Abstract
Non-cemented femoral fixation in hip arthroplasty has become the standard of practice in the USA. However, recent literature has brought attention to an increasing incidence of periprosthetic femur fractures with certain stem designs. This study examines reasons for early periprosthetic femur fractures in patients with a hip arthroplasty performed using a non-cemented tapered wedge stem design. A multivariate analysis using a matched-cohort design was performed to assess any potential risk factors that may predispose to such fractures. Six of 2,220 hips (0.3%) suffered a periprosthetic femur fracture within the first year after surgery; five of six were Vancouver Type B2. The average time to fracture was 9 weeks. This group of patients had a significantly higher canal–flare index and lower canal–calcar ratio. This complication may be preventable by having a better appreciation of the fit between the implant and the bone during pre-operative planning, with the goal of avoiding a proximal–distal mismatch.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periprosthetic fractures are among the major complications of hip arthroplasty. Treatment of these fractures can be technically demanding, with a high incidence of complications and reoperations [14]. These fractures have been shown in numerous studies to occur more frequently using non-cemented femoral fixation [1], and recent reports have suggested the incidence of periprosthetic femoral fractures may be increasing [2, 11, 14].
Non-cemented tapered wedge femoral stems are a particular type of non-cemented stem being used with increasing frequency in modern hip arthroplasty, and they have largely replaced the use of cemented stems in primary hip arthroplasty in the USA. These stems have demonstrated excellent long-term clinical results, with numerous authors reporting survivorship ranging from 98% to 100% at 10-year follow-up [3, 10–12, 15–17]. However, this particular type of stem design may have an increased rate of periprosthetic fracture due to the hand-broached preparation technique necessary to achieve a tight press-fit for immediate component stability, or due to the wedge-shaped design of the implant. This is of concern given the accelerated post-operative rehabilitation protocols associated with contemporary North American arthroplasty practice, which has been suggested as one of the reasons for the increasing prevalence of periprosthetic fractures [2].
As the number of primary arthroplasties continues to increase, and as this stem design is used with increasing frequency, it is likely the burden of these fractures will increase. Identification of risk factors for fracture in patients with this stem design will improve the ability for pre-operative planning and aid in primary prevention. Accordingly, the aims of this study are: (1) to report the incidence of early periprosthetic femur fractures in patients using this stem design at our institution and (2) to identify any factors such as proximal femoral geometry that may increase this risk.
Materials and methods
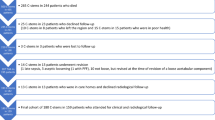
This study was designed as a retrospective consecutive cohort study, using a matched case–control population for data analysis. The study group included all patients at our institution who were implanted with a single femoral stem design over a 5-year period from January 2003 through December 2007. A total of 2,220 hips were identified from a computerized database of all arthroplasties performed using this type of stem. All pre-operative diagnoses were included in the study. The only exclusion criterion for entry into the study was a noted intra-operative periprosthetic fracture. Approval was obtained from our hospital’s Institutional Review Board prior to the study’s inception.
All patients were implanted with a single femoral implant design (Accolade® TMZF® stem; Stryker Orthopaedics, Mahwah, NJ, USA). Because this study encompasses a group of 24 surgeons, the operative approaches, operative techniques, and perioperative protocols were not standardized. However, in all cases femoral fixation was obtained using a hand-broached non-cemented press-fit technique. The post-operative therapy protocol at our institution encourages all patients to ambulate and bear weight as tolerated starting on the first post-operative day.
Fractures were identified from a retrospective review of the medical records of the operating surgeons. The cohort of early periprosthetic fractures was defined by any fracture that occurred between when the patient had left the operating room and 1 year post-operatively. Intra-operative fractures were excluded, as these have been studied extensively elsewhere in the literature and are outside the scope of this study. The Vancouver classification [8] was retrospectively used to classify the fractures on conventional anteroposterior and lateral radiographs; this classification system is widely used, and has been shown to be reproducible and reliable [4]. There was complete agreement between both authors on the fracture classification for all patients.
A second cohort of patients with the same implant that was matched for age, sex, and pre-operative diagnosis and did not have a periprosthetic fracture was randomly selected from the study population. A three-to-one matching ratio, a method commonly employed in this type of retrospective study to increase statistical validity, [6] was used to perform the statistical analysis of clinical and radiographic variables.
A radiographic analysis of the proximal femoral geometry was then performed to assess for any radiographic risk factors that might predispose to a failure of osteointegration. Proximal femoral geometry was analyzed on the immediate pre-operative radiograph in all hips using previously described radiographic parameters, including the morphological cortical index (MCI) [20], the canal–bone ratio (CBR) [21], the canal–calcar ratio (CCR) [7], and the canal–flare index (CFI) [18] (Fig. 1). A detailed discussion of the utility and meaning of each of these indices is given in the original sources; but briefly, these are each simple ratios that can be easily calculated from measurements made on an anteroposterior radiograph of the hip that allow a quantitative analysis of the proximal femoral geometry and can be a surrogate indicator of bone quality. All measurements were performed digitally using the ruler function on the Picture Archiving and Communication System at our institution (Synapse; Fujifilm Medical Systems, Stamford, CT, USA). These parameters were compared between the control group and the study group.
Statistical analyses were performed using an independent student’s t test with a significance level set at p < 0.05. Ninety-five percent confidence intervals (95% CI) were calculated for all measurements.
Results
Six fractures occurring within the first post-operative year were identified in 2,220 stems implanted over the 5-year study period, for an incidence of 0.3% (Table 1). Four occurred in patients that were treated with an elective primary total hip arthroplasty (THA), while the other two occurred following hemiarthroplasty for a femoral neck fracture. Five fractures were Vancouver Type B2, and the other was Vancouver Type A(G). The mean time to fracture was 9 weeks post-operatively (2 days to 44 weeks). All fractures occurred from low-energy mechanisms. Four occurred during a fall from standing height, one occurred from a fall out of bed, and one occurred while ambulating without a history of trauma. The single Type A fracture was managed successfully with non-operative treatment. All five of the Type B2 fractures were treated with revision of the femoral component to a modular non-cemented component designed to achieve fixation distal to the fracture site. During the revision surgery, one patient from this group sustained an intra-operative periprosthetic fracture at the distal aspect of the revision stem that was initially treated with cerclage wiring. This fixation failed within the first post-operative week and the patient was brought back to the operating room where an open reduction and internal fixation was performed with a submuscular plate.
When compared to the matched cohort, the patients in the fracture group were found to have a predictable difference in bone morphology (Table 2). Although there was no statistical significance with regard to morphological cortical index or canal–bone ratio, the fracture cohort did have a statistically lower canal–calcar ratio (p = 0.042) and statistically higher canal–flare index (p = 0.039).
Discussion
Periprosthetic fractures in hip arthroplasty are frequently discussed; however, most reports examine heterogeneous groups of implant designs. As a result, periprosthetic fractures around a non-cemented tapered wedge stem have not been looked at in isolation. Furthermore, despite numerous studies regarding intra-operative periprosthetic fractures, there has been little focus on early post-operative periprosthetic femur fractures. Based on our results, there appears to be an association between early post-operative periprosthetic fractures in certain femoral geometries and fixation using a non-cemented tapered wedge femoral stem. While relatively uncommon, these fractures warrant attention as it is a potentially serious complication that is often difficult to manage. As stems of this design are increasingly used and as the annual number of hip arthroplasties performed continues to increase, this entity may receive increasing clinical attention.
There are several limitations to our study. We are unable to determine if this entity is a problem in other proximally coated tapered stem designs, as all the patients in this study were implanted with one implant design specific to a single manufacturer. Other tapered wedge stem designs with different taper geometries may avoid this problem [9]. Further limitations of this study include the retrospective nature of our study design and its inherent problems. Our analysis likely underestimates the incidence of early periprosthetic fracture around this type of implant as some patients may have been treated at other institutions. In addition, we were unable to perform a complete demographic analysis due to the limited nature of our database, and were unable to analyze potentially important risk factors such as activity level and body mass index, among others.
Our incidence of post-operative periprosthetic femur fractures of 0.3% compares favorably with that reported by other authors. Previous studies have reported a cumulative incidence of periprosthetic fracture following primary total hip arthroplasty of 0.4% to 0.6% [13, 14]. A more recent study reported an incidence of 0.4% in the first 90 days [2]; that research found that the incidence of early fractures increased from 0.15% between 1987 and 2003 to 0.81% from 2004 to 2007. Their hypothesized risk factors were early weight bearing associated with more aggressive rehabilitation protocols, which may lead to an acute torsional force or axial load across the bone–implant interface before osteointegration. They concluded that protected weight bearing in the first few weeks may promote the best long-term result by avoidance of complications.
Although previous studies have identified numerous risk factors for periprosthetic femur fractures including age, sex, operative approach, and implant design, [1, 5, 14] none to our knowledge have investigated radiographic parameters of the host bone. Our study design attempted to control for such demographic risk factors to allow a focus on simple radiographic parameters that are able to be calculated during pre-operative templating. Our data clearly indicate that a specific proximal femoral morphology may predispose to this problem. The CCR and CFI were originally reported to guide the choice of cementless versus cemented femoral component fixation in THA [7, 18], but have also been linked to bone quality in the proximal femur [7, 19, 21]. In the present study, patients with a lower canal–calcar ratio and a higher canal–flare index were significantly more likely to sustain a periprosthetic femur fracture than those from a randomly selected matched cohort (Fig. 2). The CFI and CCR both attempt to measure similar morphological ratios (although inverses of each other) which are particularly relevant when utilizing a proximally coated tapered wedge femoral component: namely the ratio between the inner diameter of the proximal bone where the implant is designed to achieve fixation and bony ingrowth and the inner diameter of the diaphyseal bone where the uncoated distal portion of the component is intended to centralize the stem within the canal and to provide secondary stability. This emphasizes the importance of preoperatively assessing the patient’s proximal femoral geometry when choosing the method of fixation. Careful attention should be paid to avoid selecting a stem that will cause a proximal–distal mismatch, which may put the patient at an increased risk of this complication. A patient with such morphology of the proximal femur may benefit from selecting a different stem either without a tapered wedge or with a more narrow distal section that does not contact the inner cortex of the diaphysis. As two of the fractures in this series occurred in patients undergoing hemiarthroplasty for femoral neck fracture, consideration should also be given to using cemented fixation in this population in patients with this type of proximal femoral morphology.
Pre-operative radiographs from a patient in the fracture cohort (a) and a patient in the control cohort (b) demonstrating differences in proximal femoral morphology. Patients in the fracture cohort had a significantly lower canal–calcar ratio and a significantly higher canal–flare index than those in the control cohort
Although the mechanism for this type of early periprosthetic fracture cannot be elucidated from this study, it may arise from an abnormal stress distribution from the interaction between the tapered wedge stem and a tight canal. When loaded in an atypical manner, a fracture may propagate from these abnormal stress risers. Alternatively, it is possible that an intra-operative periprosthetic fracture went unrecognized and simply propagated with progressive weight bearing during the post-operative period. Additionally, the relatively high proportion of periprosthetic fractures in patients who had originally undergone arthroplasty for a displaced femoral neck fracture underscores the important role the host bone quality may have as a risk factor for such fractures. Often confounding the problem, pre-operative templating is often difficult in these patients given the difficulty in obtaining adequate pre-operative radiographs.
References
Berend ME, Smith A, Meading JB, Ritter MA, Lynch T, Davis K. Long term outcome and risk factors of proximal femoral fracture in uncemented and cemented total hip arthroplasty in 2551 hips. J Arthroplasty 2006; 21: 53-59
Berry DJ, Dorr LD, Long WT, Dastane M, Taunton MJ. Early femur fracture after THA: Increased prevalence associated with modern N. American practice. 75th Annual Meeting of the American Academy of Orthopaedic Surgeons. March 2008, San Francisco, CA
Bourne RB, Rorabeck CH, Patterson JJ, Guerin J. Tapered titanium cementless total hip replacements: a 10- to 13-year followup study. Clin Orthop Relat Res 2001; 393: 112-120
Brady OH, Garbuz DS, Masri BA, Duncan CP. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty. 2000; 15: 59–62
Cook RE, Jenkins PJ, Walmsley PJ, Patton JT, Robinson CM. Risk factors for periprosthetic fractures of the hip. Clin Orthop 2008; 466: 1652-1656
Davis ET, McKee MD, Waddell JP, Hupel T, Schemitsch EH. Total Hip Arthroplasty Following Failure of Free Vascularized Fibular Graft, J Bone Joint Surg Am 2006; 88: 110-115
Dorr LD. Total hip replacement using APR system. Tech Orthop 1986; 1: 22-34
Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect 1995; 44: 293–304
Fernandez-Fernandez R, García-Elias E, Gil-Garay E. Peroperative fractures in uncemented total hip arthrography: results with a single design of stem implant. Int Orthop 2008; 32: 307-313
Froimson MI, Garino J, Machenaud A, Vidalain JP. Minimum 10-year results of a tapered, titanium, hydroxyapatite-coated hip stem: an independent review. J Arthroplasty 2007; 22: 1-7
Haddad FS, Masri BA, Garbuz DS, Duncan CP. The prevention of periprosthetic fractures in total hip and knee arthroplasty. Orthop Clin North Am 1999; 30: 191-207
Lachiewicz PF, Soileau ES, Bryant P. Second-generation proximally coated titanium femoral component: minimum 7-year results. Clin Orthop Relat Res 2007; 465: 117-121
Lewallen DG, Berry DJ. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instructional Course Lectures 1998; 47:243
Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty 2005; 20: 857-865
Marshall AD, Mokris JG, Reitman RD, Dandar A, Mauerhan DR. Cementless titanium tapered-wedge femoral stem: 10- to 15-year follow-up. J Arthroplasty 2004; 19: 546-552
McLaughlin JR, Lee KR. Total hip arthroplasty in young patients. 8- to 13-year results using an uncemented stem. Clin Orthop Relat Res 2000; 373: 153-163
Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME. Minimum ten-year follow-up of a straight-stemmed, plasma-sprayed, titanium-alloy, uncemented femoral component in primary total hip arthroplasty. J Bone Joint Surg Am 2004; 86: 92-97
Noble PC, Alexander JW, Lindahl LJ, Yew JT, Granberry WM, Tullos HS. The anatomic basis of femoral component design. Clin Orthop Relat Res 1988; 235: 148-165
Noble PC, Box GG, Kamaric E, Fink MJ, Alexander JW, Tullos HS. The effect of aging on the shape of the proximal femur. Clin Orthop Relat Res 1995; 316: 31-44
Spotorno L, Romagnoli S. Indications for the CLS stem. In: Spotorno L, Romagnoli S, eds. The CLS uncemented total hip replacement system. Berne, Switzerland: Protek; 1991
Yeung Y, Chiu KY, Yau WP, Tang WM, Cheung WY, Ng TP. Assessment of the proximal femoral morphology using plain radiograph-can it predict the bone quality? J Arthroplasty 2006; 21:508-513
Author information
Authors and Affiliations
Corresponding author
Additional information
No financial support was received in this study. Each author certifies that he has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Prior to the commencement of this study, approval for this study was obtained from the Institutional Review Board of our institution. Research was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. Each author certifies that his or her institution has approved the reporting of these cases and that all investigations were conducted in conformity with ethical principles of research.
Level of evidence: Level III: Prognostic Study.
Rights and permissions
About this article
Cite this article
Cooper, H.J., Rodriguez, J.A. Early Post-operative Periprosthetic Femur Fracture in the Presence of a Non-cemented Tapered Wedge Femoral Stem. HSS Jrnl 6, 150–154 (2010). https://doi.org/10.1007/s11420-010-9161-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-010-9161-4