Abstract
Hyperuricemia is an independent risk factor for chronic kidney disease. We have previously showed the uric-acid-lowering effect of Eurycoma longifolia Jack, yet the renal protective effect and mechanism of E. longifolia remain obscure. The mouse model of hyperuricemic nephropathy was induced by adenine combined with potassium oxonate in male C57BL/6 J mice. E. Longifolia alkaloid components could reduce the level of serum uric acid by regulating the expression of hepatic phosphoribosyl pyrophosphate synthase (PRPS), hypoxanthine-guanine phosphoribosyl transferase (HPRT), and renal urate transporter organic anion transporter 1 (OAT1) and ATP-binding box subfamily G member 2 (ABCG2) in HN mice. Additionally, E. Longifolia alkaloid components alleviated renal injury and function caused by hyperuricemia, which was characterized by improving renal histopathology, reducing urea nitrogen and creatinine levels. E. Longifolia alkaloid components treatment could reduce the secretion of pro-inflammatory factors by inhibiting the activation of NF-κB and NLRP3 inflammatory signaling pathways, including tumor necrosis factor α (TNF-α), monocyte chemoattractant protein-1 (MCP-1), interleukin-1 β (IL-1β), and regulated activated normal T cell expression and secretion proteins (RANTES). Meanwhile, E. longifolia alkaloid components improved renal fibrosis, inhibited the transformation of calcium-dependent cell adhesion molecule E (E-cadherin) to α-smooth muscle actin (α-SMA) transformation, and decreased collagen 1 expression in HN mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hyperuricemia (HUA) is an independent risk factor for chronic kidney disease (CKD) [1]. The risk of kidney disease in people with serum uric acid levels higher than 9 mg/dl is three times higher than that normal uric acid levels [2]. Patients with long-term HUA have a greater risk of CKD, which means that HUA may accelerate the progression of CKD [1]. In the population with estimated glomerular filtration rate (eGFR) ≥ 90 mL/min/1.73m2, the prevalence of HUA is 11–13%, but the prevalence of HUA is about 6–7 times higher in people with eGFR between 15 and 29 mL/min/1.73m2 [3].
Long-term HUA can cause excessive accumulation of uric acid in the kidneys, resulting in hyperuricemic nephropathy (HN). HUA was once thought to be monosodium urate (MSU) deposited in the collecting duct of the kidney, causing kidney disease in a manner similar to gouty arthropathy [4]. Recently, new mechanisms of HN have been reported, including endothelial dysfunction, activation of the renal angiotensin system, oxidative stress, and renal tubular epithelial interstitialization [5, 6]. In addition, uric acid can also induce vascular endothelial injury and inflammation by activating transcription factors (such as NF-κB) and the NLRP3 inflammasome signaling pathway, causing kidney damage [7]. Whether it is in the form of MSU or soluble urate, the mechanism of kidney damage caused by uric acid is related to the participation of inflammatory reactions [8, 9].
At present, the safety and efficacy of uric-acid-lowering drugs for the treatment of HN have yet to be verified. Allopurinol and benzbromarone are the first-line uric-acid-lowering drugs in clinical practice. Allopurinol may cause severe hypersensitivity, agranulocytosis, and aggravate nephrotoxicity by impairing pyrimidine metabolism [10]. In patients with kidney injury, although benzbromarone can effectively reduce the blood uric acid concentration, it cannot improve the renal function damage and can cause severe liver damage [11]. Therefore, it is necessary to find new compounds that has no toxic side effects and can treat HUA complicated with renal damage.
Eurycoma longifolia Jack (E. longifolia) is a widely popular herbal medicine in Southeast Asia. E. longifolia is a traditional medicine used to treat sexual dysfunctions and intermittent fever (malaria) [12]. E. longifolia is rich in various biologically active compounds, such as quassinoids, alkaloids, squalene derivatives, benzene lignans, hydantoins, and bioactive steroids [13]. E. longifolia have shown a wide dynamic range of pharmacological activities including aphrodisiac [14], antimalarial [15], anti-inflammatory [16], antidiabetic [17], anti-hyperuricemia [18], and anticancer [19]. We have recently showed the uric-acid-lowering effect of E. longifolia [18], yet the renal protective effect and mechanism of E. longifolia on hyperuricemic mice remains obscure. To further study the anti-HN effects and mechanisms of E. longifolia alkaloid components, this study combined with in vivo and in vitro models to evaluate the effects of alkaloids from E. longifolia in reducing uric acid and improving HN kidney damage, and explore its potential mechanisms.
Materials and methods
Materials
The stems of E. longifolia were collected from Thailand. The stems of E. longifolia were identified by Dr. Wang Tao from Institute of Traditional Chinese Medicine, Tianjin University of Traditional Chinese Medicine (TJUTCM). Voucher specimen was deposited at the Institute of Traditional Chinese Medicine of TJUTCM (Voucher Number: TJUTCM-18-0155).
E. longifolia alkaloid components are provided by Tianjin Key Laboratory of Chemistry and Analysis of Traditional Chinese Medicine, the contents of the target analytes in E. longifolia alkaloid components were 28.96 and 44.34 μg/g for canthin-6-one, and 9-methoxycanthin-6-one, respectively [20]. The compounds, Compound 1 (PubChem CID: 5,320,161), Compound 2 (PubChem CID: 10,446,368), Compound 3 (PubChem CID: 102,004,796), Compound 4(PubChem CID:259,218), Compound 5 (PubChem CID: 97,176), and Compound 6 (PubChem CID: 9,881,423) were purchased from Yuanye Biotechnology Co., Ltd. Shanghai, China. Their purity was HPLC ≥ 95%.
Animals
This study was performed on mice of SPF-grade C57BL/6 J (8–10 weeks old, male). All the mice were purchased from Beijing Vital River Laboratory Animal Technology Co., Ltd. All mice were fed on a standard diet, with an indoor temperature of 22 °C ± 2 °C and a fixed artificial light time of 12 h. Before the formal experiment, the mice were adaptively fed for at least 7 days. The animal experiment of this study was approved by Science and Technological Committee and the Animal Use and Care Committee of TJUTCM (No. 202010006, 6 October 2020).
This study randomly divided mice into five groups: normal group (Sham), model group (HN), positive drug group (Ben-50), E. longifolia alkaloid components medium-dose group (T-200), and E. longifolia alkaloid components high-dose group (T-200), with 10 mice in each group.
Adenine- and potassium-oxonate-induced HN mice
HN mice model was established by oral administration of potassium oxonate and adenine (Sigma-Aldrich Co., MO, USA). Benzbromarone and E. longifolia alkaloid components were suspended in normal saline and orally administrated, with an interval of 1 h, the mice had intragastric administration of adenine (75 mg/kg/day) and potassium oxonate (200 mg/kg/day). The normal and HN groups were only administered orally the same volume of normal saline. The experiment lasted 21 days. The mice were anesthetized with isoflurane. The mice were then euthanized with carbon dioxide. The carbon dioxide filling rate is 10%–30% of the chamber volume.
Ultra-performance liquid chromatography (UPLC) was used to determine serum uric acid levels in mice [18]. The clearance of uric acid (Cur) and creatinine (Ccr) was then calculated [21].
Histopathology of renal tissues
Kidney tissue was fixed with 10% formalin and embedded in paraffin. The sections were stained with hematoxylin and eosin (H&E), periodic acid–Schiff (PAS) or Masson’s trichrome (MASSON). The stained sections were observed with an optical microscope with a magnification of × 400. The histopathological changes were evaluated by epithelial cell necrosis and renal tubule dilatation. The positive staining area of renal interstitial fibrosis was quantitatively measured by Image J program (National Institutes of Health, Bethesda, Maryland, USA).
Immunohistochemistry
The kidney embedded wax block was cut into 4 μm slices. After deparaffinization, they were treated with citrate buffer and then treated with 0.3% H2O2. 3% BSA was used to block non-specific proteins. After blocking, each slide was incubated with CD68 primary antibody (Abcam plc. Cambridge, MA, USA) at 4 °C overnight. The next day, the tissue section was incubated with the secondary antibody. Images were observed and captured with an Axio Imager 2 (Zeiss, Oberkochen, Germany).
Western blot and qRT-PCR analysis
The methods for western blotting and qRT-PCR were consistent with our previous studies [22]. Anti-ABCG2, anti-OAT1, anti-PRPS, anti-IκBα, anti-phosphor-IκBα, anti-NLRP3, anti-Caspase 1, anti-NF- κB, anti-phosphor-NF-κB, anti-Collagen 1, anti-E-cadhrein, anti-α-SMA and β-actin antibodies are purchased from Abcam plc. Cambridge, MA, USA. Other antibodies used in this study included: anti-URAT1 (ProteinTech Group. Chicago, USA) and anti-GLUT9 (Millipore Co. Ltd. Bedford, MA, USA). qRT-PCR was performed by the SYBR Green QuantiTect RT-PCR Kit (Thermo Fisher Sci. Inc., St. Austin, TX, USA). The results were detected using the 2−△△CT method. The PCR primer sequences were shown in Table 1.
Cell culture and processing
Screening of active compounds to inhibit the absorption of urate
To establish HEK293T cells with URAT1 gene overexpression, the cDNA of URAT1 was subcloned into A pHB-CMV-MCS-EF1-ZSgreen-puro (Hanheng Biotechnology Co., Ltd. Shanghai, China). HEK293T cells were then transfected using Lipofiter™. After 24 h, the transfection solution was removed and the successfully transfected cells were screened.hURAT1-HEK293T cells (HEK293T cells with URAT1 overexpression) were cultured in DMEM containing 10% fetal bovine serum and 1% diabody, and placed in a constant temperature incubator with a CO2 concentration of 5% (temperature was set at 37 °C). The compound was administered at a concentration of 5 μmol/L. The concentration of uric acid model was 100 μmol/L. When the cells grew logarithmically, they were seeded in 6-well plates. After washing with chlorine-free HBSS buffer, HBSS buffer was added for incubation. After removing the HBSS buffer, the HBSS solution containing 100 μmol/L urate and the corresponding concentration of alkaloid monomer was incubated for 30 min. RDEA3170 acted as a urate-anion transporter 1 (URAT1) inhibitor. 0.1 mmol/L NaOH was added to each well to lyse the cells, and then the uric acid content of the sample was measured.
Compounds inhibit hyperuric-acid-induced inflammatory response in renal tubular epithelial cells
NRK-52E cells (Hanheng Biotechnology Co., Ltd, Shanghai, China) were cultured in DMEM medium containing 10% fetal bovine serum concentration and 1% diabody concentration, and placed in a constant temperature incubator with a CO2 concentration of 5% (temperature was set to 37 °C). The final concentration was 15 mg/dL uric acid for 48 h to build the model. Select the logarithmic growth phase cells, inoculate them in a 6-well plate, when the cells were 70–80% of the bottom plate, starve for 11 h, and 5 μmol/L alkaloid monomer compound and inhibitor were pre-administered for 1 h. Uric acid solution was added to each well and cultured for 24 h. 5 μmol/L alkaloid monomer compound and inhibitor was added to each well to incubate for 24 h. The experiment was ended and subsequent experimental tests were carried out.
Enzyme-linked immunosorbent assay (ELISA)
For the determination of the expression levels of IL-1β, TNF-α, MCP-1 and RANTES in mouse kidneys, mouse kidneys were fully homogenized in 9 volumes of pre-chilled Tris–HCl buffer (50 mM, pH 7.4) containing 10 μg/mL indomethacin. Centrifuge at 5000 rpm for 10 min to remove insoluble proteins. All steps are carried out at 4 °C. Add antigen diluted to appropriate concentration with coating diluent in each well, 37 ℃ for 4 h. 5% calf serum was added into each well and sealed at 37 ℃ for 40 min. After washing for 3 times, add the sample to be tested. The well was washed three times after reacting at 37 ℃ for 40 min. Each well was added enzyme labeled antibody for 1 h, then added substrate solution away from light at 37 ℃ for 3–5 min. At last, each well was added termination solution, and the absorbance of the solution in each well was detected at 450 nm wavelength by a microplate reader (MuATiskanMK3, Thermo Fisher Sci. Inc., St. Austin, TX, USA).
Data analysis of network pharmacology
Use Pharmmapper online tool for compound target enrichment analysis, and then use Cytoscape software for network construction, analysis, and beautification.
Statistical analysis
The result data are shown as the mean ± S.E.M. The SPSS 20.0 statistical software was used for data analysis (version 20, SPSS; IBM, Armonk, NY, USA). The significant differences between the data were evaluated by one-way ANOVA, LSD and Dunnett's (Tukey) test were used for post hoc evaluations. P < 0.05 was considered statistically significant.
Results
The alkaloid component of E. longifolia could significantly reduce the level of serum uric acid, improve the renal dysfunction and renal histopathological damage caused by high uric acid in HN mice.
The alkaloid component of E. longifolia lowered uricemia and attenuated renal injury in HN mice
At the end of the study, the HN mice showed higher kidney coefficients and lower body weight levels (Fig. 1a–c), as well as significantly increased levels of uric acid (Fig. 1d), and serum creatinine (Fig. 1e), blood urea nitrogen (BUN) (Fig. 1f), and reduced uric acid clearance (Fig. 1g) in comparison to those of control. The alkaloid component of E. longifolia reduced uricemia and restored renal function parameters in a dose-dependent manner (Fig. 1c–f). Histopathological results further confirmed this point, among which E. longifolia alkaloid components improved the pathological changes of HN mice kidney.
Effects of E. longifolia alkaloid components on plasma uric acid, creatinine, urea nitrogen and kidney injury in HN mice. A Body weight; B body weight increase; C kidney coefficient; D serum uric acid; E serum creatinine; F blood urea nitrogen, G uric acid clearance; H representative photomicrographs (× 400) of H&E and PAS staining in mice kidneys. Sham: blank control group; HN hyperuricemia nephropathy group, Ben-50: benzbromarone 50 mg/kg; T-200 E. longifolia alkaloid components, low-dose group 200 mg/kg; T-400 E. longifolia alkaloid components, high-dose group 400 mg/kg. Data are expressed as mean ± SEM (n = 10). Compared with Sham group, ###P < 0.001; compared with HN group, *P < 0.05, **P < 0.01, ***P < 0.001
The alkaloid component of E. longifolia reduced the synthesis of uric acid and promoted the excretion of uric acid in HN mice
Hyperuricemia is related to increased uric acid production and decreased excretion. The positive control group of benzbromarone is known to promote uric acid excretion, which is consistent with our results, that is, the level of uric acidemia in the mice fed with benzbromarone is even lower than that of the control group (Fig. 1d). E. longifolia alkaloid components reduced uric acidemia to near normal levels. The liver is the main site for uric acid synthesis, phosphoribosyl pyrophosphate synthetase (PRPS) and hypoxanthine-guanine phosphoribosyl transferase (HPRT) are the rate-limiting enzymes for uric acid synthesis. We found through western blot analysis that the alkaloid component of E. longifolia significantly reduced the expression of PRPS and HPRT in the liver of HN mice (Fig. 2a–c). Uric acid transporter in the kidney mediates renal uric acid excretion. We found through western blot analysis that E. longifolia alkaloid components significantly restored the abnormal expression of organic anion transporter 1 (OAT1) and ATP-binding box subfamily G member 2 (ABCG2) in the kidney of HN mice (Fig. 2d–f). Therefore, it can be concluded that the regulation of uric acid transporter and key enzymes for uric acid synthesis may be part of the mechanism of reducing uric acid by the alkaloid component of E. longifolia.
Effects of E. longifolia alkaloid components on uric acid synthesis and transport in HN mice. A E. longifolia alkaloid components reduced the expression of PRPS, and increased the expression level of HPRT; B, C the ratio of PRPS and HPRT to β-actin was calculated; D E. longifolia alkaloid components increased the expression level of ABCG2 and OAT1; E the ratio of ABCG2 and OAT1 to β-actin was calculated. Sham: blank control group; HN: hyperuricemia nephropathy group; Ben-50: benzbromarone 50 mg/kg; T-200: E. longifolia alkaloid components, low-dose group 200 mg/kg; T-400: E. longifolia alkaloid components, high-dose group 400 mg/kg. Data are shown as mean ± SEM (n = 10). Compared with Sham group, #P < 0.05, ##P < 0.01, ###P < 0.001; compared with HN group, **P < 0.01, ***P < 0.001
The alkaloid component of E. longifolia improved renal tubulointerstitial fibrosis via relieving inflammatory reaction in HN mice
The alkaloid component of E. longifolia reduced pro-inflammatory production in the kidneys of HN mice
Excessive pro-inflammatory production plays a crucial role in the development of HUA-related kidney injury. Higher concentrations of tumor necrosis factor α (TNF-α), interleukin-1 β (IL-1β), monocyte chemoattractant protein-1 (MCP-1), and regulated activated normal T cell expression and secretion proteins (RANTES) were detected in the kidneys of HN mice compared to the control group (Fig. 3). Specifically, E. longifolia alkaloid components significantly reduced mRNA levels and protein levels of these pro-inflammatory mediators (Fig. 3), validating that E. longifolia alkaloid components attenuated inflammation in the kidneys of HN mice.
Effects of E. longifolia alkaloid components on pro-inflammatory production in HN mice. A–D The mRNA expression levels of IL-1β, MCP-1, RANTES, and TNF-α were determined; E–F the concentration of IL-1β, MCP-1, RANTES, and TNF-α in HN mice kidney was detected by ELISA. Sham: blank control group; HN: hyperuricemia nephropathy group; Ben-50: benzbromarone 50 mg/kg; T-200: E. longifolia alkaloid components, low-dose group 200 mg/kg; T-400: E. longifolia alkaloid components, high-dose group 400 mg/kg. Data are shown as mean ± SEM (n = 10). Compared with Sham group, ## P < 0.01, ### P < 0.001; compared with HN group, *P < 0.05, **P < 0.01, ***P < 0.001
The alkaloid component of E. longifolia inhibited the activation of NF-κB and NLRP3 inflammasome signaling pathway in the kidney of HN mice
Previous studies have shown that inflammation is closely related to HN, and NF-κB is expressed as an important inflammatory mediator in the context. The activation of NF-κB is the core step of NF-κB signal transduction. Through western blotting, we found that the increased phosphorylation of NF-κB and NF-κB inhibitory protein (IκBα) in the kidneys of HN mice was repressed by E. longifolia alkaloid components treatment (Fig. 4a–c). It has been confirmed that the activation of the NLRP3 inflammasome signaling pathway is a key driving factor for renal fibrosis. Therefore, the expression of NLRP3 and Caspase 1 in the kidney of HN mice was detected by immunoblotting. In Fig. 4F–H, increased expression of NLRP3 and Caspase 1 was detected in the kidney of HN mice, which was inhibited by E. longifolia alkaloid components treatment. Similarly, benzbromarone failed to inhibit the expression of NLRP3 and Caspase 1.
Effects of E. longifolia alkaloid components on NF-κB and NLRP3 inflammasome signaling pathway in HN mice. A The protein expression levels of p-NK-κB, NK-κB, and p-IκBα were determined. B–D The ratio of p-NK-κB, NK-κB, and p-IκBα to β-actin was calculated. E The protein expression levels of NLRP3 and Caspase 1 were determined. F–G The ratio of NLRP3 and Caspase 1 to β-actin was calculated. Sham: blank control group; HN: hyperuricemia nephropathy group; Ben-50: benzbromarone 50 mg/kg; T-200: E. longifolia alkaloid components, low-dose group 200 mg/kg; T-400: E. longifolia alkaloid components, high-dose group 400 mg/kg. Data are shown as mean ± SEM (n = 10). Compared with Sham group, ##P < 0.01, ###P < 0.001; compared with HN group, *P < 0.05, **P < 0.01, ***P < 0.001.
The alkaloid component of E. longifolia improved renal tubulointerstitial fibrosis in HN mice
Tubular interstitial fibrosis has been confirmed in the pathogenesis of HN and is characterized by abnormal or excessive extracellular matrix (ECM) deposition. According to Fig. 5a, b, HN mice showed increased Masson tricolor positive areas in the damaged renal tubular interstitial compartment, while E. longifolia alkaloid components improved the morphological lesions of fibrosis. Moreover, the positive cells of HN mice increased significantly, suggesting a large number of macrophage infiltration in the kidney of HN mice, the positive expression of E. longifolia alkaloid components groups decreased significantly, and the macrophage infiltration was significantly improved (Fig. 5c, d).
Effects of E. longifolia alkaloid components on renal tubulointerstitial fibrosis in HN mice. A The photomicrograph of mice kidneys stained with MASSON (× 400). B Fibrotic score. C Representative photomicrographs (× 400) of CD68 immunohistochemistry of mice kidneys. D Score of kidneys in CD68 immunohistochemistry. E The protein expression levels of E-cadherin, Collagen 1, and α-SMA were determined by western blot. F–H The ratio of E-cadherin, Collagen 1, and α-SMA to β-actin was calculated. Sham: blank control group; HN: hyperuricemia nephropathy group; Ben-50: benzbromarone 50 mg/kg; T-200: E. longifolia alkaloid components, low-dose group 200 mg/kg; T-400: E. longifolia alkaloid components, high-dose group 400 mg/kg. The data are shown as mean ± S.E.M (n = 10). Compared with Sham group, #P < 0.05, ##P < 0.01, ###P < 0.001; compared with HN group, *P < 0.05, **P < 0.01, ***P < 0.001
In addition, the expression of two key interstitial matrix components, Collagen 1 was significantly increased and calcium-dependent cell adhesion molecule E (E-cadherin) was significantly decreased in the kidneys of HN mice, and E. longifolia alkaloid components successfully inhibited its expression (Fig. 5e, g). The contractile protein α-smooth muscle actin (α-SMA) expressed by mesenchymal fibroblasts has been regarded as a key fibrotic factor and plays a vital role in the progression of renal fibrosis. In our research, the enhanced renal expression of α-SMA was found in HN mice, and its expression was inhibited after being treated with E. longifolia alkaloid components (Fig. 5h). Therefore, E. longifolia alkaloid components can alleviate tubular interstitial fibrosis in HN mice.
E. Longifolia alkaloid monomer could reduce cellular uric acid uptake, inhibit NF- κB and NLRP3 / Caspase 1 signaling pathway activation
Inhibition of E. longifolia alkaloid monomer on uric acid uptake in hURAT1-HEK293T cells
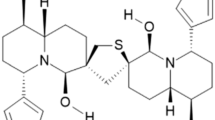
As shown in Fig. 6a, we identified 6 major alkaloids from E. longifolia. By comparing its chemical and spectral data with the data reported in the literature, it is determined that its structure is 4-methoxy-5-hydroxycanthin-6-one (1), 9,10-dimethoxycanthin-6-one (2), 4,9-dimethoxycanthin-6-one (3), 5-methoxy-canthin-6-one (4), canthin-6-one (5), and 9-methoxycanthin-6-one (6). Due to the crucial role of URAT1 in renal urate reabsorption, hURAT1-HEK293T cells were used to determine the effect of E. longifolia alkaloid components on urate reabsorption. Role in urate reabsorption in kidney, hURAT1-HEK293T cells were used to determine the effects of urate uptake regulation role of alkaloid components from E. longifolia. As shown in Fig. 6b, uric acid absorption increased significantly in cells expressing hURAT1. 1 µmol/L RDEA3170 and 5 µmol/L Compounds 1, 2, and 5 could reduce the uric acid uptake of hURAT1-expressing cells, while Compounds 3, 4, and 6 showed relatively low activity, indicating that the alkaloids in E. longifolia could inhibit URAT1.
Effects of E. longifolia alkaloid monomer on uric acid uptake in hURAT1-HEK293T cells. A Chemical structure of E. longifolia alkaloid monomer. B Uric acid concentration in hURAT1-HEK293T cells. Sham: blank control group; control: 100 mol/L urate group; RDEA: 1 μmol/L RDEA; Compounds 1–6: 5 μmol/L Compound 1-6. The data are shown as mean ± S.E.M (n = 5). Compared with Sham group, ###P < 0.001; compared with HN group, *P < 0.05, ***P < 0.001
Analysis of compound-target-pathway network of E. longifolia
To explain the potential pharmacological effects of E. longifolia in the treatment of HN, E. longifolia alkaloids were tested using network pharmacology. The results showed that Compounds 2, 5, and 6 targeted the inflammatory signal pathway, among which Compounds 2 and 6 TNF and IL-17 targeted signal pathway, and Compound 5 targeted the IL-17 signal pathway (Fig. 7). It has been confirmed by us that Compounds 2 and 5 have a significant inhibitory effect on uric acid absorption. Based on this result, we subsequently conducted follow-up in vitro experiments on Compounds 2 and 5 to explore the inhibitory effect and related mechanisms of Compounds 2 and 5 on hyperuric-acid-induced renal tubular epithelial cells NRK52E verification.
Compounds 2 and 5 alleviate pro-inflammatory effects by inhibiting the activation of NF-κB and NLRP3/Caspase 1 signaling pathways in uric-acid-stimulated NRK52E cells
We explored the effect of Compounds 2 and 5 in uric-acid-treated rat proximal tubule epithelial NRK52E cells. Further western blotting results demonstrated that Compounds 2 and 5 can inhibit the pro-inflammatory production induced by uric acid in a dose-dependent manner (Fig. 8a–d), which were consistent with E. longifolia in vivo. We further verified the mechanism by which Compounds 2 and 5 alleviate HN in NRK52E cells stimulated by uric acid. It was found that Compounds 2 and 5 inhibited the expression of NLRP3 and Caspase 1 induced by uric acid (Fig. 8e–g). In addition, the expression of α-SMA and NF-κB, the phosphorylation of NF-κB induced by uric acid was largely suppressed by compound 5 (Fig. 8h–k).
Effects of Compounds 2 and 5 on the pro-inflammatory effect in uric-acid-stimulated NRK52E cells. A The protein expression levels of MCP-1, IL-1β, and TNF-α were determined. B–D The ratio of MCP-1, IL-1β, and TNF-α to β-actin was calculated. E The protein expression levels of Caspase 1 and NLRP3 were determined. F–G The ratio of Caspase 1 and NLRP3 to β-actin was calculated. H The protein expression levels of NK-κB and p-NK-κB were determined. I–J The ratio of NK-κB and p-NK-κB to β-actin was calculated. K The protein expression levels of α-SMA were determined. Nor: blank control group; control: 100 mol/L urate group; Compound 2 or 5: 5 μmol/L Compound 2 or 5; CY-09: an inhibitor of NLRP3; JSH- an inhibitor of NF-κB. The data are shown as mean ± S.E.M (n = 5). Compared with Nor group, ##P < 0.01, ###P < 0.001; compared with control group, *P < 0.05, **P < 0.01.***P < 0.001
Discussion
HUA is an independent risk factor for chronic kidney disease (CKD), hypertension, cardiovascular and cerebrovascular diseases, diabetes, metabolic syndrome, atherosclerosis [21, 23]. With the increase of the prevalence of HUA, the incidence of related complications has also increased, seriously endangering human health [21]. Epidemiological studies show that the incidence of renal disease in Chinese patients with HUA is as high as 15.1%, while the incidence of HN in people with normal blood uric acid is 2.9% [23]. The traditional uric-acid-lowering drugs, allopurinol and benzbromarone, could not reduce the damage of visceral function in HN [11]. Therefore, it is necessary to develop new treatments to prevent renal inflammation and fibrosis caused by HUA to improve the prognosis of HN.
Traditional natural medicine has the advantages of multi-target and low toxicity. Traditional natural medicine has been widely used in the treatment of patients with HN. E. longifolia has a variety of pharmacological properties, such as reducing blood sugar, blood pressure, and serum uric acid levels [17, 18]. In addition, as the main active component of E. longifolia, alkaloids have been proved to be effective inhibitors of NF-κB in vitro, but the renal protective effect and mechanism of E. longifolia on HUA remain unknown [24]. The purpose of this study was to investigate the effect and potential mechanism of E. longifolia alkaloid components in HN induced by adenine and potassium oxonate in mice. Our data suggested that oral E. longifolia alkaloid components could reduce the level of serum uric acid, alleviate kidney inflammation and renal fibrosis, thereby effectively relieving renal insufficiency caused by HUA.
Uric-acid-lowering treatment may help to prevent or alleviate the progression of CKD [25]. Consistent with this, in our study, the reduction of high uric acid by E. longifolia alkaloid components was accompanied by the improvement of renal function. Similarly, we found that E. longifolia alkaloid components potentially reduce uric acid by promoting the excretion of uric acid in the kidney and restoring the expression of uric acid transporter. In addition, E. longifolia alkaloid components inhibited the expression of PRPS and promoted the expression of HPRT in liver, thereby reducing uric acid production. Previous studies have shown that uric acid excretion disorder is initially caused by abnormal expression of urate transporters in proximal tubules. Our study confirmed that the expression of OAT1 and ABCG2 was maladjusted in HN mice, and the alkaloid component of E. longifolia significantly increased the expression of these proteins.
It was found that uric acid not only caused renal injury by crystal-dependent inflammatory reaction, but also caused indirect renal injury by amorphous effect [26, 27]. The level of serum uric acid in patients with HN increased significantly, accompanied by obvious renal pathological changes, mainly manifested in the infiltration of a large number of inflammatory cells and macrophages, interstitial inflammatory reaction and renal tubulointerstitial fibrosis. Whether in the form of MSU crystal or soluble urate, the mechanism of renal injury caused by uric acid is related to the participation of inflammatory response [8]. In addition, uric acid activates nuclear factor NF-κB in rat renal tubular epithelial cells (NRK-52E), promoting the expression of inflammation related cytokines such as MCP-1 and RANTES, induces renal inflammation [9]. Uric acid can induce renal interstitial inflammatory cell infiltration, and the infiltrated inflammatory cells can release pro-inflammatory chemokines and cytokines, promoting the occurrence and development of kidney disease [28]. We detected the level of renal inflammation in HN mice by CD68 immunohistochemistry, qRT-PCR, and ELISA. The results showed that the alkaloid component of E. longifolia significantly reduced the infiltration of inflammatory cells in the kidney and significantly reduced inflammatory factor and chemokine IL-1 β、TNF-α. The above results showed that the alkaloid component of E. longifolia reduced renal inflammation by downregulating the expression of inflammatory factors and chemokines. Uric-acid-induced renal inflammation was confirmed to be associated with transcription factors (such as NF-κB) and NLRP3 / IL-1β signal pathway [7]. Our results showed that the alkaloid component of E. longifolia could significantly downregulate phosphorylated NF-κB and its upstream IκBα. It can also downregulate the expression of NLRP3 and Caspase 1, thereby inhibiting activation of NF- κB and NLRP3/IL-1β signal pathway.
Uric acid can also induce vascular wall thickening through amorphous effect, resulting in renal cavity occlusion and insufficient perfusion, leading to renal tubulointerstitial inflammation [29]. Studies have shown that uric acid can induce the transformation of renal tubular epithelial cells into interstitial cells, resulting in renal tubular interstitial fibrosis [30]. Uric acid induces a large amount of accumulation of extracellular matrix (ECM), a key step of renal interstitial fibrosis, by activating the process of renal tubular epithelial mesenchymal transition (EMT), which eventually leads to renal tubular interstitial fibrosis [30]. Renal tubular interstitial fibrosis is an important pathological process in the progression of CKD to end-stage renal disease, and Collagen 1 is a key component of interstitial matrix. EMT is characterized by decreased expression of E-cadherin in epithelial cells, accompanied by increased expression of interstitial cell marker α-SMA. Uric-acid-lowering treatment has become a new treatment for renal injury in patients with HN. Studies have shown that in the CKD rat model, the damage of renal tubules caused the uric acid transporter to fail to function, and the increase in uric acid levels was mainly the result of reduced uric acid filtration in the glomerulus [24]. Therefore, when kidney injury occurs, the effect of uric-acid-lowering drugs that target renal transporters may be reduced [11]. In this study, western blot showed that the alkaloid component of E. longifolia could downregulated the expression of α-SMA and collagen 1, upregulated the expression of E-cadherin, which revealed that the alkaloid component of E. longifolia inhibited the process of epithelial interstitial, and then improved renal fibrosis induced by high uric acid.
Subsequently, in vitro experiments, we further verified the inhibitory effect of E. longifolia alkaloid monomer on uric acid reabsorption and uric-acid-induced inflammation of renal tubular epithelial cells. The results showed that Compounds 1, 2, and 5 could inhibit the accumulation of uric acid and reduce the intracellular uric acid concentration in hURAT1-HEK293T cells. Combined with the results of network pharmacology, Compounds 2, 5, and 6 can target TNF and IL-17 inflammatory pathways. We used uric-acid-induced NRK-52E inflammatory model to detect the anti-inflammatory effect of alkaloid monomers Compounds 2 and 5, and found that Compounds 2 and 5 can reduce inflammatory factor IL-1 β, MCP-1, and TNF-α by inhibiting the activation of NF-κB and NLRP3 inflammatory signaling pathways. Compounds 2 and 5 are Canthin-6-one alkaloids. Canthin-6-one alkaloids have been proved to be effective inhibitors of NF-κB. Therefore, we speculate that Canthin-6-one alkaloids may be the main uric-acid-lowering active components of E. longifolia.
Conclusion
In conclusion, the alkaloid component of E. longifolia had preventive and therapeutic effects on nephropathy caused by HUA. E. longifolia alkaloid components not only played a role in reducing uric acid by regulating hepatic uric acid synthase and renal uric acid transporter, but also reduced renal inflammation and fibrosis in HN mice through NF-κB and NLRP3 signaling pathway. Therefore, the alkaloid component of E. longifolia may be a promising natural drug for HN.
Abbreviations
- ABCG2:
-
ATP-binding cassette super family G number 2
- BUN:
-
Blood urea nitrogen
- cDNA:
-
Complemental deoxyribonucleic acid
- Cur:
-
Clearance of uric acid
- ELISA:
-
Enzyme-linked immunosorbent assay
- E-cadherin:
-
Calcium-dependent cell adhesion molecule
- EMT:
-
Epithelial-to-mesenchymal transition
- ECM:
-
Extracellular matrix
- GAPDH:
-
Glyceraldehyde-3-phosphate dehydrogenase
- GLUT9:
-
Glucose transporter 9
- GMP:
-
Guanosine monophosphate
- H&E:
-
Hematoxylin–eosin staining
- HPRT:
-
Hypoxanthine-guanine phosphoribosyl transferase
- IL-1β:
-
Interleukin-1β
- Masson:
-
Masson-trichrome staining
- MCP-1:
-
Monocyte chemoattractant protein-1
- NF-κB:
-
Nuclear factor-kappa B
- NLRP3:
-
Nod-like receptor pyrin domain-containing protein 3
- OAT1:
-
Organic anion transporter 1
- PAS:
-
Periodic acid Schiff reaction
- PBS:
-
Phosphate buffered saline
- qRT-PCR:
-
Real-time quantitative polymerase chain reaction
- PRPS:
-
Phosphoribosyl pyrophosphate synthetase
- RANTES:
-
Chemokine (C–C motif) ligand 5
- TNF-α:
-
Tumor necrosis factor-α
- UPLC:
-
Ultra-performance liquid chromatography
- URAT1:
-
Urate-anion transporter
- α-SMA:
-
1α-Smooth muscle actin
References
Weiner DE, Tighiouart H, Elsayed EF, Griffith JL, Salem DN, Levey AS (2008) Uric acid and incident kidney disease in the community. J Am Soc Nephrol 19:1204–1211. https://doi.org/10.1681/ASN.2007101075
Obermayr RP, Temml C, Gutjahr G, Knechtelsdorfer M, Oberbauer R, Klauser-Braun R (2008) Elevated uric acid increases the risk for kidney disease. J Am Soc Nephrol 19:2407–2413. https://doi.org/10.1681/ASN.2008010080
Juraschek SP, Kovell LC, Miller ER, Gelber AC (2013) Dose-response association of uncontrolled blood pressure and cardiovascular disease risk factors with hyperuricemia and gout. PLoS ONE. https://doi.org/10.1371/journal.pone.0056546
Mazzali M, Hughes J, Kim YG et al (2001) Elevated uric acid increases blood pressure in the rat by a novel crystal-independent mechanism. Hypertension 38:1101–1106. https://doi.org/10.1161/hy1101.092839
Ryu ES, Kim MJ, Shin HS et al (2013) Uric acid-induced phenotypic transition of renal tubular cells as a novel mechanism of chronic kidney disease. Am J Physiol Renal Physiol 304:F471-480. https://doi.org/10.1152/ajprenal.00560.2012
Wang Y, Bao X (2013) Effects of uric acid on endothelial dysfunction in early chronic kidney disease and its mechanisms. Eur J Med Res 18:26. https://doi.org/10.1186/2047-783X-18-26
Yin W, Zhou QL, OuYang SX, Chen Y, Gong YT, Liang YM (2019) Uric acid regulates NLRP3/IL-1β signaling pathway and further induces vascular endothelial cells injury in early CKD through ROS activation and K+ efflux. BMC Nephrol. https://doi.org/10.1186/s12882-019-1506-8
Maejima I, Takahashi A, Omori H et al (2013) Autophagy sequesters damaged lysosomes to control lysosomal biogenesis and kidney injury. EMBO J 32:2336–2347. https://doi.org/10.1038/emboj.2013.171
Zhou Y, Fang L, Jiang L et al (2012) Uric acid induces renal inflammation via activating tubular NF-κB signaling pathway. PLoS ONE. https://doi.org/10.1371/journal.pone.0039738
Chen IH, Kuo MC, Hwang SJ, Chang JM, Chen HC (2005) Allopurinol-induced severe hypersensitivity with acute renal failure. Kaohsiung J Med Sci 21:228–232. https://doi.org/10.1016/S1607-551X(09)70192-5
Fujimori S, Ooyama K, Ooyama H, Moromizato H (2011) Efficacy of benzbromarone in hyperuricemic patients associated with chronic kidney disease. Nucleosides Nucleotides Nucleic Acids 30:1035–1038. https://doi.org/10.1080/15257770.2011.622732
Rehman SU, Choe K, Yoo HH (2016) Review on a traditional Herbal medicine, Eurycoma longifolia Jack (Tongkat Ali): Its traditional uses, chemistry. Evid-Based Pharm Toxicol Mol 21(3):331. https://doi.org/10.3390/molecules21030331
Chua LS, Amin NA, Neo JC et al (2011) LC-MS/MS-based metabolites of Eurycoma longifolia (Tongkat Ali) in Malaysia (Perak and Pahang). J. Chromatogr B Analyt Technol Biomed Life Sci 879:3909–3919. https://doi.org/10.1016/j.jchromb.2011.11.002
Thu HE, Mohamed IN, Hussain Z, Jayusman PA, Shuid AN (2017) Eurycoma longifolia as a potential adoptogen of male sexual health: A systematic review on clinical studies. Chin J Nat Med 15(1):71–80. https://doi.org/10.1016/S1875-5364(17)30010-9
Low BS, The CH, Yuen KH, Chan KL (2011) Physicochemical effects of the major quassinoids in a standardized Eurycoma longifolia extract (Fr 2) on the bioavailability and pharmacokinetic properties, and their implications for oral antimalarial activity. Nat Prod Commun 6:337–341. https://doi.org/10.1177/1934578X1100600307
Varghese C, Ambrose C, Jin S, Lim Y, Keisaban T (2013) Antioxidant and anti-inflammatory activity of Eurycoma longifolia Jack, A traditional medicinal plant in Malaysia. Int J Pharm Sci Nanotechnol 5:1875–1878. https://doi.org/10.37285/ijpsn.2012.5.4.7
Lahrita L, Kato E, Kawabata J (2015) Uncovering potential of Indonesian medicinal plants on glucose uptake enhancement and lipid suppression in 3T3-L1 adipocytes. J Ethnopharmacol 168:229–236. https://doi.org/10.1016/j.jep.2015.03.082
Bao R, Liu M, Wang D et al (2019) Effect of Eurycoma longifolia stem extract on uric acid excretion in Hyperuricemia Mice. Front Pharmacol 10:1464. https://doi.org/10.3389/fphar.2019.01464
Thu HE, Hussain Z, Mohamed IN, Shuid AN (2018) Eurycoma longifolia, a potential phytomedicine for the treatment of cancer: Evidence of p53-mediated apoptosis in cancerous cells. Curr Drug Targets 19(10):1109–1126. https://doi.org/10.2174/1389450118666170718151913
Zhang ZX, Wang ZD, Zhang Y, Zhang Y, Han LF, Tian F (2021) Preparation of a poly 2-thiopheneacetic acid) coating on magnetite nanoparticles with one single carbon layer (Fe3O4@1C NPs) for selective magnetic solid-phase extraction of canthin-6-one Alkaloids in Eurycoma longifolia. Chromatographia 84:1065–1075. https://doi.org/10.1007/s10337-021-04090-3
Perez-Ruiz F, Calabozo M, Erauskin GG, Ruibal A, Herrero-Beites AM (2002) Renal underexcretion of uric acid is present in patients with apparent high urinary uric acid output. Arthritis Rheum 47:610–613. https://doi.org/10.1002/art.10792
Wen S, Wang D, Yu H et al (2020) The time-feature of uric acid excretion in hyperuricemia mice induced by potassium oxonate and adenine. Int J Mol Sci. https://doi.org/10.3390/ijms21155178
Elfishawi MM, Zleik N, Kvrgic Z et al (2018) The rising incidence of gout and the increasing burden of comorbidities: a population-based study over 20 years. J Rheumatol 45:574–579. https://doi.org/10.3899/jrheum.170806
Tran TV, Malainer C, Schwaiger S et al (2014) NF-κB inhibitors from Eurycoma longifolia. J Nat Prod 77:483–488. https://doi.org/10.1021/np400701k
Kumagai T, Ota T, Tamura Y, Chang WX, Shibata S, Uchida S (2017) Time to target uric acid to retard CKD progression. Clin Exp Nephrol 21:182–192. https://doi.org/10.1007/s10157-016-1288-2
Feig DI, Rodriguez-Iturbe B, Nakagawa T, Johnson RJ (2006) Nephron number, uric acid, and renal microvascular disease in the pathogenesis of essential hypertension. Hypertension 48:25–26. https://doi.org/10.1161/01.HYP.0000223447.53155.d5
Ryu ES, Kim MJ, Shin HS et al (2013) Uric acid-induced phenotypic transition of renal tubular cells as a novel mechanism of chronic kidney disease. Am J Physiol Renal Physiol 304:471–480. https://doi.org/10.1152/ajprenal.00560.2012
Kono H, Chen CJ, Ontiveros F, Rock KL (2010) Uric acid promotes an acute inflammatory response to sterile cell death in mice. J Clin Invest 120:1939–1949. https://doi.org/10.1172/JCI40124
Zhou TB, Qin YH, Lei FY, Huang WF, Drummen GP (2014) Association of prohibitin-1 and 2 with oxidative stress in rats with renal interstitial fibrosis. Mol Biol Rep 41:3033–3043. https://doi.org/10.1007/s11033-014-3162-1
Zeisberg EM, Potenta SE, Sugimoto H, Zeisberg M, Kalluri R (2008) Fibroblasts in kidney fibrosis emerge via endothelial-to-mesenchymal transition. J Am Soc Nephrol 19:2282–2287. https://doi.org/10.1681/ASN.2008050513
Acknowledgements
The authors thank HY Cao for her help in the experiment in this study.
Funding
This research was funded by Important Drug Development Fund, Ministry of Science and Technology of China (2018ZX09735-002), National Natural Science Foundation of China (81173524; 81673688), and The Scientific Research Project of Tianjin Municipal Education Commission (2019KJ085).
Author information
Authors and Affiliations
Contributions
LL, DW, YZ, and TW completed the experimental design. KL, ML, QC, and HC were responsible for conducting experiments and analyzing data. DW and TW were responsible for writing the manuscript. ML, YZ, and TW checked the manuscript. TW and DW provided the funding.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, D., Liu, L., Li, K. et al. Eurycoma longifolia alkaloid components ameliorate hyperuricemic nephropathy via regulating serum uric acid level and relieving inflammatory reaction. J Nat Med 77, 867–879 (2023). https://doi.org/10.1007/s11418-023-01729-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-023-01729-3