non-locking plates for fixation; and (4) use of only a single plate for fixation.
Patient characteristics, including age, sex, and presence of diabetes mellitus, were recorded in a de-identified data collection sheet for each eligible patient. Ninety-six patients met all the inclusion and exclusion criteria with at least 6-week follow-up. Fifty-three percent (51/96) were female. Thirty-eight percent (37/96) sustained open injuries. Sixty-eight percent (65/96) of cases were repaired with strictly locking plate fixation, whereas 32% (31/96) utilized non-locking plates. Seventy-seven percent (74/96) featured an orthogonal plating construct; the remaining 23% (22/96) relied on parallel column plating. Of the original 96 patients with 6-week follow-up, 60 went on to have at least 6 months of follow-up: 39 patients had locking fixation and 21 with non-locking fixation. Average follow-up was 45 weeks (SD = 35 weeks; range, 6–176 weeks; Table 1).
Injury data were compiled including the mechanism of injury, associated elbow injury, presence of open fracture neurovascular injury requiring primary repair, and presence of ulnar nerve neuropathy. A total of 22 trauma or hand fellowship trained orthopedic surgeons performed open reduction and internal fixation. Details regarding the operative reconstruction and radiographic parameters were obtained from operative reports and postoperative X-rays. This included the type of plates used (non-locking or locking); the arrangement of the plates (parallel or 90–90); whether or not the plates were pre-contoured; the use of olecranon osteotomy, ulnar nerve management (transposed or protected); the number of total screws in the distal fracture fragment (including how many were locked screws); the number of screws that crossed the midline (total, number in and outside the plate); the number of column screws; and the diaphyseal–screw angle for the most distal screw both within and outside the plate. Articular step-off from immediate postoperative films was recorded. We grouped the cases into 0 mm of articular step-off versus >0 mm. Arc of motion was noted from the most recent clinic note. For the purposes of this study, bony union was defined as radiographic evidence of bridging callus across the fracture site. All final follow-up radiographs were retrospectively reviewed by the attending authors (WO, JJ, DR) to determine bony union status. Additionally, the final radiographs were compared with the immediate postoperative radiographs to determine any possible loss of reduction, defined as a displacement of the hardware relative to the bone or bony fragments relative to one another of at least 2 mm. The number of reoperations for hardware removal or contracture release was noted for each patient as well as the rate of postoperative infection.
A simple cost analysis was performed for the locking plate construct and the non-locking construct as supplied by Synthes Inc., USA (West Chester, PA). Based on the operative experience of the authors, it was assumed that the average locking construct consisted of one seven-hole, 3.5-mm LCP® medial distal humerus plate, one nine-hole, 3.5 mm LCP® posterolateral distal humerus plate, four 2.7-mm self-tapping locking screws, and six 3.5-mm self-tapping cortical screws. The average non-locking construct was assumed to include one eight-hole, 3.5-mm LC-DCP® plate, one eight-hole, 3.5-mm reconstruction plate, and twelve 3.5-mm self-tapping cortical screws. The cost for each individual component was obtained in a price quote from a company vendor in September 2008.
The primary outcome measures for this study was loss of fixation. Secondary outcome measures analyzed include bony union, presence of intra-articular step-off, mean arc range of motion, rate of reoperation (for either hardware removal or contracture release), rate of infection, cost of implants, and measures of fixation. Chi-square or Fisher’s exact test was used to assess categorical variables. A post hoc power analysis was conducted to determine the sample size necessary to detect a significant difference (p < 0.05) in loss of fixation and nonunion between locked and non-locked groups assuming beta error equaled 0.80. Assuming the true rates fixation loss were what was observed in this study, a 0.05 level Fisher’s exact test would detect a significant difference with 80% power given at least 319 cases in the locking group and 638 cases in the non-locking group. Assuming instead sample sizes equal to those in this study (65 in the locking group and 31 in the unlocking group), the power for this study was calculated to be 10%. A Wilcoxon rank sum test was used to compare continuous variables between locking and non-locking fixations, including the number and positioning of screws. A proportional odds model was fit to identify risk factors for the intra-articular step-off. A 5% significance level was used for all statistical inferences (p < 0.05). Statistical analysis was performed for patients with at least 6 weeks of follow-up. A separate analysis was performed for those completing at least 6 months of follow-up.
Results
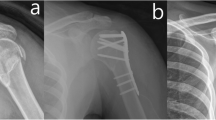
Locking plates were statistically much more likely to be arranged in an orthogonal layout (p < 0.0001) and used in older patients (p = 0.02). There was a trend toward more frequent locking plate usage in females compared with males (p = 0.13; Table 2). There were no other significant differences in patient demographics, injury patterns, or perioperative management between groups. The overall union rate was 97% (93/96). Of the three cases that went on to nonunion, two underwent revision ORIF and the last deferred any further surgical treatment. Belying the difficulty of achieving and maintaining a perfect articular reduction, 19% (18/96) of cases did have some visible articular step-off, with the average incongruity at 2 mm (SD = 1; range, 1–3 mm).
The overall rate of fixation failure was 3% (3 of 96). There was no observed difference in the rate of fixation failure between the locking plate group and the non-locking plate group (p = 0.24). Despite this loss in fixation, two of the three cases went on to heal, while the other was treated with total elbow arthroplasty.
There was no difference between the locking and non-locking groups with regard to the clinical outcomes or complications including the incidence of nonunion (p = 1.0), infection rate (p = 0.21), presence of ulnar neuropathy (p = 0.46) or rate of reoperation for hardware removal (p = 0.20) or contracture release (p = 0.54) at 6 weeks of follow-up (Table 2). Additionally, there was no difference detected in the mean arc range of elbow motion between groups (p = 0.99). When the analysis was repeated for this subset of patients with 6 months of follow-up, no differences were again found between groups for nonunion, rate of reoperation, or range of motion (Table 3).
Radiographic analysis between locking and non-locking constructs revealed that the most distal screw within non-locking plates was more likely to achieve a more perpendicular diaphyseal–screw angle compared with locking plates (p = 0.01). There was a trend toward a greater number of screws crossing the midline in non-locking plate constructs (p = 0.173; Table 4). There was no difference between groups regarding the incidence of articular step-off (p = 0.51). A proportional odds model, evaluating the risk factors for intra-articular step-off, suggested that patients sustaining an open fracture were 1.83 times more likely to demonstrate postoperative intra-articular step-off than those sustaining a closed fracture (Table 5).
The estimated average calculated cost for locking construct was US $2,740.02, and the cost for the non-locking construct was US $788.34. The locking constructs cost on average 348% more than the non-locking constructs.
Discussion
Despite the stated biomechanical and theoretical advantages that locking plate technology affords, there are scant clinical data directly comparing its efficacy to non-locking plate fixation for the management of intra-articular distal humerus fractures. This study sought to determine whether locking plates offered any advantages in the treatment of these fractures with regard to fixation, clinical and radiographic outcomes, as well as determining the average cost difference associated with locking plate use versus non-locking plate use. The results of this study have shown that fixation failure is not more likely to occur with non-locking fixation, and no differences were found between groups with regard to the rate of perioperative complications or range of motion at 6 weeks and 6 months of follow-up. The data did demonstrate that while non-locking constructs allowed for more ideal screw positioning, the rate of articular step-off was equivalent between groups. The average locking plate construct for this injury pattern was found to be over three times more expensive than the average non-locking plate construct.
There are limitations to this study. This is a retrospective case series from several institutions. There was no randomization of locking or non-locking plate fixation in these cases; the implants were chosen at the discretion of each individual surgeon. This leads to a selection bias as osteoporotic and elderly patients were more likely to receive locking plate fixation. This is reflected in our data because locking plates were significantly more likely to be used in older patients, as well as in females. Another bias inherent in the retrospective nature of this study was the fact that the treating surgeons determined union radiographically in an unblinded manner. Another limitation involved a lack of reliability testing with the measurement of articular step-off. Under the system utilized, a single surgeon determined how much step-off was present through a single measurement. Repeat measures of the same radiograph by the same surgeon or interpretation of the same radiograph by another surgeon was not performed. This did not allow for an inter- or intra-observer reliability determination, which would have been scientifically more robust. Another limitation to this study was that it was underpowered. Given that complete articular fractures of the distal humerus are not common injuries, only 96 cases were available for analysis based upon inclusion and exclusion criteria. With such a small number of cases to analyze, achieving statistically significant results between groups becomes more difficult. Lastly, the cost analysis undertaken here is quite simple. It considers only the difference in cost between the two different types of implants. It does not take into account other factors including operating time, perioperative complications, and the management thereof, which would likely have a larger impact on the ultimate cost to the patient and society.
As this is the first study to perform a direct clinical and radiographic comparison between locking and non-locking plates for fixation of intra-articular distal humerus fractures, there are minimal data for comparison. However, there are biomechanical data on the subject. A comparison of non-locking and locking plate constructs in a cadaver model found that the stiffness of the construct was no different if arranged in the same configuration; neither construct failed under cyclical loading [10]. The same group in a different study compared orthogonal constructs using conventional reconstruction plates, locking compression plates, and pre-contoured distal humerus locking plates in cadaveric specimens of varying bone mineral densities [15]. Again, there was no difference in the stiffness of all three constructs. However, under cyclical loading, conventional plates were significantly much more likely to experience screw pullout failure at lower bone mineral densities than either of the locking plate constructs. The authors concluded that fixation with either locking or non-locking plates is acceptable in patients with good bone mineral density, but locking plates could prove to be more effective in patients with lower bone mineral density. Not surprisingly, the population undergoing locked plate fixation in this study was significantly more aged than the non-locking group and likely had a higher rate of osteoporosis as a result.
Again, there are no data currently available that compare clinical outcomes and complications rates between these two types of constructs for C-type distal humerus fractures. The lack of demonstrated difference in clinical outcome or complications shown in this study should not come as a surprise. What we do know is that other studies comparing locking and non-locking fixation for fractures other than the distal humerus have not shown a major impact on outcome. This includes comparisons involving treatment of the distal radius, proximal humerus, and proximal tibia fractures; all have shown equivocal rates of nonunion, functional outcome, and complication rates [3, 5, 9, 11].
Sanchez-Sotelo et al. [12, 13] have proposed objectives for the treatment of complex fractures of the distal humerus, and they have achieved good results with this protocol. Their approach involves eight technical objectives designed to enhance the stability of these fractures by maximizing fixation and interdigitating screws for a re-bar effect. Compared with the locking plates used in this study, the non-locking plate constructs used seemed to allow more freedom for screw direction and placement as these cases were more likely to achieve a distal screw placement horizontal to the joint surface and achieve a greater number of screws crossing the midline—both proposed as objectives for ORIF of the distal humerus [12]. It should be noted that there is variable angle locking technology available that allows the surgeon to place locking screws with some surgeon control of the trajectory. This may allow for increased surgeon flexibility in screw trajectory while maintaining the fixed-angle construct. While intuitive and rational, the utility of these technical objectives has yet to be proven. In fact, despite the differences in screw placement and trajectory, our data have shown that there is no difference between these constructs with regard to the quality of reduction, loss of reduction, or rate of bony union despite the locking implants costing over three times as much as the non-locking implants.
The articular comminution in these grade 3C injuries makes them challenging to treat—be it a result of compromised bone quality from osteoporosis or a high-energy mechanism. The proportional odds model showed that the presence of an open fracture was a risk factor for intra-articular step-off while plate type was not. While we cannot fully explain this observation, it could represent a “worst of the worst” phenomenon where the grade 3C open fractures had even more comminution and bone destruction than the grade 3C closed injuries.
In conclusion, this study is the first and only clinical investigation comparing locking and non-locking constructs with specific attention toward fractures of the distal humerus. The results of this study verify what has been shown in distal radius, proximal humerus, and tibial plateau fractures when comparing these two types of fixation: there is no statistically significant advantage that locking plates provide with regard to adequacy of fixation, clinical outcomes, and complications. While non-locking fixation tended to allow for ideal screw placement, the clinical impact of this is unknown. This study does not provide enough data to make clinical recommendations at this time, but it does serve as a critical analysis of locking plate fixation that should help stimulate future research on the topic. We look forward to future randomized studies to better address this issue.
References
Arnander MW, Reeves A, MacLeod IA, Pinto TM, Khaleel A.A biomechanical comparison of plate configuration in distal humerus fractures. J Orthop Trauma. 2008;22(5):332–6.
Brown RF, Morgan RG. Intercondylar T-shaped fractures of the humerus. Results in ten cases treated by early mobilization. J Bone Joint Surg Br. 1971;53(3):425–8
Hahnloser D, Platz A, Amgwerd M, Trentz O: Internal fixation of distal radius fractures with dorsal dislocation: Pi-plate or two 1/4 tube plates? A prospective randomized study. J Trauma 1999;47:760–765.
Haidukewych GJ, Ricci W. Locked plating in orthopaedic trauma: a clinical update. J Am Acad Orthop Surg 2008;16(6):347–55 (review).
Handschin AE, Cardell M, Contaldo C, Trentz O, Wanner GA: Functional results of angular-stable plate fixation in displaced proximal humeral fractures. Injury 2008;39:306–313.
Helfet DL, Hotchkiss RN. Internal fixation of the distal humerus: a biomechanical comparison of methods. J Orthop Trauma 1990;4:224–260.
Helfet DL, Schmeling GJ. Bicondylar intraarticular fracture of the distal humerus in adults. Clin Orthop Relat Res 1993;292:26–36.
Jacobson SR, Glisson RR, Urbaniak JR. Comparison of distal humerus fracture fixation: a biomechanical study. J South Orthop Assoc. 1997;6(4):241–249 (Winter).
Jiang R, Luo CF, Wang MC, Yang TY, Zeng BF: A comparative study of Less Invasive Stabilization System (LISS) fixation and two-incision double plating for the treatment of bicondylar tibial plateau fractures. Knee 2008;15:139–143.
Korner J, Diederichs G, Arzdorf M et al. A biomechanical evaluation of methods of distal humerus fracture fixation using locking compression plates versus conventional reconstruction plates. J Orthop Trauma. 2004;18(5):286–93.
Koshimune M, Kamano M, Takamatsu K, Ohashi H: A randomized comparison of locking and non-locking palmar plating for unstable Colles’ fractures in the elderly. J Hand Surg [Br] 2005;30:499–503.
Sanchez-Sotelo J, Torchia ME, O’Driscoll SW. Complex distal humerus fractures:internal fixation with a principle-based parallel-plating technique. Surgical technique. J Bone Joint Surg Am. 2008;90 Suppl 2 Pt 1:31–46.
Sanchez-Sotelo J, Torchia ME, O’Driscoll SW. Complex distal humerus fractures:internal fixation with a principle-based parallel-plating technique. J Bone Joint Surg Am. 2007;89:961–969.
Schemitsch EH, Tencer AF, Henley MB. Biomechanical evaluation of methods of internal fixation of the distal humerus. J Orthop Trauma 1994;8:468–475.
Schuster I, Korner J, Arzdorf M, Schwieger K, Diederichs G, Linke B. Mechanical comparison in cadaver specimens of three different 90-degree double-plate osteosyntheses for simulated C2-type distal humerus fractures with varying bone densities. J Orthop Trauma. 2008;22(2):113–20.
Wong AS, Baratz ME.Elbow fractures: distal humerus. J Hand Surg [Am]. 2009;34(1):176–90.
Acknowledgment
The authors thank Yanna Song for statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
One or more of the authors (WTO) has received funding from The Southeast Fracture Consortium.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
Level of Evidence: Level III, therapeutic study. See the guidelines for authors for a complete description of levels of evidence.
Rights and permissions
About this article
Cite this article
Berkes, M., Garrigues, G., Solic, J. et al. Locking and Non-locking Constructs Achieve Similar Radiographic and Clinical Outcomes for Internal Fixation of Intra-articular Distal Humerus Fractures. HSS Jrnl 7, 244–250 (2011). https://doi.org/10.1007/s11420-011-9219-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-011-9219-y